Infertility Treatments Resulting in Twin Pregnancy: Does It Increase the Risk for Future Childhood Malignancy †
Abstract
1. Introduction
2. Methods
2.1. Ethical Approval
2.2. Study Population and Data Collection
2.3. Statistical Analysis
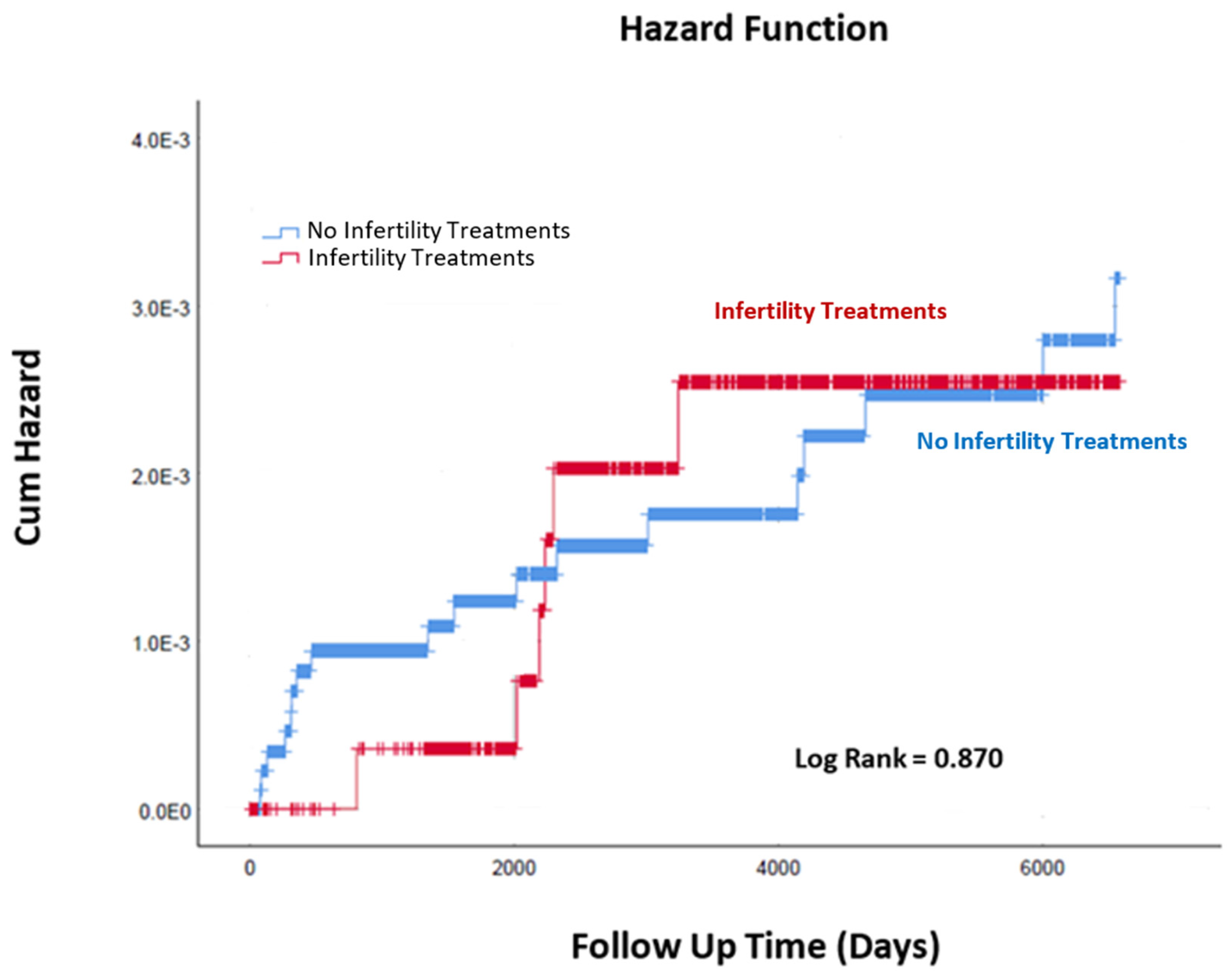
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Adashi, E.Y. Seeing Double: A Nation of Twins from Sea to Shining Sea. Obstet. Anesth. Dig. 2017, 37, 16. [Google Scholar] [CrossRef]
- Fauser, B.C. Towards the global coverage of a unified registry of IVF outcomes. Reprod. Biomed. Online 2019, 38, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Lindheim, S.R.; Glenn, T.L.; Smith, M.C.; Gagneux, P. Ovulation Induction for the General Gynecologist. J. Obstet. Gynecol. India 2018, 68, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Kamphuis, E.I.; Bhattacharya, S.; van der Veen, F.; Mol, B.W.J.; Templeton, A. Are we overusing IVF? BMJ 2014, 348, g252. [Google Scholar] [CrossRef]
- Chen, M.; Heilbronn, L.K. The health outcomes of human offspring conceived by assisted reproductive technologies (ART). J. Dev. Orig. Health Dis. 2017, 8, 388–402. [Google Scholar] [CrossRef]
- McDonald, S.D.; Han, Z.; Mulla, S.; Murphy, K.E.; Beyene, J.; Ohlsson, A. Preterm birth and low birth weight among in vitro fertilization singletons: A systematic review and meta-analyses. Eur. J. Obst. Gynecol. Reprod. Biol. 2009, 146, 138–148. [Google Scholar] [CrossRef]
- Silberstein, T.; Levy, A.; Harlev, A.; Saphier, O.; Sheiner, E. Perinatal outcome of pregnancies following in vitro fertilization and ovulation induction. J. Mater.-Fetal Neonatal Med. 2014, 27, 1316–1319. [Google Scholar] [CrossRef]
- Wen, J.; Jiang, J.; Ding, C.; Dai, J.; Liu, Y.; Xia, Y.; Liu, J.; Hu, Z. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: A meta-analysis. Fertil. Steril. 2012, 97, 1331–1337.e4. [Google Scholar] [CrossRef]
- McDonald, S.D.; Han, Z.; Mulla, S.; Ohlsson, A.; Beyene, J.; Murphy, K.E. Preterm birth and low birth weight among in vitro fertilization twins: A systematic review and meta-analyses. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 148, 105–113. [Google Scholar] [CrossRef]
- Okby, R.; Harlev, A.; Sacks, K.N.; Sergienko, R.; Sheiner, E. Preeclampsia acts differently in in vitro fertilization versus spontaneous twins. Arch. Gynecol. Obstet. 2018, 297, 653–658. [Google Scholar] [CrossRef]
- Hart, R.; Norman, R.J. The longer-term health outcomes for children born as a result of IVF treatment: Part I—General health outcomes. Hum. Reprod. Updat. 2013, 19, 232–243. [Google Scholar] [CrossRef]
- Sullivan-Pyke, C.S.; Senapati, S.; Mainigi, M.A.; Barnhart, K.T. In Vitro fertilization and adverse obstetric and perinatal outcomes. Semin. Perinatol. 2017, 41, 345–353. [Google Scholar] [CrossRef]
- Tsumi, E.; Lavy, Y.; Sheiner, E.; Barrett, C.; Harlev, A.; Hagbi Bal, M.; Wainstock, T. Assisted reproductive technology and long-term ophthalmic morbidity of the offspring. J. Dev. Orig. Health Dis. 2021, 12, 627–631. [Google Scholar] [CrossRef]
