Occurrence of Severe Arrhythmias in Patients with Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS): A Retrospective Study
Abstract
:1. Introduction
2. Materials and Methods
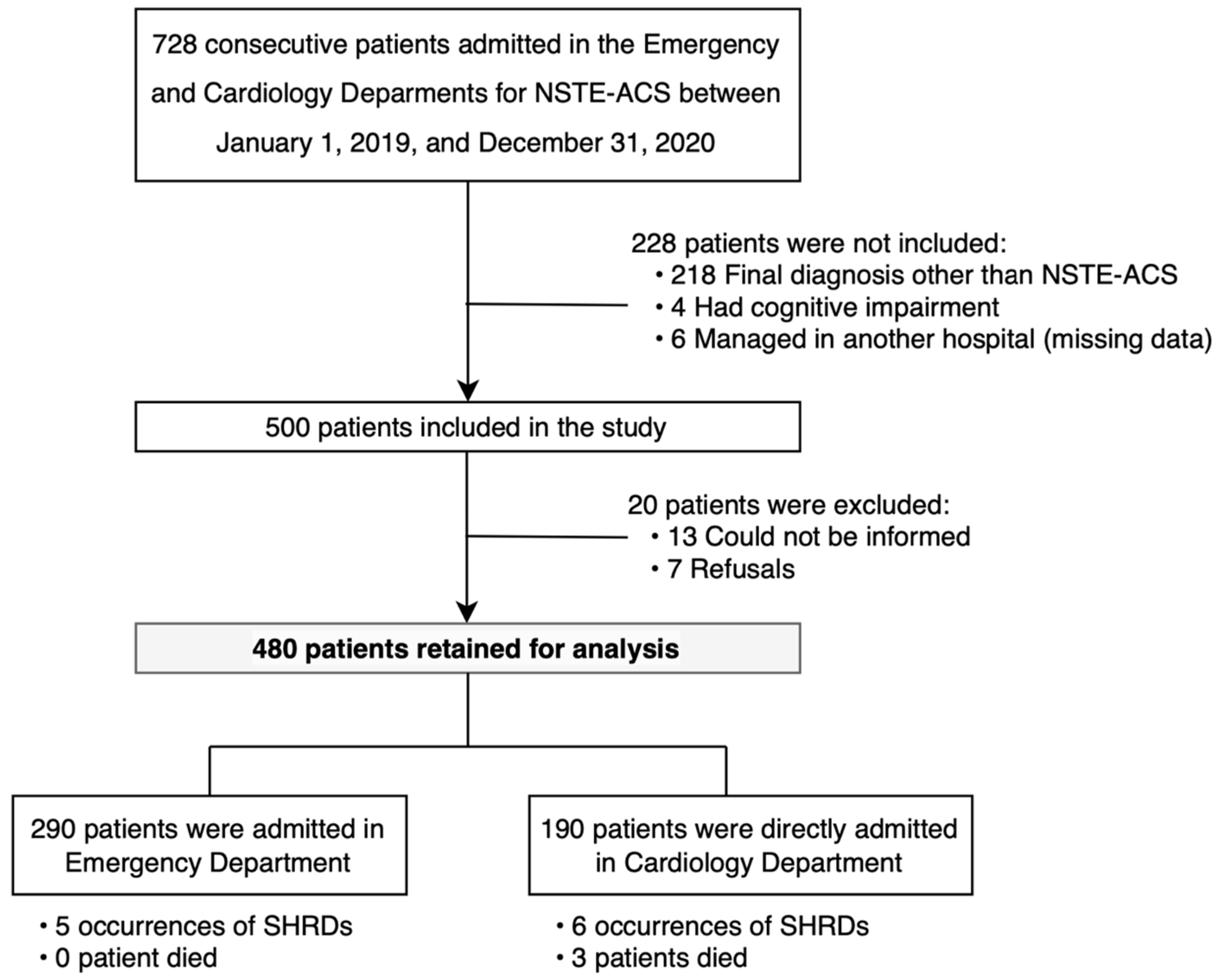
2.1. Study Design and Population
2.2. End-Point Definitions
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethics
3. Results
3.1. Baseline Characteristics of the Study Population
| Variable | Study Population | No SHRD | SHRD | p-Value | |
|---|---|---|---|---|---|
| n = 480 | n = 469 | n = 11 | |||
| Individual characteristics, median [IQR] | |||||
| Age, in years | 69.0 [59.0; 78.0] | 69.0 [59.0; 78.0] | 85.0 [71.5; 88.5] | 0.004 * | |
| BMI, kg/m2 | 26.46 [23.89; 30.45] | 26.5 [24.1; 30.5] | 23.9 [22.8; 30.2] | 0.361 | |
| Female, n (%) | 150 (31.2) | 144 (30.7) | 6 (54.5) | 0.175 | |
| Cardiovascular risk factors (CVRFs), n (%) | |||||
| Heredity | 102 (21.2) | 101 (21.5) | 1 (9.1) | 0.532 | |
| Smoking | 125 (26.0) | 124 (26.4) | 1 (9.1) | 0.343 | |
| High blood pressure | 329 (68.5) | 321 (68.4) | 8 (72.7) | 1.000 | |
| Diabetes mellitus | 175 (36.5) | 169 (36.0) | 6 (54.5) | 0.345 | |
| Dyslipidemia | 250 (52.1) | 244 (52.0) | 6 (54.5) | 1.000 | |
| Obesity | 122 (25.4) | 118 (25.2) | 4 (36.4) | 0.622 | |
