Comprehensive Cardiovascular and Renal Protection in Patients with Type 2 Diabetes
Abstract
1. Introduction
2. Multifactorial Approach to Reduce the Vascular-Renal Risk
2.1. Weight
2.2. Physical Activity
- Intensity level: it should be between 60% and 75% of what is called the cardiac reserve level. The simplest way to calculate exercise intensity is to use the Talking Test. In this case, it is about exercising hard enough that the person has difficulty having a conversation.
- Frequency and progression: the exercise must be carried out continuously. At least five days a week is recommended.
- Duration: A minimum of 30 min a day of moderate aerobic exercise is recommended, performed at least five days a week, or 90 min a week of high intensity exercise.
2.3. Smoking
- Total cessation of tobacco use should be recommended.
- Even if you gain weight, you should insist on cessation of tobacco, since the benefits of quitting smoking are greater [29].
2.4. Lipids
2.5. Blood Pressure
2.6. Glycated Hemoglobin
2.7. Cognitive Impairment
3. Antihyperglycemic Drugs
3.1. Biguanides (Metformin)
3.2. Sulfonylureas
3.3. Glinides
3.4. α-Glucosidase Inhibitors
3.5. Thiazolidinediones or Glitazones
3.6. Inhibitors of the Enzyme Dipeptidyl Peptidase Type 4
3.7. Sodium-Glucose Cotransporter Type 2 Inhibitors
3.8. Glucagon-Like Peptide 1 Receptor Agonists
3.9. Insulin
4. Metabolic Surgery
5. Diabetes and CKD. Importance of Estimating Renal Function and Albuminuria in Patients with T2DM
5.1. Assessment of Renal Involvement: How?
5.2. What Type of Equation Should Be Use to Estimate GFR?
5.3. Which Is the Best Sample to Estimate Albuminuria?
5.4. How Often Should Renal Function Be Estimated in Patients with T2DM?
- At the time of diagnosis of T2DM.
- At the time of routine controls and, in any case, once a year.
- When starting an antihyperglycemic treatment that may require dosage adjustment.
- If any complication occurs that may involve changes in renal function, or any type of acute complication, comorbidities, or treatments that may temporarily modify renal function (e.g., excessive volume depletion by diuretics, hypotension, vomiting, use of non-steroidal anti-inflammatory drugs, etc.).
- In cases of unexpected hypoglycemic episodes, in the absence of changes in glucose-lowering.
- When insulin requirements are consistently reduced over time (<3 months).
- When starting treatment with SGLT2i, a subsequent evaluation of renal function should be carried out between the first and third month after the initiation of therapy.
5.5. Drugs of Choice in Patients with Diabetes and CKD
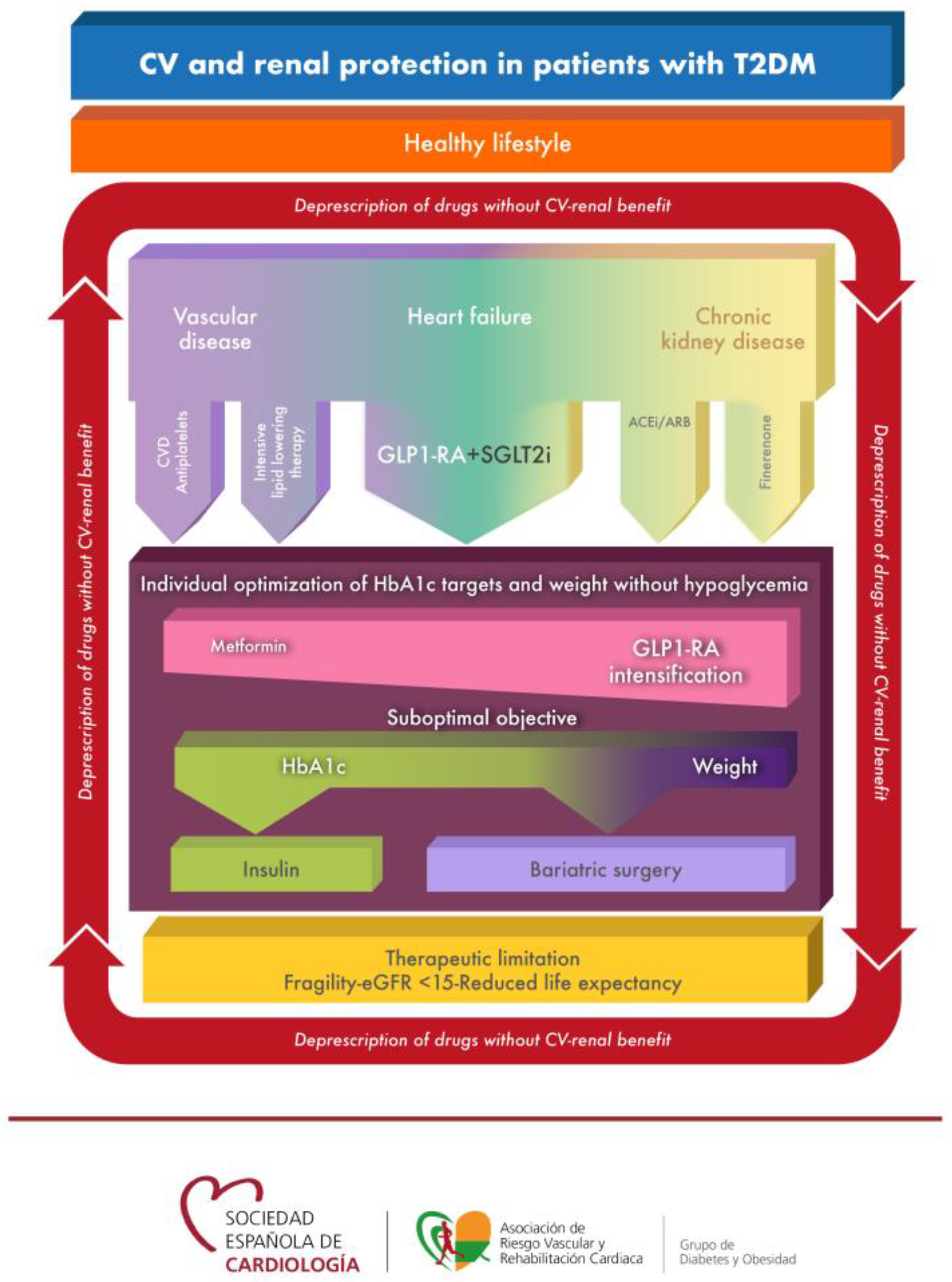
6. Treatment Proposal
6.1. Definition of Metabolic Control
6.1.1. Recommendation
- (a)
- Glycemic control:
- HbA1c < 5.7% in patients without prior pharmacological treatment, or with a short evolution of DM, with the aim of reaching normoglycemia with the combination of GLP-1 receptor agonists/SGLT2i.