- Wainstock, T.; Sheiner, E.; Yoles, I.; Sergienko, R.; Landau, D.; Harlev, A. Fertility treatments and offspring pediatric infectious morbidities: Results of a population-based cohort with a median follow-up of 10 years. Fertil. Steril. 2019, 112, 1129–1135. [Google Scholar] [CrossRef]
- Shachor, N.; Wainstock, T.; Sheiner, E.; Harlev, A. Fertility treatments and gastrointestinal morbidity of the offspring. Early Hum. Dev. 2020, 144, 105021. [Google Scholar] [CrossRef]
- Pinborg, A.; Loft, A.; Romundstad, L.B.; Wennerholm, U.B.; Söderström-Anttila, V.; Bergh, C.; Aittomäki, K. Epigenetics and assisted reproductive technologies. Acta Obstet. Gynecol. Scand. 2016, 95, 10–15. [Google Scholar] [CrossRef]
- Lazaraviciute, G.; Kauser, M.; Bhattacharya, S.; Haggarty, P.; Bhattacharya, S. A systematic review and meta-analysis of DNA methylation levels and imprinting disorders in children conceived by IVF/ICSI compared with children conceived spontaneously. Hum. Reprod. Update 2014, 20, 840–852. [Google Scholar] [CrossRef]
- Tobi, E.W.; Goeman, J.J.; Monajemi, R.; Gu, H.; Putter, H.; Zhang, Y.; Slieker, R.C.; Stok, A.P.; Thijssen, P.E.; Müller, F.; et al. DNA methylation signatures link prenatal famine exposure to growth and metabolism. Nat. Commun. 2014, 5, 5592. [Google Scholar] [CrossRef]
- Neelanjana, M.; Sabaratnam, A. Malignant Conditions in Children Born After Assisted Reproductive Technology. Obstet. Gynecol. Surv. 2008, 63, 669–676. [Google Scholar] [CrossRef]
- Lim, D.H.K.; Maher, E.R. Genomic Imprinting Syndromes and Cancer. Adv. Genet. 2010, 70, 145–175. [Google Scholar]
- Källén, B.; Finnström, O.; Lindam, A.; Nilsson, E.; Nygren, K.G.; Olausson, P.O. Cancer Risk in Children and Young Adults Conceived by In Vitro Fertilization. Pediatrics 2010, 126, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Tournaire, M.; Devouche, E.; Espié, M.; Asselain, B.; Levadou, A.; Cabau, A.; Dunbavand, A.; Grosclaude, P.; Epelboin, S. Cancer Risk in Women Exposed to Diethylstilbestrol in Utero. Therapies 2015, 70, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, L.S.; Fenton, S.E. Cancer and developmental exposure to endocrine disruptors. Environ. Health Perspect. 2003, 111, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Wainstock, T.; Walfisch, A.; Shoham-Vardi, I.; Segal, I.; Harlev, A.; Sergienko, R.; Landau, D.; Sheiner, E. Fertility treatments and pediatric neoplasms of the offspring: Results of a population-based cohort with a median follow-up of 10 years. Am. J. Obstet. Gynecol. 2017, 216, 314.e1–314.e14. [Google Scholar] [CrossRef] [PubMed]
- Weng, S.S.; Huang, Y.T.; Huang, Y.T.; Li, Y.P.; Chien, L.Y. Assisted Reproductive Technology and Risk of Childhood Cancers. JAMA Netw. Open 2022, 5, e2230157. [Google Scholar] [CrossRef]
