Radiographic Analysis in Extra-Articular and Intra-Articular Distal Radius Fractures Treated with Variable-Angle Volar Locking Plate Fixation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design and Planning
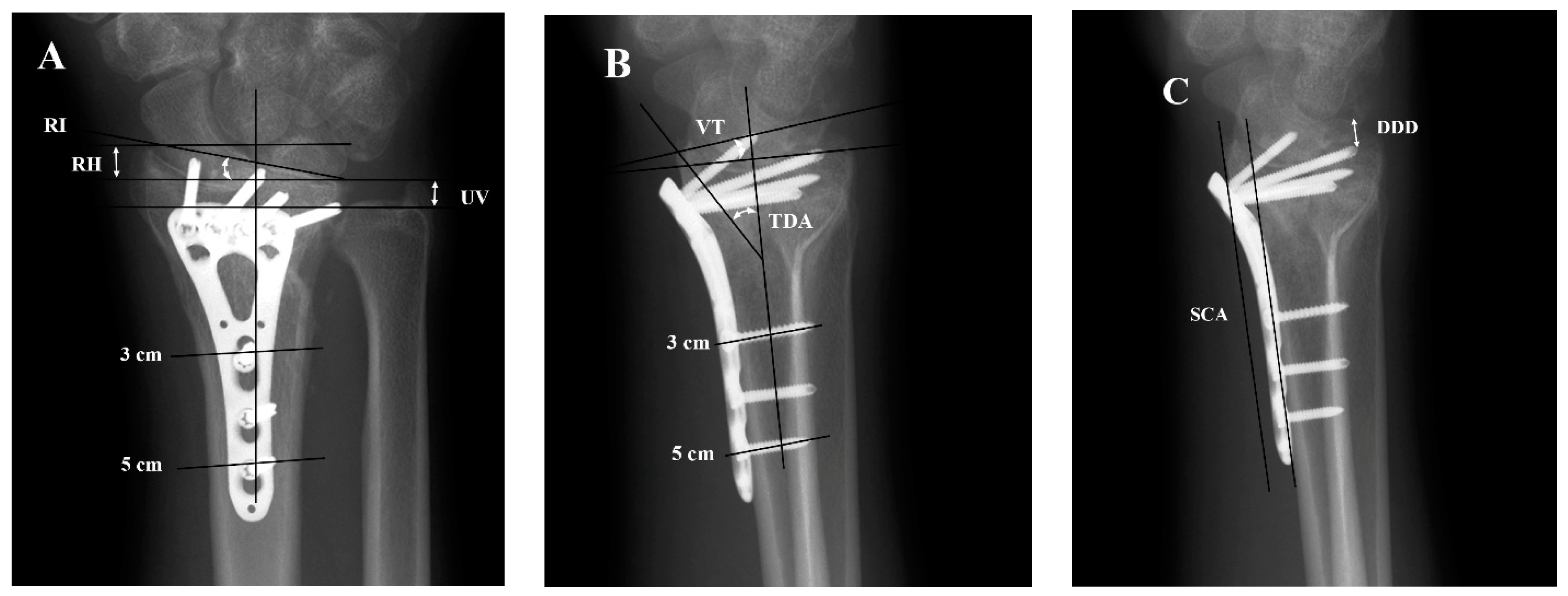
2.2. Analysis of Forearm X-ray Images
2.3. Statistical Analysis
- Paired t-tests and Wilcoxon signed-rank tests were used to compare radial height (RH), ulnar variance (UV), radial inclination (RI), volar tilt (VT), teardrop angle (TDA), and distal dorsal cortical distance (DDD) immediately after the operation and 3 months following the operation within each of the two groups.
- Student’s t-tests were used to compare RH, UV, RI, VT, TDA, and DDD immediately after the operation with 3-months follow-up in the extra-articular and intra-articular groups, as well as to compare the 3-month change in RH, UV, RI, VT, TDA, and DDD between these two groups.
- The Soong classification gradings were divided into low-risk (Grade 0) and high-risk (Grade 1 and Grade 2) groups to analyze the relationship between the risk of flexion tendon rupture and types of fracture using the likelihood Chi-square test and Fisher’s exact test.
