Systemic Anti-Inflammatory Effects of Intravenous Lidocaine in Surgical Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction Process
2.4. Risk of Bias and Certainty Assessment
2.5. Statistical Analysis
3. Results
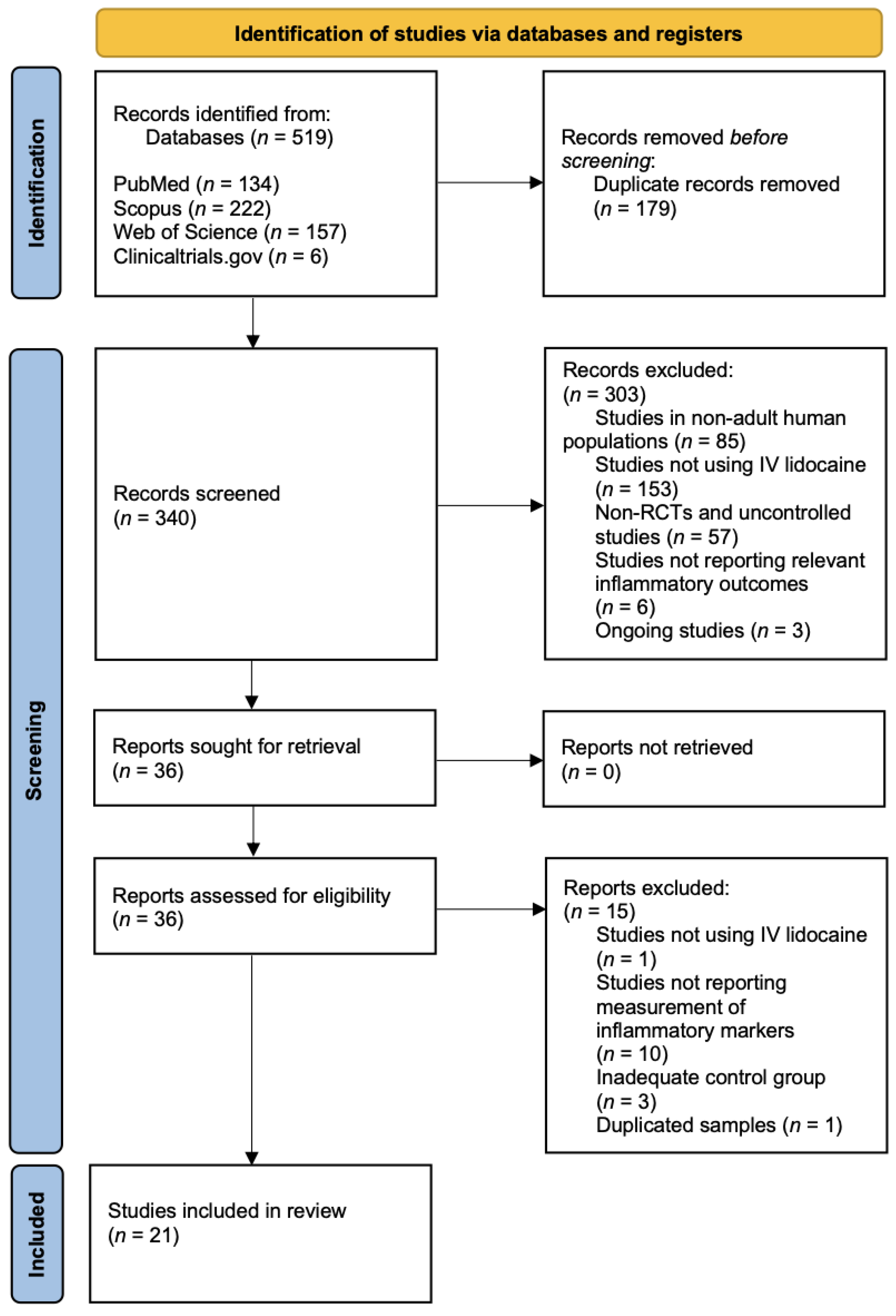
3.1. Selection of Studies
3.2. Study Sample Characteristics
3.3. Surgical Procedures
| Authors | Year | Country | Type of Surgery | ASA Physical Status | Sample Size | Intervention Group | Control Group | Markers Assessed | Time of Assessment | Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|
| Afzal et al. [45] | 2022 | Pakistan | abdominal cholecystectomy | Not reported (NR) | 80 | IV lidocaine bolus (2 mg/kg) followed by continuous infusion (1.5 mg/kg/h) intraoperatively | Treated likewise intervention group with NS | IL-6 and IL-8 | End of surgery, 2 h postoperatively, 6 h postoperatively and 8 h postoperatively | IL-6 and IL-8 levels were significantly lower in IG than in CG |
| Zhao et al. [44] | 2022 | China | supratentorial tumour resection | I, II and III | 60 | IV lidocaine bolus (1.5 mg/kg) before induction of anaesthesia followed by continuous infusion (2 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-6 and TNF-α | Preoperatively and end of surgery | IL-6 and TNF-α levels were significantly lower in IG than in CG |
| Hou et al. [38] | 2021 | China | video-assisted thoracic surgery for non-small-cell lung cancer | I, II and III | 60 | IV lidocaine bolus (1.0 mg/kg) followed by continuous infusion (1.0 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-17 and cortisol | 24 h postoperatively and at the time of post-anaesthesia care unit discharge | IL-17 and cortisol levels were significantly lower in IG than in CG |
| Xu et al. [40] | 2021 | China | laparoscopic hysterectomy | I and II | 80 | IV lidocaine bolus (1.5 mg/kg) 10 min before induction of anaesthesia followed by continuous infusion (1.5 mg/kg/h) until 30 min before the end of the surgery | Treated likewise intervention group with NS | IL-1, IL-6 and TNF-α | Baseline, end of surgery, 2 h postoperatively and 24 h postoperatively | IL-1, IL-6 and TNF-α levels were not significantly lower in IG than in CG |
| van den Heuvel et al. [34] | 2020 | Netherlands | lumpectomy | I and II | 16 | IV lidocaine bolus (1.5 mg/kg) 10 min before induction of anaesthesia followed by continuous infusion (2 mg/kg/h) until 1 h postoperatively | Treated likewise intervention group with NS | IL-1β, IL-1Ra, IL-6 and IL-10 | Before surgery and 4 h postoperatively | IL-1β, IL-1Ra, IL-6 and IL-10 levels were not significantly lower in IG than in CG |