| Number of CVRFs, median [IQR] | 2.0 [1.0; 3.0] | 2.0 [1.0; 3.0] | 2.0 [1.0; 3.5] | 0.872 | |
| Comorbidities, n (%) | |||||
| Ischemic heart disease | 231 (48.1) | 225 (48.0) | 6 (54.5) | 0.900 | |
| Ischemic stroke | 41 (8.5) | 40 (8.5) | 1 (9.1) | 1.000 | |
| Peripheral arterial disease | 67 (14.0) | 65 (13.9) | 2 (18.2) | 1.000 | |
| Renal failure | 81 (16.9) | 77 (16.4) | 4 (36.4) | 0.181 | |
| Heart failure | 23 (4.8) | 23 (4.9) | 0 (0.0) | 0.969 | |
| Supraventricular rhythm disorder | 65 (13.5) | 63 (13.4) | 2 (18.2) | 0.993 | |
| Long-term treatment, n (%) | |||||
| Anticoagulant | 67 (14.0) | 65 (13.9) | 2 (18.2) | 0.010 * | |
| Antiplatelet agent | 243 (50.6) | 237 (50.5) | 6 (54.5) | 1.000 | |
| ACE inhibitor | 134 (27.9) | 132 (28.1) | 2 (18.2) | 0.698 | |
| ARB | 116 (24.2) | 115 (24.5) | 1 (9.1) | 0.409 | |
| Beta-blocker | 237 (49.5) | 233 (49.8) | 4 (36.4) | 0.565 | |
| Statin | 215 (44.8) | 210 (44.8) | 5 (45.5) | 1.000 | |
3.2. In-Hospital Management
3.3. Primary End-Point
3.4. Multivariable Analysis
4. Discussion
4.1. Strengths and Limitations
4.2. Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- World Health Organization. Cardiovascular Diseases. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 19 November 2022).
