Mindful Coping Power Effects on Children’s Autonomic Nervous System Functioning and Long-Term Behavioral Outcomes
Abstract
1. Introduction
1.1. Proactive and Reactive Aggression
1.2. Active Mechanisms of Reactive Aggression
1.3. Polyvagal Theory and Reactive Aggression
1.4. Mindfulness Training Effects
1.5. Targeting Active Mechanisms of Dysregulation with Mindful Coping Power
1.6. The Current Study
- (1)
- Does Mindful Coping Power (MCP) produce better child behavioral outcomes at a 1-year follow-up than Coping Power (CP), as measured by teacher-rated child reactive aggression, externalizing behavior problems, proactive aggression, and social skills?
- (2)
- Does the Coping Power preventive intervention (full sample with both MCP and CP) have a beneficial impact on children’s physiological stress reactivity (SCL and RSA reactivities) from pre- to post-intervention? If so, does MCP produce stronger beneficial effects on children’s stress physiology than CP?
- (3)
- Do intervention-produced improvements in children’s stress physiology (SCL and RSA reactivities) and perceived self-regulation and mindful awareness (total dysregulation, inhibitory control, breath awareness) from pre- to post-intervention mediate improvements in child behavioral outcomes at a 1-year follow-up (as measured by child reactive aggression, externalizing behavior problems, proactive aggression, and social skills)?
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures and Tasks
2.4. Statistical Approach
3. Results
3.1. Results
3.1.1. Research Question 1
3.1.2. Research Question 2
3.1.3. Research Question 3
4. Discussion
4.1. MCP Effects on Children’s Long-Term Behavioral Outcomes
4.2. MCP Effects on Children’s Autonomic Nervous System Functioning
4.3. Mediational Analyses
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Powell, N.P.; Lochman, J.E.; Boxmeyer, C.L.; Barry, T.D.; Pardini, D.A. The coping power program for aggressive behavior in children. In Evidence-Based Psychotherapies for Children and Adolescents; Weisz, J.R., Kazdin, A.E., Eds.; The Guilford Press: New York, NY, USA, 2018; pp. 159–176. [Google Scholar]
- Lochman, J.E.; Wells, K.C. Contextual social-cognitive mediators and child outcome: A test of the theoretical model in the Coping Power program. Dev. Psychopathol. 2002, 14, 945–967. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.; Boxmeyer, C.; Romero, D.; Powell, N.; Jones, S.; Lochman, J. Theoretical Model of Mindful Coping Power: Optimizing a Cognitive Behavioral Program for High-Risk Children and Their Parents by Integrating Mindfulness. Clin. Child. Fam. Psychol. Rev. 2020, 23, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Lochman, J.E.; Baden, R.E.; Boxmeyer, C.L.; Powell, N.P.; Qu, L.; Salekin, K.L.; Windle, M. Does a booster intervention augment the preventive effects of an abbreviated version of the coping power program for aggressive children? J. Abnorm. Child. Psychol. 2014, 42, 367–381. [Google Scholar] [CrossRef]
- Lochman, J.E.; Wells, K.C. The coping power program for preadolescent aggressive boys and their parents: Outcome effects at the 1-year follow-up. J. Consult. Clin. Psychol. 2004, 72, 571–578. [Google Scholar] [CrossRef]
- Lochman, J.E.; Wells, K.C.; Qu, L.; Chen, L. Three year follow-up of Coping Power intervention effects: Evidence of neighborhood moderation? Prev. Sci. 2013, 14, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Lochman, J.E.; Boxmeyer, C.L.; Powell, N.P.; Qu, L.; Wells, K.; Windle, M. Coping Power dissemination study: Intervention and special education effects on academic outcomes. Behav. Disord. 2012, 37, 192–205. [Google Scholar] [CrossRef]
- Muratori, P.; Milone, A.; Levantini, V.; Ruglioni, L.; Lambruschi, F.; Pisano, S.; Masi, G.; Lochman, J.E. Six-year outcome for children with ODD or CD treated with the coping power program. Psychiatry Res. 2019, 271, 454–458. [Google Scholar] [CrossRef]
- Zonnevylle-Bender, M.J.S.; Matthys, W.; van de Wiel, N.M.H.; Lochman, J.E. Preventive effects of treatment of disruptive behavior disorder in middle childhood on substance use and delinquent behavior. J. Am. Acad. Child. Adolesc. Psychiatry 2007, 46, 33–39. [Google Scholar] [CrossRef]
- Dodge, K.A. The structure and function of reactive and proactive aggression. In The Development and Treatment of Childhood Aggression; Lawrence Erlbaum Associates, Inc.: Hillsdale, MI, USA, 1991; Volume 16, pp. 201–218. [Google Scholar]
- Bezdjian, S.; Tuvblad, C.; Raine, A.; Baker, L.A. The genetic and environmental covariation among psychopathic personality traits, and reactive and proactive aggression in childhood. Child. Dev. 2011, 82, 1267–1281. [Google Scholar] [CrossRef]
- Dodge, K.A.; Lochman, J.E.; Harnish, J.D.; Bates, J.E.; Pettit, G.S. Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. J. Abnorm. Psychol. 1997, 106, 37–51. [Google Scholar] [CrossRef]
- Vitaro, F.; Brendgen, M.; Tremblay, R.E. Reactively and proactively aggressive children: Antecedent and subsequent characteristics. J. Child Psychol. Psychiatry 2002, 43, 495–505. [Google Scholar] [CrossRef] [PubMed]
- Card, N.A.; Little, T.D. Proactive and reactive aggression in childhood and adolescence: A meta-analysis of differential relations with psychosocial adjustment. Int. J. Behav. Dev. 2016, 30, 466–480. [Google Scholar] [CrossRef]
- Card, N.A.; Little, T.D. Differential relations of instrumental and reactive aggression with maladjustment: Does adaptivity depend on function? In Aggression and Adaptation; Routledge: New York, NY, USA, 2007; pp. 107–134. [Google Scholar]
- Fite, P.J.; Raine, A.; Stouthamer-Loeber, M.; Loeber, R.; Pardini, D.A. Reactive and proactive aggression in adolescent males: Examining differential outcomes 10 years later in early adulthood. Crim. Justice Behav. 2010, 37, 141–157. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Zhou, X.; Xia, L.X. Brain structures and functional connectivity associated with individual differences in trait proactive aggression. Sci. Rep. 2019, 9, 7731. [Google Scholar] [CrossRef] [PubMed]
