The Efficacy of Different Voice Treatments for Vocal Fold Polyps: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Searches
2.2. Study Selection
2.3. Risk of Bias Assessments
2.4. Statistics
3. Results
3.1. Auditory–Perceptual Judgment
3.2. Acoustics
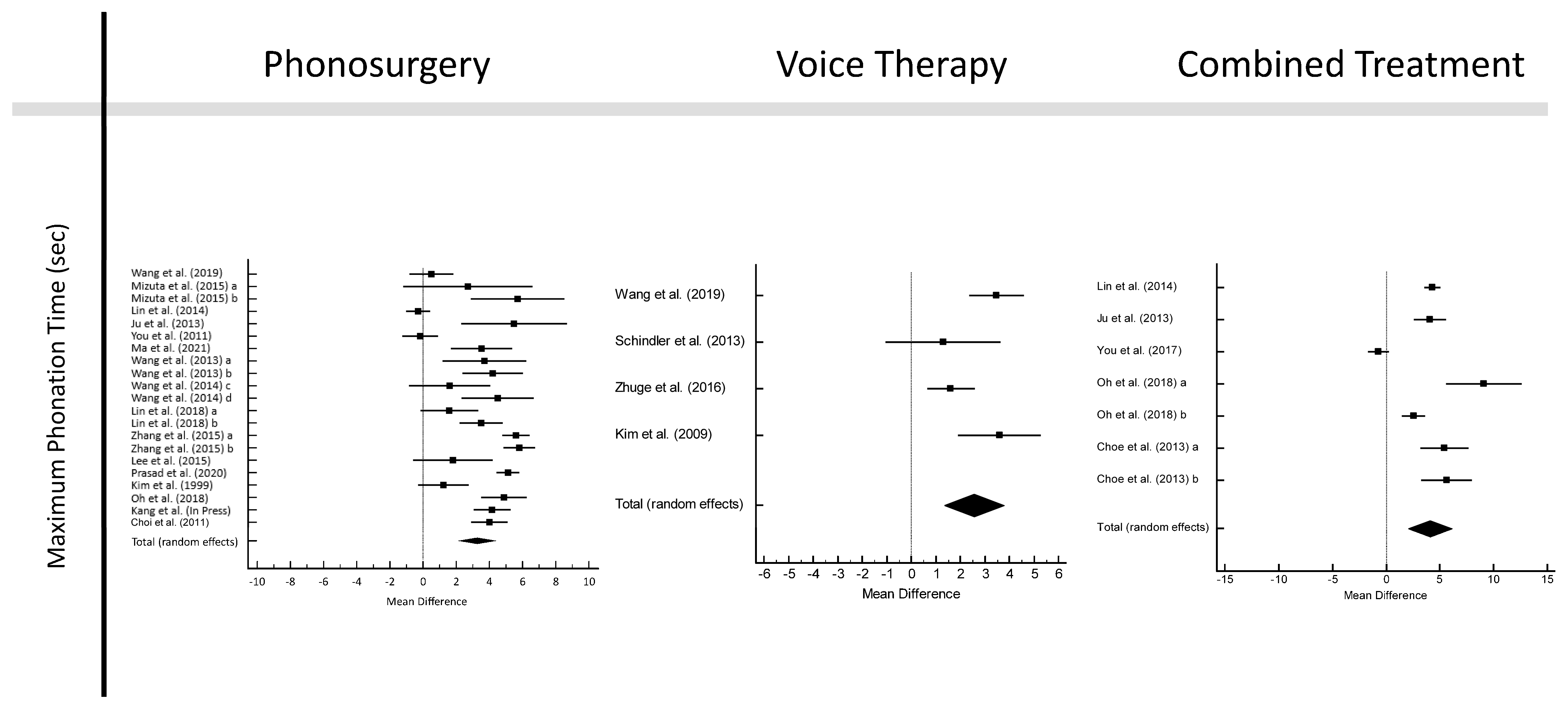
3.3. Maximum Phonation Time
3.4. Voice Handicap Index—30
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vasconcelos, D.; Gomes, A.O.C.; Araújo, C.M.T. Vocal fold polyps: Literature review. Int. Arch. Otorhinolaryngol. 2019, 23, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.J.; Nam, I.C.; Hwang, Y.S.; Shim, M.R.; Park, J.O.; Cho, J.H.; Joo, Y.H.; Kim, M.S.; Sun, D.I. Analysis of factors influencing voice quality and therapeutic approaches in vocal polyp patients. Eur. Arch. Otorhinolaryngol. 2011, 268, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Hah, J.H.; Sim, S.; An, S.Y.; Sung, M.W.; Choi, H.G. Evaluation of the prevalence of and factors associated with laryngeal diseases among the general population. Laryngoscope 2015, 125, 2536–2542. [Google Scholar] [CrossRef] [PubMed]
- Van Houtte, E.; Van Lierde, K.; D’Haeseleer, E.; Claeys, S. The prevalence of laryngeal pathology in a treatment-seeking population with dysphonia. Laryngoscope 2010, 120, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Martins, R.H.; do Amaral, H.A.; Tavares, E.L.; Martins, M.G.; Gonçalves, T.M.; Dias, N.H. Voice disorders: Etiology and diagnosis. J. Voice 2016, 30, 761.e1–761.e9. [Google Scholar] [CrossRef]
- Martins, R.H.; Defaveri, J.; Domingues, M.A.; de Albuquerque e Silva, R. Vocal polyps: Clinical, morphological, and immunohistochemical aspects. J. Voice 2011, 25, 98–106. [Google Scholar] [CrossRef]
- Dejonckere, P.H.; Bradley, P.; Clemente, P.; Cornut, G.; Crevier-Buchman, L.; Friedrich, G.; Van De Heyning, P.; Remacle, M.; Woisard, V.; Committee on Phoniatrics of the European Laryngological Society (ELS). A basic protocol for functional assessment of voice pathology, especially for investigating the efficacy of (phonosurgical) treatments and evaluating new assessment techniques. Guideline elaborated by the Committee on Phoniatrics of the European Laryngological Society (ELS). Eur. Arch. Otorhinolaryngol. 2001, 258, 77–82. [Google Scholar] [CrossRef]
- Öcal, B.; Tatar, E.Ç.; Toptaş, G.; Barmak, E.; Saylam, G.; Korkmaz, M.H. Evaluation of voice quality in patients with vocal fold polyps: The size of a polyp matters or does it? J. Voice 2020, 34, 294–299. [Google Scholar] [CrossRef]
- Sulica, L.; Behrman, A. Management of benign vocal fold lesions: A survey of current opinion and practice. Ann. Otol. Rhinol. Laryngol. 2003, 112, 827–833. [Google Scholar] [CrossRef]
- Cohen, S.M.; Pitman, M.J.; Noordzij, J.P.; Courey, M. Management of dysphonic patients by otolaryngologists. Otolaryngol. Head. Neck Surg. 2012, 147, 289–294. [Google Scholar] [CrossRef]