- Pines, J.M.; Pollack, C.V.; Diercks, D.B.; Chang, A.M.; Shofer, F.S.; Hollander, J.E. The Association between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients with Chest Pain. Acad. Emerg. Med. 2009, 16, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef] [PubMed]
- McManus, D.D.; Gore, J.; Yarzebski, J.; Spencer, F.; Lessard, D.; Goldberg, R.J. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with STEMI and NSTEMI. Am. J. Med. 2011, 124, 40–47. [Google Scholar] [CrossRef]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E., Jr.; Ganiats, T.G.; Holmes, D.R., Jr.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. J. Am. Coll. Cardiol. 2014, 64, e139–e228. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef]
- Lenglet, A.; Balen, F.; Charpentier, S.; Sourbes, A.; Arcuset, D.; Delonglée, V.; Fort, P.; Bounes, V.; Dadone, B.C. Adverse events during inter-hospital transports of patients with Non ST-elevation acute coronary syndrome. Ann. Fr. Med. Urgence 2019, 9, 369–374. [Google Scholar] [CrossRef]
- Trebouet, E.; Boiffard, E.; Debierre, V.; Fradin, P. Study of complications occuring during inter-hospital transports of patients Non ST-elevation acute coronary syndrome. Ann. Cardiol. Angéiologie 2019, 68, 13–16. [Google Scholar] [CrossRef]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Ghuran, A.V.; Camm, A.J. Ischaemic heart disease presenting as arrhythmias. Br. Med. Bull. 2001, 59, 193–210. [Google Scholar] [CrossRef]
- Gupta, S.; Pressman, G.S.; Figueredo, V.M. Incidence of, predictors for, and mortality associated with malignant ventricular arrhythmias in non-ST elevation myocardial infarction patients. Coron. Artery Dis. 2010, 21, 460–465. [Google Scholar] [CrossRef]
- Serruys, P.; Onuma, Y.; Garg, S.; Sarno, G.; Brand, M.V.D.; Kappetein, A.-P.; Van Dyck, N.; Mack, M.; Holmes, D.; Feldman, T.; et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention 2009, 5, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Garg, S.; Sarno, G.; Garcia-Garcia, H.M.; Girasis, C.; Wykrzykowska, J.; Dawkins, K.D.; Serruys, P.W.; on behalf of the ARTS-II Investigators. A New Tool for the Risk Stratification of Patients With Complex Coronary Artery Disease: The Clinical SYNTAX Score. Circ. Cardiovasc. Interv. 2010, 3, 317–326. [Google Scholar] [CrossRef]
- Misumida, N.; Ogunbayo, G.O.; Kim, S.M.; Abdel-Latif, A.; Ziada, K.M.; Elayi, C.S. Frequency and Significance of High-Degree Atrioventricular Block and Sinoatrial Node Dysfunction in Patients with Non-ST-Elevation Myocardial Infarction. Am. J. Cardiol. 2018, 122, 1598–1603. [Google Scholar] [CrossRef]
- Pokorney, S.D.; Radder, C.; Schulte, P.J.; Al-Khatib, S.M.; Tricocci, P.; Van de Werf, F.; James, S.K.; Cannon, C.P.; Armstrong, P.W.; White, H.D.; et al. High-degree atrioventricular block, asystole, and electro-mechanical dissociation complicating non–ST-segment elevation myocardial infarction. Am. Heart J. 2016, 171, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.H.; Huang, Y.C. Comparison of STEMI and NSTEMI patients in the emergency department. J. Acute Med. 2011, 1, 1–4. [Google Scholar] [CrossRef]
- Tran, H.V.; Ash, A.S.; Gore, J.M.; Darling, C.E.; Kiefe, C.I.; Goldberg, R.J. Twenty-five year trends (1986–2011) in hospital incidence and case-fatality rates of ventricular tachycardia and ventricular fibrillation complicating acute myocardial infarction. Am. Heart J. 2019, 208, 1–10. [Google Scholar] [CrossRef]
- Toulouse, E.; Masseguin, C.; Lafont, B.; McGurk, G.; Harbonn, A.; Roberts, J.A.; Granier, S.; Dupeyron, A.; Bazin, J.E. French legal approach to clinical research. Anaesth. Crit. Care Pain Med. 2018, 37, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Piccini, J.P.; White, J.A.; Mehta, R.H.; Lokhnygina, Y.; Al-Khatib, S.M.; Tricoci, P.; Pollack, J.C.V.; Montalescot, G.; Van de Werf, F.; Gibson, C.M.; et al. Sustained Ventricular Tachycardia and Ventricular Fibrillation Complicating Non–ST-Segment–Elevation Acute Coronary Syndromes. Circulation 2012, 126, 41–49. [Google Scholar] [CrossRef]
- Alnsasra, H.; Ben-Avraham, B.; Gottlieb, S.; Ben-Avraham, M.; Kronowski, R.; Iakobishvili, Z.; Goldenberg, I.; Strasberg, B.; Haim, M. High-grade atrioventricular block in patients with acute myocardial infarction. Insights from a contemporary multi-center survey. J. Electrocardiol. 2018, 51, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Gach, O.; Davin, L.; Lempereur, M.; Marechal, P.; Martinez, C.; Lancellotti, P. Diagnostic coronarography. Rev. Med. Liege 2019, 74, S17–S21. Available online: https://orbi.uliege.be/bitstream/2268/239766/1/2019S1_04.pdf (accessed on 22 November 2022).