- HbA1c ≤ 6.5% in patients with more advanced disease, if it can be achieved with drugs that do not induce hypoglycemia or weight gain.
- HbA1c ≤ 7% (or higher) in patients at high risk of severe hypoglycemia, frail patients, or patients with limited life expectancy.
- In patients using continuous glucose monitoring systems, the glucose management indicator target (previously called estimated HbA1c) will be the same as that of the laboratory HbA1c, maintaining a time in range greater than 80% (if target HbA1c < 6.5%) or higher than 70% (if target HbA1c < 7%), as well as low glycemic variability (coefficient of variation ≤ 36%).
- (b)
- Avoid hypoglycemia:
- Do not use SU, glinides or rapid insulin and limit basal insulin to patients who do not achieve adequate glycemic control despite intensification with cardioprotective antihyperglycemic drugs.
- In patients receiving insulin treatment, the use of continuous glucose monitoring is recommended (with the activation of hypoglycemia alarms) and to achieve a time in hypoglycemia <70 mg/dL less than 4% and a time in hypoglycemia <55 mg/dL less than 1%.
- (c)
- Weight loss:
- The general objective is to promote a weight loss of at least 10% in 1 year in patients with a BMI ≥ 25 kg/m2 or increased abdominal circumference (≥102 cm in men and ≥88 cm in women), at the expense of ectopic fat deposition and preserving muscle mass. Weight loss can also contribute to achieving other general patient goals such as LDLc or blood pressure control.
- In patients with a short time of evolution of T2DM, losses ≥15% can achieve remission of diabetes.
- In all other patients (except cases of frailty) it is recommended to avoid weight gain.
6.1.2. Support of the Recommendation
6.2. Explanation of Optimization of Metabolic Control
6.2.1. Recommendation
- Start (first assessment)
- Intensification (after the introduction of GLP-1 receptor agonists/SGLT2i)
6.2.2. Support of the Recommendation
6.3. Explanation of De-Intensification
6.3.1. Recommendation
- If the patient has an optimal glycemic control but is receiving non-cardioprotective antihyperglycemic therapy, drugs without CV benefit, such as SU, glinides or DPP4i, will be replaced by cardioprotective drugs.
- In those patients on insulin treatment, complex regimens will be simplified by switching to basal insulin and the daily dose of insulin will be reduced, in order to reduce the risk of hypoglycemia and weight gain.
6.3.2. Support of the Recommendation
- Withdrawal of all rapid insulin.
- Decrease basal insulin by 20%.
- Metformin maintenance.
- In patients with two or three fixed mixtures, replacement by a single dose of basal insulin, in an amount equivalent to 40% of the total dose of the mixture.
- Addition of an SGLT2i.
- Addition of a GLP-1 receptor agonist, with progressive dose escalation.
6.4. Explanation of the Choice of Drugs in Patients with eGFR < 15 mL/min
- In patients with eGFR < 15 mL/min/1.73 m2 on treatment with canagliflozin 100 mg, empagliflozin 10 mg or dapagliflozin 10 mg, maintain treatment until dialysis, given the CV and renal benefits.
- Dapagliflozin: Dose of 10 mg/day. Initiate dapagliflozin up to 25 mL/min/1.73 m2, which can be maintained until the start of dialysis. Dapagliflozin can also be used for CKD or HF, regardless of T2DM status.
- Empagliflozin: In T2DM, 10 mg/day, which can be increased to 25 mg/day if tighter glycemic control is required. In HF the dose is 10 mg/day. Empagliflozin can be used in patients with T2DM and CV disease, up to eGFR of 30 mL/min/1.73 m2; and up to 20 mL/min/1.73 m2 in case of HF.