- White, S.F.; VanTieghem, M.; Brislin, S.J.; Sypher, I.; Sinclair, S.; Pine, D.S.; Hwang, S.; Blair, R.J. Neural Correlates of the Propensity for Retaliatory Behavior in Youths With Disruptive Behavior Disorders. Am. J. Psychiatry 2016, 173, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Joshi, S.H.; Jahanshad, N.; Thompson, P.M.; Baker, L.A. Neural correlates of proactive and reactive aggression in adolescent twins. Aggress. Behav. 2017, 43, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Lochman, J.E.; Wells, K.C. The Coping Power program at the middle-school transition: Universal and indicated prevention effects. Psychol. Addict. Behav. 2002, 16, S40–S54. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, A.; Lochman, J.E.; Tariq, P.N.; Sabih, F. Preliminary Effectiveness Study of Coping Power Program for Aggressive Children in Pakistan. Prev. Sci. 2017, 18, 762–771. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, E.P.; Speck, J.S.; Frick, P.J.; Walker, T.M.; Robertson, E.L.; Ray, J.V.; Wall-Myers, T.D.; Thornton, L.C.; Syeinberg, L.; Cauffman, E. Proactive and reactive aggression: Development trajectories and longitudinal associations with callous-unemotional traits, impulsivity, and internalizing emotions. Dev. Psychopathol. 2023, 1–9. [Google Scholar] [CrossRef]
- Fite, P.J.; Colder, C.R.; Lochman, J.E.; Wells, K.C. Pathways from proactive and reactive aggression to substance use. Psychol. Addict. Behav. 2007, 21, 355–364. [Google Scholar] [CrossRef]
- Lickley, R.A.; Sebastian, C.L. The neural basis of reactive aggression and its development in adolescence. Psychol. Crime Law 2018, 24, 313–333. [Google Scholar] [CrossRef]
- Barry, T.D.; Thompson, A.; Barry, C.T.; Lochman, J.E.; Adler, K.; Hill, K. The importance of narcissism in predicting proactive and reactive aggression in moderately to highly aggressive children. Aggress. Behav. 2007, 33, 185–197. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, N.; Fabes, R.A.; Nyman, M.; Bernzweig, J.; Pinuelas, A. The relations of emotionality and regulation to children’s anger-related reactions. Child Dev. 1994, 65, 109–128. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.L.; Weiss, B.; Lochman, J.E. Executive functions in children: Associations with aggressive behavior and appraisal processing. J. Abnorm. Child Psychol. 2009, 37, 945–956. [Google Scholar] [CrossRef]
- Choe, D.E.; Shaw, D.S.; Forbes, E.E. Maladaptive social information processing in childhood predicts young men’s atypical amygdala reactivity to threat. J. Child Psychol. Psychiatry 2015, 56, 549–557. [Google Scholar] [CrossRef]
- Hubbard, J.A.; Smithmyer, C.M.; Ramsden, S.R.; Parker, E.H.; Flanagan, K.D.; Dearing, K.F.; Relyea, N.; Simons, R.F. Observational, physiological, and self-report measures of children’s anger: Relations to reactive versus proactive aggression. Child Dev. 2002, 73, 1101–1118. [Google Scholar] [CrossRef]
- Lopez-Duran, N.L.; Olson, S.L.; Hajal, N.J.; Felt, B.T.; Vazquez, D.M. Hypothalamic pituitary adrenal axis functioning in reactive and proactive aggression in children. J. Abnorm. Child Psychol. 2009, 37, 169–182. [Google Scholar] [CrossRef]
- Fite, P.J.; Colder, C.R.; Pelham, W.E., Jr. A factor analytic approach to distinguish pure and co-occurring dimensions of proactive and reactive aggression. J. Clin. Child Adolesc. Psychol. 2006, 35, 578–582. [Google Scholar] [CrossRef]
- de Castro, B.O.; Merk, W.; Koops, W.; Veerman, J.W.; Bosch, J.D. Emotions in social information processing and their relations with reactive and proactive aggression in referred aggressive boys. J. Clin. Child. Adolesc. Psychol. 2005, 34, 105–116. [Google Scholar] [CrossRef]
- Denson, T.F.; DeWall, C.N.; Finkel, E.J. Self-control and aggression. Curr. Dir. Psychol. Sci. 2012, 21, 20–25. [Google Scholar] [CrossRef]
- Rohlf, H.L.; Holl, A.K.; Kirsch, F.; Krahe, B.; Elsner, B. Longitudinal Links between Executive Function, Anger, and Aggression in Middle Childhood. Front. Behav. Neurosci. 2018, 12, 27. [Google Scholar] [CrossRef]
- Thomson, N.D.; Kevorkian, S.; Blair, J.; Farrell, A.; West, S.J.; Bjork, J.M. Psychophysiological underpinnings of proactive and reactive aggression in young men and women. Physiol. Behav. 2021, 242, 113601. [Google Scholar] [CrossRef] [PubMed]
- Raine, A.; Dodge, K.; Loeber, R.; Gatzke-Kopp, L.; Lynam, D.; Reynolds, C.; Stouthamer-Loeber, M.; Liu, J. The Reactive-Proactive Aggression Questionnaire: Differential Correlates of Reactive and Proactive Aggression in Adolescent Boys. Aggress. Behav. 2006, 32, 159–171. [Google Scholar] [CrossRef]
- Porges, S.W. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology 1995, 32, 301–318. [Google Scholar] [CrossRef]
- Moore, C.C.; Hubbard, J.; Morrow, M.T.; Barhight, L.R.; Lines, M.M.; Sallee, M.; Hyde, C.T. The simultaneous assessment of and relations between children’s sympathetic and parasympathetic psychophysiology and their reactive and proactive aggression. Aggress. Behav. 2018, 44, 614–623. [Google Scholar] [CrossRef]
- van Goozen, S.H.; Fairchild, G.; Snoek, H.; Harold, G.T. The evidence for a neurobiological model of childhood antisocial behavior. Psychol. Bull. 2007, 133, 149–182. [Google Scholar] [CrossRef]
- Murray-Close, D.; Holterman, L.A.; Breslend, N.L.; Sullivan, A. Psychophysiology of proactive and reactive relational aggression. Biol. Psychol. 2017, 130, 77–85. [Google Scholar] [CrossRef]
- Kassing, F.; Lochman, J.E.; Glenn, A.L. Autonomic functioning in reactive versus proactive aggression: The influential role of inconsistent parenting. Aggress. Behav. 2018, 44, 524–536. [Google Scholar] [CrossRef]
- Glenn, A.L.; Lochman, J.E.; Dishion, T.; Powell, N.P.; Boxmeyer, C.; Kassing, F.; Qu, L.; Romero, D. Toward Tailored Interventions: Sympathetic and Parasympathetic Functioning Predicts Responses to an Intervention for Conduct Problems Delivered in Two Formats. Prev. Sci. 2019, 20, 30–40. [Google Scholar] [CrossRef]
- Raine, A. Autonomic nervous system factors underlying disinhibited, antisocial, and violent behavior. Biosocial perspectives and treatment implications. Ann. N. Y. Acad. Sci. 1996, 794, 46–59. [Google Scholar] [CrossRef]