- Linear regression was used to analyze the DDD estimated immediately after the operation and the change at 3-months follow-up in both the extra-articular and intra-articular groups, as well as in all patients in both groups.
3. Results
3.1. Characteristics in Study Subject
3.2. Radiographic Parameters of Immediately Post-Operation and 3 Months following Operation in Extra-Articular Group and Intra-Articular Group
3.3. Comparison of Risk of Tendon Rupture by Soong Classification at Two Timings and Change of Tendon Rupture Risk in 3 Months between Extra-Articular Group and Intra-Articular Group
3.4. Linear Regression of DDD of Immediately Post-Operation and Changes in 3 Months following the Operation in the Extra-Articular Group, Intra-Articular Group and All- Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jerrhag, D.; Englund, M.; Karlsson, M.K.; Rosengren, B.E. Epidemiology and Time Trends of Distal Forearm Fractures in Adults—A Study of 11.2 Million Person-Years in Sweden. BMC Musculoskelet. Disord. 2017, 18, 240. [Google Scholar] [CrossRef] [PubMed]
- Mellstrand-Navarro, C.; Pettersson, H.J.; Tornqvist, H.; Ponzer, S. The Operative Treatment of Fractures of the Distal Radius Is Increasing: Results from a Nationwide Swedish Study. Bone Jt. J. 2014, 96-b, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Hevonkorpi, T.P.; Launonen, A.P.; Huttunen, T.T.; Kannus, P.; Niemi, S.; Mattila, V.M. Incidence of Distal Radius Fracture Surgery in Finns Aged 50 Years or More between 1998 and 2016—Too Many Patients Are yet Operated On? BMC Musculoskelet. Disord. 2018, 19, 70. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Schroeder, M.; Kossow, K.; Gruber-Rathmann, M.; Ruecker, A.H. Radiological Dorsal Tilt Analysis of Ao Type a, B, and C Fractures of the Distal Radius Treated Conservatively or with Extra-Focal K-Wire Plus External Fixateur. Skelet. Radiol. 2012, 41, 1133–1139. [Google Scholar] [CrossRef]
- Smith, D.W.; Henry, M.H. Volar Fixed-Angle Plating of the Distal Radius. J. Am. Acad. Orthop. Surg. 2005, 13, 28–36. [Google Scholar] [CrossRef]
- Khatri, K.; Sharma, V.; Farooque, K.; Tiwari, V. Surgical Treatment of Unstable Distal Radius Fractures with a Volar Variable-Angle Locking Plate: Clinical and Radiological Outcomes. Arch. Trauma Res. 2016, 5, e25174. [Google Scholar] [CrossRef] [PubMed]
- Mehrzad, R.; Kim, D.C. Complication Rate Comparing Variable, Angle Distal Locking Plate to Fixed Angle Plate Fixation of Distal Radius Fractures. Ann. Plast. Surg. 2016, 77, 623–625. [Google Scholar] [CrossRef]
- Stanbury, S.J.; Salo, A.; Elfar, J.C. Biomechanical Analysis of a Volar Variable-Angle Locking Plate: The Effect of Capturing a Distal Radial Styloid Fragment. J. Hand Surg. Am. 2012, 37, 2488–2494. [Google Scholar] [CrossRef]
- Hart, A.; Collins, M.; Chhatwal, D.; Steffen, T.; Harvey, E.J.; Martineau, P.A. Can the Use of Variable-Angle Volar Locking Plates Compensate for Suboptimal Plate Positioning in Unstable Distal Radius Fractures? A Biomechanical Study. J. Orthop. Trauma 2015, 29, e1–e6. [Google Scholar] [CrossRef]