| Oliveira et al. [53] | 2020 | Brazil | laparoscopic gastroplasty | II and III | 58 | IV lidocaine bolus (1.5 mg/kg) 5 min before induction of anaesthesia followed by continuous infusion (2 mg/kg/h) until the end of the skin suture | Treated likewise intervention group with NS | IL-6 | Before surgery, 1 h and 5 h after the start of the surgery and 24 h postoperatively | IL-6 levels were not significantly lower in IG than in CG |
| Ortiz et al. [51] | 2016 | Brazil | laparoscopic cholecystectomy | I and II | 43 | IV lidocaine bolus (1.5 mg/kg) at the start of the surgery followed by continuous infusion (3 mg/kg/h) until 1 h postoperatively | Treated likewise intervention group with NS | IL-1, IL-6, IL-10, IFN-γ and TNF-α | Before surgery, 1 h and 5 h after the start of the surgery and 24 h postoperatively | IL-1, IL-6 IFN-γ and TNF-α levels were significantly lower in IG than in CG; IL-10 was significantly higher in IG than in CG |
| Wang et al. [39] | 2015 | China | radical hysterectomy | I and II | 30 | Intravenous (IS) lidocaine bolus (1.5 mg/kg) 10 min before induction of anaesthesia followed by continuous infusion (1.5 mg/kg/h) until discharge from the operation room | Treated likewise intervention group with normal saline (NS) | HMGB1, IFN-γ and IL-4 | Before surgery and 48 h postoperatively | HMBG1 levels were significantly lower in the intervention group (IG) than in the control group (CG); IFN-γ and IL-4 levels were not significantly lower in IG than in CG |
| Sridhar et al. [35] | 2014 | India | open abdominal surgeries | I, II and III | 134 | IV lidocaine bolus (1.5 mg/kg) at intubation followed by continuous infusion (1.5 mg/kg/h) until 1 h postoperatively | Treated likewise intervention group with NS | CRP and IL-6 | Before surgery, immediately after surgery and 24 h postoperatively | CRP levels were significantly lower in IG than in CG in the immediate postoperative period; IL-6 levels were significantly lower in IG than in CG |
| Wuethrich et al. [52] | 2012 | Switzerland | laparoscopic renal surgery | I, II and III | 64 | IV lidocaine bolus (1.5 mg/kg) during induction of anaesthesia followed by continuous infusion (2 mg/kg/h) until the end of the surgery, followed by continuous infusion (1.3 mg/kg/h) until 24 h postoperatively | Treated likewise intervention group with NS | CRP and cortisol | Before surgery, 24 h postoperatively and 48 h postoperatively | CRP and cortisol levels did not differ significantly between the two groups |
| Elhafz et al. [43] | 2012 | Egypt | laparoscopic colorectal surgery | I, II and III | 18 | IV lidocaine infusion (2 mg/min if BW > 70 kg or 1 mg/min if BW < 70 kg) after induction of anaesthesia | Treated likewise intervention group with NS | IL6, IL8 and TNF-α | Before surgery, 1 h, 24 h and 48 h postoperatively | IL-6, IL-8 and C3a levels were significantly lower in IG than in CG; TNF-α levels were not significantly lower in IG than in IC |