- Beauchaine, T. Vagal tone, development, and Gray’s motivational theory: Toward an integrated model of autonomic nervous system functioning in psychopathology. Dev. Psychopathol. 2001, 13, 183–214. [Google Scholar] [CrossRef]
- Fowles, D.C.; Kochanska, G.; Murray, K. Electrodermal activity and temperament in preschool children. Psychophysiology 2000, 37, 777–787. [Google Scholar] [CrossRef]
- Posthumus, J.A.; Bocker, K.B.; Raaijmakers, M.A.; Van Engeland, H.; Matthys, W. Heart rate and skin conductance in four-year-old children with aggressive behavior. Biol. Psychol. 2009, 82, 164–168. [Google Scholar] [CrossRef]
- Porges, S.W. The polyvagal theory: New insights into adaptive reactions of the autonomic nervous system. Cleve. Clin. J. Med. 2009, 76 (Suppl. S2), S86–S90. [Google Scholar] [CrossRef]
- Berntson, G.G.; Bigger, J.T., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef]
- Beauchaine, T.P. Respiratory Sinus Arrhythmia: A Transdiagnostic Biomarker of Emotion Dysregulation and Psychopathology. Curr. Opin. Psychol. 2015, 3, 43–47. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Bell, Z.; Knapton, E.; McDonough-Caplan, H.; Shader, T.; Zisner, A. Respiratory sinus arrhythmia reactivity across empirically based structural dimensions of psychopathology: A meta-analysis. Psychophysiology 2019, 56, e13329. [Google Scholar] [CrossRef]
- Hastings, P.D.; Miller, J.G. Autonomic regulation, polyvagal theory, and children’s prosocial development. Prosocial Dev. A Multidimens. Approach 2014, 112–127. [Google Scholar] [CrossRef]
- Beauchaine, T.P.; Gatzke-Kopp, L.; Neuhaus, E.; Chipman, J.; Reid, M.J.; Webster-Stratton, C. Sympathetic- and parasympathetic-linked cardiac function and prediction of externalizing behavior, emotion regulation, and prosocial behavior among preschoolers treated for ADHD. J. Consult. Clin. Psychol. 2013, 81, 481–493. [Google Scholar] [CrossRef]
- Cui, L.; Morris, A.S.; Harrist, A.W.; Larzelere, R.E.; Criss, M.M.; Houltberg, B.J. Adolescent RSA responses during an anger discussion task: Relations to emotion regulation and adjustment. Emotion 2015, 15, 360–372. [Google Scholar] [CrossRef]
- Sullivan, M.B.; Erb, M.; Schmalzl, L.; Moonaz, S.; Noggle Taylor, J.; Porges, S.W. Yoga Therapy and Polyvagal Theory: The Convergence of Traditional Wisdom and Contemporary Neuroscience for Self-Regulation and Resilience. Front. Hum. Neurosci. 2018, 12, 67. [Google Scholar] [CrossRef]
- Baer, R.A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pract. 2003, 10, 125–143. [Google Scholar] [CrossRef]
- Kabat-Zinn, J.; Hachette, U.K. Full Catastrophe Living, Revised Edition: How to Cope with Stress, Pain and Illness Using Mindfulness Meditation; New Harbinger Publications: Oakland, CA, USA, 2013. [Google Scholar]
- Black, D.S.; Fernando, R. Mindfulness training and classroom behavior among lower-income and ethnic minority elementary school children. J. Child Fam. Stud. 2013, 22, 1–5. [Google Scholar] [CrossRef]
- Flook, L.; Smalley, S.L.; Kitil, M.J.; Galla, B.M.; Kaiser-Greenland, S. Effects of mindful awareness practices on executive function in elementary school children. J. Appl. Sch. Psychol. 2010, 26, 70–95. [Google Scholar] [CrossRef]
- Sibinga, E.M.; Perry-Parrish, C.; Chung, S.E.; Johnson, S.B.; Smith, M.; Ellen, J.M. School-based mindfulness instruction for urban male youth: A small randomized controlled trial. Prev. Med. 2013, 57, 799–801. [Google Scholar] [CrossRef]
- Schonert-Reichl, K.A.; Oberle, E.; Lawlor, M.S.; Abbott, D.; Thomson, K.; Oberlander, T.F.; Diamond, A. Enhancing cognitive and social-emotional development through a simple-to-administer mindfulness-based school program for elementary school children: A randomized controlled trial. Dev. Psychol. 2015, 51, 52–66. [Google Scholar] [CrossRef]
- Franco, C.; Amutio, A.; Lopez-Gonzalez, L.; Oriol, X.; Martinez-Taboada, C. Effect of a Mindfulness Training Program on the Impulsivity and Aggression Levels of Adolescents with Behavioral Problems in the Classroom. Front. Psychol. 2016, 7, 1385. [Google Scholar] [CrossRef]
- Bögels, S.; Hoogstad, B.; van Dun, L.; de Schutter, S.; Restifo, K. Mindfulness Training for Adolescents with Externalizing Disorders and their Parents. Behav. Cogn. Psychother. 2008, 36, 193–209. [Google Scholar] [CrossRef]
- Metz, S.M.; Frank, J.L.; Reibel, D.; Cantrell, T.; Sanders, R.; Broderick, P.C. The Effectiveness of the Learning to BREATHE Program on Adolescent Emotion Regulation. Res. Hum. Dev. 2013, 10, 252–272. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Ma, Y.; Wang, J.; Fan, Y.; Feng, S.; Lu, Q.; Yu, Q.; Sui, D.; Rothbart, M.K.; Fan, M.; et al. Short-term meditation training improves attention and self-regulation. Proc. Natl. Acad. Sci. USA 2007, 104, 17152–17156. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Tang, R.; Posner, M.I. Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug Alcohol Depend. 2016, 163 (Suppl. S1), S13–S18. [Google Scholar] [CrossRef] [PubMed]
- Muratori, P.; Conversano, C.; Levantini, V.; Masi, G.; Milone, A.; Villani, S.; Bogels, S.; Gemignani, A. Exploring the Efficacy of a Mindfulness Program for Boys with Attention-Deficit Hyperactivity Disorder and Oppositional Defiant Disorder. J. Atten. Disord. 2021, 25, 1544–1553. [Google Scholar] [CrossRef]
- van der Oord, S.; Bogels, S.M.; Peijnenburg, D. The Effectiveness of Mindfulness Training for Children with ADHD and Mindful Parenting for their Parents. J. Child. Fam. Stud. 2012, 21, 139–147. [Google Scholar] [CrossRef]
- Boxmeyer, C.L.; Miller, S.; Romero, D.E.; Powell, N.P.; Jones, S.; Qu, L.; Tueller, S.; Lochman, J.E. Mindful Coping Power: Comparative Effects on Children’s Reactive Aggression and Self-Regulation. Brain. Sci. 2021, 11, 1119. [Google Scholar] [CrossRef]
- Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; Schulenberg, J.E. Monitoring the Future National Survey Results on Drug Use, 1975–2010. Volume I, Secondary School Students. 2011. Available online: https://rhyclearinghouse.acf.hhs.gov/sites/default/files/docs/20897-Monitoring_the_Future-Secondary-2010.pdf (accessed on 19 May 2023).