- Erhart, S.; Toth, S.; Kaiser, P.; Kastenberger, T.; Deml, C.; Arora, R. Comparison of Volarly and Dorsally Displaced Distal Radius Fracture Treated by Volar Locking Plate Fixation. Arch. Orthop. Trauma Surg. 2018, 138, 879–885. [Google Scholar] [CrossRef]
- Andersen, D.J.; Blair, W.F.; Steyers, C.M., Jr.; Adams, B.D.; el-Khouri, G.Y.; Brandser, E.A. Classification of Distal Radius Fractures: An Analysis of Interobserver Reliability and Intraobserver Reproducibility. J. Hand Surg. Am. 1996, 21, 574–582. [Google Scholar] [CrossRef] [PubMed]
- Bozentka, D.J.; Beredjiklian, P.K.; Westawski, D.; Steinberg, D.R. Digital Radiographs in the Assessment of Distal Radius Fracture Parameters. Clin. Orthop. Relat. Res. 2002, 397, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.Q.Y.; Chiow, S.M.; Lai, S.H.S.; Chia, D.S.Y. The Effect of Hand Dominance, Age, Gender, Fracture Comminution and Asa Status on Time to Fracture Healing Following Surgical Fixation of Distal Radius Fractures. J. Hand Surg. Asian Pac. Vol. 2022, 27, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Kreder, H.J.; Hanel, D.P.; McKee, M.; Jupiter, J.; McGillivary, G.; Swiontkowski, M.F. X-ray Film Measurements for Healed Distal Radius Fractures. J. Hand Surg. Am. 1996, 21, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Thuysbaert, G.; Ringburg, A.; Petronilia, S.; Vanden Berghe, A.; Hollevoet, N. Measurement of Ulnar Variance and Radial Inclination on X-Rays of Healed Distal Radius Fractures. With the Axis of the Distal Radius or Ulna? Acta Orthop Belg. 2015, 81, 308–314. [Google Scholar]
- Medoff, R.J. Essential Radiographic Evaluation for Distal Radius Fractures. Hand Clin. 2005, 21, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Fujitani, R.; Omokawa, S.; Iida, A.; Santo, S.; Tanaka, Y. Reliability and Clinical Importance of Teardrop Angle Measurement in Intra-Articular Distal Radius Fracture. J. Hand Surg. Am. 2012, 37, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Vosbikian, M.M.; Ketonis, C.; Huang, R.; Ilyas, A.M. Optimal Positioning for Volar Plate Fixation of a Distal Radius Fracture: Determining the Distal Dorsal Cortical Distance. Orthop. Clin. North. Am. 2016, 47, 235–244. [Google Scholar] [CrossRef]
- Soong, M.; Earp, B.E.; Bishop, G.; Leung, A.; Blazar, P. Volar Locking Plate Implant Prominence and Flexor Tendon Rupture. J. Bone Jt. Surg. Am. 2011, 93, 328–335. [Google Scholar] [CrossRef]
- Elerian, S.; Singh, T.; Jagodzinsk, N.A.; Norris, R.; Tan, S.; Power, D.; Jones, J.; Chen, Z.; Eltagy, H. Early Results of a Variable-Angle Volar Locking Plate for Distal Radius Fractures: A Bi-Centre Study. Cureus 2021, 13, e18321. [Google Scholar] [CrossRef]
- Fang, P.C.; Lo, T.Y.Y.; Cheng, C.Y.; Chou, Y.C.; Chen, A.C.Y. Radiographic Analysis in Reduction Loss and Parameters Maintenance after Distal Radius Fracture Fixation with Variable-Angle Volar Locking Plate. Formos. J. Musculoskelet. Disorders. 2021, 12, 43–50. [Google Scholar] [CrossRef]