- Bal, M.H.; Harlev, A.; Sergienko, R.; Levitas, E.; Har-Vardi, I.; Zeadna, A.; Mark-Reich, A.; Becker, H.; Ben-David, N.; Naggan, L.; et al. Possible association between in vitro fertilization technologies and offspring neoplasm. Fertil. Steril. 2021, 116, 105–113. [Google Scholar] [CrossRef]
- Klip, H.; Burger, C.W.; de Kraker, J.; van Leeuwen, F.E.; on behalf of the OMEGA-project group. Risk of cancer in the offspring of women who underwent ovarian stimulation for IVF. Hum. Reprod. 2001, 16, 2451–2458. [Google Scholar] [CrossRef]
- Gilboa, D.; Koren, G.; Barer, Y.; Katz, R.; Rotem, R.; Lunenfeld, E.; Shalev, V. Assisted reproductive technology and the risk of pediatric cancer: A population based study and a systematic review and meta analysis. Cancer Epidemiol. 2019, 63, 101613. [Google Scholar] [CrossRef]
- Sundh, K.J.; Henningsen, A.K.A.; Kallen, K.; Bergh, C.; Romundstad, L.B.; Gissler, M.; Pinborg, A.; Skjaerven, R.; Tiitinen, A.; Vassard, D. Cancer in children and young adults born after assisted reproductive technology: A Nordic cohort study from the Committee of Nordic ART and Safety (CoNARTaS). Hum. Reprod. 2014, 29, 2050–2057. [Google Scholar] [CrossRef]
- Puumala, S.E.; Carozza, S.E.; Chow, E.J.; Fox, E.E.; Horel, S.; Johnson, K.J.; McLaughlin, C.; Mueller, B.A.; Reynolds, P.; Von Behern, J. Childhood Cancer among Twins and Higher Order Multiples. Cancer Epidemiol. Biomark. Prev. 2009, 18, 162–168. [Google Scholar] [CrossRef]
- Pinborg, A. IVF/ICSI twin pregnancies: Risks and prevention. Hum. Reprod. Update 2005, 11, 575–593. [Google Scholar] [CrossRef]
- Pinborg, A.; Loft, A.; Andersen, A.N. Neonatal outcome in a Danish national cohort of 8602 children born after in vitro fertilization or intracytoplasmic sperm injection: The role of twin pregnancy: Neonatal outcome in IVF/ICSI twins and singletons. Acta Obstet. Gynecol. Scand. 2004, 83, 1071–1078. [Google Scholar] [CrossRef]
- Sunderam, S.; Kissin, D.M.; Crawford, S.B.; Folger, S.G.; Jamieson, D.J.; Warner, L.; Barfield, W.D. Assisted Reproductive Technology Surveillance—United States, 2014. MMWR Surveill. Summ. 2017, 66, 1–24. [Google Scholar] [CrossRef]
- Spector, L.G.; Brown, M.B.; Wantman, E.; Letterie, G.S.; Toner, J.P.; Doody, K.; Ginsburg, E.; Williams, M.; Koch, L.; Schymura, M.; et al. Association of In Vitro Fertilization with Childhood Cancer in the United States. JAMA Pediatr. 2019, 173, e190392. [Google Scholar] [CrossRef]
- Catford, S.R.; McLachlan, R.I.; O’Bryan, M.K.; Halliday, J.L. Long-term follow-up of intra-cytoplasmic sperm injection-conceived offspring compared with in vitro fertilization-conceived offspring: A systematic review of health outcomes beyond the neonatal period. Andrology 2017, 5, 610–621. [Google Scholar] [CrossRef]
- Rudant, J.; Amigou, A.; Orsi, L.; Althaus, T.; Leverger, G.; Baruchel, A.; Bertrand, Y.; Nelken, B.; Plat, G.; Michel, G.; et al. Fertility treatments, congenital malformations, fetal loss, and childhood acute leukemia: The ESCALE study (SFCE): Maternal and Birth Characteristics and AL. Pediatr. Blood Cancer 2013, 60, 301–308. [Google Scholar] [CrossRef]