- Dodge, K.A.; Coie, J.D. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. J. Pers. Soc. Psychol. 1987, 53, 1146–1158. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, C.R.; Kamphaus, R.W. The Clinician’s Guide to the Behavior Assessment System for Children (BASC); Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Lochman, J.E.; Wells, K.C.; Lenhart, L.A. Coping Power: Child Group Program Facilitator’s Guide; Oxford University Press: New York, NY, USA, 2008; ISBN 9780195327878. [Google Scholar]
- Wells, K.C.; Lochman, J.E.; Lenhart, L.A. Coping Power: Parent Group Program Facilitator’s Guide; Oxford University Press: New York, NY, USA, 2008; ISBN 9780195327885. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-based stress reduction (MBSR). Constr. Hum. Sci. 2003, 8, 73–107, ISSN 1520-2984. [Google Scholar]
- Reynolds, C.R.; Kamphaus, R.W. Behavior Assessment System for Children; American Guidance Service: Circle Pines, MN, USA, 1992. [Google Scholar]
- Mezzich, A.C.; Tarter, R.E.; Giancola, P.R.; Kirisci, L. The dysregulation inventory: A new scale to assess the risk for substance use disorder. J. Child Adolesc. Subst. Abus. 2001, 10, 35–43. [Google Scholar] [CrossRef]
- Capaldi, D.M.; Rothbart, M.K. Development and validation of an early adolescent temperament measure. J. Early Adolesc. 1992, 12, 153–173. [Google Scholar] [CrossRef]
- Price, C.J.; Thompson, E.A.; Cheng, S.C. Scale of Body Connection: A multi-sample construct validation study. PLoS ONE 2017, 12, e0184757. [Google Scholar] [CrossRef]
- Porges, S. Inter-Beat Interval Editing for Heart Period Variability Analysis: An Integrated Training Program with Standards for Student Reliability Assessment; The Brain-Body Center at the University of Illinois: Chicago, IL, USA, 2007. [Google Scholar]
- Lewis, G.F.; Furman, S.A.; McCool, M.F.; Porges, S.W. Statistical strategies to quantify respiratory sinus arrhythmia: Are commonly used metrics equivalent? Biol. Psychol. 2012, 89, 349–364. [Google Scholar] [CrossRef]
- Benedek, M.; Kaernbach, C. A continuous measure of phasic electrodermal activity. J. Neurosci. Methods 2010, 190, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Bechara, A.; Damasio, A.R.; Damasio, H.; Anderson, S.W. Insensitivity to future consequences following damage to human prefrontal cortex. Cognition 1994, 50, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Brevers, D.; Bechara, A.; Cleeremans, A.; Noel, X. Iowa Gambling Task (IGT): Twenty years after - gambling disorder and IGT. Front. Psychol. 2013, 4, 665. [Google Scholar] [CrossRef] [PubMed]
- Kully-Martens, K.; Treit, S.; Pei, J.; Rasmussen, C. Affective decision-making on the Iowa gambling task in children and adolescents with fetal alcohol spectrum disorders. J. Int. Neuropsychol. Soc. 2013, 19, 137–144. [Google Scholar] [CrossRef]
- Schutter, D.J.; van Bokhoven, I.; Vanderschuren, L.J.; Lochman, J.E.; Matthys, W. Risky decision making in substance dependent adolescents with a disruptive behavior disorder. J. Abnorm. Child. Psychol. 2011, 39, 333–339. [Google Scholar] [CrossRef]
- Umbach, R.; Leonard, N.R.; Luciana, M.; Ling, S.; Laitner, C. The Iowa Gambling Task in Violent and Nonviolent Incarcerated Male Adolescents. Crim. Justice Behav. 2019, 46, 1611–1629. [Google Scholar] [CrossRef]
- Bechara, A.; Damasio, H.; Tranel, D.; Damasio, A.R. Deciding advantageously before knowing the advantageous strategy. Science 1997, 275, 1293–1295. [Google Scholar] [CrossRef]
- Arıkan İyilikci, E.; Amado, S. The uncertainty appraisal enhances the prominent deck B effect in the Iowa gambling task. Motiv. Emot. 2017, 42, 1–16. [Google Scholar] [CrossRef]
- Northoff, G.; Grimm, S.; Boeker, H.; Schmidt, C.; Bermpohl, F.; Heinzel, A.; Hell, D.; Boesiger, P. Affective judgment and beneficial decision making: Ventromedial prefrontal activity correlates with performance in the Iowa Gambling Task. Hum. Brain. Mapp. 2006, 27, 572–587. [Google Scholar] [CrossRef]
- Almy, B.; Kuskowski, M.; Malone, S.M.; Myers, E.; Luciana, M. A longitudinal analysis of adolescent decision-making with the Iowa Gambling Task. Dev. Psychol. 2018, 54, 689–702. [Google Scholar] [CrossRef]
- Li, Y.; Chen, R.; Zhang, S.; Turel, O.; Bechara, A.; Feng, T.; Chen, H.; He, Q. Hemispheric mPFC asymmetry in decision making under ambiguity and risk: An fNIRS study. Behav. Brain. Res. 2019, 359, 657–663. [Google Scholar] [CrossRef]
- Statistical Analysis Software (SAS/STAT 15.1), SAS Institute Inc.: Cary, NC, USA, 2016.
