Sagittal and Vertical Changes of the Maxilla after Surgically Assisted Rapid Palatal Expansion: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Selection Criteria
2.2. Search Strategy
2.3. Data Extraction and Analysis
- SNA—the angle from sella to nasion to A point.
- Nvertical to A—the distance from a vertical line passing nasion to A point.
- NA–FH—the angle between nasion–A point and Frankfurt horizontal line.
- Cf–A—the distance from the facial center to A point.
- S–A—the distance from sella to A point.
- Co–A—the distance from condylion to A point.
- SN–PP—the angle between the sella-nasion and the palatal plane.
- FH–PP—the angle between the Frankfurt horizontal line and the palatal plane.
- N–ANS—the distance from nasion to the anterior nasal spine.
- FH–ANS—the distance from the Frankfurt horizontal line to the anterior nasal spine.
- ANS drop—the displacement of the anterior nasal spine on the vertical axis based on the cranial base superimposition.
- FH–PNS—the distance from Frankfurt horizontal line to the posterior nasal spine.
- PNS drop—the displacement of the posterior nasal spine on the vertical axis based on the cranial base superimposition.
- N–Cf–A—the angle from nasion to the facial center to A point.
- FH–A—the distance from the Frankfurt horizontal line to A point.
2.4. Risk of Bias/Quality Assessment
2.5. Statistical Analysis
3. Results
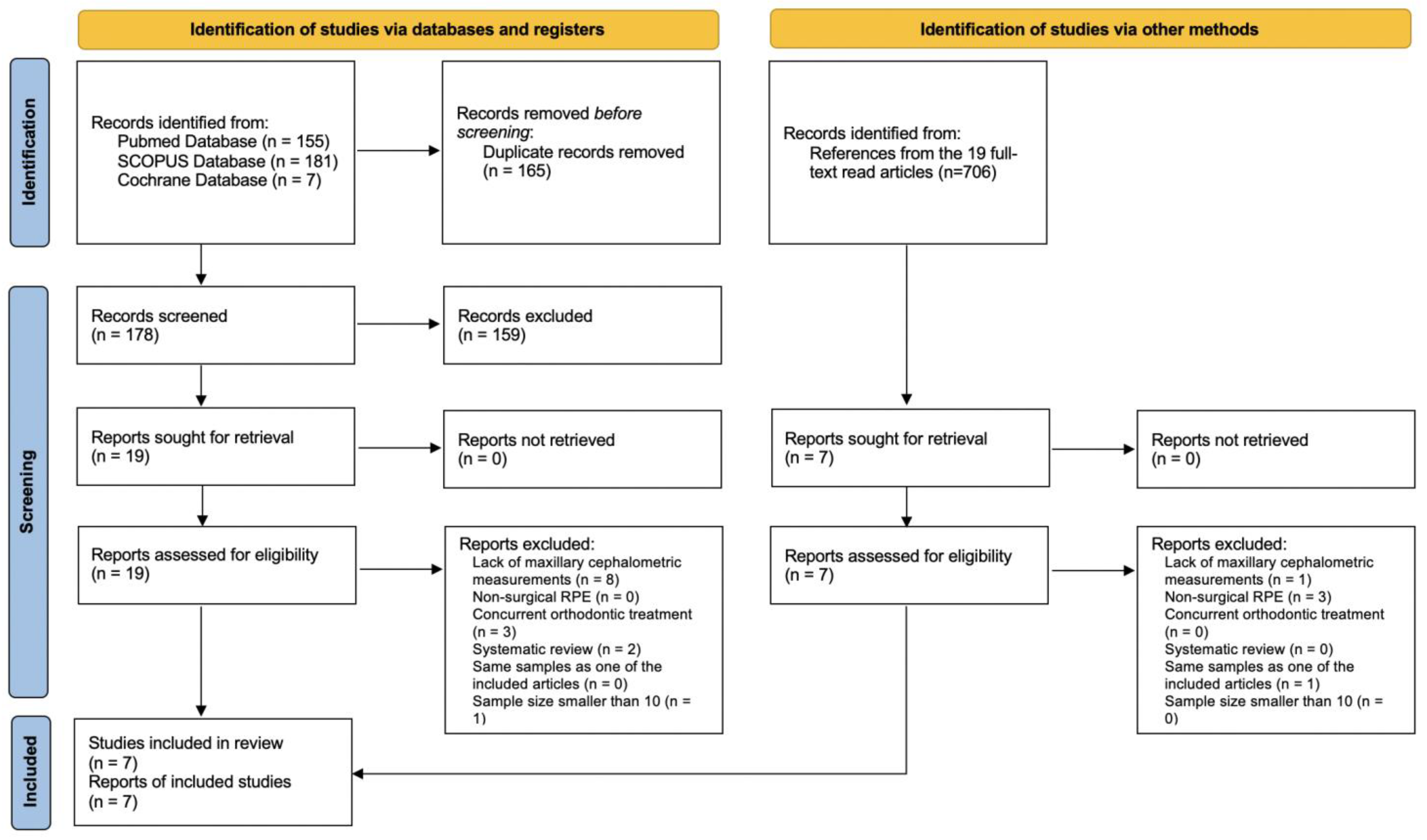
3.1. Literature Searching and Study Selections
3.2. Risk of Bias
3.3. Demographics
3.4. Maxillary Changes in the Sagittal Dimension
- (a)
- (b)
- (c)
- (d)
- Increase in Cf–A angle by Bretos et al. [14] (1.8°, p < 0.05).
| Parameters | References | Changes |
|---|---|---|
| SNA (°) | Chung et al. (2001) [9] | 0.60 ± 1.01 * |
| Bretos et al. (2007) [14] | Haas: 2.2 *; Hyrax: 1.3 | |
| Günbay et al. (2008) [15] | 1.00 ± 0.47 *** | |
| Kurt et al. (2010) [16] | 0.18 ± 0.36 | |
| Gungor et al. (2012) [17] & | 0.45 | |
| Iodice et al. (2013) [11] & | 0.6 | |
| Farfel et al. (2022) [18] & | Post expansion: −0.3 | |
| 4 months after expansion: −0.7 | ||
| 10 months after expansion: 0 | ||
| Nvertical to A (mm) | Chung et al. (2001) [9] | 0.55 ± 0.78 * |
| Bretos et al. (2007) [14] | Haas: 2.0 *; Hyrax: 0.9 | |
| Farfel et al. (2022) [18] & | Post expansion: −0.11 | |
| 4 months after expansion: −0.23 | ||
| 10 months after expansion: −0.24 | ||
| NA–FH (°) | Chung et al. (2001) [9] | 0.65 ± 0.76 * |
| Bretos et al. (2007) [14] | Haas: 2.2 *; Hyrax: 0.8 | |
| Iodice et al. (2013) [11] & | 0.3 | |
| Farfel et al. (2022) [18] & | Post expansion: −0.4 | |
| 4 months after expansion: −0.1 | ||
| 10 months after expansion: −0.3 | ||
| Cf–A (°) | Bretos et al. (2007) [14] | Haas: 1.5; Hyrax: 1.8 * |