| Yardeni et al. [41] | 2009 | Israel | transabdominal hysterectomy | I and II | 60 | IV lidocaine bolus (2 mg/kg) 20 min before the beginning of the surgery followed by continuous infusion (1.5 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-1RA and IL-6 | Before surgery, 24 h postoperatively, 48 h postoperatively and 72 h postoperatively | IL-6 levels were significantly lower in IG than in CG; IL-1RA levels were not significantly lower in IG than in CG |
| Herroeder et al. [47] | 2007 | Germany | colorectal surgery | I, II and III | 60 | IV lidocaine bolus (1.5 mg/kg) before induction of anaesthesia followed by continuous infusion (2 mg/min) until 4 h postoperatively | Treated likewise intervention group with NS | IL-6, IL-8, IL-1β, TNF-α, IL-1RA, IL-10 | End of surgery, 2 h postoperatively and 24 h postoperatively | IL-6, IL-8 and IL-1RA levels were significantly lower in IG than in CG; TNF-α and IL-10 were not significantly lower in IG than in CG |
| Kuo et al. [46] | 2006 | Taiwan | colonic surgery | I and II | 40 | IV lidocaine bolus (2 mg/kg) for 10 min followed by continuous infusion (3 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-6, IL-8 and IL-1RA | Before surgery, end of surgery, 12 h postoperatively and 24 h postoperatively | IL-6, IL-8 and IL-1ra levels were significantly lower in IG than in CG |
| Hamed et al. [48] | 2022 | Egypt | major abdominal surgery | I and II | 54 | IV lidocaine bolus (1.5 mg/kg) followed by continuous infusion (2 mg/min) until 4 h postoperatively | Treated likewise intervention group with NS | TNF-α and TGF-β | 4 h after recovery from anaesthesia | TNF-α levels were significantly lower in IC than in CG; TGF-β levels were significantly higher in IG than in CG |
| Hassan et al. [49] | 2022 | Egypt | pelvi-abdominal cancer surgery | II and III | 36 | IV lidocaine bolus (1.5 mg/kg) followed by continuous infusion (1.5 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-6 and TNF-α | Before surgery, end of surgery and 24 h postoperatively | IL-6 and TNF-α were significantly lower in IG than in CG |
| Song et al. [50] | 2017 | China | laparoscopic cholecystectomy | I, II and III | 71 | IV lidocaine bolus (1.5 mg/kg) 30 min before the skin incisions followed by a continuous infusion (2 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-1RA, IL-6 and IL-8 | Before surgery, end of surgery and 12 h postoperatively | IL-6 and IL-8 were significantly lower in IG than in CG; IL-1RA was not significantly different between IG and CG |