- Cohen, S.M.; Garrett, C.G. Utility of voice therapy in the management of vocal fold polyps and cysts. Otolaryngol. Head. Neck Surg. 2007, 136, 742–746. [Google Scholar] [CrossRef] [PubMed]
- Stachler, R.J.; Francis, D.O.; Schwartz, S.R.; Damask, C.C.; Digoy, G.P.; Krouse, H.J.; McCoy, S.J.; Ouellette, D.R.; Patel, R.R.; Reavis, C.C.W.; et al. Clinical practice guideline: Hoarseness (dysphonia) (update). Otolaryngol. Head. Neck Surg. 2018, 158, S1–S42. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Sulica, L. Recurrence of benign phonotraumatic vocal fold lesions after microlaryngoscopy. Laryngoscope 2020, 130, 1989–1995. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W65–W94. [Google Scholar] [CrossRef] [PubMed]
- Herbst, C.T.; Oh, J.; Vydrová, J.; Švec, J.G. DigitalVHI—A freeware open-source software application to capture the Voice Handicap Index and other questionnaire data in various languages. Logoped Phoniatr. Vocol 2015, 40, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates: Hillsdale, MI, USA, 1988. [Google Scholar]
- Kim, Y.M.; Cho, J.I.; Kim, C.H.; Kim, Y.J.; Ha, H.R. Vocal dynamic studies before and after laryngeal microsurgery. Korean J. Otolaryngol. 1999, 42, 1174–1178. (In Korean) [Google Scholar]
- Kim, H.T.; Auo, H.J. Office-based 585 nm pulsed dye laser treatment for vocal polyps. Acta Otolaryngol. 2008, 128, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Kluch, W.; Olszewski, J. Videolaryngostroboscopic examination of treatment effects in patients with chronic hyperthrophic larynges. Otolaryngol. Pol. 2008, 62, 680–685. (In Polish) [Google Scholar] [CrossRef] [PubMed]
- Kim, B.S.; Shin, J.H.; Kim, K.Y.; Lee, Y.S.; Kim, K.R.; Tae, K. Change of Acoustic Parameter and Voice Handicap Index after Laryngeal Microsurgery. J. Korean Soc. Laryngol. Phoniatr. Logop. 2008, 19, 142–145. (In Korean) [Google Scholar]
- Kluch, W.; Olszewski, J. The use of laryngostroboscopy in diagnostics and results evaluation of treatment of patients with organic lesions in the larynx. Otolaryngol. Pol. 2009, 63, 11–15. (In Polish) [Google Scholar] [CrossRef] [PubMed]
- Kim, S.T.; Jeong, G.E.; Kim, S.Y.; Choi, S.H.; Lim, G.C.; Han, J.H.; Nam, S.Y. The effect of voice therapy in vocal polyp patients. Phon. Speech Sci. 2009, 1, 43–49. (In Korean) [Google Scholar]
- Choi, J.I.; Yeo, J.O.; Jin, S.M.; Lee, S.H. Result of voice analysis after laryngeal microsurgery for vocal polyp in elderly. J. Korean Soc. Laryngol. Phoniatr. Logop. 2011, 22, 47–51. (In Korean) [Google Scholar]
- Petrović-Lazić, M.; Babac, S.; Vuković, M.; Kosanović, R.; Ivanković, Z. Acoustic voice analysis of patients with vocal fold polyp. J. Voice 2011, 25, 94–97. [Google Scholar] [CrossRef]
- Ju, Y.H.; Jung, K.Y.; Kwon, S.Y.; Woo, J.S.; Cho, J.G.; Park, M.W.; Park, E.H.; Baek, S.K. Effect of voice therapy after phonomicrosurgery for vocal polyps: A prospective, historically controlled, clinical study. J. Laryngol. Otol. 2013, 127, 1134–1138. [Google Scholar] [CrossRef]
