Guided Zygomatic Implantology for Oral Cancer Rehabilitation: A Case Report
Abstract
:1. Introduction
2. CASE Presentation
3. Patient History
3.1. Detailed Medical History
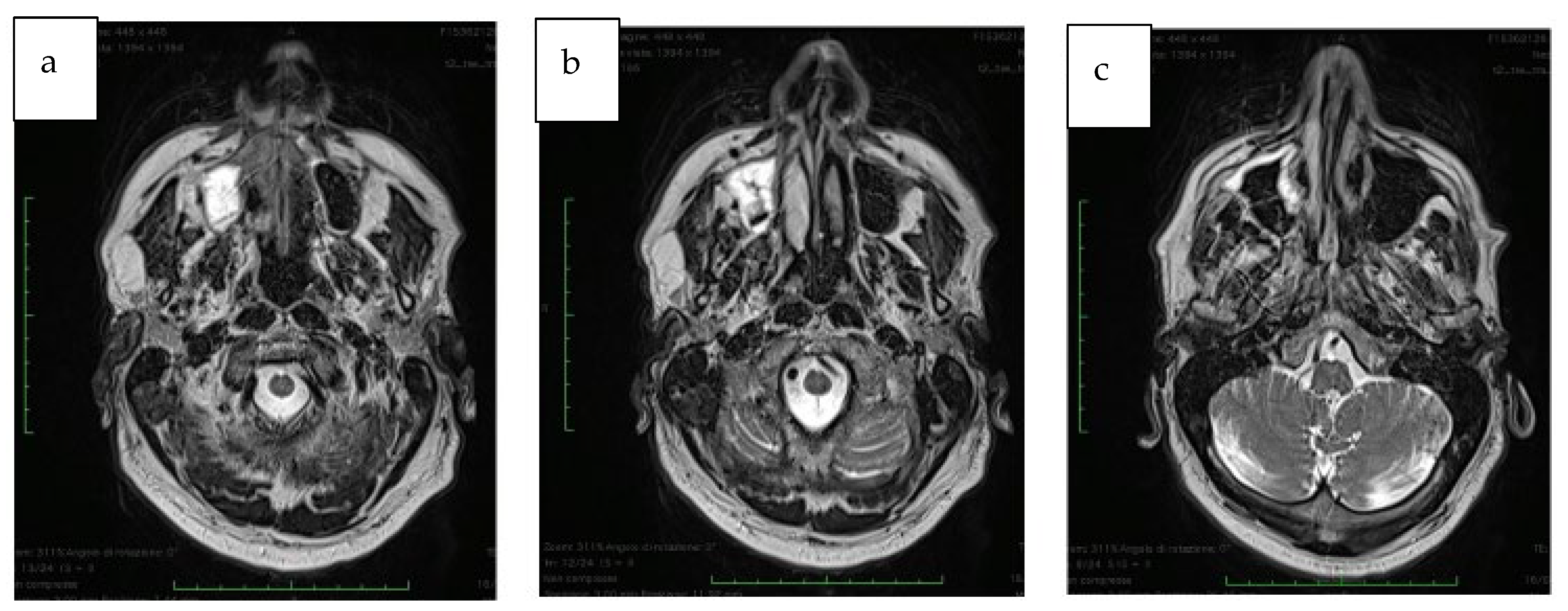
3.2. Preoperative Oral Situation
3.3. Preoperative Protocol
3.4. Preoperative Digital Planning
3.5. Pre-Surgical Medication
4. Surgical Technique
Post-Operative Report
5. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Takushima, A.; Harii, K.; Asato, H.; Momosawa, A.; Okazaki, M.; Nakatsuka, T. Choice of osseous and osteocutaneous flaps for mandibular reconstruction. Int. J. Clin. Oncol. 2005, 10, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Baccarani, A.; De Santis, G. Mandible Reconstruction: A Review Article. J. Surg. 2015, 1, 7. [Google Scholar]
- Piazza, C.; Paderno, A.; Del Bon, F.; Taglietti, V.; Grammatica, A.; Montalto, N.; Nicolai, P. Palato-maxillary reconstruction by the angular branch-based tip of scapula free flap. Eur. Arch. Otorhinolaryngol. 2017, 274, 939–945. [Google Scholar] [CrossRef]
- Okay, D.J.; Genden, E.; Buchbinder, D.; Urken, M. Prosthodontic guidelines for surgical reconstruction of the maxilla: A classification system of defects. J. Prosthet. Dent. 2001, 86, 352–363. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.; Shaw, R.J. Reconstruction of the maxilla and midface: Introducing a new classification. Lancet Oncol. 2010, 11, 1001–1008. [Google Scholar] [CrossRef]
- Kessler, P.; Poort, L.; Böckmann, R.; Lethaus, B. Definition of quality indicators in microsurgery in head and neck reconstruction based on a 5-year follow-up without a loss. J. Craniomaxillofac. Surg. 2013, 41, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Copelli, C.; Bianchi, B.; Ferri, A.; Poli, T.; Ferri, T.; Gallesi, P.; Sesenna, E.; Brevi, B.C. Rehabilitation with endosseous implants in fibula free-flap mandibular reconstruction: A case series of up to 10 years. J. Craniomaxillofac. Surg. 2013, 41, 172–178. [Google Scholar] [CrossRef]
- Gerressen, M.; Pastaschek, C.I.; Riediger, D.; Hilgers, R.D.; Hölzle, F.; Noroozi, N.; Ghassemi, A. Microsurgical free flap reconstructions of head and neck region in 406 cases: A 13-year experience. J. Oral Maxillofac. Surg. 2013, 71, 628–635. [Google Scholar] [CrossRef]
- Pellegrino, G.; Tarsitano, A.; Ferri, A.; Corinaldesi, G.; Bianchi, A.; Marchetti, C. Long-term results of osseointegrated implant-based dental rehabilitation in oncology patients reconstructed with a fibula free flap. Clin. Implant. Dent. Relat. Res. 2018, 20, 852–859. [Google Scholar] [CrossRef]
- Seikaly, H.; Idris, S.; Chuka, R.; Jeffery, C.; Dzioba, A.; Makki, F.; Logan, H.; O’Connell, D.A.; Harris, J.; Ansari, K.; et al. The Alberta Reconstructive Technique: An Occlusion-Driven and Digitally Based Jaw Reconstruction. Laryngoscope 2019, 129 (Suppl. S4), S1–S14. [Google Scholar] [CrossRef]