| Oliveira et al. [37] | 2015 | Brazil | hysterectomy | I and II | 40 | IV lidocaine infusion (2 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-6 | Before surgery, 5 h after the beginning of the surgery and 24 h postoperatively | IL-6 levels were not significantly different between IG and CG |
| Choi et al. [36] | 2016 | South Korea | thyroidectomy | I, II and III | 56 | IV lidocaine bolus (1.5 mg/kg) followed by continuous infusion (2 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | CRP | Before surgery, 2 h postoperatively, 24 h postoperatively and 72 h postoperatively | CRP levels were significantly lower in IG than CG |
| Lv et al. [54] | 2021 | China | laparoscopic radical gastrectomy | I, II and III | 90 | IV lidocaine bolus (1.5 mg/kg) followed by continuous infusion (1.5 mg/kg/h) until the end of the surgery | Treated likewise intervention group with NS | IL-6, IL-10 and TNF-α | Before induction, 2 h after ventilation and at the end of surgery, 24 h postoperatively and 72 h postoperatively | IL-6, IL-10 and TNF-α levels were significantly lower in IG than in CG |
| Yuan et al. [42] | 2019 | China | radical esophagectomy | II and III | 59 | IV lidocaine bolus (1.5 mg/kg) 5 min before induction of anaesthesia followed by continuous infusion (1.5 mg/kg/h) until 1 h postoperatively | Treated likewise intervention group with NS | IL-6 and CRP | Before surgery, admission to the ICU, 12 h postoperatively and 36 h postoperatively | IL-6, IL-10 and TNF-α levels were significantly lower in IG than in CG |
3.4. Study Conduct
3.5. Details of Lidocaine Administration
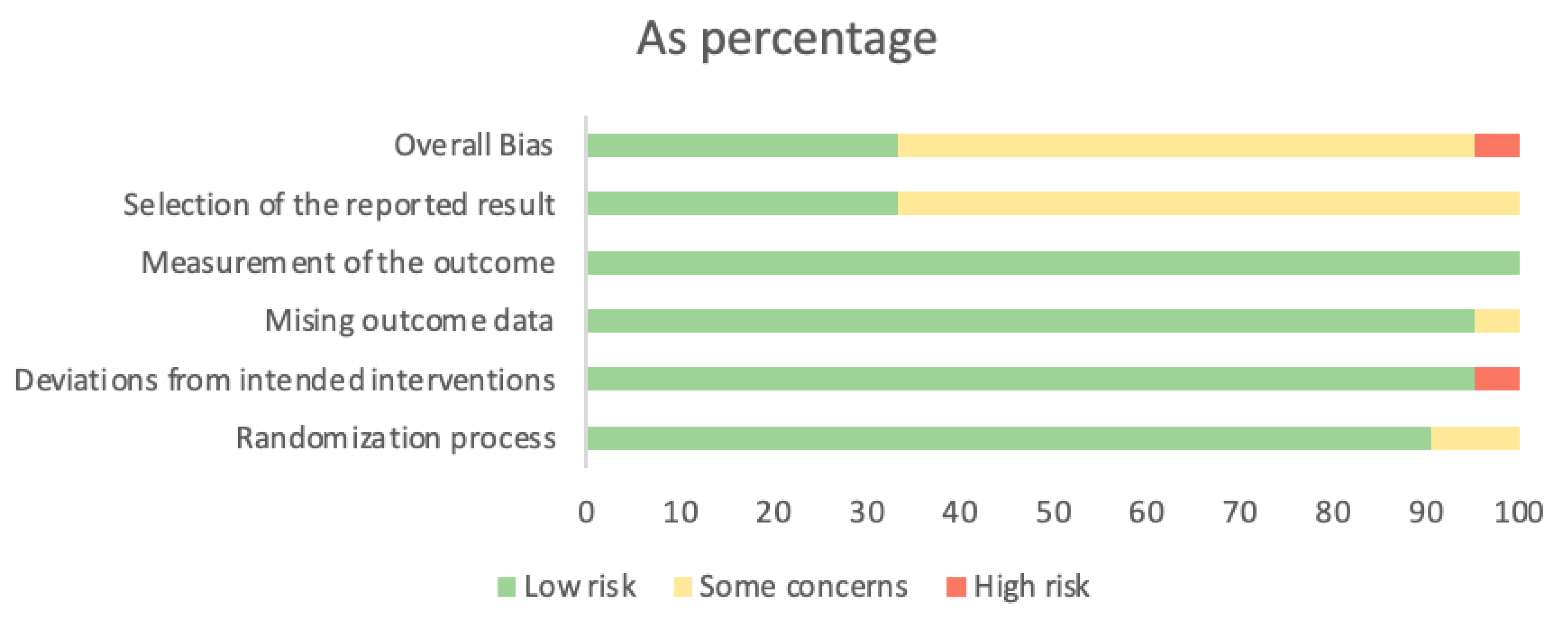
3.6. Risk of Bias
3.7. Outcomes
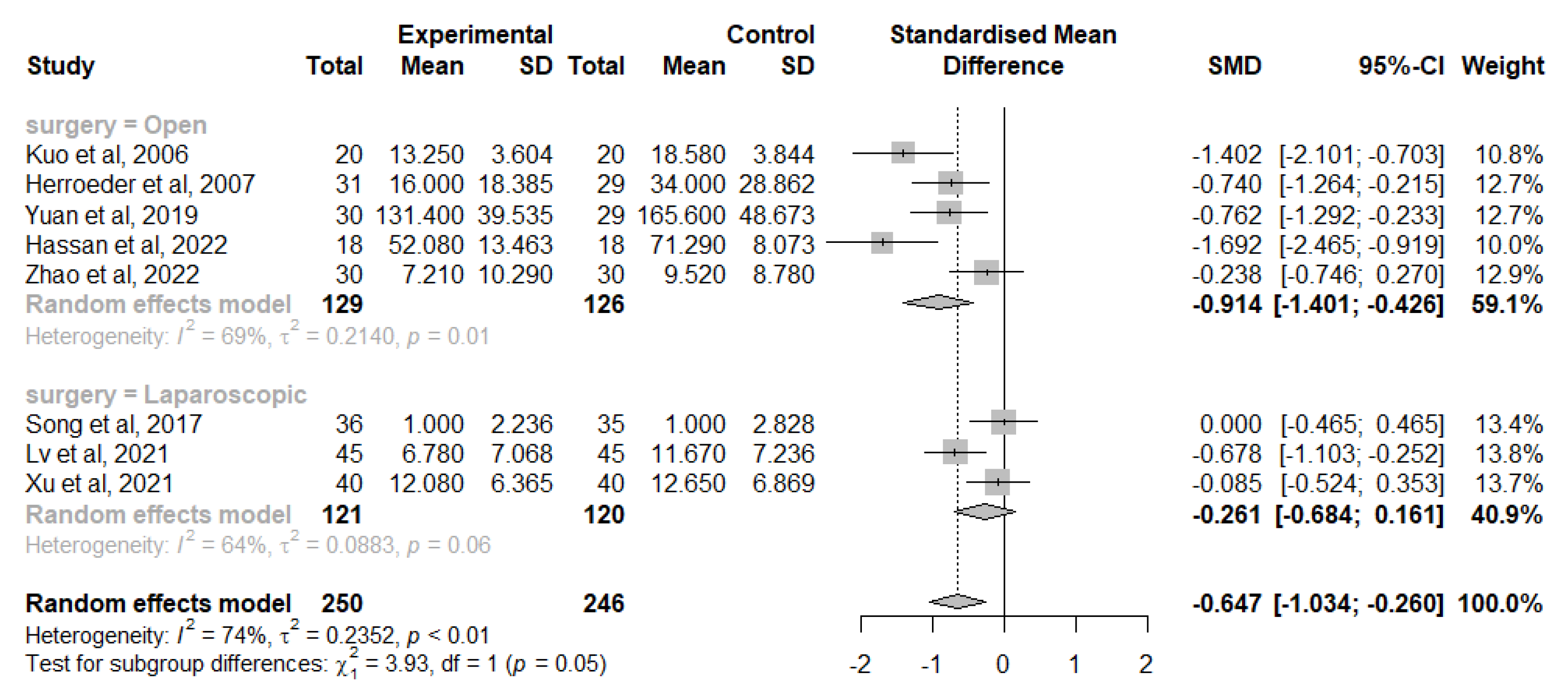
3.7.1. IL-6
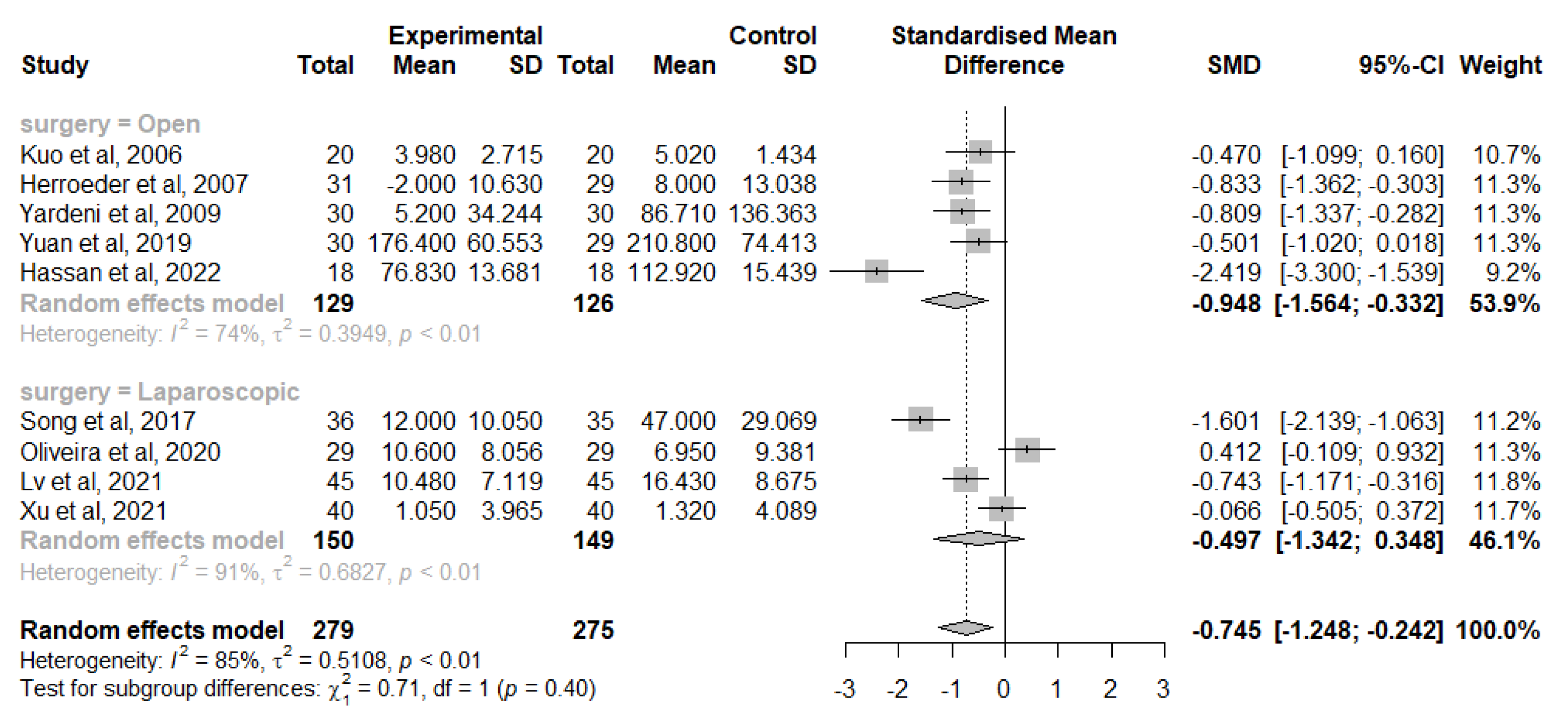
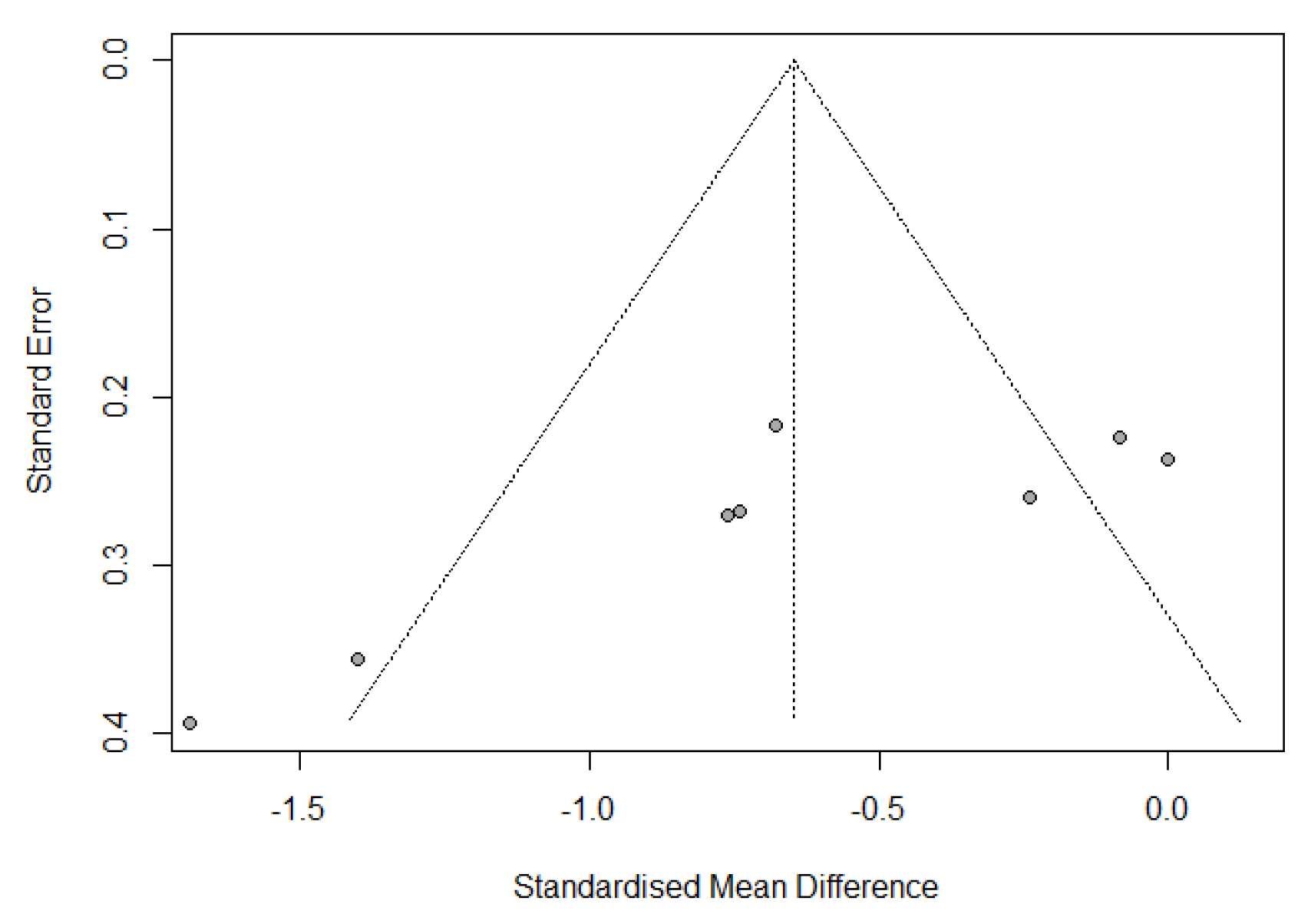
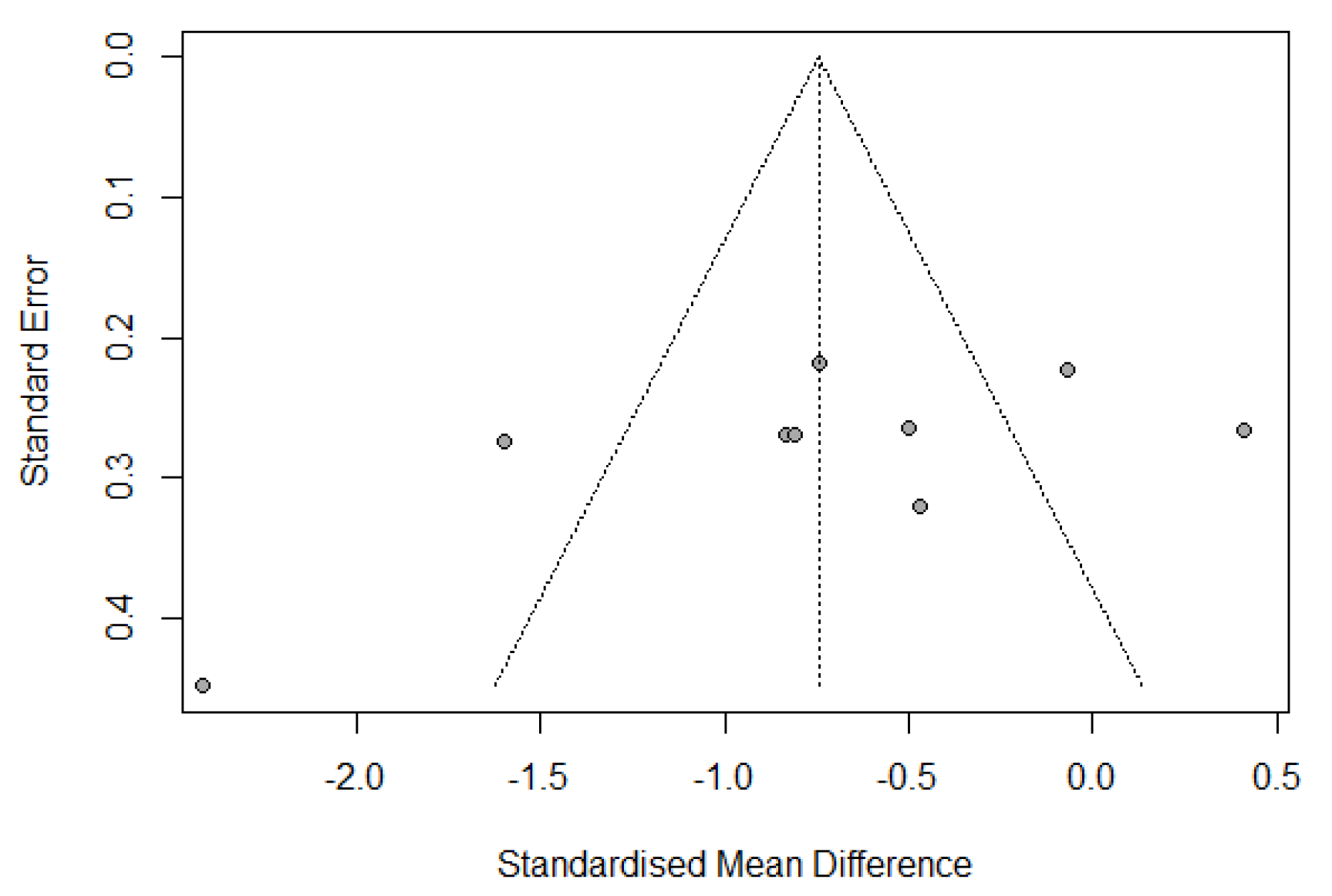
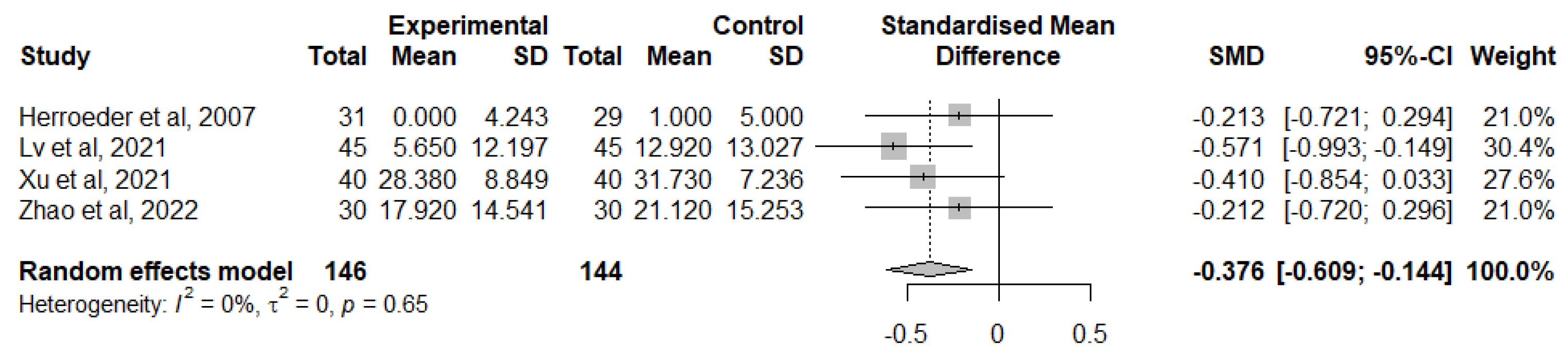
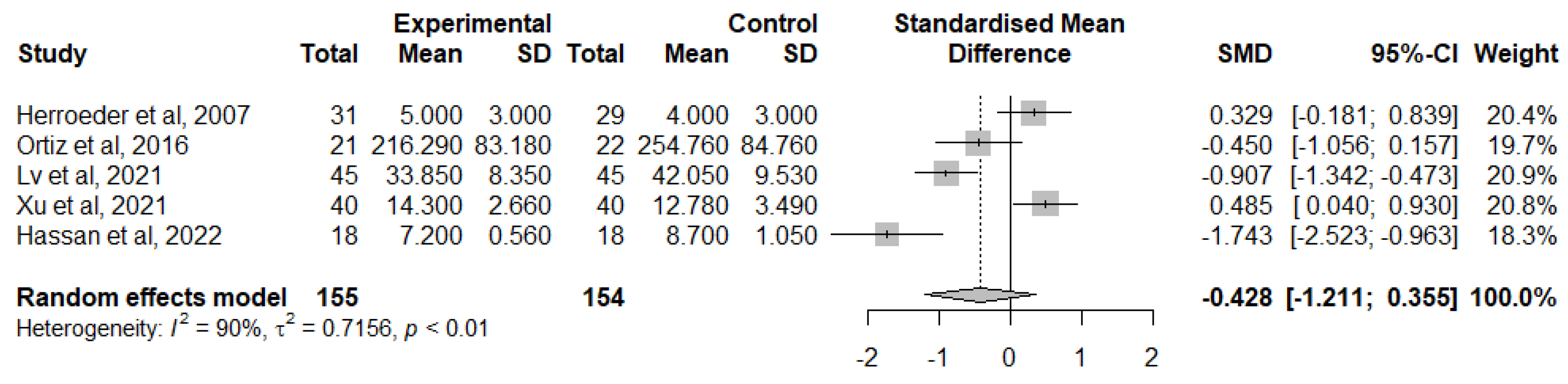
3.7.2. TNF-α
3.7.3. IL-1RA
3.7.4. IL-8
3.7.5. IL-10
3.7.6. CRP
3.7.7. IL-1
3.7.8. IL-1β
3.7.9. IFN-γ
3.7.10. Cortisol
3.7.11. IL-4, IL-17, HMGB1 and TGF-β
3.8. GRADE Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Helander, E.M.; Webb, M.P.; Bias, M.; Whang, E.E.; Kaye, A.D.; Urman, R.D. A Comparison of Multimodal Analgesic Approaches in Institutional Enhanced Recovery after Surgery Protocols for Colorectal Surgery: Pharmacological Agents. J. Laparoendosc. Adv. Surg. Tech. A 2017, 27, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Vigneault, L.; Turgeon, A.F.; Côté, D.; Lauzier, F.; Zarychanski, R.; Moore, L.; McIntyre, L.A.; Nicole, P.C.; Fergusson, D.A. Perioperative intravenous lidocaine infusion for postoperative pain control: A meta-analysis of randomized controlled trials. Can. J. Anaesth. 2011, 58, 22–37. [Google Scholar] [CrossRef]