- Schindler, A.; Mozzanica, F.; Maruzzi, P.; Atac, M.; De Cristofaro, V.; Ottaviani, F. Multidimensional assessment of vocal changes in benign vocal fold lesions after voice therapy. Auris Nasus Larynx 2013, 40, 291–297. [Google Scholar] [CrossRef]
- Choe, H.; Jung, K.Y.; Kwon, S.Y.; Woo, J.S.; Park, M.W.; Baek, S.K. The usefulness of CO2 laser-assisted phonomicrosurgery using a computer-guided scanner in broad-based vocal polyp. Korean J. Otorhinolaryngol.-Head. Neck Surg. 2013, 56, 511–515. (In Korean) [Google Scholar] [CrossRef]
- Wang, C.T.; Huang, T.W.; Liao, L.J.; Lo, W.C.; Lai, M.S.; Cheng, P.W. Office-based potassium titanyl phosphate laser-assisted endoscopic vocal polypectomy. JAMA Otolaryngol. Head. Neck Surg. 2013, 139, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Karasu, M.F.; Gundogdu, R.; Cagli, S.; Aydin, M.; Arli, T.; Aydemir, S.; Yuce, I. Comparison of effects on voice of diode laser and cold knife microlaryngology techniques for vocal fold polyps. J. Voice 2014, 28, 387–392. [Google Scholar] [CrossRef]
- Lin, L.; Sun, N.; Yang, Q.; Zhang, Y.; Shen, J.; Shi, L.; Fang, Q.; Sun, G. Effect of voice training in the voice rehabilitation of patients with vocal cord polyps after surgery. Exp. Ther. Med. 2014, 7, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.T.; Liao, L.J.; Huang, T.W.; Lo, W.C.; Cheng, P.W. Comparison of treatment outcomes of transnasal vocal fold polypectomy versus microlaryngoscopic surgery. Laryngoscope 2015, 125, 1155–1160. [Google Scholar] [CrossRef] [PubMed]
- Mizuta, M.; Hiwatashi, N.; Kobayashi, T.; Kaneko, M.; Tateya, I.; Hirano, S. Comparison of vocal outcomes after angiolytic laser surgery and microflap surgery for vocal polyps. Auris Nasus Larynx 2015, 42, 453–457. [Google Scholar] [CrossRef]
- Petrovic-Lazic, M.; Jovanovic, N.; Kulic, M.; Babac, S.; Jurisic, V. Acoustic and perceptual characteristics of the voice in patients with vocal polyps after surgery and voice therapy. J. Voice 2015, 29, 241–246. [Google Scholar] [CrossRef]
- Zhang, Y.; Liang, G.; Sun, N.; Guan, L.; Meng, Y.; Zhao, X.; Liu, L.; Sun, G. Comparison of CO2 laser and conventional laryngomicrosurgery treatments of polyp and leukoplakia of the vocal fold. Int. J. Clin. Exp. Med. 2015, 8, 18265–18274. [Google Scholar]
- Lee, Y.C.; Na, S.Y.; Kim, H.J.; Yang, C.W.; Kim, S.I.; Byun, Y.S.; Jung, A.R.; Ryu, I.Y.; Eun, Y.G. Effect of postoperative proton pump inhibitor therapy on voice outcomes following phonomicrosurgery for vocal fold polyp: A randomized controlled study. Clin. Otolaryngol. 2016, 41, 730–736. [Google Scholar] [CrossRef]
- Zhuge, P.; You, H.; Wang, H.; Zhang, Y.; Du, H. An Analysis of the effects of voice therapy on patients with early vocal fold polyps. J. Voice 2016, 30, 698–704. [Google Scholar] [CrossRef]
- Barillari, M.R.; Volpe, U.; Mirra, G.; Giugliano, F.; Barillari, U. Surgery or rehabilitation: A randomized clinical trial comparing the treatment of vocal fold polyps via phonosurgery and traditional voice therapy with “voice therapy expulsion” training. J. Voice 2017, 31, 379.e13–379.e20. [Google Scholar] [CrossRef] [PubMed]