| Characteristics | Infertility Treatments * N = 2910 |
No Infertility Treatments N = 9076 | OR | 95% CI | p-Value | |
|---|---|---|---|---|---|---|
| Maternal Age (Years; Mean ± SD) | 30.80 ± 5.33 | 29.36 ± 5.62 | 0.001 | |||
| Gestational Age at delivery (Weeks; Mean ± SD) | 35.07 ± 3.01 | 35.72 ± 2.93 | 0.152 | |||
| Parity | 1 | 56.5% | 21.2% | 0.001 | ||
| 2–4 | 42.3% | 50.4% | ||||
| >5 | 1.20% | 28.4% | ||||
| Smoking during pregnancy | 0.7% | 0.7% | 1.11 | 0.67–1.83 | 0.68 | |
| Obesity during pregnancy | 2.5% | 1.6% | 1.55 | 1.16–2.06 | 0.002 | |
| Preterm delivery | <37 weeks’ gestation | 64.8% | 54.9% | 1.51 | 1.39–1.65 | <0.001 |
| <34 weeks’ gestation | 19.2% | 14.8% | 1.36 | 1.22–1.52 | 0.001> | |
| Childhood Malignancy | Infertility Treatments N = 2910 (per 1000) | No infertility Treatments N = 9076 (per 1000) | OR | 95% CI | p-Value |
|---|---|---|---|---|---|
| Skin | 1(0.3) | 1(0.1) | 3.12 | 0.19–49.89 | 0.4 |
| Vagina vulva | 1(0.3) | 0 | - | - | 0.07 |
| Testis | 1(0.3) | 0 | - | - | 0.07 |
| Kidney | 1(0.3) | 4(0.4) | 0.78 | 0.87–6.97 | 0.82 |
| Ophthalmic | 0 | 1(0.1) | - | - | 0.57 |
| Brain | 1(0.3) | 3(0.3) | 1.04 | 0.11–9.99 | 0.97 |
| Lymphoma | 0 | 3(0.3) | - | - | 0.32 |
| Leukemia | 1(0.3) | 5(0.5) | 0.62 | 0.07–5.34 | 0.66 |
| Secondary | 0 | 1(0.1) | - | - | 0.57 |
| Other | 0 | 2(0.2) | - | - | 0.42 |
| Total | 6(2.0) | 18 (2.0) | 1.04 | 0.41–2.62 | 0.93 |
| Variables | Adjusted HR | 95% CI | p-Value | |
|---|---|---|---|---|
| Min | Max | |||
| Infertility Treatments (Y/N) | 0.826 | 0.491 | 1.389 | 0.472 |
| Mother Age at Birth (years) | 1.011 | 0.973 | 1.051 | 0.571 |
| Gestational Age (Weeks) | 0.876 | 0.818 | 0.939 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shabtai, T.; Sheiner, E.; Wainstock, T.; Raziel, A.; Kessous, R. Infertility Treatments Resulting in Twin Pregnancy: Does It Increase the Risk for Future Childhood Malignancy. J. Clin. Med. 2023, 12, 3728. https://doi.org/10.3390/jcm12113728
Shabtai T, Sheiner E, Wainstock T, Raziel A, Kessous R. Infertility Treatments Resulting in Twin Pregnancy: Does It Increase the Risk for Future Childhood Malignancy. Journal of Clinical Medicine. 2023; 12(11):3728. https://doi.org/10.3390/jcm12113728
Chicago/Turabian StyleShabtai, Tal, Eyal Sheiner, Tamar Wainstock, Arie Raziel, and Roy Kessous. 2023. "Infertility Treatments Resulting in Twin Pregnancy: Does It Increase the Risk for Future Childhood Malignancy" Journal of Clinical Medicine 12, no. 11: 3728. https://doi.org/10.3390/jcm12113728
APA StyleShabtai, T., Sheiner, E., Wainstock, T., Raziel, A., & Kessous, R. (2023). Infertility Treatments Resulting in Twin Pregnancy: Does It Increase the Risk for Future Childhood Malignancy. Journal of Clinical Medicine, 12(11), 3728. https://doi.org/10.3390/jcm12113728