- Lodders, J.N.; Leusink, F.K.J.; Ridwan-Pramana, A.; Winters, H.A.H.; Karagozoglu, H.K.; Dekker, H.; Tymour Forouzanfar, T.; Schulten, E.A.J.M. Long-term outcomes of implant-based dental rehabilitation in head and neck cancer patients after reconstruction with the free vascularized fibula flap. J. Craniomaxillofac. Surg. 2021, 49, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.N.; Adatia, A.; Hackett, S.; Boscarino, A.; Patel, A.; Lowe, D.; Butterworth, C.J. Changing trends in the microvascular reconstruction and oral rehabilitation following maxillary cancer. Eur. Arch. Otorhinolaryngol. 2022, 279, 4113–4126. [Google Scholar] [CrossRef] [PubMed]
- Ohrnell, L.O.; Hirsch, J.M.; Ericsson, I.; Brånemark, P.I. Single-tooth rehabilitation using osseointegration. A modified surgical and prosthodontic approach. Quintessence Int. 1988, 19, 871–876. [Google Scholar] [PubMed]
- Rosenstein, J.; Dym, H. Zygomatic Implants: A Solution for the Atrophic Maxilla: 2021 Update. Dent. Clin. N. Am. 2021, 65, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Varghese, K.G.; Gandhi, N.; Kurian, N.; Daniel, A.Y.; Dhawan, K.; Joseph, M.; Varghese, M.G. Rehabilitation of the severely resorbed maxilla by using quad zygomatic implant-supported prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, in press. [Google Scholar] [CrossRef]
- Andre, A.; Dym, H. Zygomatic Implants: A Review of a Treatment Alternative for the Severely Atrophic Maxilla. Atlas. Oral Maxillofac. Surg. Clin. N. Am. 2021, 29, 163–172. [Google Scholar] [CrossRef]
- Di Cosola, M.; Ballini, A.; Zhurakivska, K.; Ceccarello, A.; Nocini, R.; Malcangi, A.; Mori, G.; Lo Muzio, L.; Cantore, S.; Olivo, A. Retrospective Analysis of Clinical and Radiologic Data Regarding Zygomatic Implant Rehabilitation with a Long-Term Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 12963. [Google Scholar] [CrossRef]
- Boyes-Varley, J.G.; Howes, D.G.; Davidge-Pitts, K.D.; Brånemark, I.; McAlpine, J.A. A protocol for maxillary reconstruction following oncology resection using zygomatic implants. Int. J. Prosthodont. 2007, 20, 521–531. [Google Scholar]
- Hackett, S.; El-Wazani, B.; Butterworth, C. Zygomatic implant-based rehabilitation for patients with maxillary and mid-facial oncology defects: A review. Oral Dis. 2021, 27, 27–41. [Google Scholar] [CrossRef]
- Sales, P.H.; Gomes, M.V.; Oliveira-Neto, O.B.; de Lima, F.J.; Leão, J.C. Quality assessment of systematic reviews regarding the effectiveness of zygomatic implants: An overview of systematic reviews. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e541–e548. [Google Scholar] [CrossRef]