- Sauer, F.; Jesel, L.; Marchandot, B.; Derimay, F.; Bochaton, T.; Amaz, C.; Roubille, F.; Cayla, G.; Rioufol, G.; Garcia-Dorado, D.; et al. Life-threatening arrhythmias in anterior ST-segment elevation myocardial infarction patients treated by percutaneous coronary intervention: Adverse impact of morphine. Eur. Heart J. Acute Cardiovas. Care 2021, 10, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.V.; Gore, J.M.; Darling, C.E.; Ash, A.S.; Kiefe, C.I.; Goldberg, R.J. Hyperglycemia and risk of ventricular tachycardia among patients hospitalized with acute myocardial infarction. Cardiovasc. Diabetol. 2018, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Li, Z.; Xing, S.; Xu, Y. Effect of Admission Hyperglycemia on Short-Term Prognosis of Patients with Non-ST Elevation Acute Coronary Syndrome without Diabetes Mellitus. J. Diabetes Res. 2021, 2021, 1321289. [Google Scholar] [CrossRef] [PubMed]

| Variable | Study Population | No SHRD | SHRD | p-Value | |
|---|---|---|---|---|---|
| n = 480 | n = 469 | n = 11 | |||
| Initial admission in cardiology department, n (%) | 190 (39.6) | 184 (39.2) | 6 (54.5) | 0.475 | |
| Typical chest pain, n (%) | 266 (55.6) | 259 (55.5) | 7 (63.6) | 0.816 | |
| Vital signs at admission, median [IQR] | |||||
| Heart rate, in beats per min (bpm) | 77.0 [67.0; 89.0] | 77.0 [67.0; 89.0] | 80.0 [66.0; 91.5] | 0.813 | |
| Systolic BP, in mmHg | 144.0 [128.0; 160.0] | 144.0 [128.0; 160.0] | 136.0 [125.5; 150.0] | 0.295 | |
| Diastolic BP, in mmHg | 79.0 [70.0; 90.0] | 79.0 [70.0; 90.0] | 77.0 [68.0; 85.5] | 0.396 | |
| Pulse oximetry, in % | 97.0 [96.0; 98.0] | 97.0 [96.0; 98.0] | 98.0 [97.5; 98.5] | 0.110 | |
| Capillary blood glucose, in mmol/L | 1.19 [1.01; 1.58] | 6.54 [5.55.; 8.69] | 8.47 [7.09; 10.56] | 0.082 | |
| Temperature, in °C | 36.6 [36.2; 37.0] | 36.6 [36.2; 37.0] | 36.5 [36.2; 36.8] | 0.429 | |
| ECG upon admission | |||||
| Abnormal ECG, n (%) | 279 (58.1) | 273 (58.2) | 6 (54.5) | 1.000 | |
| ST segment depression, n (%) | 71 (14.8) | 69 (14.7) | 2 (18.2) | 1.000 | |
| Sum of the depression, median [IQR] | 5.0 [3.0; 6.0] | 4.5 [3.0; 6.0] | 8.5 [6.8; 10.3] | 0.160 | |
| Abnormal T waves, n (%) | 194 (40.7) | 189 (40.6) | 5 (45.5) | 0.987 | |
| QTc interval, median [IQR] in ms | 405.0 [380.0; 426.0] | 405.0 [380.0; 426.0] | 392.0 [374.5; 415.5] | 0.375 | |
| RT interval, median [IQR] in ms | 260.0 [240.0; 280.0] | 260.0 [240.0; 280.0] | 280.0 [250.0; 320.0] | 0.119 | |
| Biology upon admission, median [IQR] | |||||
| Troponin, in ng/L | 288.4 [37.1; 1562.6] | 276.0 [34.9; 1525.1] | 2096.1 [1180.2; 11,995.4] | 0.002 * | |