- Canagliflozin: In T2DM, dose of 100 mg/day. In patients with eGFR > 60 mL/min/1.73 m2 and if greater glycemic control is required, it can be increased to 300 mg/day. For the treatment of diabetic CKD, the dose is 100 mg/day. Treatment can be maintained up to eGFR of 30 mL/min/1.73 m2. If the patient has eGFR < 30 mL/min/1.73 m2 and a urine albumin/creatinine ratio >300 mg/g, it can be maintained until the start of dialysis or renal transplantation.
- Ertugliflozin: Dose of 5 mg/day. It can be increased to 15 mg/day when greater glycemic control is needed. It is not recommended to start ertugliflozin in patients with eGFR < 45 mL/min/1.73 m2. Interrupt treatment in case of eGFR < 30 mL/min/1.73 m2.
6.4.1. Explanation of Choice of GLP-1 Receptor Agonists
Recommendations
- According to EMA regulations and the summary of product characteristics, semaglutide, dulaglutide and liraglutide can be administered up to 15 mL/min/1.73 m2; exenatide, and lixisenatide up to 30 mL/min/1.73 m2 [157].
- In patients with eGFR < 15 mL/mL/1.73 m2 on previous treatment with a GLP-1 receptor agonist and well tolerated, consider maintaining it given their CV benefits.
- In case of intolerance to GLP-1 receptor agonists with drop in glomerular filtration, prescribe a DPP4i.
Support of the Recommendation
6.5. Explanation of Choice of Insulin
6.5.1. Recommendation
6.5.2. Support of the Recommendation
6.6. Explanation of the Indication for Bariatric/Metabolic Surgery
6.6.1. Recommendation
6.6.2. Support of the Recommendation
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Soriguer, F.; Goday, A.; Bosch-Comas, A.; Bordiu, E.; Calle-Pascual, A.; Carmena, R.; Casamitjana, R.; Castaño, L.; Castell, C.; Catalá, M.; et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: The Di@bet.es Study. Diabetologia 2012, 55, 88–93. [Google Scholar] [CrossRef]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC guidelines on diabetes; pre-diabetes; and cardiovascular diseases developed in collaboration with the EASD: The Task Force for diabetes; pre-diabetes; and cardiovascular diseases of the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [PubMed]
- Cebrián-Cuenca, A.M.; Mata-Cases, M.; Franch-Nadal, J.; Mauricio, D.; Orozco-Beltrán, D.; Consuegra-Sánchez, L. Half of patients with type 2 diabetes mellitus are at very high cardiovascular risk according to the ESC/EASD: Data from a large Mediterranean population. Eur. J. Prev. Cardiol. 2022, 28, e32–e34. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 6. Glycemic Targets: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46 (Suppl. S1), S97–S110. [Google Scholar] [CrossRef] [PubMed]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Hilliard, M.E.; Isaacs, D.; Johnson, E.L.; et al. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46 (Suppl. S1), S140–S157. [Google Scholar] [CrossRef]
- Giugliano, D.; Ceriello, A.; De Nicola, L.; Perrone-Filardi, P.; Cosentino, F.; Esposito, K. Primary versus secondary cardiorenal prevention in type 2 diabetes: Which newer anti-hyperglycaemic drug matters? Diabetes Obes. Metab. 2020, 22, 149–157. [Google Scholar] [CrossRef]
- Garcia-Moll, X.; Barrios, V.; Franch-Nadal, J. Moving from the stratification of primary and secondary prevention of cardiovascular risk in diabetes towards a continuum of risk: Need for a new paradigm. Drugs Context. 2021, 10, 2021–6-3. [Google Scholar] [CrossRef]
- Reyes-García, R.; Mezquita-Raya, P.; Moreno-Pérez, Ó.; Muñoz-Torres, M.; Merino-Torres, J.F.; Márquez Pardo, R.; Jódar-Gimeno, E.; Escalada San Martín, J.; Gargallo-Fernández, M.; Soto-Gonzalez, A.; et al. Executive summary: Position document: Evaluation and management of hypoglycemia in the patient with diabetes mellitus 2020. Diabetes Mellitus Working Group of the Spanish Society of Endocrinology and Nutrition. Endocrinol. Diabetes Nutr. 2021, 68, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Diabetes and Obesity Task Force. Spanish Society of Cardiology. T2DM Algorithm Updated (2022). Available online: https://secardiologia.es/images/grupos-trabajo/diabetes/algoritmo_diabetes_2022.jpg (accessed on 1 June 2023).