| SN–ANS (°) | Iodice et al. (2013) [11] & | 0.6 |
| S–A (mm) | Farfel et al. (2022) [18] & | Post expansion: −0.6 |
| 4 months after expansion: −0.6 | ||
| 10 months after expansion: −0.3 | ||
| Co–A (mm) | Farfel et al. (2022) [18] & | Post expansion: 0.5 |
| 4 months after expansion: 0.9 | ||
| 10 months after expansion: 1.0 |
3.5. Maxillary Change in the Vertical Dimension
4. Discussion
4.1. Expander Type
4.2. Sagittal Change of the Maxilla
4.3. Vertical Change of the Maxilla
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AJ, H. Rapid expansion of the maxillary dental arch and nasal cavity by opening of the midpalatal suture. Angle Orthod. 1961, 31, 73–90. [Google Scholar]
- Rachmiel, A.; Turgeman, S.; Shilo, D.; Emodi, O.; Aizenbud, D. Surgically Assisted Rapid Palatal Expansion to Correct Maxillary Transverse Deficiency. Ann. Maxillofac. Surg. 2020, 10, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Koudstaal, M.J.; Smeets, J.B.; Kleinrensink, G.J.; Schulten, A.J.; van der Wal, K.G. Relapse and stability of surgically assisted rapid maxillary expansion: An anatomic biomechanical study. J. Oral. Maxillofac. Surg. 2009, 67, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Park, Y.C.; Park, J.Y.; Hwang, W.S. Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Mommaerts, M.Y. Transpalatal distraction as a method of maxillary expansion. Br. J. Oral. Maxillofac. Surg. 1999, 37, 268–272. [Google Scholar] [CrossRef]
- Betts, N.J.; Vanarsdall, R.L.; Barber, H.D.; Higgins-Barber, K.; Fonseca, R.J. Diagnosis and treatment of transverse maxillary deficiency. Int. J. Adult Orthodon. Orthognath. Surg. 1995, 10, 75–96. [Google Scholar]
- Suri, L.; Taneja, P. Surgically assisted rapid palatal expansion: A literature review. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 290–302. [Google Scholar] [CrossRef]
- Huizinga, M.P.; Meulstee, J.W.; Dijkstra, P.U.; Schepers, R.H.; Jansma, J. Bone-borne surgically assisted rapid maxillary expansion: A retrospective three-dimensional evaluation of the asymmetry in expansion. J. Craniomaxillofac. Surg. 2018, 46, 1329–1335. [Google Scholar] [CrossRef]
- Chung, C.H.; Woo, A.; Zagarinsky, J.; Vanarsdall, R.L.; Fonseca, R.J. Maxillary sagittal and vertical displacement induced by surgically assisted rapid palatal expansion. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 144–148. [Google Scholar] [CrossRef]
- Xi, T.; Laskowska, M.; van de Voort, N.; Ghaeminia, H.; Pawlak, W.; Bergé, S.; Maal, T. The effects of surgically assisted rapid maxillary expansion (SARME) on the dental show and chin projection. J. Craniomaxillofac. Surg. 2017, 45, 1835–1841. [Google Scholar] [CrossRef]