| BNP, in ng/L | 108.5 [40.0; 305.0] | 107.0 [39.0; 272.0] | 431.0 [270.0; 987.0] | 0.002 * | |
| CRP, in mg/L | 0.0 [0.0; 10.5] | 0.0 [0.0; 9.25] | 17.8 [5.4; 34.3] | 0.005 * | |
| Hemoglobin, in g/dL | 13.40 [12.0; 14.6] | 13.5 [12.1; 14.7] | 10.7 [10.5; 11.7] | 0.001 * | |
| Leukocytes, in G/L | 8.57 [7.03; 10.43] | 8.57 [7.03; 10.44] | 8.44 [7.26; 9.44] | 0.848 | |
| Platelets, in G/L | 240.5 [204.0; 293.0] | 240.0 [203.0; 292.0] | 267.0 [224.5; 348.5] | 0.078 | |
| Mean platelet volume, in fl | 10.4 [9.8; 11.0] | 10.4 [9.8; 11.0] | 10.9 [9.95; 11.2] | 0.352 | |
| Potassium, in mmol/L | 4.0 [3.8; 4.3] | 4.0 [3.8; 4.3] | 4.2 [3.9; 4.3] | 0.481 | |
| Creatinine, in µmol/L | 73.4 [61.8; 96.6] | 75.3 [61.7; 96.0] | 84.9 [72.2; 128.0] | 0.102 | |
| Urea, in mmol/L | 6.4 [5.0; 8.5] | 6.35 [5.0; 8.5] | 7.2 [6.5; 14.9] | 0.150 | |
| GFR (CKD-EPI), in mL/min/1.73m2 | 83.5 [61.0; 98.0] | 84.0 [62.0; 98.0] | 63.0 [39.0; 70.5] | 0.005 * | |
| LVEF, in %, median [IQR] | 57.0 [50.0; 64.0] | 58.0 [50.0; 64.0] | 47.0 [42.0; 56.0] | 0.028 * | |
| Initial management, n (%) | |||||
| Coronary angiography | 362 (75.4) | 354 (75.5) | 8 (72.7) | 1.000 | |
| Coronary angioplasty | 288 (60.0) | 280 (59.7) | 8 (72.7) | 0.575 | |
| SXS, median [IQR] | 7.0 [0.0; 14.0] | 7.0 [0.0; 14.0] | 13.0 [4.5; 19.0] | 0.160 | |
| CSS, median [IQR] | 8.1 [0.0; 22.5] | 8.0 [0.0; 22.2] | 33.0 [6.8; 41.7] | 0.066 | |
| Oxygen therapy | 74 (15.4) | 71 (15.1) | 3 (27.3) | 0.497 | |
| Analgesic | 97 (20.2) | 96 (20.5) | 1 (9.1) | 0.781 | |
| Early complications, n (%) | |||||
| STEMI | 1 (0.2) | 1 (0.2) | 0 (0.0) | 1.000 | |
| Cardiogenic shock | 4 (0.8) | 1 (0.2) | 3 (27.3) | <0.001 * | |
| Acute pulmonary oedema | 17 (3.5) | 16 (3.4) | 1 (9.1) | 0.855 | |
| Non-life-threatening rhythm disorder | 64 (13.3) | 62 (13.2) | 2 (18.1) | 0.229 | |
| Death | 3 (0.6) | 0 (0.0) | 3 (27.3) | <0.001 * | |
| Patient | Type of SHRD | Symptom | Persistent Chest Pain | Time of Occurrence in Relation to Coronary Angiography | Therapeutic Measure | Ionic Disorders | Death |
|---|---|---|---|---|---|---|---|
| N°1 | 2nd-degree AVB type Mobitz II (transient, 10 s) | No | No | Before coronary angiography, nocturnal occurrence | No | Yes, hypokalemia 2.8 mmol/L | No |
| N°2 | Ventricular tachycardia | No | No | Before coronary angiography | No | No | No |
| N°3 | 3rd-degree AVB | Faintness | No | Before coronary angiography | Non-invasive temporary cardiac pacing | No | No |
| N°4 | Ventricular tachycardia | CRA | No | Before coronary angiography | 1 EEC, amiodarone | No | No |
