Machine Learning Analysis of the Anatomical Parameters of the Upper Airway Morphology: A Retrospective Study from Cone-Beam CT Examinations in a French Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Data Acquisition
2.3. Radiographic Analysis
2.4. Volume Reorientation
2.5. Volume Segmentation, Volume, and Minimal Cross-Sectional Area (CSAmin)
2.6. Landmarks
2.7. Statistical Analyses
3. Results
3.1. Study Sample
3.2. Reproducibility of Measurements
3.3. Descriptive Analysis
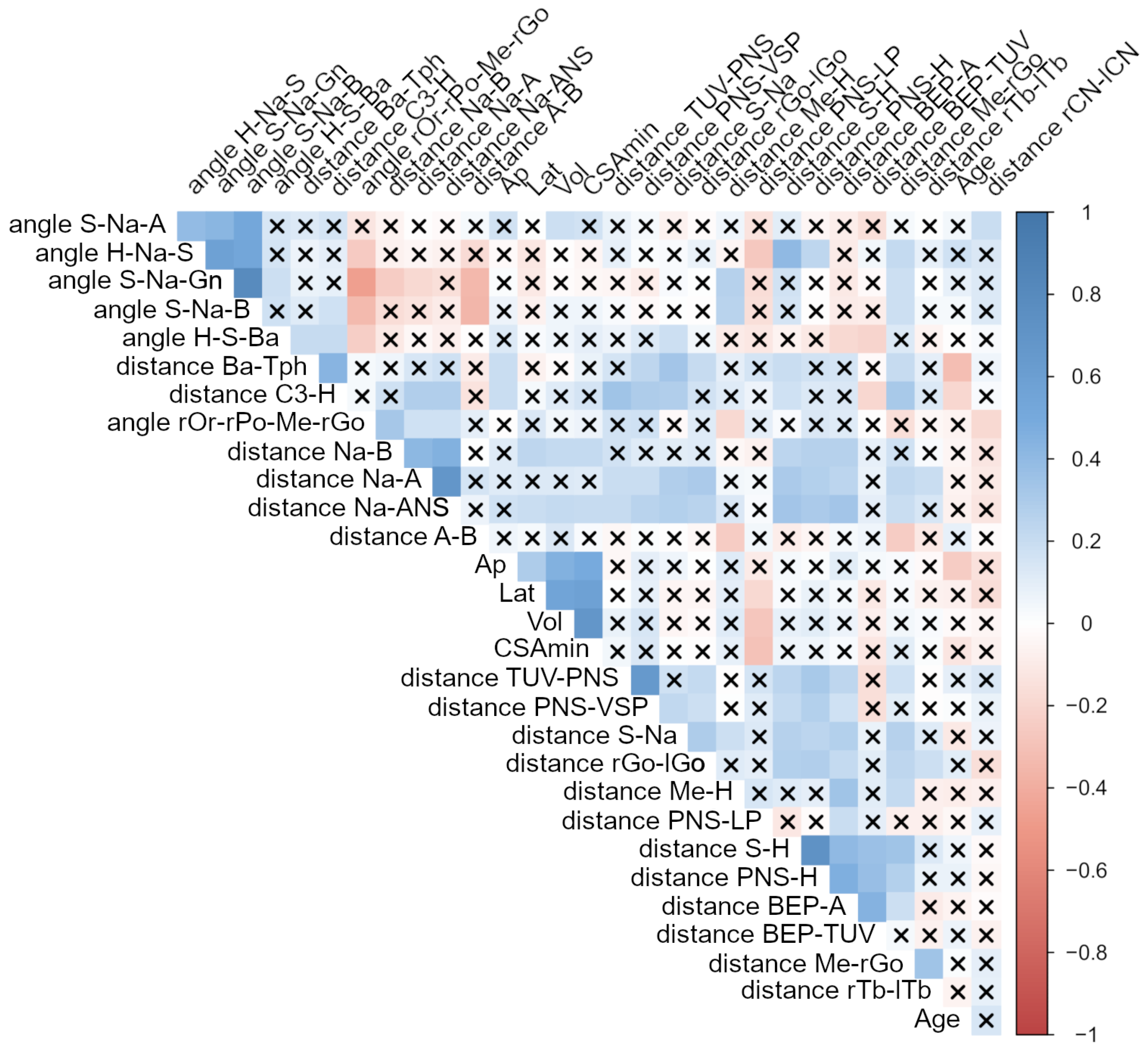
3.4. Bi-Variate Analysis
3.5. Results from the Principal Component Analysis
3.6. Machine Learning Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yitschaky, O.; Redlich, M.; Abed, Y.; Faerman, M.; Casap, N.; Hiller, N. Comparison of common hard tissue cephalometric measurements between computed tomography 3D reconstruction and conventional 2D cephalometric images. Angle Orthod. 2011, 81, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Bruwier, A.; Poirrier, R.; Albert, A.; Maes, N.; Limme, M.; Charavet, C.; Milicevic, M.; Raskin, S.; Poirrier, A.L. Analyse tridimensionnelle des os craniofaciaux et des tissus mous dans l’apnée obstructive du sommeil utilisant la tomographie volumétrique à faisceau conique. Int. Orthod. 2016, 14, 449–461. [Google Scholar] [CrossRef] [PubMed]
- Friedlander-Barenboim, S.; Hamed, W.; Zini, A.; Yarom, N.; Abramovitz, I.; Chweidan, H.; Finkelstein, T.; Almoznino, G. Patterns of Cone-Beam Computed Tomography (CBCT) Utilization by Various Dental Specialties: A 4-Year Retrospective Analysis from a Dental and Maxillofacial Specialty Center. Healthcare 2021, 9, 1042. [Google Scholar] [CrossRef] [PubMed]
- Maret, D.; Vergnes, J.N.; Peters, O.A.; Peters, C.; Nasr, K.; Monsarrat, P. Recent Advances in Cone-beam CT in Oral Medicine. Curr. Med. Imaging 2020, 16, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Portelli, M.; Militi, A.; Lo Giudice, A.; Lo Giudice, R.; Fastuca, R.; Ielo, I.; Mongelli, V.; Lo Giudice, G.; Martintoni, A.; Manuelli, M.; et al. Standard and low-dose cone beam computer tomography protocol for orthognatodontic diagnosis: A comparative evaluation. J. Biol. Regul. Homeost. Agents 2018, 32, 59–66. [Google Scholar]
- Zimmerman, J.N.; Lee, J.; Pliska, B.T. Reliability of upper pharyngeal airway assessment using dental CBCT: A systematic review. Eur. J. Orthod. 2017, 39, 489–496. [Google Scholar] [CrossRef] [PubMed]
- Buchanan, A.; Cohen, R.; Looney, S.; Kalathingal, S.; De Rossi, S. Cone-beam CT analysis of patients with obstructive sleep apnea compared to normal controls. Imaging Sci. Dent. 2016, 46, 9–16. [Google Scholar] [CrossRef][Green Version]
- Guijarro-Martínez, R.; Swennen, G.R.J. Cone-beam computerized tomography imaging and analysis of the upper airway: A systematic review of the literature. Int. J. Oral Maxillofac. Surg. 2011, 40, 1227–1237. [Google Scholar] [CrossRef]