- You, H.; Zhuge, P.; Wang, H.; Zhang, Y.; Du, H. Clinical observation of the effect of voice training on patients with vocal cordpolyps after phonomicrosurgery. Biomed. Res. 2017, 28, 3874–3879. [Google Scholar]
- Lin, Y.H.; Wang, C.T.; Lin, F.C.; Liao, L.J.; Lo, W.C.; Cheng, P.W. Treatment outcomes and adverse events following in-office angiolytic laser with or without concurrent polypectomy for vocal fold polyps. JAMA Otolaryngol. Head. Neck Surg. 2018, 144, 222–230. [Google Scholar] [CrossRef]
- Sahin, M.; Gode, S.; Dogan, M.; Kirazli, T.; Ogut, F. Effect of voice therapy on vocal fold polyp treatment. Eur. Arch. Otorhinolaryngol. 2018, 275, 1533–1540. [Google Scholar] [CrossRef]
- Oh, D.J.; Kim, S.Y.; Choi, I.H.; Han, H.M.; Byeon, H.K.; Jung, K.Y.; Baek, S.K. The usefulness of postoperative direct voice therapy in vocal polyps. Korean J. Otorhinolaryngol.-Head. Neck Surg. 2018, 61, 686–691. (In Korean) [Google Scholar] [CrossRef][Green Version]
- Wang, H.; Zhuge, P.; You, H.; Zhang, Y.; Zhang, Z. Comparison of the efficacy of vocal training and vocal microsurgery in patients with early vocal fold polyp. Braz. J. Otorhinolaryngol. 2019, 85, 678–684. [Google Scholar] [CrossRef]
- Prasad, S.; Raychowdhury, R.; Roychoudhury, A. Assessment of pre and postoperative voice quality in cases of vocal fold polyp. Inter. J. Otorhinolaryngol. Head. Neck Surg. 2020, 6, 352–358. [Google Scholar] [CrossRef]
- Kim, S.W.; Kim, S.Y.; Cho, J.K.; Jin, S.M.; Lee, S.H. Reliability of OperaVOXTM against multi-dimensional voice program to assess voice quality before and after laryngeal microsurgery in patient with vocal polyp. J. Korean Soc. Laryngol. Phoniatr. Logop. 2020, 31, 71–77. (In Korean) [Google Scholar] [CrossRef]
- Ma, J.; Fang, R.; Zhen, R.; Mao, W.; Wu, X.; He, P.; Wei, C. A 532-nm KTP laser for vocal fold polyps: Efficacy and relative factors. Ear Nose Throat J. 2021, 100, 87S–93S. [Google Scholar] [CrossRef]
- Lee, Y.; Park, H.J.; Bae, I.H.; Kwon, S.; Kim, G. The usefulness of multi voice evaluation for measuring voice recovery after endolaryngeal phonomicrosurgery in patients with vocal fold polyps. J. Voice 2021, in press. [Google Scholar] [CrossRef]
- Kang, D.W.; Kim, S.I.; Noh, J.K.; Jeong, S.J.; Lee, Y.C.; Ko, S.G.; Eun, Y.G. Voice outcome after cold knife surgery according to the characteristics of vocal fold polyp. J. Voice 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Barsties v. Latoszek, B.; Watts, C.R.; Neumann, K. The effectiveness of voice therapy on voice-related handicap: A network meta-analysis. Clin. Otolaryngol. 2020, 45, 796–804. [Google Scholar] [CrossRef] [PubMed]