- Hollmann, M.W.; Strümper, D.; Durieux, M.E. The poor man’s epidural: Systemic local anesthetics for improving postoperative outcomes. Med. Hypotheses 2004, 63, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Van der Wal, S.E.; van den Heuvel, S.A.; Radema, S.A.; van Berkum, B.F.; Vaneker, M.; Steegers, M.A.; Scheffer, G.J.; Vissers, K.C. The in vitro mechanisms and in vivo efficacy of intravenous lidocaine on the neuroinflammatory response in acute and chronic pain. Eur. J. Pain 2016, 20, 655–674. [Google Scholar] [CrossRef]
- Mendonça, F. Systemic Lidocaine for Perioperative Analgesia: A Literature Review. J. Anesth. Intensive Care Med. 2015, 1, 555551. [Google Scholar]
- Daykin, H. The efficacy and safety of intravenous lidocaine for analgesia in the older adult: A literature review. Br. J. Pain 2017, 11, 23–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Wang, G.; Xu, W.; Ding, M.; Yu, W. Efficacy of intravenous lidocaine on pain relief in patients undergoing laparoscopic cholecystectomy: A meta-analysis from randomized controlled trials. Int. J. Surg. 2018, 50, 137–145. [Google Scholar] [CrossRef]
- Rollins, K.E.; Javanmard-Emamghissi, H.; Scott, M.J.; Lobo, D.N. The impact of peri-operative intravenous lidocaine on postoperative outcome after elective colorectal surgery: A meta-analysis of randomised controlled trials. Eur. J. Anaesthesiol. 2020, 37, 659–670. [Google Scholar] [CrossRef]
- Hung, K.C.; Chang, Y.J.; Chen, I.W.; Chang, Y.P.; Chiu, S.F.; Sun, C.K. Efficacy of intraoperative intravenous lidocaine for postoperative analgesia following bariatric surgery: A meta-analysis of randomized controlled studies. Surg. Obes. Relat. Dis. 2022, 18, 135–147. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Supplemental Approval for New Drug Application 018461/S-058. February 2017. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2017/018461Orig1s058ltr.pdf (accessed on 27 January 2023).
- Foo, I.; Macfarlane, A.J.R.; Srivastava, D.; Bhaskar, A.; Barker, H.; Knaggs, R.; Eipe, N.; Smith, A.F. The use of intravenous lidocaine for postoperative pain and recovery: International consensus statement on efficacy and safety. Anaesthesia 2021, 76, 238–250. [Google Scholar] [CrossRef]
- Wright, J.L.; Durieux, M.E.; Groves, D.S. A brief review of innovative uses for local anesthetics. Curr. Opin. Anaesthesiol. 2008, 21, 651–656. [Google Scholar] [CrossRef]
- Beloeil, H.; Mazoit, J.X. Effect of local anesthetics on the postoperative inflammatory response. Ann. Fr. Anesth. Reanim. 2009, 28, 231–237. [Google Scholar] [CrossRef]