- Enciso, R.; Nguyen, M.; Shigeta, Y.; Ogawa, T.; Clark, G.T. Comparison of cone-beam CT parameters and sleep questionnaires in sleep apnea patients and control subjects. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 285–293. [Google Scholar] [CrossRef]
- Alsufyani, N.A.; Noga, M.L.; Witmans, M.; Major, P.W. Upper airway imaging in sleep-disordered breathing: Role of cone-beam computed tomography. Oral Radiol. 2017, 33, 161–169. [Google Scholar] [CrossRef]
- Alsufyani, N.A.; Al-Saleh, M.A.Q.; Major, P.W. CBCT assessment of upper airway changes and treatment outcomes of obstructive sleep apnoea: A systematic review. Sleep Breath. 2013, 17, 911–923. [Google Scholar] [CrossRef] [PubMed]
- Glupker, L.; Kula, K.; Parks, E.; Babler, W.; Stewart, K.; Ghoneima, A. Three-dimensional computed tomography analysis of airway volume changes between open and closed jaw positions. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Aarab, G.; Parsa, A.; de Lange, J.; van der Stelt, P.F.; Lobbezoo, F. Reliability of three-dimensional measurements of the upper airway on cone beam computed tomography images. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 122, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.Y. Correlation between hyoid bone position and airway dimensions in Chinese adolescents by cone beam computed tomography analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Alsufyani, N.A.; Flores-Mir, C.; Major, P.W. Three-dimensional segmentation of the upper airway using cone beam CT: A systematic review. Dentomaxillofac. Radiol. 2012, 41, 276–284. [Google Scholar] [CrossRef]
- Chen, H.; Li, Y.; Reiber, J.H.; de Lange, J.; Tu, S.; van der Stelt, P.; Lobbezoo, F.; Aarab, G. Analyses of aerodynamic characteristics of the oropharynx applying CBCT: Obstructive sleep apnea patients versus control subjects. Dentomaxillofac. Radiol. 2018, 47, 20170238. [Google Scholar] [CrossRef]
- Eslami, E.; Katz, E.S.; Baghdady, M.; Abramovitch, K.; Masoud, M.I. Are three-dimensional airway evaluations obtained through computed and cone-beam computed tomography scans predictable from lateral cephalograms? A systematic review of evidence. Angle Orthod. 2017, 87, 159–167. [Google Scholar] [CrossRef]
- Ghoneima, A.; Kula, K. Accuracy and reliability of cone-beam computed tomography for airway volume analysis. Eur. J. Orthod. 2013, 35, 256–261. [Google Scholar] [CrossRef]
- Schlicher, W.; Nielsen, I.; Huang, J.C.; Maki, K.; Hatcher, D.C.; Miller, A.J. Consistency and precision of landmark identification in three-dimensional cone beam computed tomography scans. Eur. J. Orthod. 2012, 34, 263–275. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Low, C.; Flores-Mir, C.; Chung, R.; Carey, J.P.; Heo, G.; Major, P.W. Intraexaminer and interexaminer reliabilities of landmark identification on digitized lateral cephalograms and formatted 3-dimensional cone-beam computerized tomography images. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 598–604. [Google Scholar] [CrossRef]