- Barsties v. Latoszek, B.; Watts, C.R.; Schwan, K.; Hetjens, S. The maximum phonation time as marker for voice treatment efficacy: A network meta-analysis. Clin. Otolaryngol. 2023, 48, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.S.; Lee, D.H.; Jeong, G.E.; Kim, J.W.; Roh, J.L.; Choi, S.H.; Kim, S.Y.; Nam, S.Y. Treatment efficacy of voice therapy for vocal fold polyps and factors predictive of its efficacy. J. Voice 2017, 31, 120.e9–120.e13. [Google Scholar] [CrossRef]
- Gilbert, M.R.; Gartner-Schmidt, J.L.; Rosen, C.A. The VHI-10 and VHI item reduction translations-are we all speaking the same language? J. Voice 2017, 31, 250.e1–250.e7. [Google Scholar] [CrossRef]
- Björck, G.; Hertegård, S.; Ekelund, J.; Marsk, E. Voice rest after vocal fold polyp surgery: A Swedish register study of 588 patients. Laryngoscope Investig. Otolaryngol. 2022, 7, 486–493. [Google Scholar] [CrossRef]
- King, R.E.; Novaleski, C.K.; Rousseau, B. Voice Handicap Index changes after microflap surgery for benign vocal fold lesions are not associated with recommended absolute voice rest duration. Am. J. Speech Lang. Pathol. 2022, 31, 912–922. [Google Scholar] [CrossRef]
- Chi, H.W.; Cho, H.C.; Yang, A.Y.; Chen, Y.C.; Chen, J.W. Effects of different voice rest on vocal function after microlaryngeal surgery: A systematic review and meta-analysis. Laryngoscope 2023, 133, 154–161. [Google Scholar] [CrossRef]



| Study | Type and Features of VFP | N | Intervention Groups | Interventions with Durations Between Pre- and Post-Treatment | Duration of Voice Therapy in Weeks | Outcome Measures |
|---|---|---|---|---|---|---|
| Kim et al. (1999) [22] | All types and features of VFP | 58 | Phonosurgery | Treatment method: cold knife Duration: 2 months | n.a. | Jitter Shimmer NHR MPT |
| Kim & Auo (2008) [23] | All types and features of VFP | 62 | Phonosurgery | Treatment method: 585 nm pulsed dye laser (office-based) Duration: 2 months | n.a. | Jitter Shimmer NHR G, R, B |
| Kluch & Olszewski (2008) [24] | All types and features of VFP | 16 | Combination of phonosurgery and voice therapy | Treatment method: cold knife or CO2 laser using microlaryngoscopy under general anesthesia, and breathing and voice exercises Duration: > 1 month | 4 weeks | G, R, B |
| Kim et al. (2008) [25] | Unilateral; all sizes and features of VFP | 8 | Phonosurgery | Treatment method: cold knife Duration: 2–3 months | n.a. | VHI-T |
| Kluch & Olszewski (2009) [26] | All types and features of VFP | 25 | Combination of phonosurgery and voice therapy | Treatment method: cold knife or CO2 laser using microlaryngoscopy under general anesthesia, and breathing and voice exercises Duration: >1 month | 4 weeks | G, R, B |
| Kim et al. (2009) [27] | Small VFP | 33 | Voice therapy | Treatment method: Vocal hygiene and Seong-Tae Kim’s multiple voice therapy technique Duration: >1 month | 4 to 16 weeks | Jitter Shimmer NHR MPT |
| Choi et al. (2011) [28] | All types and features of VFP | 128 | Phonosurgery | Treatment method: cold knife Duration: >1 month | n.a. | Jitter Shimmer NHR MPT |
| Petrovic-Lazic et al. (2011) [29] | All types and features of VFP | 46 | Phonosurgery | Treatment method: cold knife Duration: 3 weeks | n.a. | Jitter Shimmer NHR |