- Morris, S.B. Estimating Effect Sizes from Pretest-Posttest-Control Group Designs. Organ. Res. Methods 2007, 11, 364–386. [Google Scholar] [CrossRef]
- Valente, M.J.; MacKinnon, D.P. Comparing models of change to estimate the mediated effect in the pretest-posttest control group design. Struct. Equ. Model. 2017, 24, 428–450. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, D.P.; Fritz, M.S.; Williams, J.; Lockwood, C.M. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behav. Res. Methods 2007, 39, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, J.D.; Catalano, R.F.; Miller, J.Y. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol. Bull. 1992, 112, 64–105. [Google Scholar] [CrossRef]
- Lochman, J.E.; Boxmeyer, C.L.; Jones, S.; Qu, L.; Ewoldsen, D.; Nelson, W.M., 3rd. Testing the feasibility of a briefer school-based preventive intervention with aggressive children: A hybrid intervention with face-to-face and internet components. J. Sch. Psychol. 2017, 62, 33–50. [Google Scholar] [CrossRef]
- Lochman, J.E.; Wells, K.C. A social-cognitive intervention with aggressive children: Prevention effects and contextual implementation issues. In Prevention and Early Intervention: Childhood Disorders, Substance Use, and Delinquency; Peters, R.D., McMahon, R.J., Eds.; Sage: Newbury Park, CA, USA, 1996; pp. 111–143. [Google Scholar]
- Crick, N.R.; Dodge, K.A. Social information-processing mechanisms in reactive and proactive aggression. Child. Dev. 1996, 67, 993–1002. [Google Scholar] [CrossRef]
- Lochman, J.E.; Vernberg, E.; Glenn, A.; Jarrett, M.; McDonald, K.; Powell, N.P.; Abel, M.; Boxmeyer, C.L.; Kassing, F.; Qu, L.; et al. Effects of Autonomic Nervous System Functioning and Tornado Exposure on Long-Term Outcomes of Aggressive Children. Res. Child Adolesc. Psychopathol. 2021, 49, 471–489. [Google Scholar] [CrossRef]
- Vasilev, C.A.; Crowell, S.E.; Beauchaine, T.P.; Mead, H.K.; Gatzke-Kopp, L.M. Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. J. Child Psychol. Psychiatry 2009, 50, 1357–1364. [Google Scholar] [CrossRef]
- Gazelle, H.; Druhen, M.J. Anxious solitude and peer exclusion predict social helplessness, upset affect, and vagal regulation in response to behavioral rejection by a friend. Dev. Psychol. 2009, 45, 1077–1096. [Google Scholar] [CrossRef]
- Jimenez-Camargo, L.A.; Lochman, J.E.; Sellbom, M. Externalizing behavior in at-risk preadolescents: Relationships among effortful control, affective experiences, and autonomic psychophysiology. J. Psychopathol. Behav. Assess. 2017, 39, 383–395. [Google Scholar] [CrossRef]
- Rothbart, M.K. Temperament in childhood: A framework. In Temperament in Childhood; Kohnstamm, G., Bates, J., Rothbart, M.K., Eds.; Wiley: Chichester, UK, 1989; pp. 59–73. [Google Scholar]
- Raaijmakers, M.A.; Smidts, D.P.; Sergeant, J.A.; Maassen, G.H.; Posthumus, J.A.; van Engeland, H.; Matthys, W. Executive functions in preschool children with aggressive behavior: Impairments in inhibitory control. J. Abnorm. Child Psychol. 2008, 36, 1097–1107. [Google Scholar] [CrossRef] [PubMed]
- Sarkisian, K.; Van Hulle, C.; Lemery-Chalfant, K.; Goldsmith, H. Childhood inhibitory control and adolescent impulsivity and novelty seeking as differential predictors of relational and overt aggression. J. Res. Personal. 2017, 67, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Fosco, W.D.; Hawk, L.W., Jr.; Colder, C.R.; Meisel, S.N.; Lengua, L.J. The development of inhibitory control in adolescence and prospective relations with delinquency. J. Adolesc. 2019, 76, 37–47. [Google Scholar] [CrossRef]