- Souza, K.R.S.d.; Oltramari-Navarro, P.V.P.; Navarro, R.d.L.; Conti, A.C.d.C.F.; Almeida, M.R.d. Reliability of a method to conduct upper airway analysis in cone-beam computed tomography. Braz. Oral Res. 2013, 27, 48–54. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nalçaci, R.; Oztürk, F.; Sökücü, O. A comparison of two-dimensional radiography and three-dimensional computed tomography in angular cephalometric measurements. Dentomaxillofac. Radiol. 2010, 39, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Aarab, G.; de Ruiter, M.H.T.; de Lange, J.; Lobbezoo, F.; van der Stelt, P.F. Three-dimensional imaging of the upper airway anatomy in obstructive sleep apnea: A systematic review. Sleep Med. 2016, 21, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Osorio, F.; Perilla, M.; Doyle, D.J.; Palomo, J.M. Cone beam computed tomography: An innovative tool for airway assessment. Anesth. Analg. 2008, 106, 1803–1807. [Google Scholar] [CrossRef]
- Ludlow, J.B.; Gubler, M.; Cevidanes, L.; Mol, A. Precision of cephalometric landmark identification: Cone-beam computed tomography vs conventional cephalometric views. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 312.e1–312.e10; discussion 312–313. [Google Scholar] [CrossRef]
- Naji, P.; Alsufyani, N.A.; Lagravère, M.O. Reliability of anatomic structures as landmarks in three-dimensional cephalometric analysis using CBCT. Angle Orthod. 2014, 84, 762–772. [Google Scholar] [CrossRef]
- de Oliveira, A.E.F.; Cevidanes, L.H.S.; Phillips, C.; Motta, A.; Burke, B.; Tyndall, D. Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, 256–265. [Google Scholar] [CrossRef]
- Cheng, E.; Chen, J.; Yang, J.; Deng, H.; Wu, Y.; Megalooikonomou, V.; Gable, B.; Ling, H. Automatic Dent-landmark detection in 3-D CBCT dental volumes. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011. [Google Scholar]
- Alsufyani, N.A.; Dietrich, N.H.; Lagravère, M.O.; Carey, J.P.; Major, P.W. Cone beam computed tomography registration for 3-D airway analysis based on anatomic landmarks. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, 371–383. [Google Scholar] [CrossRef]
- Bobak, C.A.; Barr, P.J.; O’Malley, A.J. Estimation of an inter-rater intra-class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales. BMC Med. Res. Methodol. 2018, 18. [Google Scholar] [CrossRef]
- Vladislavleva, K.; Veeramachaneni, K.; Burland, M.; Parcon, J.; O’Reilly, U.M. Knowledge mining with genetic programming methods for variable selection in flavor design. In Proceedings of the 12th Annual Conference on Genetic and Evolutionary Computation—GECCO’10, Portland, OR, USA, 7–11 July 2010; ACM Press: New York, NY, USA, 2010. [Google Scholar]
- Neelapu, B.C.; Kharbanda, O.P.; Sardana, H.K.; Balachandran, R.; Sardana, V.; Kapoor, P.; Gupta, A.; Vasamsetti, S. Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: A systematic review and meta-analysis of cephalometric studies. Sleep Med. Rev. 2017, 31, 79–90. [Google Scholar] [CrossRef]