- Iodice, G.; Bocchino, T.; Casadei, M.; Baldi, D.; Robiony, M. Evaluations of sagittal and vertical changes induced by surgically assisted rapid palatal expansion. J. Craniofac. Surg. 2013, 24, 1210–1214. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Rev. Esp. Cardiol. (Engl. Ed.) 2021, 74, 790–799. [Google Scholar] [CrossRef]
- Muñoz-Pereira, M.E.; Haas-Junior, O.L.; Da Silva Meirelles, L.; Machado-Fernández, A.; Guijarro-Martínez, R.; Hernández-Alfaro, F.; de Oliveira, R.B.; Pagnoncelli, R.M. Stability and surgical complications of tooth-borne and bone-borne appliances in surgical assisted rapid maxillary expansion: A systematic review. Br. J. Oral. Maxillofac. Surg. 2021, 59, e29–e47. [Google Scholar] [CrossRef]
- Bretos, J.L.; Pereira, M.D.; Gomes, H.C.; Toyama Hino, C.; Ferreira, L.M. Sagittal and vertical maxillary effects after surgically assisted rapid maxillary expansion (SARME) using Haas and Hyrax expanders. J. Craniofac. Surg. 2007, 18, 1322–1326. [Google Scholar] [CrossRef]
- Günbay, T.; Akay, M.C.; Günbay, S.; Aras, A.; Koyuncu, B.O.; Sezer, B. Transpalatal distraction using bone-borne distractor: Clinical observations and dental and skeletal changes. J. Oral. Maxillofac. Surg. 2008, 66, 2503–2514. [Google Scholar] [CrossRef]
- Kurt, G.; Altug-Ataç, A.T.; Ataç, M.S.; Karasu, H.A. Stability of surgically assisted rapid maxillary expansion and orthopedic maxillary expansion after 3 years’ follow-up. Angle Orthod. 2010, 80, 425–431. [Google Scholar] [CrossRef]
- Gungor, A.Y.; Türkkahraman, H.; Baykul, T.; Alkis, H. Comparison of the effects of rapid maxillary expansion and surgically assisted rapid maxillary expansion in the sagittal, vertical, and transverse planes. Med. Oral. Patol. Oral. Cir. Bucal. 2012, 17, e311–e319. [Google Scholar] [CrossRef]
- Farfel, V.; Morea, G.C.; Ferreira, L.M.; Pereira, M.D. Evaluation of Sagittal and Vertical Changes in Maxillary Dental, Skeletal, and Soft Tissue following Surgically Assisted Rapid Maxillary Expansion: A Retrospective Longitudinal Study. J. Craniofac. Surg. 2022, 33, e398–e401. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010, 1, 97–111. [Google Scholar] [CrossRef]
- Zemann, W.; Schanbacher, M.; Feichtinger, M.; Linecker, A.; Kärcher, H. Dentoalveolar changes after surgically assisted maxillary expansion: A three-dimensional evaluation. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2009, 107, 36–42. [Google Scholar] [CrossRef]
- Zandi, M.; Miresmaeili, A.; Heidari, A. Short-term skeletal and dental changes following bone-borne versus tooth-borne surgically assisted rapid maxillary expansion: A randomized clinical trial study. J. Craniomaxillofac. Surg. 2014, 42, 1190–1195. [Google Scholar] [CrossRef]