| N°5 | 3rd-degree AVB | No | No | Before coronary angiography, nocturnal occurrence | No | No | No |
| N°6 | EMD | CRA | Yes | In catheterization room, after angioplasty | CPR | Yes, hypocalcemia 1.52 mmol/L (with QTc = 519 ms) | Yes |
| N°7 | Ventricular fibrillation | CRA | No | In catheterization room, after angioplasty | 1 EEC | No | No |
| N°8 | EMD | CRA | No | In catheterization room, after angioplasty | CPR | No | Yes |
| N°9 | EMD | CRA | No | 5 h after coronary angioplasty | CPR | No | Yes |
| N°10 | Asystole (transient, <30 s) | Syncope | No | 9 h after coronary angioplasty | ECM, amiodarone | No | No |
| N°11 | 3rd-degree AVB | No | No | 15 h after coronary angioplasty, nocturnal occurrence | Isoprenaline | No | No |
| Variable | OR | CI95% | p-Value |
|---|---|---|---|
| Age a, in years | 1.69 | [0.96; 3.32] | 0.073 |
| LVEF a, in % | 0.86 | [0.52; 1.43] | 0.569 |
| Troponin > 37 ng/L | 4.87 | [0.53; 649.67] | 0.195 |
| BNP b, in ng/L | 0.98 | [0.88; 1.04] | 0.471 |
| CRP > 4 mg/L | 2.60 | [0.69; 11.73] | 0.159 |
| GFR < 60 mL/min/1.73m2 | 0.81 | [0.20; 3.01] | 0.749 |
| Hemoglobin > 12 g/dL | 0.12 | [0.02; 0.48] | 0.002 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilmé, V.; Harscoat, S.; Séverac, F.; Carmona, A.; Le Borgne, P.; Bilbault, P.; Morel, O.; Kepka, S. Occurrence of Severe Arrhythmias in Patients with Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS): A Retrospective Study. J. Clin. Med. 2023, 12, 3456. https://doi.org/10.3390/jcm12103456
Wilmé V, Harscoat S, Séverac F, Carmona A, Le Borgne P, Bilbault P, Morel O, Kepka S. Occurrence of Severe Arrhythmias in Patients with Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS): A Retrospective Study. Journal of Clinical Medicine. 2023; 12(10):3456. https://doi.org/10.3390/jcm12103456
Chicago/Turabian StyleWilmé, Valérie, Sébastien Harscoat, François Séverac, Adrien Carmona, Pierrick Le Borgne, Pascal Bilbault, Olivier Morel, and Sabrina Kepka. 2023. "Occurrence of Severe Arrhythmias in Patients with Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS): A Retrospective Study" Journal of Clinical Medicine 12, no. 10: 3456. https://doi.org/10.3390/jcm12103456
APA StyleWilmé, V., Harscoat, S., Séverac, F., Carmona, A., Le Borgne, P., Bilbault, P., Morel, O., & Kepka, S. (2023). Occurrence of Severe Arrhythmias in Patients with Non-ST Elevation Acute Coronary Syndrome (NSTE-ACS): A Retrospective Study. Journal of Clinical Medicine, 12(10), 3456. https://doi.org/10.3390/jcm12103456