- Alves, M., Jr.; Baratieri, C.; Mattos, C.T.; Brunetto, D.; Fontes, R.d.C.; Santos, J.R.L.; Ruellas, A.C.d.O. Is the airway volume being correctly analyzed? Am. J. Orthod. Dentofac. Orthop. 2012, 141, 657–661. [Google Scholar] [CrossRef] [PubMed]
- Grauer, D.; Cevidanes, L.S.H.; Styner, M.A.; Ackerman, J.L.; Proffit, W.R. Pharyngeal airway volume and shape from cone-beam computed tomography: Relationship to facial morphology. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wu, W.; Yan, G.; Liu, L.; Liu, H.; Li, G.; Li, J.; Liu, D. Analogue simulation of pharyngeal airflow response to Twin Block treatment in growing patients with Class II1 and mandibular retrognathia. Sci. Rep. 2016, 6, 26012. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, T.; Enciso, R.; Shintaku, W.H.; Clark, G.T. Evaluation of cross-section airway configuration of obstructive sleep apnea. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 102–108. [Google Scholar] [CrossRef]
- El, H.; Palomo, J.M. Measuring the airway in 3 dimensions: A reliability and accuracy study. Am. J. Orthod. Dentofac. Orthop. 2010, 137, S50.e1–S50.e9; discussion S50–S52. [Google Scholar] [CrossRef] [PubMed]
- Shah, D.H.; Kim, K.B.; McQuilling, M.W.; Movahed, R.; Shah, A.H.; Kim, Y.I. Computational fluid dynamics for the assessment of upper airway changes in skeletal Class III patients treated with mandibular setback surgery. Angle Orthod. 2016, 86, 976–982. [Google Scholar] [CrossRef]
- Indriksone, I.; Jakobsone, G. The upper airway dimensions in different sagittal craniofacial patterns: A systematic review. Stomatologija 2014, 16, 109–117. [Google Scholar]
- Lisboa, C.d.O.; Masterson, D.; da Motta, A.F.J.; Motta, A.T. Reliability and reproducibility of three-dimensional cephalometric landmarks using CBCT: A systematic review. J. Appl. Oral Sci. 2015, 23, 112–119. [Google Scholar] [CrossRef]
- Jung, P.K.; Lee, G.C.; Moon, C.H. Comparison of cone-beam computed tomography cephalometric measurements using a midsagittal projection and conventional two-dimensional cephalometric measurements. Korean J. Orthod. 2015, 45, 282–288. [Google Scholar] [CrossRef]
- Hatcher, D.C. Cone beam computed tomography: Craniofacial and airway analysis. Dent. Clin. N. Am. 2012, 56, 343–357. [Google Scholar] [CrossRef]
- Kikuchi, M.; Higurashi, N.; Miyazaki, S.; Itasaka, Y. Facial patterns of obstructive sleep apnea patients using Ricketts’ method. Psychiatry Clin. Neurosci. 2000, 54, 336–337. [Google Scholar] [CrossRef] [PubMed]
- Schwab, R.J.; Pasirstein, M.; Pierson, R.; Mackley, A.; Hachadoorian, R.; Arens, R.; Maislin, G.; Pack, A.I. Identification of upper airway anatomic risk factors for obstructive sleep apnea with volumetric magnetic resonance imaging. Am. J. Respir. Crit. Care Med. 2003, 168, 522–530. [Google Scholar] [CrossRef] [PubMed]