- Gæde, P.; Lund-Andersen, H.; Parving, H.H.; Pedersen, O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N. Engl. J. Med. 2008, 358, 580–591. [Google Scholar] [CrossRef]
- Gaede, P.; Oellgaard, J.; Carstensen, B.; Rossing, P.; Lund-Andersen, H.; Parving, H.-H.; Pedersen, O. Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 2016, 59, 2298–2307. [Google Scholar] [CrossRef]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G.; et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label; cluster-randomised trial. Lancet 2018, 391, 541–551. [Google Scholar] [CrossRef]
- Tang, B.; Zhang, Y.; Wang, Y.; Wang, X.; An, Z.; Yu, X. Effect of bariatric surgery on long-term cardiovascular outcomes: A systematic review and meta-analysis of population-based cohort studies. Surg. Obes. Relat. Dis. 2022, 18, 1074–1086. [Google Scholar] [CrossRef]
- Yan, G.; Wang, J.; Zhang, J.; Gao, K.; Zhao, Q.; Xu, X. Long-term outcomes of macrovascular diseases and metabolic indicators of bariatric surgery for severe obesity type 2 diabetes patients with a meta-analysis. PLoS ONE 2019, 14, e0224828. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1990. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Lazaro, C.I.; Toledo, E.; Buil-Cosiales, P.; Salas-Salvadó, J.; Corella, D.; Fitó, M.; Martínez, J.A.; Alonso-Gómez, Á.M.; Wärnberg, J.; Vioque, J.; et al. Factors associated with successful dietary changes in an energy-reduced Mediterranean diet intervention: A longitudinal analysis in the PREDIMED-Plus trial. Eur. J. Nutr. 2022, 61, 1457–1475. [Google Scholar] [CrossRef]
- Sluik, D.; Buijsse, B.; Muckelbauer, R.; Kaaks, R.; Teucher, B.; Johnsen, N.F.; Tjønneland, A.; Overvad, K.; Ostergaard, J.N.; Amiano, P.; et al. Physical activity and mortality in individuals with diabetes mellitus: A prospective study and meta-analysis. Arch. Intern. Med. 2012, 172, 1285–1295. [Google Scholar] [CrossRef] [PubMed]
- Vanhees, L.; Geladas, N.; Hansen, D.; Kouidi, E.; Niebauer, J.; Reiner, Z.; Cornelissen, V.; Adamopoulos, S.; Prescott, E.; Börjesson, M.; et al. Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular risk factors: Recommendations from the EACPR. Part II. Eur. J. Prev. Cardiol. 2012, 19, 1005–1033. [Google Scholar] [CrossRef]
- Church, T.S.; Blair, S.N.; Cocreham, S.; Johannsen, N.; Johnson, W.; Kramer, K.; Mikus, C.R.; Myers, V.; Nauta, M.; Rodarte, R.Q.; et al. Effects of aerobic and resistance training on hemoglobin A1c levels in patients with type 2 diabetes: A randomized controlled trial. JAMA 2010, 304, 2253–2262. [Google Scholar] [CrossRef]
- Śliwińska-Mossoń, M.; Milnerowicz, H. The impact of smoking on the development of diabetes and its complications. Diabetes Vasc. Dis. Res. 2017, 14, 265–276. [Google Scholar] [CrossRef]
- Gupta, R.; Gupta, S.; Sharma, S.; Sinha, D.N.; Mehrotra, R. Risk of Coronary Heart Disease Among Smokeless Tobacco Users: Results of Systematic Review and Meta-Analysis of Global Data. Nicotine Tob. Res. 2019, 21, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Peng, N.; Chen, G.; Wan, Q.; Yan, L.; Wang, G.; Qin, Y.; Luo, Z.; Tang, X.; Huo, Y.; et al. Interaction between smoking and diabetes in relation to subsequent risk of cardiovascular events. Cardiovasc. Diabetol. 2022, 21, 14. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Shi, F.; Ma, Y.; Yang, D.; Yu, C.; Cao, J. The Global Burden of Type 2 Diabetes Attributable to Tobacco: A Secondary Analysis From the Global Burden of Disease Study 2019. Front. Endocrinol. 2022, 13, 905367. [Google Scholar] [CrossRef]
- Hartmann-Boyce, J.; Chepkin, S.C.; Ye, W.; Bullen, C.; Lancaster, T. Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst. Rev. 2018, 5, CD000146. [Google Scholar] [CrossRef] [PubMed]
- Hughes, J.R.; Stead, L.F.; Lancaster, T. Antidepressants for smoking cessation. Cochrane Database Syst. Rev. 2007, 1, CD000031. [Google Scholar]
- Suissa, K.; Lariviere, J.; Eisenberg, M.J.; Eberg, M.; Gore, G.C.; Grad, R.; Joseph, L.; Reynier, P.M.; Filion, K.B. Efficacy and Safety of Smoking Cessation Interventions in Patients with Cardiovascular Disease: A Network Meta-Analysis of Randomized Controlled Trials. Circ. Cardiovasc. Qual. Outcomes 2017, 10, e002458. [Google Scholar] [CrossRef]