- Nigg, J.T.; Wong, M.M.; Martel, M.M.; Jester, J.M.; Puttler, L.I.; Glass, J.M.; Adams, K.M.; Fitzgerald, H.E.; Zucker, R.A. Poor response inhibition as a predictor of problem drinking and illicit drug use in adolescents at risk for alcoholism and other substance use disorders. J. Am. Acad. Child Adolesc. Psychiatry 2006, 45, 468–475. [Google Scholar] [CrossRef]
- Tarter, R.E.; Kirisci, L.; Mezzich, A.; Cornelius, J.R.; Pajer, K.; Vanyukov, M.; Gardner, W.; Blackson, T.; Clark, D. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am. J. Psychiatry 2003, 160, 1078–1085. [Google Scholar] [CrossRef]
- Oldehinkel, A.J.; Hartman, C.A.; Ferdinand, R.F.; Verhulst, F.C.; Ormel, J. Effortful control as modifier of the association between negative emotionality and adolescents’ mental health problems. Dev. Psychopathol. 2007, 19, 523–539. [Google Scholar] [CrossRef]
- Greco, L.A.; Baer, R.A.; Smith, G.T. Assessing mindfulness in children and adolescents: Development and validation of the Child and Adolescent Mindfulness Measure (CAMM). Psychol. Assess. 2011, 23, 606–614. [Google Scholar] [CrossRef]
- Erath, S.A.; Su, S.; Tu, K.M. Electrodermal Reactivity Moderates the Prospective Association Between Peer Victimization and Depressive Symptoms in Early Adolescence. J. Clin. Child Adolesc. Psychol. 2018, 47, 992–1003. [Google Scholar] [CrossRef]

| Cases with Complete 1-Year Follow-Up Data | Full Intent-to-Treat Sample | |||||
| Overall (n = 80) | MCP (n = 43) | CP (n = 37) | Overall (n = 102) | MCP (n = 52) | CP (n = 50) | |
| m (sd) | m (sd) | m (sd) | m (sd) | m (sd) | m (sd) | |
| Child’s age | 10.0 (0.46) | 10.0 (0.49) | 10.0 (0.44) | 10.0 (0.48) | 10.0 (0.49) | 9.9 (.47) |
| Child’s reactive aggression 4th grade | 11.3 (2.44) | 11.2 (2.47) | 11.3 (2.45) | 11.2 (2.37) | 11.2 (2.39) | 11.2 (2.37) |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Child’s gender | ||||||
| Male | 51 (63.7%) | 28 (65.1%) | 23 (62.2%) | 62 (60.8%) | 33 (63.5%) | 29 (58.0%) |
| Female | 29 (36.3%) | 15 (34.9%) | 14 (37.8%) | 40 (39.2%) | 19 (36.5%) | 21 (42.0%) |
| Child’s ethnicity | ||||||
| Hispanic or Latino | 2 (2.5%) | 1 (2.3%) | 1 (2.7%) | 3 (2.9%) | 1 (1.9%) | 2 (4.0%) |
| Not Hispanic or Latino | 72 (90%) | 39 (90.7%) | 33 (89.2%) | 91 (89.2%) | 47 (90.4%) | 44 (88.0%) |
| Unknown or not reported | 6 (7.5%) | 3 (7.0%) | 3 (8.1%) | 8 (7.8%) | 4 (7.7%) | 4 (8.0%) |
| Child’s race | ||||||
| Black or African American | 70 (87.5%) | 38 (88.4%) | 32 (86.5%) | 89 (87.3%) | 47 (90.4%) | 42 (84%) |
| White or Caucasian | 4 (5.0%) | 2 (4.7%) | 2 (5.4%) | 6 (5.9%) | 2 (3.9%) | 4 (8.0%) |
| More than one race | 4 (5.0%) | 1 (2.3%) | 3 (8.1%) | 4 (3.9%) | 1 (1.9%) | 3 (6.0%) |
| Unknown or not reported | 2 (2.5%) | 2 (4.7%) | 0 (0%) | 3 (2.9%) | 2 (3.8%) | 1 (2.0%) |
| Annual family income | ||||||
| Less than USD 15,000 | 30 (37.5%) | 15 (34.9%) | 15 (40.5%) | 34 (33.3%) | 17 (32.7%) | 17 (34.0%) |
| USD 15,000 to <29,999 | 23 (28.8%) | 10 (23.3%) | 13 (35.1%) | 30 (29.4%) | 13 (25.0%) | 17 (34.0%) |
| USD 30,000 to <49,999 | 15 (18.8%) | 10 (23.3%) | 5 (13.5%) | 22 (21.6%) | 14 (26.9%) | 8 (16.0%) |
| More than USD 50,000 | 10 (12.5%) | 6 (14.0%) | 4 (10.8%) | 14 (13.7%) | 7 (13.5%) | 7 (14.0%) |
| Unknown or not reported | 2 (2.5%) | 2 (4.5%) | 0 (0%) | 2 (1.9%) | 1 (1.9%) | 1 (2.0%) |