- Butterworth, C.J.; Rogers, S.N. The zygomatic implant perforated (ZIP) flap: A new technique for combined surgical reconstruction and rapid fixed dental rehabilitation following low-level maxillectomy. Int. J. Implant. Dent. 2017, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Salvatori, P.; Mincione, A.; Rizzi, L.; Costantini, F.; Bianchi, A.; Grecchi, E.; Garagiola, U.; Grecchi, F. Maxillary resection for cancer, zygomatic implants insertion, and palatal repair as single-stage procedure: Report of three cases. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 13. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, C.J. Primary vs secondary zygomatic implant placement in patients with head and neck cancer-A 10-year prospective study. Head Neck 2019, 41, 1687–1695. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, C.J.; Lowe, D.; Rogers, S.N. The Zygomatic Implant Perforated (ZIP) flap reconstructive technique for the management of low-level maxillary malignancy—Clinical & patient related outcomes on 35 consecutively treated patients. Head Neck 2022, 44, 345–358. [Google Scholar] [CrossRef]
- Grecchi, E.; Stefanelli, L.V.; Grecchi, F.; Grivetto, F.; Franchina, A.; Pranno, N. A novel guided zygomatic implant surgery system compared to free hand: A human cadaver study on accuracy. J. Dent. 2022, 119, 103942. [Google Scholar] [CrossRef] [PubMed]
- Grecchi, F.; Stefanelli, L.V.; Grivetto, F.; Grecchi, E.; Siev, R.; Mazor, Z.; Del Fabbro, M.; Pranno, N.; Franchina, A.; Di Lucia, V.; et al. A Novel Guided Zygomatic and Pterygoid Implant Surgery System: A Human Cadaver Study on Accuracy. Int. J. Environ. Res. Public Health 2021, 18, 6142. [Google Scholar] [CrossRef] [PubMed]
- Landes, C.A.; Paffrath, C.; Koehler, C.; Thai, V.D.; Stübinger, S.; Sader, R.; Lauer, H.C.; Piwowarczyk, A. Zygoma implants for midfacial prosthetic rehabilitation using telescopes: 9-year follow-up. Int. J. Prosthodont. 2009, 22, 20–32. [Google Scholar]
- Yeung, R.W.; Samman, N.; Cheung, L.K.; Zhang, C.; Chow, R.L. Stereomodel-assisted fibula flap harvest and mandibular reconstruction. J. Oral Maxillofac. Surg. 2007, 65, 1128–1134. [Google Scholar] [CrossRef]
- Goker, F.; Baj, A.; Bolzoni, A.R.; Maiorana, C.; Giannì, A.B.; Del Fabbro, M. Dental implant-based oral rehabilitation in patients reconstructed with free fibula flaps: Clinical study with a follow-up 3 to 6 years. Clin. Implant. Dent. Relat. Res. 2020, 22, 514–522. [Google Scholar] [CrossRef]
- Ferri, A.; Varazzani, A.; Bolzoni, A.R.; Monaca, M.D.; Tarabbia, F.; Tarsitano, A.; Zavattero, E.; Gessaroli, M.; Copelli, C.; De Riu, G.; et al. A multicenter survey on computer-aided design and computer-aided manufacturing mandibular reconstruction from Italian community. Microsurgery 2019, 39, 673–674. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 416–435. [Google Scholar] [CrossRef] [PubMed]
- Vercruyssen, M.; Hultin, M.; Van Assche, N.; Svensson, K.; Naert, I.; Quirynen, M. Guided surgery: Accuracy and efficacy. Periodontology 2000 2014, 66, 228–246. [Google Scholar] [CrossRef] [PubMed]
- Rivara, F.; Lumetti, S.; Calciolari, E.; Toffoli, A.; Forlani, G.; Manfredi, E. Photogrammetric method to measure the discrepancy between clinical and software-designed positions of implants. J. Prosthet. Dent. 2016, 115, 703–711. [Google Scholar] [CrossRef]