- Hu, Y.; Zong, G.; Liu, G.; Wang, M.; Rosner, B.; Pan, A.; Willett, W.C.; Manson, J.E.; Hu, F.B.; Sun, Q. Smoking Cessation; Weight Change Type 2 Diabetes; and Mortality. N. Engl. J. Med. 2018, 379, 623–632. [Google Scholar] [CrossRef]
- Cheung, Y.M.; O’Brien, R.; Ekinci, E.I. What is new in lipid-lowering therapies in diabetes? Intern. Med. J. 2019, 49, 1472–1480. [Google Scholar] [CrossRef]
- Dayar, E.; Pechanova, O. Targeted Strategy in Lipid-Lowering Therapy. Biomedicines 2022, 10, 1090. [Google Scholar] [CrossRef]
- Wang, X.; Zhang, Y.; Tan, H.; Wang, P.; Zha, X.; Chong, W.; Zhou, L.; Fang, F. Efficacy and safety of bempedoic acid for prevention of cardiovascular events and diabetes: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2020, 19, 128. [Google Scholar] [CrossRef]
- Nissen, S.E.; Lincoff, A.M.; Brennan, D.; Ray, K.K.; Mason, D.; Kastelein, J.J.P.; Thompson, P.D.; Libby, P.; Cho, L.; Plutzky, J.; et al. Bempedoic Acid and Cardiovascular Outcomes in Statin-Intolerant Patients. N. Engl. J. Med. 2023, 388, 1353–1364. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Steg, P.G.; Miller, M.; Brinton, E.A.; Jacobson, T.A.; Ketchum, S.B.; Doyle, R.T., Jr.; Juliano, R.A.; Jiao, L.; Granowitz, C.; et al. Cardiovascular Risk Reduction with Icosapent Ethyl for Hypertriglyceridemia. N. Engl. J. Med. 2019, 380, 11–22. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Thomopoulos, C.; Parati, G.; Zanchetti, A. Effects of blood pressure-lowering treatment on outcome incidence in hypertension: 10-Should blood pressure management differ in hypertensive patients with and without diabetes mellitus? Overview and meta-analyses of randomized trials. J. Hypertens. 2017, 35, 922–944. [Google Scholar] [CrossRef] [PubMed]
- Hemmingsen, B.; Lund, S.S.; Gluud, C.; Vaag, A.; Almdal, T.; Hemmingsen, C.; Wetterslev, J. Intensive glycaemic control for patients with type 2 diabetes: Systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ 2011, 343, d6898. [Google Scholar] [CrossRef]
- Heinemann, L. Continuous Glucose Monitoring (CGM) or Blood Glucose Monitoring (BGM): Interactions and Implications. J. Diabetes Sci. Technol. 2018, 12, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Goto, A.; Arah, O.A.; Goto, M.; Terauchi, Y.; Noda, M. Severe hypoglycaemia and cardiovascular disease: Systematic review and meta-analysis with bias analysis. BMJ 2013, 347, f4533. [Google Scholar] [CrossRef]
- Lee, A.K.; Warren, B.; Lee, C.J.; McEvoy, J.W.; Matsushita, K.; Huang, E.S.; Sharrett, A.R.; Coresh, J.; Selvin, E. The association of severe hypoglycemia with incident cardiovascular events and mortality in adults with type 2 diabetes. Diabetes Care 2018, 41, 104–111. [Google Scholar] [CrossRef]
- Reno, C.M.; Daphna-Iken, D.; Chen, Y.S.; VanderWeele, J.; Jethi, K.; Fisher, S.J. Severe hypoglycemia-induced lethal cardiac arrhythmias are mediated by sympathoadrenal activation. Diabetes 2013, 62, 3570–3581. [Google Scholar] [CrossRef]
- ElSayed, N.A.; Aleppo, G.; Aroda, V.R.; Bannuru, R.R.; Brown, F.M.; Bruemmer, D.; Collins, B.S.; Cusi, K.; Hilliard, M.E.; Isaacs, D.; et al. 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes-2023. Diabetes Care 2023, 46 (Suppl. S1), S49–S67. [Google Scholar] [CrossRef]
- Chen, X.; Li, W.; Huang, Y.; Yang, J.; Tao, Y.; Huang, L.; Shen, J.; Ma, Y.; Liu, Z.; Xu, X.; et al. Association of Type 2 Diabetes Mellitus with Cognitive Function in Adults: A Prospective Cohort Study. J. Alzheimers Dis. 2023; ahead of print. [Google Scholar] [CrossRef]
- Scuteri, A.; Benetos, A.; Sierra, C.; Coca, A.; Chicherio, C.; Frisoni, G.B.; Gasecki, D.; Hering, D.; Lovic, D.; Manios, E.; et al. Routine assessment of cognitive function in older patients with hypertension seen by primary care physicians: Why and how-a decision-making support from the working group on ‘hypertension and the brain’ of the European Society of Hypertension and from the European Geriatric Medicine Society. J. Hypertens. 2021, 39, 90–100. [Google Scholar] [PubMed]
- Gorgojo-Martínez, J.J. New glucose-lowering drugs for reducing cardiovascular risk in patients with type2 diabetes mellitus. Hipertens. Riesgo Vasc. 2019, 36, 145–161. [Google Scholar] [CrossRef] [PubMed]
- Metformin. Summary of Product Characteristics. Available online: https://cima.aemps.es/cima/pdfs/ft/73309/FT_73309.pdf (accessed on 1 June 2023).