- Gogna, P.; Selhi, H.S.; Singla, R.; Devgan, A.; Magu, N.K.; Mahindra, P.; Yamin, M. Dorsally Comminuted Fractures of the Distal End of the Radius: Osteosynthesis with Volar Fixed Angle Locking Plates. ISRN Orthop. 2013, 2013, 131757. [Google Scholar] [CrossRef] [PubMed]
- Forward, D.; Davis, T. The Teardrop Angle and Ap Distance in Fractures of the Distal Radius. Orthop. Proc. 2011, 93-B, 6. [Google Scholar] [CrossRef]
- Snoddy, M.C.; An, T.J.; Hooe, B.S.; Kay, H.F.; Lee, D.H.; Pappas, N.D. Incidence and Reasons for Hardware Removal Following Operative Fixation of Distal Radius Fractures. J. Hand Surg. Am. 2015, 40, 505–507. [Google Scholar] [CrossRef] [PubMed]
- Gören, Y.; Sauerbier, M.; Arsalan-Werner, A. Impact of Soong Grading on Flexor Tendon Ruptures Following Palmar Plating for Distal Radial Fractures. J. Hand Surg. Eur. Vol. 2020, 45, 348–353. [Google Scholar] [CrossRef]
- Selles, C.A.; Reerds, S.T.H.; Roukema, G.; van der Vlies, K.H.; Cleffken, B.I.; Schep, N.W.L. Relationship between Plate Removal and Soong Grading Following Surgery for Fractured Distal Radius. J. Hand Surg. Eur. Vol. 2018, 43, 137–141. [Google Scholar] [CrossRef]
- Yamak, K.; Karahan, H.G.; Karatan, B.; Kayalı, C.; Altay, T. Evaluation of Flexor Pollicis Longus Tendon Rupture after Treatment of Distal Radius Fracture with the Volar Plate. J. Wrist Surg. 2020, 9, 219–224. [Google Scholar] [CrossRef]
- Lee, S.K.; Chun, Y.S.; Shin, H.M.; Kim, S.M.; Choy, W.S. Double-Tiered Subchondral Support Fixation with Optimal Distal Dorsal Cortical Distance Using a Variable-Angle Volar Locking-Plate System for Distal Radius Fracture in the Elderly. Orthop. Traumatol. Surg. Res. 2018, 104, 883–891. [Google Scholar] [CrossRef]

| Extra-Articular Group (N = 21) | Intra-Articular Group (N = 25) | p-Value | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Age (year) | 52.9 ± 18.5 | 54.0 ± 18.9 | 0.659 a |
| Time of image taken after operation (Day) | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.000 a |
| Time of 3 months follow-up image taken (Day) | 83.3 ± 8.8 | 83.6 ± 13.1 | 0.956 a |
| N (%) | N (%) | ||
| Dominant | 0.551 b | ||
| Right | 7 (33.3) | 11 (44.0) | |
| Left | 14 (66.7) | 14 (56.0) | |
| Gender | 0.760 b | ||
| Male | 13 (61.9) | 17 (68) | |
| Female | 8 (38.1) | 8 (32) |
| Extra-Articular Group | Intra-Articular Group | p-Value a | |||
|---|---|---|---|---|---|
| RH | Post-OP | mean (mm) | 10.75 | 11.40 | |
| SD (mm) | 2.41 | 2.23 | 0.348 | ||
| range (mm) | 7.27~15.15 | 7.11~15.58 | |||
| 3m-f | mean (mm) | 10.80 | 11.35 | ||
| SD (mm) | 2.00 | 3.00 | 0.474 | ||
| range (mm) | 6.48~14.51 | 3.16~17.28 | |||
| p-value b | 0.899 | 0.926 | |||
| UV | Post-OP | mean (mm) | 0.58 | 1.96 | |
| SD (mm) | 2.32 | 2.53 | 0.063 | ||
| range (mm) | −4.05~4.22 | −1.91~11.16 | |||
| 3m-f | mean (mm) | 1.23 | 1.87 | ||
| SD (mm) | 2.05 | 2.05 | 0.300 | ||
| range (mm) | −3.76~4.41 | −3.90~6.06 | |||
| p-value | 0.090 b | 0.503 c | |||
| RI | Post-OP | mean (°) | 20.14 | 21.45 | |