- Weijs, W.L.; Coppen, C.; Schreurs, R.; Vreeken, R.D.; Verhulst, A.C.; Merkx, M.A.; Bergé, S.J.; Maal, T.J. Accuracy of virtually 3D planned resection templates in mandibular reconstruction. J. Craniomaxillofac. Surg. 2016, 44, 1828–1832. [Google Scholar] [CrossRef]
- Pellegrino, G.; Tarsitano, A.; Basile, F.; Pizzigallo, A.; Marchetti, C. Computer-Aided Rehabilitation of Maxillary Oncological Defects Using Zygomatic Implants: A Defect-Based Classification. Oral Maxillofac. Surg. 2015, 73, 2446.e1–2446.e11. [Google Scholar] [CrossRef]
- Ozaki, H.; Sakurai, H.; Yoshida, Y.; Yamanouchi, H.; Iino, M. Oral Rehabilitation of Oral Cancer Patients Using Zygomatic Implant-Supported Maxillary Prostheses with Magnetic Attachment: Three Case Reports. Case Rep. Dent. 2018, 2018, 1694063. [Google Scholar] [CrossRef] [PubMed]
- Urken, M.L.; Roche, A.M.; Kiplagat, K.J.; Dewey, E.H.; Lazarus, C.; Likhterov, I.; Buchbinder, D.; Okay, D.J. Comprehensive approach to functional palatomaxillary reconstruction using regional and free tissue transfer: Report of reconstructive and prosthodontic outcomes of 140 patients. Head Neck 2018, 40, 1639–1666. [Google Scholar] [CrossRef]
- Van der Sloot, P.G. Hard and soft palate reconstruction. Curr. Opin. Otolaryngol. Head Neck Surg. 2003, 11, 225–229. [Google Scholar] [CrossRef]
- Shrime, M.G.; Gilbert, R.W. Reconstruction of the midface and maxilla. Facial Plast. Surg. Clin. N. Am. 2009, 17, 211–223. [Google Scholar] [CrossRef]
- Schmidt, B.L.; Pogrel, M.A.; Young, C.W.; Sharma, A. Reconstruction of extensive maxillary defects using zygomaticus implants. J. Oral Maxillofac. Surg. 2004, 62, 82–89. [Google Scholar] [CrossRef]
- Barraclough, O.; Patel, J.; Milne, S.; Ho, M.W.; Ali, Z. Pathways for the rehabilitation of resection defects in the maxilla. Br. Dent. J. 2022, 232, 783–789. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Hafliger, J.; Seto, I.; Rahal, A.; Mericske-Stern, R.; Smolka, K. Oral rehabilitation after mandibular reconstruction using an osteocutaneous fibula free flap with endosseous implants: Factors affecting the functional outcome in patients with oral cancer. Clin. Oral Implant. Res. 2005, 16, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Smolka, K.; Kraehenbuehl, M.; Eggensperger, N.; Hallermann, W.; Thoren, H.; Iizuka, T.; Smolka, W. Fibula free flap reconstruction of the mandible in cancer patients: Evaluation of a combined surgical and prosthodontic treatment concept. Oral Oncol. 2008, 44, 571–581. [Google Scholar] [CrossRef]
- Chiapasco, M.; Biglioli, F.; Autelitano, L.; Romeo, E.; Brusati, R. Clinical outcome of dental implants placed in fibula-free flaps used for the reconstruction of maxillo-mandibular defects following ablation for tumors or osteoradionecrosis. Clin. Oral Implant. Res. 2006, 17, 220–228. [Google Scholar] [CrossRef] [PubMed]