- Trefný, P.; Krajíček, V.; Velemínská, J. Three-dimensional analysis of palatal shape in patients treated with SARME using traditional and geometric morphometrics. Orthod. Craniofac. Res. 2016, 19, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, T.F.M.; Pereira-Filho, V.A.; Gabrielli, M.F.R.; Gonçales, E.S.; Santos-Pinto, A. Effects of surgically assisted rapid maxillary expansion on mandibular position: A three-dimensional study. Prog. Orthod. 2017, 18, 22. [Google Scholar] [CrossRef] [PubMed]
- Kober, C.; Kannenberg, S.; Frank, B.; Al-Hakim, G.; Parvin, A.; Landes, C.; Sader, R. Computer-assisted pre- and postoperative evaluation of surgically assisted rapid maxillary expansion. Int. J. Comput. Dent. 2011, 14, 233–241. [Google Scholar] [PubMed]
- Byloff, F.K.; Mossaz, C.F. Skeletal and dental changes following surgically assisted rapid palatal expansion. Eur. J. Orthod. 2004, 26, 403–409. [Google Scholar] [CrossRef]
- Goldenberg, D.C.; Alonso, N.; Goldenberg, F.C.; Gebrin, E.S.; Amaral, T.S.; Scanavini, M.A.; Ferreira, M.C. Using computed tomography to evaluate maxillary changes after surgically assisted rapid palatal expansion. J. Craniofac. Surg. 2007, 18, 302–311. [Google Scholar] [CrossRef]
- Chung, C.H.; Font, B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 569–575. [Google Scholar] [CrossRef]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Sagittal and vertical effects of rapid maxillary expansion in Class I, II, and III occlusions. Angle Orthod. 2011, 81, 298–303. [Google Scholar] [CrossRef]
- Altındiş, S.; Toy, E.; Başçiftçi, F.A. Effects of different rapid maxillary expansion appliances on facial soft tissues using three-dimensional imaging. Angle Orthod. 2016, 86, 590–598. [Google Scholar] [CrossRef]
- Koudstaal, M.J.; Wolvius, E.B.; Schulten, A.J.; Hop, W.C.; van der Wal, K.G. Stability, tipping and relapse of bone-borne versus tooth-borne surgically assisted rapid maxillary expansion; a prospective randomized patient trial. Int. J. Oral. Maxillofac. Surg. 2009, 38, 308–315. [Google Scholar] [CrossRef]
- Parhiz, A.; Schepers, S.; Lambrichts, I.; Vrielinck, L.; Sun, Y.; Politis, C. Lateral cephalometry changes after SARPE. Int. J. Oral. Maxillofac. Surg. 2011, 40, 662–671. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Major, P.W.; Flores-Mir, C. Dental and skeletal changes following surgically assisted rapid maxillary expansion. Int. J. Oral Maxillofac. Surg. 2006, 35, 481–487. [Google Scholar] [CrossRef]
- Hamedi Sangsari, A.; Sadr-Eshkevari, P.; Al-Dam, A.; Friedrich, R.E.; Freymiller, E.; Rashad, A. Surgically Assisted Rapid Palatomaxillary Expansion with or without Pterygomaxillary Disjunction: A Systematic Review and Meta-Analysis. J. Oral. Maxillofac. Surg. 2016, 74, 338–348. [Google Scholar] [CrossRef]