- deBerry Borowiecki, B.; Kukwa, A.; Blanks, R.H. Cephalometric analysis for diagnosis and treatment of obstructive sleep apnea. Laryngoscope 1988, 98, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Noud, M.; Hovis, K.; Gelbard, A.; Sathe, N.A.; Penson, D.F.; Feurer, I.D.; McPheeters, M.L.; Francis, D.O. Patient-reported outcome measures in upper airway–related dyspnea. JAMA Otolaryngol. Head Neck Surg. 2017, 143, 824. [Google Scholar] [CrossRef] [PubMed]
- Hassoumi, A.; Peysakhovich, V.; Hurter, C. Improving eye-tracking calibration accuracy using symbolic regression. PLoS ONE 2019, 14, e0213675. [Google Scholar] [CrossRef]
- Miracle, A.; Mukherji, S. Conebeam CT of the Head and Neck, Part 2: Clinical Applications. Am. J. Neuroradiol. 2009, 30, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Alsubai, S. A Critical Review on the 3D Cephalometric Analysis Using Machine Learning. Computers 2022, 11, 154. [Google Scholar] [CrossRef]
- Orhan, K.; Shamshiev, M.; Ezhov, M.; Plaksin, A.; Kurbanova, A.; Ünsal, G.; Gusarev, M.; Golitsyna, M.; Aksoy, S.; Mısırlı, M.; et al. AI-based automatic segmentation of craniomaxillofacial anatomy from CBCT scans for automatic detection of pharyngeal airway evaluations in OSA patients. Sci. Rep. 2022, 12, 11863. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, R.; Giudice, A.L.; Farronato, M.; Ronsivalle, V.; Allegrini, S.; Musumeci, G.; Spampinato, C. Fully automatic segmentation of sinonasal cavity and pharyngeal airway based on convolutional neural networks. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 824–835.e1. [Google Scholar] [CrossRef]
- Feragalli, B.; Rampado, O.; Abate, C.; Macrì, M.; Festa, F.; Stromei, F.; Caputi, S.; Guglielmi, G. Cone beam computed tomography for dental and maxillofacial imaging: Technique improvement and low-dose protocols. Radiol. Med. 2017, 122, 581–588. [Google Scholar] [CrossRef]
- Dremmen, M.; Wagner, M.; Bosemani, T.; Tekes, A.; Agostino, D.; Day, E.; Soares, B.; Huisman, T. Does the Addition of a “Black Bone” Sequence to a Fast Multisequence Trauma MR Protocol Allow MRI to Replace CT after Traumatic Brain Injury in Children? Am. J. Neuroradiol. 2017, 38, 2187–2192. [Google Scholar] [CrossRef] [PubMed]


| Landmark Reference Lines | Definition (Anatomic Region) |
|---|---|
| A | Deepest anterior point in the concavity of the anterior maxilla |
| ANS | Anterior nasal spine, most anterior point of the nasal spine |
| B | Deepest anterior point in the concavity of the anterior mandible |
| Ba | Basion, most posteroinferior point on the clivus |
| BEP | Base of epiglottis, bottom of epiglottis crypt |
| C3 | Most anterior point of the third cervical vertebral body |
| H | Most anterosuperior point of the hyoid bone |
| lCN | Left nasal cavity |
| lGo | Left mandibular gonion, angle of the left mandibular body |
| lOr | Left orbital, deepest point of the infraorbital margin: lateral-inferior contour of the left orbit |
| lTb | Left tuberosity, distal contour of the left maxillary tuberosity |
| MGNM | Foramen magnum, mid-posterior point of the large opening in the occipital bone |
| Me | Menton, most inferior point of the chin bone |