- UKPDS Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998, 352, 854–865. [Google Scholar] [CrossRef]
- Griffin, S.J.; Leaver, J.K.; Irving, G.J. Impact of metformin on cardio-vascular disease: A meta-analysis of randomised trials among people with type 2 diabetes. Diabetologia 2017, 60, 1620–1629. [Google Scholar] [CrossRef]
- Pladevall, M.; Patel, A.; MacMahon, S.; Chalmers, J.; Billot, L.; Woodward, M.; Marre, M.; Cooper, M.; Glasziou, P.; Grobbee, D.; et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar]
- Knowles, H.C., Jr. The UGDP-tolbutamide and mortality. Horm. Metab. Res. 1974, 4, 186–188. [Google Scholar]
- Fernandez, C.J.; Raveendran, A.V.; Htwe, N. Efficacy and Cardiovascular Safety of Sulfonylureas. Curr. Drug Saf. 2021, 16, 142–153. [Google Scholar] [CrossRef]
- Azoulay, L.; Suissa, S. Sulfonylureas and the Risks of Cardiovascular Events and Death: A Methodological Meta-Regression Analysis of the Observational Studies. Diabetes Care 2017, 40, 706–714. [Google Scholar] [CrossRef]
- Vaccaro, O.; Masulli, M.; Nicolucci, A.; Bonora, E.; Del Prato, E.; Maggioni, A.; Rivellese, A.A.; Squatrito, S.; Giorda, C.B.; Sesti, G.; et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin (TOSCA.IT): A randomised; multicentre trial. Lancet Diabetes Endocrinol. 2017, 5, 887–897. [Google Scholar] [CrossRef]
- Rosenstock, J.; Kahn, S.E.; Johansen, O.E.; Zinman, B.; Espeland, M.A.; Woerle, H.J.; Pfarr, E.; Keller, A.; Mattheus, M.; Baanstra, D.; et al. Effect of Linagliptin vs. Glimepiride on Major Adverse Cardiovascular Outcomes in Patients with Type 2 Diabetes: The CAROLINA Randomized Clinical Trial. JAMA 2019, 322, 1155–1166. [Google Scholar] [CrossRef]
- Lv, W.; Wang, X.; Xu, Q.; Lu, W. Mechanisms and Characteristics of Sulfonylureas and Glinides. Curr. Top. Med. Chem. 2020, 20, 37–56. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R.; Haffner, S.M.; McMurray, J.J.; Bethel, M.A.; Holzhauer, B.; Hua, T.A.; Belenkov, Y.; Boolell, M.; Buse, J.B.; Buckley, B.M.; et al. Effect of nateglinide on the incidence of diabetes and cardiovascular events. N. Engl. J. Med. 2010, 362, 1463–1476. [Google Scholar]
- Hedrington, M.S.; Davis, S.N. Considerations when using alpha-glucosidase inhibitors in the treatment of type 2 diabetes. Expert Opin. Pharmacother. 2019, 20, 2229–2235. [Google Scholar] [CrossRef] [PubMed]
- Chiasson, J.-L.; Josse, R.G.; Gomis, R.; Hanefeld, M.; Karasik, A.; Laakso, M. Acarbose for prevention of type 2 diabetes mellitus: The STOP-NIDDM randomised trial. Lancet 2002, 359, 2072–2077. [Google Scholar] [CrossRef]
- Chiasson, J.L. Acarbose for the prevention of diabetes; hypertension; and cardiovascular disease in subjects with impaired glucose tolerance: The Study to Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM) Trial. Endocr. Pract. 2006, 12 (Suppl. S1), 25–30. [Google Scholar] [CrossRef]
- Holman, R.R.; Coleman, R.L.; Chan, J.C.N.; Chiasson, J.-L.; Feng, H.; Ge, J.; Gerstein, H.C.; Gray, R.; Huo, Y.; Lang, Z.; et al. Effects of acarbose on cardiovascular and diabetes outcomes in patients with coronary heart disease and impaired glucose tolerance (ACE): A randomised; double-blind; placebo-controlled trial. Lancet Diabetes Endocrinol. 2017, 5, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Nanjan, M.J.; Mohammed, M.; Prashantha Kumar, B.R.; Chandrasekar, M.J.N. Thiazolidinediones as antidiabetic agents: A critical review. Bioorg. Chem. 2018, 77, 548–567. [Google Scholar] [CrossRef]
- Bourg, C.A.; Phillips, B.B. Rosiglitazone; myocardial ischemic risk; and recent regulatory actions. Ann. Pharmacother. 2012, 46, 282–289. [Google Scholar] [CrossRef]
- Dormandy, J.A.; Charbonnel, B.; Eckland, D.J.; Erdmann, E.; Massi-Benedetti, M.; Moules, I.K.; Skene, A.M.; Tan, M.H.; Lefèbvre, P.J.; Murray, G.D.; et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PRO-spective pioglitAzone Clinical Trial In macroVascular Events): A randomized controlled trial. Lancet 2005, 366, 1279–1289. [Google Scholar] [CrossRef]
- Kernan, W.N.; Viscoli, C.M.; Furie, K.L.; Young, L.H.; Inzucchi, S.E.; Gorman, M.; Guarino, P.D.; Lovejoy, A.M.; Peduzzi, P.N.; Conwit, R.; et al. Pioglitazone after Ischemic Stroke or Transient Ischemic Attack. N. Engl. J. Med. 2016, 374, 1321–1331. [Google Scholar] [CrossRef]
- Deacon, C.F. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat. Rev. Endocrinol. 2020, 16, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Green, J.B.; Bethel, M.A.; Armstrong, P.W.; Buse, J.B.; Engel, S.S.; Garg, J.; Josse, R.; Kaufman, K.D.; Koglin, J.; Korn, S.; et al. Effect of Sitagliptin on Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 232–242. [Google Scholar] [CrossRef]
- FDA Drug Safety Communication: FDA Adds Warnings about Heart Failure Risk to Labels of Type 2 Diabetes Medicines Containing Saxagliptin and Alogliptin. Available online: http://www.fda.gov/Drugs/Drug-Safety/ucm486096.htm (accessed on 1 June 2023).