| Cases with Complete SCL Data | Cases with Complete RSA Data | |||||
| Overall (n = 46) | MCP (n = 29) | CP (n = 17) | Overall (n = 45) | MCP (n = 25) | CP (n = 20) | |
| m (sd) | m (sd) | m (sd) | m (sd) | m (sd) | m (sd) | |
| Child’s age | 10.0 (0.49) | 10.0 (0.54) | 9.9 (0.43) | 10.0 (0.45) | 10.1 (0.49) | 10.0 (0.39) |
| Child’s reactive aggression 4th grade | 10.9 (2.26) | 10.9 (2.25) | 11.1 (2.33) | 11.2 (2.54) | 11.4 (2.41) | 11.0 (2.74) |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Child’s gender | ||||||
| Male | 27 (58.7%) | 18 (62.1%) | 9 (52.9%) | 28 (62.2%) | 16 (64.0%) | 12 (60.0%) |
| Female | 19 (41.3%) | 11 (37.9%) | 8 (47.1%) | 17 (37.8%) | 9 (36.0%) | 8 (40.0%) |
| Child’s ethnicity | ||||||
| Hispanic or Latino | 2 (4.3%) | 1 (3.4%) | 1 (5.9%) | 2 (4.4%) | 1 (4.0%) | 1 (5.0%) |
| Not Hispanic or Latino | 40 (87.0%) | 26 (89.7%) | 14 (82.3%) | 41 (91.1%) | 23 (92.0%) | 18 (90.0%) |
| Unknown or not reported | 4 (8.7%) | 2 (6.8%) | 2 (11.8%) | 2 (4.4%) | 1 (4.0%) | 1 (5.0%) |
| Child’s race | ||||||
| Black or African American | 39 (84.8%) | 25 (86.2%) | 14 (82.4%) | 37 (82.2%) | 21 (84.0%) | 16 (80.0%) |
| White or Caucasian | 3 (6.5%) | 2 (6.9%) | 1 (5.9%) | 4 (8.9%) | 2 (8.0%) | 2 (10.0%) |
| More than one race | 2 (4.3%) | 0 (0%) | 2 (11.8%) | 2 (4.4%) | 0 (0%) | 2 (10.0%) |
| Unknown or not reported | 2 (4.4%) | 2 (6.9%) | 0 (0%) | 2 (4.4%) | 2 (8.0%) | 0 (0%) |
| Annual family income | ||||||
| Less than USD 15,000 | 16 (34.8%) | 10 (34.5%) | 6 (35.3%) | 15 (33.3%) | 7 (28.0%) | 8 (40.0%) |
| USD 15,000 to <29,999 | 10 (21.7%) | 5 (17.2%) | 5 (29.4%) | 12 (26.7%) | 7 (28.0%) | 5 (25.0%) |
| USD 30,000 to <49,999 | 12 (26.1%) | 8 (27.6%) | 4 (23.5%) | 10 (22.2%) | 6 (24.0%) | 4 (2.0%) |
| More than USD 50,000 | 6 (13.0%) | 4 (13.8%) | 2 (11.8%) | 5 (11.1%) | 3 (12.0%) | 2 (10.0%) |
| Unknown or not reported | 2 (4.3%) | 2 (6.9%) | 0 (0%) | 3 (6.7%) | 2 (8.0%) | 1 (5.0%) |
| Coping Power (CP) | Mindful Coping Power (MCP) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Intervention | 1-Year Follow-Up | Pre-Intervention | 1-Year Follow-Up | ES | |||||||
| n | Mean | S.D. | Mean | S.D. | n | Mean | S.D. | Mean | S.D. | ||
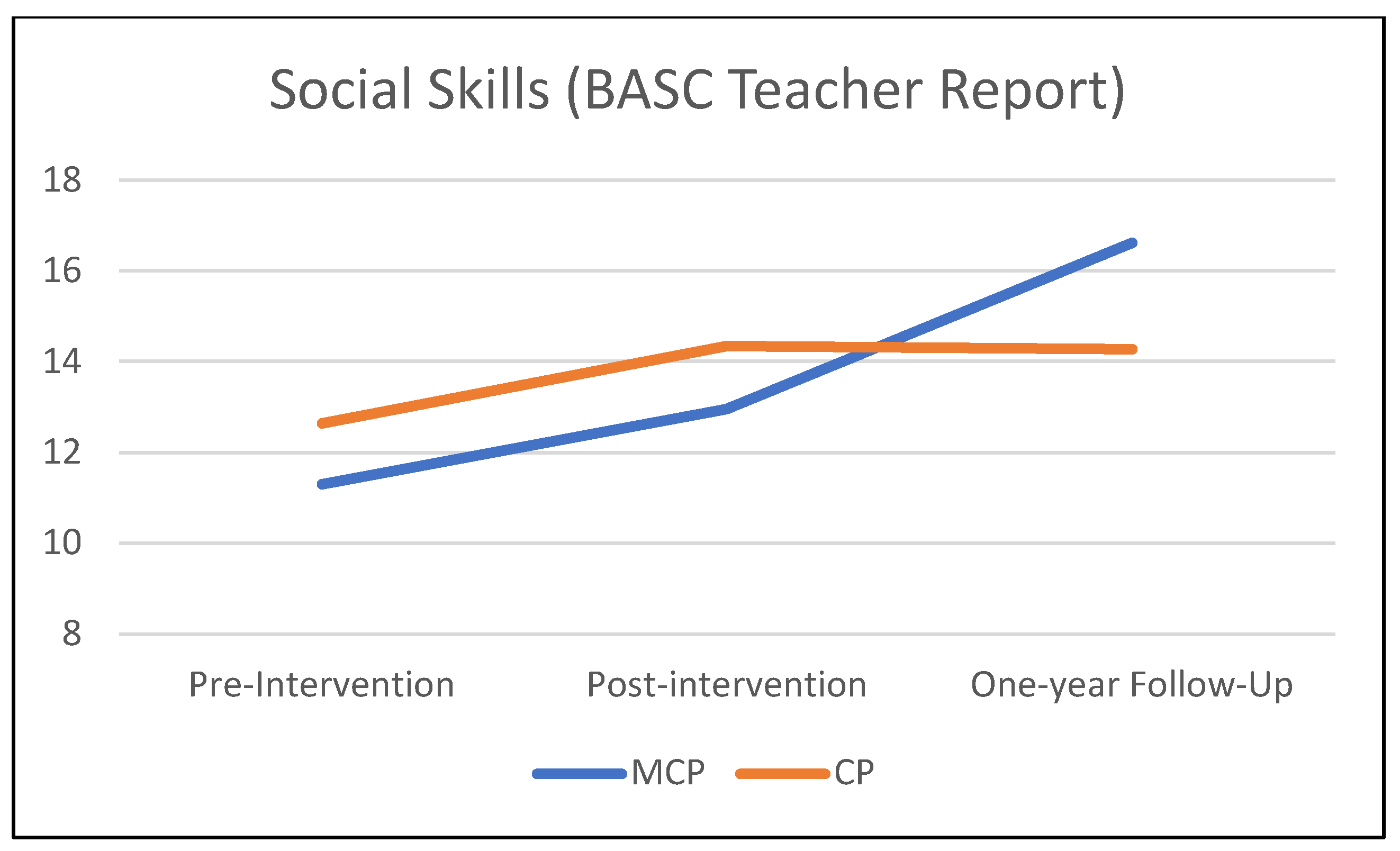
| Social Skills | 37 | 12.65 | 6.45 | 14.27 | 7.09 | 43 | 11.30 | 6.45 | 16.63 | 8.01 | 0.57 |
| Externalizing Problems | 37 | 26.86 | 17.75 | 33.59 | 21.47 | 43 | 29.81 | 20.95 | 29.37 | 21.32 | −0.36 |
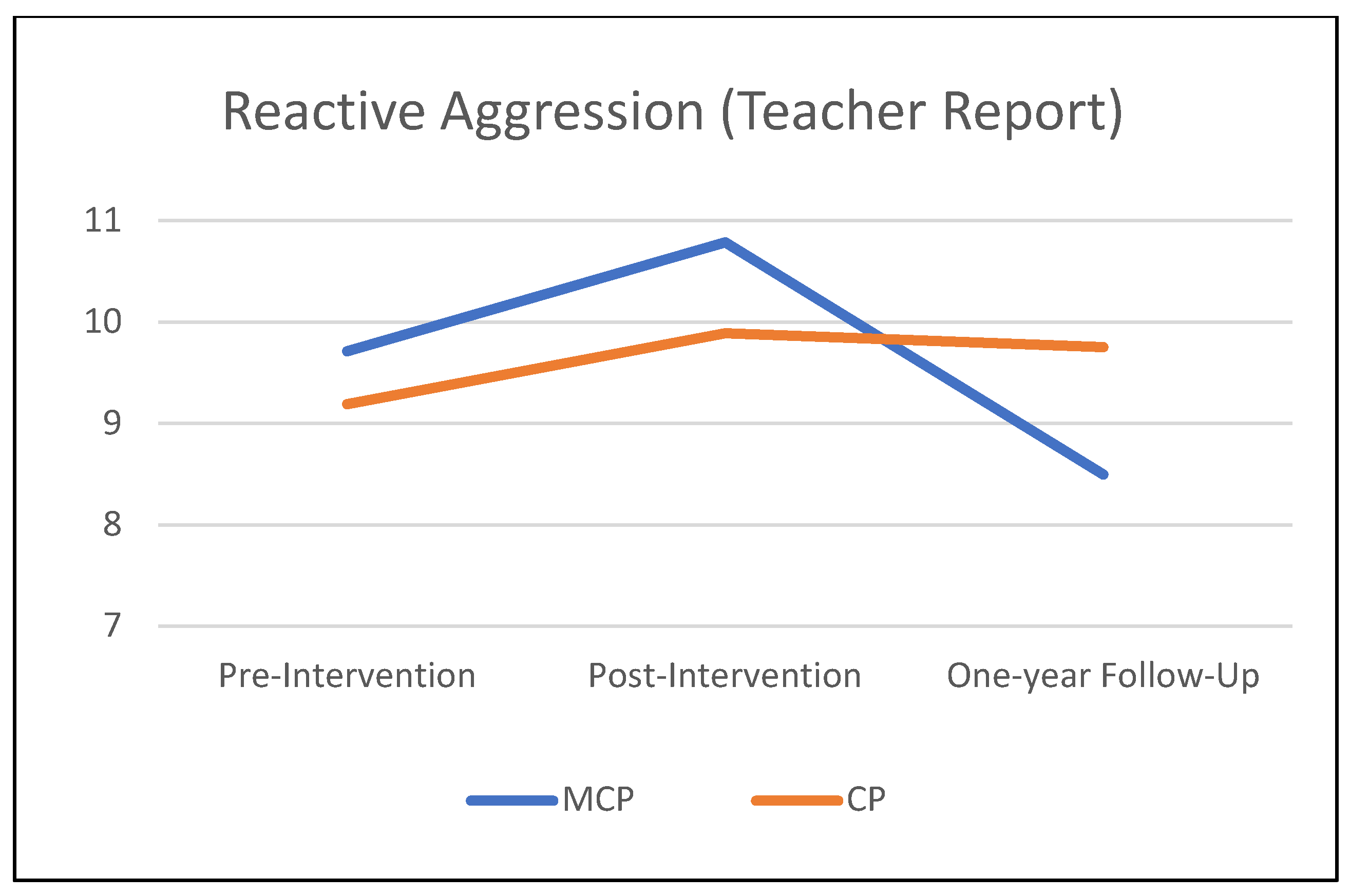
| Reactive Aggression | 36 | 9.19 | 4.04 | 9.75 | 4.26 | 42 | 9.71 | 3.68 | 8.50 | 4.01 | −0.46 |
| Proactive Aggression | 36 | 7.08 | 3.11 | 6.13 | 2.70 | 42 | 7.38 | 3.47 | 5.57 | 2.97 | −0.26 |
| Social Skills (n = 80) | Externalizing (n = 80) | |||||||
| b | se | t-Value | p | b | se | t-Value | p | |
| Condition (MCP vs. CP) | −1.369 | 1.627 | −0.84 | 0.402 | 1.974 | 4.526 | 0.44 | 0.664 |
| Time | 0.705 | 0.555 | 1.27 | 0.208 | 2.926 | 1.410 | 2.07 | 0.041 |
| Time × condition | 1.610 | 0.757 | 2.13 | 0.037 | −3.118 | 1.924 | −1.62 | 0.109 |
| Time slope (CP) | 0.705 | 0.555 | 1.27 | 0.208 | 2.926 | 1.410 | 2.07 | 0.041 |
| Time slope (MCP) | 2.316 | 0.515 | 4.50 | <0.01 | −0.192 | 1.308 | −0.15 | 0.884 |
| Reactive Aggression (n = 78) | Proactive Aggression (n = 78) | |||||||
| b | se | t-value | p | b | se | t-value | p | |
| Condition (MCP vs. CP) | 0.278 | 0.885 | 0.31 | 0.753 | 0.154 | 0.687 | 0.22 | 0.823 |