| Na | Nasion, anterior point at the frontonasal suture |
| Pg | Prognathion, most anterior point of the symphysis of the mandible |
| PNS | Posterior nasal spine, most posterior point of the nasal spine |
| rCN | Right nasal cavity |
| rGo | Right mandibular gonion, angle of the right mandibular body |
| rOr | Right orbital, deepest point of the infraorbital margin: lateral-inferior contour of the right orbit |
| rPo | Right porion, upper point of the right bony ear opening |
| rTb | Right tuberosity, distal contour of the right maxillary tuberosity |
| S | Sella, midpoint of the fossa hypophysealis |
| Tph | Pharyngeal hypertrophy |
| TUV | Tip of uvula, inferior point of caudal margin of the uvula at the mid-sagittal plane |
| Variable | Definition |
|---|---|
| Volume of the upper airway (Vol) | Superior boundary (i.e., the plane across PNS and ANS parallel to Frankfort plane (FH plane))—the inferior boundary (i.e., the plane across the anteroinferior point of the body of the 3rd cervical spinal vertebra parallel to the FH plane) in a mid-sagittal view |
| Minimum cross-sectional area (CSAmin) | The minimum cross-sectional area of the upper airway in an axial view |
| Lateral dimension of the CSAmin (Lat) | Width of CSAmin in a coronal view |
| Anteroposterior dimension of the CSAmin (Ap) | Length of CSAmin in a sagittal view |
| Variable | Definition |
|---|---|
| Related to hard tissues | |
| Mandible dimension | Mid-sagittal view, distance from: Me to rGo, in axial view distance between rGo and lGo |
| Anteroposterior position of maxilla and mandible | Mid-sagittal view, distance from Na to B, or from Na to A |
| Anteroposterior shift | Mid-sagittal view, distance from A to B projected on the Frankfort plane |
| Cranial basis dimension | Mid-sagittal view, distance from S to Na |
| Facial angle (SNPg) | Mid-sagittal view, angle formed by S-Na-Pg |
| FMA angle | Mid-sagittal view, angle formed by Frankfort plane and mandible plane (angle between rPo–rOr–Me–rGo) |
| Localization of hyoid bone | Mid-sagittal view, distance from C3 to H, Me to H, H to PNS, angle formed by H–S–Ba, H–Na–S |
| Maxilla dimension | Mid-sagittal view, distance between rTb and lTb |
| Nasal cavity dimension | Mid-sagittal view, distance from rCN to lCN or from Na to ANS |
| SNA angle | Mid-sagittal view, angle formed by S–Na–A |
| SNB angle | Mid-sagittal view, angle formed by S–Na–B |
| Related to soft tissues | |
| Dimension of the tongue | Mid-sagittal view, distance from BEP to A, from BEP to TUV |
| Horizontal soft palate (HSP) | Mid-sagittal view, distance from the PNS to the vertical line going through the most posterior contour of soft palate |
| Localization of soft palate | Mid-sagittal view, distance from PNS to TUV |
| Pharyngeal tonsils of soft tissue | Mid-sagittal view, distance from Ba to the most anterior point of pharyngeal hypertrophy (TPh) |
| Vertical soft palate (VSP) | Mid-sagittal view, distance from the horizontal line going through the PNS to the tip of soft palate |