- White, W.B.; Cannon, C.P.; Heller, S.R.; Nissen, S.E.; Bergenstal, R.M.; Bakris, G.L.; Perez, A.T.; Fleck, P.R.; Mehta, C.R.; Kupfer, S.; et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N. Engl. J. Med. 2013, 369, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- Scirica, B.M.; Bhatt, D.L.; Braunwald, E.; Steg, P.G.; Davidson, J.; Hirshberg, B.; Ohman, P.; Frederich, R.; Wiviott, S.D.; Hoffman, E.B.; et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N. Engl. J. Med. 2013, 369, 1317–1326. [Google Scholar] [CrossRef] [PubMed]
- Rosenstock, J.; Perkovic, V.; Johansen, O.E.; Cooper, M.E.; Kahn, S.E.; Marx, N.; Alexander, J.H.; Pencina, M.; Toto, R.D.; Wanner, C.; et al. Effect of linagliptin vs. placebo on major cardiovascular events in adults with type 2 diabetes and high cardiovascular and renal risk: The CARMELINA randomized clinical trial. JAMA 2019, 321, 69–79. [Google Scholar] [CrossRef]
- Zhang, Y.; Han, Q. A review of cardiovascular benefits of SGLT2 inhibitors. Medicine 2022, 101, e30310. [Google Scholar] [CrossRef]
- Maccari, R.; Ottanà, R. Sodium-Glucose Cotransporter Inhibitors as Antidiabetic Drugs: Current Development and Future Perspectives. J. Med. Chem. 2022, 65, 10848–10881. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin; Cardiovascular Outcomes; and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef]
- Wanner, C.; Inzucchi, S.E.; Lachin, J.M.; Fitchett, D.; von Eynatten, M.; Mattheus, M. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 323–334. [Google Scholar] [CrossRef]
- Neal, B.; Perkovi, B.; Mahaffey, K.W.; Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Multicenter Trial to Evaluate the Effect of Dapagliflozin on the Incidence of Cardiovascular Events (DECLARE TIMI 58). N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef]
- Cannon, C.P.; Pratley, R.; Dagogo-Jack, S.; Mancuso, J.; Huyck, S.; Masiukiewicz, U.; Charbonnel, B.; Frederich, R.; Gallo, S.; Cosentino, F.; et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N. Engl. J. Med. 2020, 383, 1425–1435. [Google Scholar] [CrossRef]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.L.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef]
- Herrington, W.G.; Staplin, N.; Wanner, C.; Green, J.B.; Hauske, S.J.; Emberson, J.R.; Preiss, D.; Judge, P.; Mayne, K.J.; Ng, S.Y.A.; et al. Empagliflozin in Patients with Chronic Kidney Disease. N. Engl. J. Med. 2023, 388, 117–127. [Google Scholar]
- Bhatt, D.L.; Szarek, M.; Pitt, B.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Inzucchi, S.E.; Kosiborod, M.N.; et al. SCORED Investigators. Sotagliflozin in Patients with Diabetes and Chronic Kidney Disease. N. Engl. J. Med. 2021, 384, 129–139. [Google Scholar] [CrossRef]
- McMurray, J.V.; Solomon, S.D.; Inzucchi, S.E.; Kober, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Szarek, M.; Steg, P.G.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Voors, A.A.; Metra, M.; et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N. Engl. J. Med. 2021, 384, 117–128. [Google Scholar] [CrossRef]
- Voors, A.A.; Angermann, C.E.; Teerlink, J.R.; Collins, S.P.; Kosiborod, M.; Biegus, J.; Ferreira, J.P.; Nassif, M.E.; Psotka, M.A.; Tromp, J.; et al. The SGLT2 inhibitor empagliflozin in patients hospitalized for acute heart failure: A multinational randomized trial. Nat. Med. 2022, 28, 568–574. [Google Scholar] [CrossRef]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2022, 387, 1089–1098. [Google Scholar] [CrossRef]
- Bosch, C.; Carriazo, S.; Soler, M.J.; Ortiz, A.; Fernandez-Fernandez, B. Tirzepatide and prevention of chronic kidney disease. Clin. Kidney J. 2022, 16, 797–808. [Google Scholar] [CrossRef]
- Nauck, M.A.; Quast, D.R.; Wefers, J.; Meier, J.J. GLP-1 receptor agonists in the treatment of type 2 diabetes—State of the art. Mol. Metab. 2021, 46, 101102. [Google Scholar] [CrossRef]
- Ng, E.; Shaw, J.E.; Wood, A.; Maple-Brown, L.J.; Hare, M.J. Glucagon-like peptide-1 receptor agonist (GLP1-RA) therapy in type 2 diabetes. Aust. J. Gen. Pract. 2022, 51, 513–518. [Google Scholar] [CrossRef]
- Marso, S.P.; Daniels, G.H.; Brown Frandsen, K.; Kristensen, P.; Mann, J.F.E.; Nauck, M.A.; Nissen, S.E.; Pocock, S.; Poulter, N.R.; Ravn, L.S.; et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 311–322. [Google Scholar] [CrossRef]
- Marso, S.P.; Bain, S.C.; Consoli, A.; Eliaschewitz, F.G.; Jodar, E.; Leiter, L.A.; Lingvay, I.; Rosenstock, J.; Seufert, J.; Warren, M.L.; et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 1834–1844. [Google Scholar] [CrossRef]
- Husain, M.; Birkenfeld, A.L.; Donsmark, M.; Dungan, K.; Eliaschewitz, F.G.; Franco, D.R.; Jeppesen, O.K.; Lingvay, I.; Mosenzon, O.; Pedersen, S.D.; et al. Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 2019, 381, 841–851. [Google Scholar] [CrossRef]