- Votta-Velis, E.G.; Piegeler, T.; Minshall, R.D.; Aguirre, J.; Beck-Schimmer, B.; Schwartz, D.E.; Borgeat, A. Regional anaesthesia and cancer metastases: The implication of local anaesthetics. Acta Anaesthesiol. Scand. 2013, 57, 1211–1229. [Google Scholar] [CrossRef]
- Lirk, P.; Fiegl, H.; Weber, N.C.; Hollmann, M.W. Epigenetics in the perioperative period. Br. J. Pharmacol. 2015, 172, 2748–2755. [Google Scholar] [CrossRef] [Green Version]
- Jeon, Y.-T.; Na, H.; Ryu, H.; Chung, Y. Modulation of Dendritic Cell Activation and Subsequent Th1 Cell Polarization by Lidocaine. PLoS ONE 2015, 10, e0139845. [Google Scholar] [CrossRef] [PubMed]
- Cata, J.P.; Lasala, J.; Bugada, D. Best practice in the administration of analgesia in postoncological surgery. Pain Manag. 2015, 5, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Gray, A.; Marrero-Berrios, I.; Ghodbane, M.; Maguire, T.; Weinberg, J.; Manchikalapati, D.; SchianodiCola, J.; Schloss, R.S.; Yarmush, J. Effect of Local Anesthetics on Human Mesenchymal Stromal Cell Secretion. Nano Life 2015, 5, 1550001–1550014. [Google Scholar] [CrossRef] [PubMed]
- Galoș, E.V.; Tat, T.F.; Popa, R.; Efrimescu, C.I.; Finnerty, D.; Buggy, D.J.; Ionescu, D.C.; Mihu, C.M. Neutrophil extracellular trapping and angiogenesis biomarkers after intravenous or inhalation anaesthesia with or without intravenous lidocaine for breast cancer surgery: A prospective, randomised trial. Br. J. Anaesth. 2020, 125, 712–721. [Google Scholar] [CrossRef] [PubMed]
- Wall, T.P.; Buggy, D.J. Perioperative Intravenous Lidocaine and Metastatic Cancer Recurrence—A Narrative Review. Front. Oncol. 2021, 11, 688896. [Google Scholar] [CrossRef]
- Zhang, C.; Xie, C.; Lu, Y. Local Anesthetic Lidocaine and Cancer: Insight into Tumor Progression and Recurrence. Front. Oncol. 2021, 11, 669746. [Google Scholar] [CrossRef]
- Müller, S.D.; Ziegler, J.S.H.; Piegeler, T. Local Anesthetics and Recurrence after Cancer Surgery—What’s New? A Narrative Review. J. Clin. Med. 2021, 10, 719. [Google Scholar] [CrossRef]
- Zi, H.; Chen, L.; Ruan, Q. Lidocaine represses the malignant behavior of lung carcinoma cells via the circ_PDZD8/miR-516b-5p/GOLT1A axis. Histol. Histopathol. 2022, 37, 461–474. [Google Scholar]
- Lee, I.W.; Schraag, S. The Use of Intravenous Lidocaine in Perioperative Medicine: Anaesthetic, Analgesic and Immune-Modulatory Aspects. J. Clin. Med. 2022, 11, 3543. [Google Scholar] [CrossRef]
- Hollmann, M.W.; Durieux, M.E. Local anesthetics and the inflammatory response: A new therapeutic indication? Anesthesiology 2000, 93, 858–875. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, Version 6.3; Updated February 2022; Cochrane: Oxford, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 12 February 2023).