| Variable | ICC Intra | p-Value |
|---|---|---|
| CSAmin | 0.94 [0.85; 0.98] | <0.001 |
| CSAmin width (Lat) | 0.70 [0.37; 0.87] | <0.001 |
| CSAmin length (Ap) | 0.77 [0.49; 0.90] | <0.001 |
| Volume | 0.96 [0.91; 0.98] | <0.001 |
| Anteroposterior position of maxilla (Na–A) | 0.74 [0.42; 0.89] | <0.001 |
| Anteroposterior position of mandible (Na–B) | 0.92 [0.81; 0.97] | <0.001 |
| Anteroposterior shift (A–B) | 0.81 [0.58; 0.92] | <0.001 |
| Cranial basis dimension (S–Na) | 0.88 [0.71; 0.95] | <0.001 |
| Dimension of tongue (height: BEP–A) | 0.93 [0.78; 0.97] | <0.001 |
| Dimension of tongue (width: BEP–TUV) | 0.88 [0.72; 0.95] | <0.001 |
| Facial angle (S–Na–Pg) | 0.95 [0.87; 0.98] | <0.001 |
| FMA angle | 0.94 [0.81; 0.98] | <0.001 |
| Horizontal soft palate (PNS–LP: HSP) | 0.76 [0.47; 0.90] | <0.001 |
| Length of the mandible (Me–rGo) | 0.89 [0.74; 0.95] | <0.001 |
| Localization of hyoid bone (C3–H) | 0.97 [0.91; 0.99] | <0.001 |
| Localization hyoid bone (H–Na–S angle) | 0.96 [0.90; 0.98] | <0.001 |
| Localization of hyoid bone (H–PNS) | 0.98 [0.95; 0.99] | <0.001 |
| Localization hyoid bone (H–S–Ba angle) | 0.98 [0.94; 0.99] | <0.001 |
| Localization of hyoid bone (Me–H) | 0.91 [0.77; 0.96] | <0.001 |
| Localization of hyoid bone (S–H) | 0.98 [0.95; 0.99] | <0.001 |
| Localization of soft palate (TUV–PNS) | 0.73 [0.43; 0.89] | <0.001 |
| Maxilla dimension (rTb–lTb) | 0.83 [0.62; 0.93] | <0.001 |
| Nasal dimension (width: rCN–lCN) | 0.60 [0.23; 0.82] | <0.001 |
| Nasal dimension (height: Na–ANS) | 0.84 [0.60; 0.94] | <0.001 |
| SNA angle | 0.67 [0.34; 0.86] | <0.001 |
| SNB angle | 0.93 [0.84; 0.97] | <0.001 |
| Thickness of soft tissue—pharyngeal hypertrophy (Ba-Tph) | 0.74 [0.45; 0.89] | <0.001 |
| Vertical soft palate (PNS–VSP) | 0.50 [0.10; 0.77] | <0.001 |
| Width of the mandible (rGo–lGo) | 0.89 [0.33; 0.97] | <0.001 |
| Variable | Average ± SD | Median [Q1; Q3] | Min; Max |
|---|---|---|---|
| Age | 39.9 ± 13.5 | 40 [27.5; 50.0] | 22–72 |
| Anteroposterior position of mandible (Na–B, mm) | 94.6 ± 7.5 | 94.0 [90.5; 97.7] | 77.1; 118 |
| Anteroposterior position of maxilla (Na–A, mm) | 57.1 ± 4.1 | 56.4 [54.2; 59.6] | 47.3; 67.0 |
| Anteroposterior shift (A–B, mm) | 4.0 ± 4.5 | 4.5 [1.4; 6.9] | −12.1; 13.9 |
| Cranial Basis dimension (S–Na, mm) | 66.2 ± 4.1 | 64.8 [63.3; 68.5] | 58.6; 77.9 |
| CSAmin (mm) | 206 ± 123 | 190 [115; 275] | 46; 618 |
| CSAmin Lat (mm) | 27.0 ± 7.0 | 26.0 [22.0; 32.7] | 13.7; 44.6 |
| CSAmin AP (mm) | 10.2 ± 3.6 | 9.7 [7.7; 13.0] | 3.1; 18.8 |
| Dimension of tongue (height: BEP–A, mm) | 85.7 ± 6.9 | 84.0 [80.3; 90.7] | 75.0; 102 |
| Dimension of tongue (width: BEP–TUV, mm) | 30.0 ± 7.2 | 31.5 [25.1; 35.3] | 15.5; 43.8 |
| Facial Angle (S–Na–Pg, °) | 79.0 ± 5.2 | 78.2 [75.9; 83.1] | 68.7; 93.4 |
| FMA Angle (°) | 33.3 ± 6.5 | 33.2 [28.1; 37.7] | 18.2; 48.1 |
| Horizontal soft palate (PNS–LP: HSP, mm) | 19.1 ± 4.5 | 19.0 [15.5; 21.8] | 11.1; 34.9 |