- Altug Atac, A.T.; Karasu, H.A.; Aytac, D. Surgically assisted rapid maxillary expansion compared with orthopedic rapid maxillary expansion. Angle Orthod. 2006, 76, 353–359. [Google Scholar]
- Romano, F.L.; Mestriner, M.A. Skeletal posterior crossbite in patient with mandibular asymmetry: An alternative solution. Dental. Press J. Orthod. 2021, 26, e21bbo23. [Google Scholar] [CrossRef]
- Chamberland, S.; Proffit, W.R. Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 815–822.e811. [Google Scholar] [CrossRef]
- Hardin, A.M.; Knigge, R.P.; Oh, H.S.; Valiathan, M.; Duren, D.L.; McNulty, K.P.; Middleton, K.M.; Sherwood, R.J. Estimating Craniofacial Growth Cessation: Comparison of Asymptote- and Rate-Based Methods. Cleft. Palate Craniofac. J. 2022, 59, 230–238. [Google Scholar] [CrossRef]



| Criteria | Description |
|---|---|
| Population | Patients with transverse maxillary deficiency and without craniofacial anomaly |
| Intervention | Two-piece SARPE |
| Comparisons | Pre- and post-SARPE cephalometric measurements |
| Outcome | Maxillary position change in the vertical and sagittal dimensions |
| Chung et al. (2001) [9] | Bretos et al. (2007) [14] | Günbay et al. (2008) [15] | Kurt et al. (2010) [16] | Gungor et al. (2012) [17] | Iodice et al. (2013) [11] | Farfel et al. (2022) [18] | |
|---|---|---|---|---|---|---|---|
| Sample randomization | No | No | No | No | No | No | No |
| Comparison between treatments | No | Yes | No | Yes | Yes | No | No |
| Blind assessments | No | No | No | No | No | No | Yes |
| Validation of measurements | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Statistical analysis | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Defined inclusion and exclusion criteria | No | No | Yes | Yes | Yes | Yes | Yes |
| Report of follow-up | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Risk of bias | High | High | High | Medium | Medium | High | Medium |
| Author | Number | Age (y) | Method | Device | Expansion during Surgery (mm) | Expander Activation Protocol after Surgery |
|---|---|---|---|---|---|---|
| Chung et al. (2001) [9] | 20 (6 M, 14 F) | 25.6 (14.9–43.0) | Retrospective Case Series | T.B. | 1–1.5 | 0.5 mm/day for about 2 weeks until the jackscrew was fully opened. |
| Bretos et al. (2007) [14] | 33 (14 M, 19 F) | 25 (18–40) | Retrospective Cohort Study | T.B. Haas (16) | 1.6 | 0.4 mm/day started 4 days post-Sx until planned expansion was reached. |
| T.B. Hyrax (17) | ||||||
| Günbay et al. (2008) [15] | 10 (6 M, 4F) | 22.3 | Retrospective Case Series | B.B. | - | 1 mm/day started 7 days post-Sx until appropriate posterior overbite was achieved. |