| Ju et al. (2013) [30] | All types and features of VFP | 118 |
|
|
| Jitter Shimmer NHR MPT VHI-T, VHI-P, VHI-F, VHI-E G, R, B |
| Schindler et al. (2013) [31] | All types and features of gelatinous VFP | 20 | Voice therapy | Treatment method: vocal hygiene, abdominal breathing, resonant voice, yawn sigh approach, and manual therapy Duration: 1–2 months | 1 to 2 months | Jitter Shimmer NHR MPT VHI-T, VHI-P, VHI-F, VHI-E G, R, B |
| Choe et al. (2013) [32] | Unilateral; no giant VFP but other types and features | 41 | Combination of phonosurgery and voice therapy (two groups) | Treatment method: CO2 laser using microlaryngoscopy under general anesthesia or cold knife, vocal hygiene, and resonant voice Duration: 7 weeks | 4 weeks | Jitter Shimmer NHR MPT VHI-T, VHI-P, VHI-F, VHI-E |
| Wang et al. (2013) [33] | Unilateral; hemorrhagic small to medium vocal polyps | 36 | Phonosurgery (two groups) | Treatment method: KTP laser (office-based) or KTP plus cold knife using microlaryngoscopy under general anesthesia Duration: 6 weeks | n.a. | Jitter Shimmer NHR MPT |
| Karasu et al. (2014) [34] | All types and features of VFP | 51 | Phonosurgery (two groups) | Treatment method: diode laser using microlaryngoscopy under general anesthesia or cold knife Duration: 2 months | n.a. | Jitter Shimmer NHR VHI-T, VHI-P, VHI-F, VHI-E |
| Lin et al. (2014) [35] | Unilateral; all sizes and features of VFP | 60 |
|
|
| Jitter Shimmer NHR MPT VHI-T G, R, B |
| Wang et al. (2015) [36] | Small to medium sizes and all features of VFP | 34 | Phonosurgery (two groups) | Treatment method: KTP2 laser (office-based) or cold knife Duration: 6 weeks | n.a. | Jitter Shimmer NHR MPT |
| Mizuta et al. (2015) [37] | All types and features of VFP | 54 | Phonosurgery (two groups) | Treatment method: angiolytic laser (office-based) or cold knife Duration: 6 weeks | n.a. | Jitter Shimmer MPT |
| Petrovic-Lazic et al. (2015) [38] | Medium sizes and all features of VFP | 41 | Combination of phonosurgery and voice therapy | Treatment method: cold knife and voice therapy Duration: 6 weeks | 4 weeks | Jitter Shimmer NHR G, R, B |
| Zhang et al. (2015) [39] | Bilateral; all sizes and features of VFP | 60 | Phonosurgery (two groups) | Treatment method: CO2 laser using microlaryngoscopy under general anesthesia or cold knife Duration: 3 months | n.a. | Jitter Shimmer NHR MPT VHI-T G, R, B |
| Lee et al. (2016) [40] | Unilateral; all sizes and diffuse or pedunculated growths of VFP | 23 | Phonosurgery | Treatment method: cold knife Duration: 2 months | n.a. | Jitter Shimmer NHR MPT VHI-T |
| Zhuge et al. (2016) [41] | Small fusiform translucent bulge unilateral or bilateral VFP located at the junction of 1/3 of the front and the middle of the vocal fold | 66 | Voice therapy | Treatment method: relaxation training, breathing exercises, vocal function exercises, resonant voice, and vocal hygiene Duration: 3 months | 12 weeks | MPT VHI-T, VHI-P, VHI-F, VHI-E |