- Garrett, N.; Roumanas, E.D.; Blackwell, K.E.; Freymiller, E.; Abemayor, E.; Wong, W.K.; Gerratt, B.; Berke, G.; Beumer, J.; Kapur, K.K. Efficacy of conventional and implant-supported mandibular resection prostheses: Study overview and treatment outcomes. J. Prosthet. Dent. 2006, 96, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, S.; Ujigawa, K.; Kizu, Y.; Tonogi, M.; Yamane, G.Y. Biomechanical three-dimensional finite-element analysis of maxillary prostheses with implants. Design of number and position of implants for maxillary prostheses after hemimaxillectomy. Int. J. Oral Maxillofac. Surg. 2010, 39, 1120–1126. [Google Scholar] [CrossRef]
- Vosselman, N.; Glas, H.H.; Merema, B.J.; Kraeima, J.; Reintsema, H.; Raghoebar, G.M.; Witjes, M.; de Visscher, S. Three-Dimensional Guided Zygomatic Implant Placement after Maxillectomy. J. Pers. Med. 2022, 12, 588. [Google Scholar] [CrossRef]
- Ishak, M.I.; Kadir, M.R.; Sulaiman, E.; Kasim, N.H. Finite element analysis of zygomatic implants in intrasinus and extramaxillary approaches for prosthetic rehabilitation in severely atrophic maxillae. Int. J. Oral Maxillofac. Implant. 2013, 28, e151–e160. [Google Scholar] [CrossRef]
- Depprich, R.; Naujoks, C.; Lind, D.; Ommerborn, M.; Meyer, U.; Kübler, N.R.; Handschel, J. Evaluation of the quality of life of patients with maxillofacial defects after prosthodontic therapy with obturator prostheses. Int. J. Oral Maxillofac. Surg. 2011, 40, 71–79. [Google Scholar] [CrossRef]
- Beumer, J.; Marunick, M.T.; Esposito, S.C. Maxillofacial Rehabilitation: Prosthodontic and Surgical Management of Cancer-Related, Acquired, and Congenital Defects of the Head and Neck, 3rd ed.; Quintessence Publishing: New Malden, UK, 2011. [Google Scholar]
- Goiato, M.C.; Pesqueira, A.A.; Ramos da Silva, C.; Gennari Filho, H.; Micheline Dos Santos, D. Patient satisfaction with maxillofacial prosthesis. Literature review. J. Plast. Reconstr. Aesthet. Surg. 2009, 62, 175–180. [Google Scholar] [CrossRef]
- Ali, M.M.; Khalifa, N.; Alhajj, M.N. Quality of life and problems associated with obturators of patients with maxillectomies. Head Face Med. 2018, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Buurman, D.J.M.; Speksnijder, C.M.; Engelen, B.H.B.T.; Kessler, P. Masticatory performance and oral health-related quality of life in edentulous maxillectomy patients: A cross-sectional study to compare implant-supported obturators and conventional obturators. Clin. Oral Implant. Res. 2020, 31, 405–416. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Huang, W.; Zhang, C.; Sun, J.; Qu, X.; Wu, Y. Functional outcome and quality of life after a maxillectomy: A comparison between an implant supported obturator and implant supported fixed prostheses in a free vascularized flap. Clin. Oral Implant. Res. 2017, 28, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Tolman, D.E.; Desjardins, R.P.; Jackson, I.T. Complex craniofacial reconstruction using an implant-supported prosthesis: Case report with long-term follow-up. Int. J. Oral Maxillofac. Implant. 1997, 12, 243–251. [Google Scholar]