| SD (°) | 3.94 | 4.07 | 0.278 | ||
| range (°) | 13.50~26.40 | 14.10~31.40 | |||
| 3m-f | mean (mm) | 20.74 | 22.18 | ||
| SD (mm) | 3.95 | 5.46 | 0.320 | ||
| range (mm) | 10.50~31.70 | 7.10~33.40 | |||
| p-value c | 1.000 | 0.108 | |||
| VT | Post-OP | mean (°) | 13.14 | 12.77 | |
| SD (°) | 5.50 | 5.57 | 0.822 | ||
| range (°) | 4.70~22.30 | 0.80~22.70 | |||
| 3m-f | mean (°) | 13.60 | 12.80 | ||
| SD (°) | 5.69 | 4.94 | 0.614 | ||
| range (°) | 2.40~24.40 | 4.40~21.90 | |||
| p-value b | 0.521 | 0.963 | |||
| TDA | Post-OP | mean (°) | 59.00 | 53.99 | |
| SD (°) | 5.71 | 10.55 | 0.048 | ||
| range (°) | 46.80~70.20 | 25.20~74.50 | |||
| 3m-f | mean (°) | 56.67 | 53.06 | ||
| SD (°) | 9.14 | 8.63 | 0.176 | ||
| range (°) | 33.00~68.80 | 35.00~69.30 | |||
| p-value b | 0.274 | 0.551 | |||
| DDD | Post-OP | mean (°) | 4.69 | 5.55 | |
| SD (°) | 1.75 | 1.87 | 0.118 | ||
| range (°) | 1.99~8.49 | 3.68~8.66 | |||
| 3m-f | mean (°) | 4.71 | 4.77 | ||
| SD (°) | 1.66 | 1.58 | 0.893 | ||
| range (°) | 1.83~8.82 | 2.53~9.01 | |||
| p-value b | 0.956 | 0.008 |
| Extra-Articular Group (N = 21) | Intra-Articular Group (N = 25) | p-Value | ||
|---|---|---|---|---|
| N (%) | N (%) | |||
| Risk of tendon rupture in post-op | Low risk | 19 (90.5) | 22 (88.0) | 0.585 a |
| High risk | 2 (9.5) | 3 (12.0) | ||
| Risk of tendon rupture in 3m-f | Low risk | 19 (90.5) | 24 (96) | 0.443 a |
| High risk | 2 (9.5) | 1 (4.0) | ||
| The change of risk in 3 months | Low risk to low risk | 19 (90.5) | 22 (88.0) | 0.225 b |
| Low risk to high risk | 0 (0.0) | 2 (8.0) | ||
| High risk to high risk | 2 (9.5) | 1 (4.0) |
| Variable | B | p-Value a | |
|---|---|---|---|
| Extra-articular group (N = 21) | Post-op Distal dorsal cortical distance | 4.649 | 0.907 |
| C3m Distal dorsal cortical distance | 0.052 | ||
| Intra-articular group (N = 25) | Post-op Distal dorsal cortical distance | 4.519 | 0.031 |
| C3m Distal dorsal cortical distance | 0.850 | ||
| Combined two groups (N = 46) | Post-op Distal dorsal cortical distance | 4.561 | 0.048 |
| C3m Distal dorsal cortical distance | 0.573 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, P.-C.; Lo, T.-Y.-Y.; Cheng, C.-Y.; Wu, C.-T.; Chen, A.C.-Y. Radiographic Analysis in Extra-Articular and Intra-Articular Distal Radius Fractures Treated with Variable-Angle Volar Locking Plate Fixation. J. Clin. Med. 2023, 12, 3494. https://doi.org/10.3390/jcm12103494
Fang P-C, Lo T-Y-Y, Cheng C-Y, Wu C-T, Chen AC-Y. Radiographic Analysis in Extra-Articular and Intra-Articular Distal Radius Fractures Treated with Variable-Angle Volar Locking Plate Fixation. Journal of Clinical Medicine. 2023; 12(10):3494. https://doi.org/10.3390/jcm12103494
Chicago/Turabian StyleFang, Pin-Chieh, Tak-Yu-Yubie Lo, Chun-Ying Cheng, Chun-Te Wu, and Alvin Chao-Yu Chen. 2023. "Radiographic Analysis in Extra-Articular and Intra-Articular Distal Radius Fractures Treated with Variable-Angle Volar Locking Plate Fixation" Journal of Clinical Medicine 12, no. 10: 3494. https://doi.org/10.3390/jcm12103494