| Barillari et al. (2017) [42] | Unilateral; all sizes and features of the VFP at the free edge of the vocal fold | 140 |
|
|
| VHI-T G |
| You et al. (2017) [43] | VFP that were smooth and had translucent pedunculated neoplasm or fusiform translucent smooth neoplasm with a wider base by the free edge of the vocal folds | 96 |
|
|
| MPT VHI-T, VHI-P, VHI-F, VHI-E |
| Lin et al. (2018) [44] | All types and features of VFP | 90 | Phonosurgery (two groups) | Treatment method: KTP laser (office-based) or cold knife Duration: 1–2 months | n.a. | Jitter Shimmer NHR MPT |
| Sahin et al. (2018) [45] | All types and features of VFP | 165 |
|
|
| Jitter Shimmer NHR G, R, B |
| Oh et al. (2018) [46] | Unilateral; all sizes and features of VFP | 130 |
|
|
| Jitter Shimmer NHR MPT VHI-T, VHI-P, VHI-F, VHI-E G, R, B, |
| Wang et al. (2019) [47] | Small fusiform translucent bulge VFP’s located at the junction of 1/3 of the front and the middle of the vocal fold | 69 |
|
|
| MPT VHI-T, VHI-P, VHI-F, VHI-E |
| Prasad et al. (2020) [48] | All types and features of VFP | 40 | Phonosurgery | Treatment method: cold knife Duration: 3 months | n.a. | MPT |
| Kim et al. (2020) [49] | Unilateral; all sizes and features of VFP | 20 | Phonosurgery | Treatment method: cold knife Duration: 1 month | n.a. | Jitter Shimmer NHR |
| Ma et al. (2021) [50] | All types and features of VFP | 25 | Phonosurgery | Treatment method: KTP laser (office-based) Duration: 3–14 months | n.a. | Jitter Shimmer MPT VHI-T, VHI-P, VHI-F, VHI-E |
| Lee et al. (In Press) [51] | All types and features of VFP | 72 | Phonosurgery | Treatment method: cold knife Duration: 10–14 days | n.a. | VHI-T, VHI-P, VHI-F, VHI-E |
| Kang et al. (In Press) [52] | Unilateral; all sizes and features of VFP | 77 | Phonosurgery | Treatment method: cold knife Duration: 6 weeks | n.a. | Jitter Shimmer NHR MPT VHI-T, VHI-P, VHI-F, VHI-E G, R, B |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barsties v. Latoszek, B.; Watts, C.R.; Hetjens, S.; Neumann, K. The Efficacy of Different Voice Treatments for Vocal Fold Polyps: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 3451. https://doi.org/10.3390/jcm12103451
Barsties v. Latoszek B, Watts CR, Hetjens S, Neumann K. The Efficacy of Different Voice Treatments for Vocal Fold Polyps: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(10):3451. https://doi.org/10.3390/jcm12103451
Chicago/Turabian StyleBarsties v. Latoszek, Ben, Christopher R. Watts, Svetlana Hetjens, and Katrin Neumann. 2023. "The Efficacy of Different Voice Treatments for Vocal Fold Polyps: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 10: 3451. https://doi.org/10.3390/jcm12103451
APA StyleBarsties v. Latoszek, B., Watts, C. R., Hetjens, S., & Neumann, K. (2023). The Efficacy of Different Voice Treatments for Vocal Fold Polyps: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(10), 3451. https://doi.org/10.3390/jcm12103451