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PlotDigitizer. Available online: https://plotdigitizer.com (accessed on 12 February 2023).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 12 February 2023).
- Richardson, M.; Garner, P.; Donegan, S. Interpretation of subgroup analyses in systematic reviews: A tutorial. Clin. Epidemiol. Glob. Health 2019, 7, 192–198. [Google Scholar] [CrossRef] [Green Version]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Van den Heuvel, S.A.S.; van der Wal, S.E.I.; Bronkhorst, E.M.; Warlé, M.C.; Ronday, M.; Plat, J.; van Alfen, N.; Joosten, L.A.B.; Lerou, J.G.C.; Vissers, K.C.P.; et al. Acute Cytokine Response During Breast Cancer Surgery: Potential Role of Dexamethasone and Lidocaine and Relationship with Postoperative Pain and Complications—Analysis of Three Pooled Pilot Randomized Controlled Trials. J. Pain Res. 2020, 13, 1243–1254. [Google Scholar] [CrossRef]
- Sridhar, P.; Sistla, S.C.; Ali, S.M.; Karthikeyan, V.S.; Badhe, A.S.; Ananthanarayanan, P.H. Effect of intravenous lignocaine on perioperative stress response and post-surgical ileus in elective open abdominal surgeries: A double-blind randomized controlled trial. ANZ J. Surg. 2015, 85, 425–429. [Google Scholar] [CrossRef]
- Choi, G.J.; Kang, H.; Ahn, E.J.; Oh, J.I.; Baek, C.W.; Jung, Y.H.; Kim, J.Y. Clinical Efficacy of Intravenous Lidocaine for Thyroidectomy: A Prospective, Randomized, Double-Blind, Placebo-Controlled Trial. World J. Surg. 2016, 40, 2941–2947. [Google Scholar] [CrossRef]
- De Oliveira, C.M.B.; Sakata, R.K.; Slullitel, A.; Salomao, R.; Lanchote, V.L.; Issy, A.M. Effect of intraoperative intravenous lidocaine on pain and plasma interleukin-6 in patients undergoing hysterectomy. Rev. Bras. Anestesiol. 2015, 65, 92–98. [Google Scholar] [CrossRef] [Green Version]
- Hou, Y.H.; Shi, W.C.; Cai, S.; Liu, H.; Zheng, Z.; Qi, F.W.; Li, C.; Feng, X.M.; Peng, K.; Ji, F.H. Effect of Intravenous Lidocaine on Serum Interleukin-17 after Video-Assisted Thoracic Surgery for Non-Small-Cell Lung Cancer: A Randomized, Double-Blind, Placebo-Controlled Trial. Drug. Des. Dev. Ther. 2021, 15, 3379–3390. [Google Scholar] [CrossRef]
- Wang, H.L.; Yan, H.D.; Liu, Y.Y.; Sun, B.Z.; Huang, R.; Wang, X.S.; Lei, W.F. Intraoperative intravenous lidocaine exerts a protective effect on cell-mediated immunity in patients undergoing radical hysterectomy. Mol. Med. Rep. 2015, 12, 7039–7044. [Google Scholar] [CrossRef] [Green Version]
- Xu, S.; Hu, S.; Ju, X.; Li, Y.; Li, Q.; Wang, S. Effects of intravenous lidocaine, dexmedetomidine, and their combination on IL-1, IL-6 and TNF-α in patients undergoing laparoscopic hysterectomy: A prospective, randomized controlled trial. BMC Anesthesiol. 2021, 21, 3. [Google Scholar] [CrossRef]
- Yardeni, I.Z.; Beilin, B.; Mayburd, E.; Levinson, Y.; Bessler, H. The effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesth. Analg. 2009, 109, 1464–1469. [Google Scholar] [CrossRef] [PubMed]
- Linfang, Y.; Wenjing, Z.; Yue, L.; Bianliang, W.; Yizhou, H. Lung Protective Effect of Perioperative Intravenous Infusion of Lidocaine in Patients after Radical Resection of Esophageal Cancer. Chin. Gen. Pract. 2019, 22, 4465–4470. [Google Scholar] [CrossRef]
- Elhafz, A.A.; Elgebaly, A.S.; Bassuoni, A.S.; El Dabaa, A.A. Is lidocaine patch as effective as intravenous lidocaine in pain and illus reduction after laparoscopic colorectal surgery? A randomized clinical trial. Anesth. Essays Res. 2012, 6, 140–146. [Google Scholar] [CrossRef] [Green Version]
- Zhao, K.; Dong, Y.; Su, G.; Wang, Y.; Ji, T.; Wu, N.; Cui, X.; Li, W.; Yang, Y.; Chen, X. Effect of Systemic Lidocaine on Postoperative Early Recovery Quality in Patients Undergoing Supratentorial Tumor Resection. Drug. Des. Dev. Ther. 2022, 16, 1171–1181. [Google Scholar] [CrossRef]
- Afzal, A.; Syed, A.W.; Mansoor, Q.; Farooqi, R.; Farhat, K.; Khan, A.; Ara, I. Role of lidocaine and its effect on postoperative outcomes in abdominal cholecystectomy. J. Pak. Med. Assoc. 2022, 72, 1048–1052. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.P.; Jao, S.W.; Chen, K.M.; Wong, C.S.; Yeh, C.C.; Sheen, M.J.; Wu, C.T. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br. J. Anaesth. 2006, 97, 640–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herroeder, S.; Pecher, S.; Schönherr, M.E.; Kaulitz, G.; Hahnenkamp, K.; Friess, H.; Böttiger, B.W.; Bauer, H.; Dijkgraaf, M.G.; Durieux, M.E.; et al. Systemic lidocaine shortens length of hospital stay after colorectal surgery: A double-blinded, randomized, placebo-controlled trial. Ann. Surg. 2007, 246, 192–200. [Google Scholar] [CrossRef]
- Hamed, E.; El-Melegy, N.; Ammar, S.; Hamed, R. Effects of Anesthetic Management on Inflammatory Markers in Patients after Major Abdominal Surgeries: A Double-Blind Controlled Study. J. Cell. Mol. Anesth. 2022, 7, 153–159. [Google Scholar] [CrossRef]
- Hassan, M.M.; Saleh, E.G.; Abdalla, N.O.; Radwan, N.H.; Abdelghfar, E.M. Effect of lidocaine infusion compared to dexmedetomidine infusion on proinflammatory cytokines and stress response in pelvi-abdominal cancer a randomized clinical trial. Anaesth. Pain Intensive Care 2022, 26, 44–52. [Google Scholar] [CrossRef]