- Brånemark, P.I.; Gröndahl, K.; Ohrnell, L.O.; Nilsson, P.; Petruson, B.; Svensson, B.; Engstrand, P.; Nannmark, U. Zygoma fixture in the management of advanced atrophy of the maxilla: Technique and long-term results. Scand J. Plast. Reconstr. Surg. Hand Surg. 2004, 38, 70–85. [Google Scholar] [CrossRef]
- Wang, F.; Monje, A.; Lin, G.H.; Wu, Y.; Monje, F.; Wang, H.L.; Davó, R. Reliability of four zygomatic implant-supported prostheses for the rehabilitation of the atrophic maxilla: A systematic review. Int. J. Oral Maxillofac. Implant. 2015, 30, 293–298. [Google Scholar] [CrossRef]
- Tuminelli, F.J.; Walter, L.R.; Neugarten, J.; Bedrossian, E. Immediate loading of zygomatic implants: A systematic review of implant survival, prosthesis survival and potential complications. Eur. J. Oral Implantol. 2017, 10 (Suppl. S1), 79–87. [Google Scholar]
- Zhang, H.Y.; Shao, Z.; Jia, J.; Liu, B.; Bu, L.L. Analysis of intraoral microvascular anastomosis in maxillofacial defects reconstruction. J. Craniomaxillofac. Surg. 2023, 51, 31–43. [Google Scholar] [CrossRef]
- Shi, Y.; Liu, J.; Du, M.; Zhang, S.; Liu, Y.; Yang, H.; Shi, R.; Guo, Y.; Song, F.; Zhao, Y.; et al. Customized Barrier Membrane (Titanium Alloy, Poly Ether-Ether Ketone and Unsintered Hydroxyapatite/Poly-l-Lactide) for Guided Bone Regeneration. Front. Bioeng. Biotechnol. 2022, 28, 916967. [Google Scholar] [CrossRef]

















Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grecchi, F.; D’Ambrogio, R.G.; Stefanelli, L.V.; Grivetto, F.; Goker, F.; Del Fabbro, M.; Schreiber, A.; Piazza, C.; Salgarello, S.; Dosio, C.; et al. Guided Zygomatic Implantology for Oral Cancer Rehabilitation: A Case Report. J. Clin. Med. 2023, 12, 3653. https://doi.org/10.3390/jcm12113653
Grecchi F, D’Ambrogio RG, Stefanelli LV, Grivetto F, Goker F, Del Fabbro M, Schreiber A, Piazza C, Salgarello S, Dosio C, et al. Guided Zygomatic Implantology for Oral Cancer Rehabilitation: A Case Report. Journal of Clinical Medicine. 2023; 12(11):3653. https://doi.org/10.3390/jcm12113653
Chicago/Turabian StyleGrecchi, Francesco, Roberto Giuseppe D’Ambrogio, Luigi Vito Stefanelli, Fabrizio Grivetto, Funda Goker, Massimo Del Fabbro, Alberto Schreiber, Cesare Piazza, Stefano Salgarello, Camilla Dosio, and et al. 2023. "Guided Zygomatic Implantology for Oral Cancer Rehabilitation: A Case Report" Journal of Clinical Medicine 12, no. 11: 3653. https://doi.org/10.3390/jcm12113653
APA StyleGrecchi, F., D’Ambrogio, R. G., Stefanelli, L. V., Grivetto, F., Goker, F., Del Fabbro, M., Schreiber, A., Piazza, C., Salgarello, S., Dosio, C., & Grecchi, E. (2023). Guided Zygomatic Implantology for Oral Cancer Rehabilitation: A Case Report. Journal of Clinical Medicine, 12(11), 3653. https://doi.org/10.3390/jcm12113653