| Kurt et al. (2010) [16] | 10 (7 M, 3 F) | 19.01 (16.25–25.58) | Retrospective Cohort Study | T.B. | - | 0.5 mm/day until desired expansion was reached. |
| Gungor et al. (2012) [17] | 14 (4 M, 10 F) | 19.6 ± 2.73 | Retrospective Cohort Study | T.B. | 1 | 0.5 mm/day started 7 days post-Sx until the necessary amount was achieved. |
| Iodice et al. (2013) [11] | 21 (7 M, 14 F) | 25.6 ± 6.3 (20.2–30.1) | Retrospective Case Series | T.B. | 1.6 | 0.4 mm/day started 4 days post-Sx until planned expansion was reached. |
| Farfel et al. (2022) [18] | 28 (14 M, 14 F) | 25.8 (19–39) | Retrospective Case Series | T.B. | 1.6 | 0.4 mm/day started 4 days post-Sx until desired expansion was reached. |
| Parameters | References | Changes |
|---|---|---|
| SN–PP (°) | Chung et al. (2001) [9] | 0.23 ± 1.26 |
| Kurt et al. (2010) [16] | 0.65 ± 0.33 | |
| Iodice et al. (2013) [11] & | 0.4 | |
| Farfel et al. (2022) [18] & | Post expansion: −0.07 | |
| 4 months after expansion: −0.07 | ||
| 10 months after expansion: 0.3 | ||
| FH–PP (°) | Iodice et al. (2013) [11] & | 1.0 |
| N–ANS (mm) | Kurt et al. (2010) [16] | 1.21 ± 0.28 ** |
| Gungor et al. (2012) [17] & | −0.11 | |
| FH–ANS (mm) | Bretos et al. (2007) [14] | Haas: 0.3; Hyrax: 0 |
| Farfel et al. (2022) [18] & | Post expansion: −0.1 | |
| 4 months after expansion: −0.4 | ||
| 10 months after expansion: −0.1 | ||
| ANS drop (mm) | Chung et al. (2001) [9] | 0.45 ± 1.10 |
| FH–PNS (mm) | Bretos et al. (2007) [14] | Haas: 0.1; Hyrax: −0.3 |
| Farfel et al. (2022) [18] # | Post-expansion: 1.37 ± 0.10 | |
| 4 months after expansion: 1.22 ± 0.12 | ||
| 10 months after expansion: 0.51 ± 0.09 | ||
| PNS drop (mm) | Chung et al. (2001) [9] | 0.60 ± 0.90 |
| N–Cf–A (°) | Bretos et al. (2007) [14] | Haas: −0.9; Hyrax: −0.5 |
| FH–A (mm) | Farfel et al. (2022) [18] & | Post expansion: −0.1 |
| 4 months after expansion: −0.7 | ||
| 10 months after expansion: −0.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, J.-H.; Wang, S.; Abdullah, U.A.; Le, A.D.; Chung, C.-H.; Li, C. Sagittal and Vertical Changes of the Maxilla after Surgically Assisted Rapid Palatal Expansion: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 3488. https://doi.org/10.3390/jcm12103488
Lin J-H, Wang S, Abdullah UA, Le AD, Chung C-H, Li C. Sagittal and Vertical Changes of the Maxilla after Surgically Assisted Rapid Palatal Expansion: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(10):3488. https://doi.org/10.3390/jcm12103488
Chicago/Turabian StyleLin, Jia-Hong, Steven Wang, Usama Al Abdullah, Anh D. Le, Chun-Hsi Chung, and Chenshuang Li. 2023. "Sagittal and Vertical Changes of the Maxilla after Surgically Assisted Rapid Palatal Expansion: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 10: 3488. https://doi.org/10.3390/jcm12103488