- Song, X.; Sun, Y.; Zhang, X.; Li, T.; Yang, B. Effect of perioperative intravenous lidocaine infusion on postoperative recovery following laparoscopic Cholecystectomy-A randomized controlled trial. Int. J. Surg. 2017, 45, 8–13. [Google Scholar] [CrossRef]
- Ortiz, M.P.; Godoy, M.C.; Schlosser, R.S.; Ortiz, R.P.; Godoy, J.P.; Santiago, E.S.; Rigo, F.K.; Beck, V.; Duarte, T.; Duarte, M.M.; et al. Effect of endovenous lidocaine on analgesia and serum cytokines: Double-blinded and randomized trial. J. Clin. Anesth. 2016, 35, 70–77. [Google Scholar] [CrossRef]
- Wuethrich, P.Y.; Romero, J.; Burkhard, F.C.; Curatolo, M. No benefit from perioperative intravenous lidocaine in laparoscopic renal surgery: A randomised, placebo-controlled study. Eur. J. Anaesthesiol. 2012, 29, 537–543. [Google Scholar] [CrossRef]
- de Oliveira, C.M.B.; Coelho, L.M.G.; Valadão, J.A.; Moura, E.C.R.; da Silva, A.A.M.; de Lima, R.C.; Brunialti, M.K.C.; Salomão, R.; da Cunha Leal, P.; Sakata, R.K. Assessment of the Effect of Perioperative Venous Lidocaine on the Intensity of Pain and IL-6 Concentration after Laparoscopic Gastroplasty. Obes. Surg. 2020, 30, 3912–3918. [Google Scholar] [CrossRef]
- Lv, X.L.; Li, X.X.; Guo, K.D.; Li, T.; Yang, Y.P.; Lu, W.S.; Wang, S.T.; Liu, S. Effects of Systemic Lidocaine on Postoperative Recovery Quality and Immune Function in Patients Undergoing Laparoscopic Radical Gastrectomy. Drug Des. Dev. Ther. 2021, 15, 1861–1872. [Google Scholar] [CrossRef]
- Hermanns, H.; Hollmann, M.W.; Stevens, M.F.; Lirk, P.; Brandenburger, T.; Piegeler, T.; Werdehausen, R. Molecular mechanisms of action of systemic lidocaine in acute and chronic pain: A narrative review. Br. J. Anaesth. 2019, 123, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Weibel, S.; Jelting, Y.; Pace, N.L.; Helf, A.; Eberhart, L.H.; Hahnenkamp, K.; Hollmann, M.W.; Poepping, D.M.; Schnabel, A.; Kranke, P. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery in adults. Cochrane Database Syst. Rev. 2018, 6, Cd009642. [Google Scholar] [CrossRef] [PubMed]
- Junttila, I.S. Tuning the Cytokine Responses: An Update on Interleukin (IL)-4 and IL-13 Receptor Complexes. Front. Immunol. 2018, 9, 888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akdis, M.; Aab, A.; Altunbulakli, C.; Azkur, K.; Costa, R.A.; Crameri, R.; Duan, S.; Eiwegger, T.; Eljaszewicz, A.; Ferstl, R.; et al. Interleukins (from IL-1 to IL-38), interferons, transforming growth factor β, and TNF-α: Receptors, functions, and roles in diseases. J. Allergy Clin. Immunol. 2016, 138, 984–1010. [Google Scholar] [CrossRef] [Green Version]
- Chen, R.; Kang, R.; Tang, D. The mechanism of HMGB1 secretion and release. Exp. Mol. Med. 2022, 54, 91–102. [Google Scholar] [CrossRef]
- Ricciotti, E.; Fitzgerald, G.A. Prostaglandins and inflammation. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 986–1000. [Google Scholar] [CrossRef]
- Briukhovetska, D.; Dörr, J.; Endres, S.; Libby, P.; Dinarello, C.A.; Kobold, S. Interleukins in cancer: From biology to therapy. Nat. Rev. Cancer 2021, 21, 481–499. [Google Scholar] [CrossRef]
| Outcomes | № of Participants (Studies) | Certainty of the Evidence (GRADE) | Relative Effect (95% CI) | Anticipated Absolute Effects | |
|---|---|---|---|---|---|
| Risk with Control | Risk Difference with Intravenous Lidocaine Infusion | ||||
| change from IL-6 baseline levels at the end of the surgery | 496 (8 RCTs) | Moderate a | - | - | SMD 0.647 SD lower (1.034 lower to 0.26 lower) |
| change from IL-6 baseline levels at 24 h after surgery | 554 (9 RCTs) | Moderate a | - | - | SMD 0.745 SD lower (1.248 lower to 0.242 lower) |
| change from TNF-α baseline levels at the end of the surgery | 290 (4 RCTs) | Moderate b | - | - | SMD 0.376 SD lower (0.609 lower to 0.144 lower) |
| change from TNF-α baseline levels 24 h after surgery | 309 (5 RCTs) | Low a,b | - | - | SMD 0.428 SD lower (1.211 lower to 0.355 higher) |
| IL-1RA levels at 24 h after surgery | 160 (3 RCTs) | Moderate b | - | - | SMD 0.553 SD lower (0.901 lower to 0.205 lower) |
| IL-8 levels at the end of surgery | 171 (3 RCTs) | Low a,b | - | - | SMD 0.792 SD lower (1.6 lower to 0.016 higher) |
| IL-10 levels at the end of surgery | 193 (3 RCTs) | Low a,b | - | - | SMD 0.624 SD lower (1.263 lower to 0.015 higher) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro, I.; Carvalho, P.; Vale, N.; Monjardino, T.; Mourão, J. Systemic Anti-Inflammatory Effects of Intravenous Lidocaine in Surgical Patients: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 3772. https://doi.org/10.3390/jcm12113772
Castro I, Carvalho P, Vale N, Monjardino T, Mourão J. Systemic Anti-Inflammatory Effects of Intravenous Lidocaine in Surgical Patients: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2023; 12(11):3772. https://doi.org/10.3390/jcm12113772
Chicago/Turabian StyleCastro, Irene, Pedro Carvalho, Nuno Vale, Teresa Monjardino, and Joana Mourão. 2023. "Systemic Anti-Inflammatory Effects of Intravenous Lidocaine in Surgical Patients: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 12, no. 11: 3772. https://doi.org/10.3390/jcm12113772
APA StyleCastro, I., Carvalho, P., Vale, N., Monjardino, T., & Mourão, J. (2023). Systemic Anti-Inflammatory Effects of Intravenous Lidocaine in Surgical Patients: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(11), 3772. https://doi.org/10.3390/jcm12113772