| Length of the mandible (Me–rGo, mm) | 83.0 ± 6.4 | 83.2 [79.6; 87.2] | 57.5; 95.8 |
| Localization of hyoid bone (C3–H, mm) | 34.6 ± 4.8 | 34.1 [31.1; 37.2] | 25.8; 45.2 |
| Localization of hyoid bone (H–S–Ba angle, °) | 39.4 ± 6.4 | 39.3 [33.8; 43.6] | 25.6; 54.7 |
| Localization of hyoid bone (H–Na–S angle, °) | 56.1 ± 4.3 | 56.0 [52.8; 59.2] | 46.8; 68.6 |
| Localization of hyoid bone (S–H, mm) | 103 ± 8.8 | 102 [97.1; 109] | 77.9; 122 |
| Localization of hyoid bone (Me–H, mm) | 42.0 ± 4.8 | 42.0 [38.9; 45.9] | 27.7; 51.7 |
| Localization of hyoid bone (H–PNS, mm) | 61.3 ± 6.9 | 61.4 [56.3; 66.0] | 44.2; 76.0 |
| Localization of soft palate (TUV–PNS, mm) | 36.5 ± 4.3 | 36.9 [33.3; 39.4] | 27.1; 44.9 |
| Maxilla dimension (rTb–lTb, mm) | 49.1 ± 4.0 | 49.5 [45.9; 51.7] | 41.7; 58.3 |
| Nasal dimension (height: Na–ANS, mm) | 50.3 ± 3.6 | 49.9 [48.0; 52.5] | 42.2; 60.5 |
| Nasal dimension (width: rCN–lCN, mm) | 20.5 ± 5.6 | 19.8 [17.5; 22.0] | 12.9; 54.4 |
| SNA Angle (°) | 81.8 ± 4.4 | 81.6 [78.5; 84.5] | 72.8; 92.2 |
| SNB Angle (°) | 77.8 ± 5.0 | 77.3 [74.7; 81.4] | 66.6; 96.5 |
| Thickness of soft tissue—pharyngeal hypertrophy (Ba–Tph, mm) | 18.4 ± 5.1 | 17.5 [14.9; 20.7] | 11.3; 38.9 |
| Vertical soft palate (PNS–VSP, mm) | 36.2 ± 5.0 | 35.5 [33.2; 38.6] | 26.6; 49.0 |
| Volume (mm) | 14,460 ± 7399 | 13,645 [8495; 18,092] | 1614; 40,720 |
| Width of the mandible (lGo–rGo, mm) | 92.0 ± 5.8 | 92.1 [88.4; 96.3] | 78.8; 107 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Bataille, C.; Bernard, D.; Dumoncel, J.; Vaysse, F.; Cussat-Blanc, S.; Telmon, N.; Maret, D.; Monsarrat, P. Machine Learning Analysis of the Anatomical Parameters of the Upper Airway Morphology: A Retrospective Study from Cone-Beam CT Examinations in a French Population. J. Clin. Med. 2023, 12, 84. https://doi.org/10.3390/jcm12010084
de Bataille C, Bernard D, Dumoncel J, Vaysse F, Cussat-Blanc S, Telmon N, Maret D, Monsarrat P. Machine Learning Analysis of the Anatomical Parameters of the Upper Airway Morphology: A Retrospective Study from Cone-Beam CT Examinations in a French Population. Journal of Clinical Medicine. 2023; 12(1):84. https://doi.org/10.3390/jcm12010084
Chicago/Turabian Stylede Bataille, Caroline, David Bernard, Jean Dumoncel, Frédéric Vaysse, Sylvain Cussat-Blanc, Norbert Telmon, Delphine Maret, and Paul Monsarrat. 2023. "Machine Learning Analysis of the Anatomical Parameters of the Upper Airway Morphology: A Retrospective Study from Cone-Beam CT Examinations in a French Population" Journal of Clinical Medicine 12, no. 1: 84. https://doi.org/10.3390/jcm12010084
APA Stylede Bataille, C., Bernard, D., Dumoncel, J., Vaysse, F., Cussat-Blanc, S., Telmon, N., Maret, D., & Monsarrat, P. (2023). Machine Learning Analysis of the Anatomical Parameters of the Upper Airway Morphology: A Retrospective Study from Cone-Beam CT Examinations in a French Population. Journal of Clinical Medicine, 12(1), 84. https://doi.org/10.3390/jcm12010084