| Time | 0.242 | 0.293 | 0.83 | 0.412 | −0.411 | 0.261 | −1.57 | 0.120 |
| Time × condition | −0.770 | 0.399 | −1.93 | 0.057 | −0.376 | 0.356 | −1.06 | 0.294 |
| Time slope (CP) | 0.242 | 0.293 | 0.83 | 0.412 | −0.411 | 0.261 | −1.57 | 0.120 |
| Time slope (MCP) | −0.528 | 0.271 | −1.95 | 0.055 | −0.787 | 0.242 | −3.25 | 0.002 |
| CP | MCP | ES | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Intervention | Post-Intervention | Pre-Intervention | Post-Intervention | ||||||||
| n | Mean | S.D. | Mean | S.D. | n | Mean | S.D. | Mean | S.D. | ||
| SCL Reactivity | 17 | 3.20 | 3.10 | 0.76 | 1.28 | 29 | 2.06 | 3.10 | 1.69 | 2.69 | 0.66 |
| RSA Reactivity | 20 | 0.12 | 1.14 | 0.26 | 0.74 | 25 | 0.23 | 0.60 | 0.15 | 0.45 | −0.25 |
| SCL Reactivity (n = 46) | RSA Reactivity (n = 45) | |||||||
|---|---|---|---|---|---|---|---|---|
| b | se | t-Value | p | b | se | t-Value | p | |
| Condition (MCP vs. CP) | −1.322 | 0.792 | −1.67 | 0.099 | 0.109 | 0.227 | 0.48 | 0.631 |
| Time | −2.333 | 0.792 | −2.95 | 0.005 | 0.166 | 0.222 | 0.75 | 0.459 |
| Time × condition | 2.205 | 0.964 | 2.29 | 0.027 | −0.239 | 0.292 | −0.82 | 0.418 |
| Time slope (CP) | −2.333 | 0.792 | −2.95 | 0.005 | 0.166 | 0.222 | 0.75 | 0.459 |
| Time slope (MCP) | −0.128 | 0.596 | −0.22 | 0.830 | −0.073 | 0.192 | −0.38 | 0.707 |
| Inhibitory Control (Post-Intervention) | Reactive Aggression (1-Year Follow-Up) | |||||||
|---|---|---|---|---|---|---|---|---|
| b | se | t-Value | p | b | se | t-Value | p | |
| Condition (MCP vs. CP) | 0.217 | 0.118 | 1.84 | 0.070 | −1.382 | 0.752 | −1.84 | 0.070 |
| Inhibitory control (baseline) | 0.329 | 0.082 | 4.00 | <0.001 | 0.267 | 0.591 | 0.45 | 0.652 |
| Inhibitory control (post-intervention) | −1.614 | 0.701 | −2.30 | 0.024 | ||||
| Reactive aggression (baseline) | −0.047 | 0.015 | −3.18 | 0.002 | 0.456 | 0.115 | 3.96 | <0.001 |
| b | se | t-Value | p | |
|---|---|---|---|---|
| RSA | 6.605 | 2.183 | 3.03 | <0.01 |
| Reactive aggression | 2.724 | 0.692 | 3.94 | <0.01 |
| Proactive aggression | 0.507 | 0.836 | 0.61 | 0.549 |
| Social skills | −0.183 | 0.290 | −0.63 | 0.533 |
| Time | 3.394 | 1.146 | 2.96 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boxmeyer, C.L.; Stager, C.G.; Miller, S.; Lochman, J.E.; Romero, D.E.; Powell, N.P.; Bui, C.; Qu, L. Mindful Coping Power Effects on Children’s Autonomic Nervous System Functioning and Long-Term Behavioral Outcomes. J. Clin. Med. 2023, 12, 3621. https://doi.org/10.3390/jcm12113621
Boxmeyer CL, Stager CG, Miller S, Lochman JE, Romero DE, Powell NP, Bui C, Qu L. Mindful Coping Power Effects on Children’s Autonomic Nervous System Functioning and Long-Term Behavioral Outcomes. Journal of Clinical Medicine. 2023; 12(11):3621. https://doi.org/10.3390/jcm12113621
Chicago/Turabian StyleBoxmeyer, Caroline L., Catanya G. Stager, Shari Miller, John E. Lochman, Devon E. Romero, Nicole P. Powell, Chuong Bui, and Lixin Qu. 2023. "Mindful Coping Power Effects on Children’s Autonomic Nervous System Functioning and Long-Term Behavioral Outcomes" Journal of Clinical Medicine 12, no. 11: 3621. https://doi.org/10.3390/jcm12113621
APA StyleBoxmeyer, C. L., Stager, C. G., Miller, S., Lochman, J. E., Romero, D. E., Powell, N. P., Bui, C., & Qu, L. (2023). Mindful Coping Power Effects on Children’s Autonomic Nervous System Functioning and Long-Term Behavioral Outcomes. Journal of Clinical Medicine, 12(11), 3621. https://doi.org/10.3390/jcm12113621