- Holman, R.R.; Bethel, M.A.; Mentz, R.J.; Thompson, V.P.; Lokhnygina, Y.; Buse, J.B.; Chan, J.C.; Choi, J.; Gustavson, S.M.; Iqbal, N.; et al. Effects of Once-Weekly Exenatide on Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 1228–1239. [Google Scholar] [CrossRef]
- Hernandez, A.F.; Green, J.B.; Janmohamed, S.; D’Agostino Sr, R.B.; Granger, C.B.; Jones, N.P.; Leiter, L.A.; Rosenberg, A.E.; Sigmon, K.N.; Somerville, M.C.; et al. Harmony Outcomes committees and investigators. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): A double-blind; randomised placebo-controlled trial. Lancet 2018, 392, 1519–1529. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Colhoun, H.M.; Dagenais, G.R.; Diaz, R.; Lakshmanan, M.; Pais, P.; Probstfield, J.; Riesmeyer, J.S.; Riddle, M.C.; Rydén, L.; et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): A double-blind; randomised placebo-controlled trial. Lancet 2019, 394, 121–130. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Sattar, N.; Rosenstock, J.; Ramasundarahettige, C.; Pratley, R.; Lopes, R.D.; Lam, C.S.P.; Khurmi, N.S.; Heenan, L.; Del Prato, S.; et al. Cardiovascular and Renal Outcomes with Efpeglenatide in Type 2 Diabetes. N. Engl. J. Med. 2021, 385, 896–907. [Google Scholar] [CrossRef]
- Nathan, D.M.; Cleary, P.A.; Backlund, J.-Y.C.; Genuth, S.M.; Lachin, J.M.; Orchard, T.J.; Raskin, P.; Zinman, B. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N. Engl. J. Med. 2005, 353, 2643–2653. [Google Scholar]
- Yapanis, M.; James, S.; Craig, M.E.; O’Neal, D.; Ekinci, E.I. Complications of Diabetes and Metrics of Glycemic Management Derived From Continuous Glucose Monitoring. J. Clin. Endocrinol. Metab. 2022, 107, e2221–e2236. [Google Scholar] [CrossRef]
- Lachin, J.M.; Orchard, T.J.; Nathan, D.M.; DCCT/EDIC Research Group. Update on cardiovascular outcomes at 30 years of the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care 2014, 37, 39–43. [Google Scholar] [CrossRef]
- ORIGIN Trial Investigators; Gerstein, H.C.; Bosch, J.; Dagenais, G.R.; Díaz, R.; Jung, H.; Maggioni, A.P.; Pogue, J.; Probstfield, J.; Ramachandran, A.; et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N. Engl. J. Med. 2012, 367, 319–328. [Google Scholar]
- Marso, S.P.; McGuire, D.K.; Zinman, B.; Poulter, N.R.; Emerson, S.S.; Pieber, T.R.; Pratley, R.E.; Haahr, P.M.; Lange, M.; Brown-Frandsen, K.; et al. Efficacy and Safety of Degludec versus Glargine in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 723–732. [Google Scholar] [CrossRef]
- Zinman, B.; Marso, S.P.; Poulter, N.R.; Emerson, S.S.; Pieber, T.R.; Pratley, R.E.; Lange, M.; Brown-Frandsen, K.; Moses, A.; Ocampo Francisco, A.M.; et al. Day-to-day fasting glycaemic variability in DEVOTE: Associations with severe hypoglycaemia and cardiovascular outcomes (DEVOTE 2). Diabetologia 2018, 61, 48–57. [Google Scholar] [CrossRef]
- Pieber, T.R.; Marso, S.P.; McGuire, D.K.; Zinman, B.; Poulter, N.R.; Emerson, S.S.; Pratley, R.E.; Woo, V.; Heller, S.; Lange, M.; et al. DEVOTE 3: Temporal relationships between severe hypoglycaemia; cardiovascular outcomes and mortality. Diabetologia 2018, 61, 58–65. [Google Scholar] [CrossRef]
- Philis-Tsimikas, A.; Klonoff, D.C.; Khunti, K.; Bajaj, H.S.; Leiter, L.A.; Hansen, M.V.; Troelsen, L.N.; Ladelund, S.; Heller, S.; Pieber, T.R.; et al. Risk of hypoglycaemia with insulin degludec versus insulin glargine U300 in insulin-treated patients with type 2 diabetes: The randomised; head-to-head CONCLUDE trial. Diabetologia 2020, 63, 698–710. [Google Scholar] [CrossRef]
- Sheng, B.; Truong, K.; Spitler, H.; Zhang, L.; Tong, X.; Chen, L. The Long-Term Effects of Bariatric Surgery on Type 2 Diabetes Remission; Microvascular and Macrovascular Complications; and Mortality: A Systematic Review and Meta-Analysis. Obes. Surg. 2017, 27, 2724–2732. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2020 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int. 2020, 98 (Suppl. S4), S1–S115. [Google Scholar] [CrossRef]
- Gansevoort, R.T.; Anders, H.J.; Cozzolino, M.; Fliser, D.; Fouque, D.; Ortiz, A.; Soler, M.J.; Wanner, C. What should European nephrology do with the new CKD-EPI equation? Nephrol. Dial Transplant. 2023, 38, 1–6. [Google Scholar] [CrossRef]
- Lewis, E.J.; Hunsicker, L.G.; Bain, R.P.; Rohde, R.D. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N. Engl. J. Med. 1993, 329, 1456–1462. [Google Scholar] [CrossRef]
- Brenner, B.M.; Cooper, M.E.; de Zeeuw, D.; Keane, W.F.; Mitch, W.E.; Parving, H.H.; Remuzzi, G.; Snapinn, S.M.; Zhang, Z.; Shahinfar, S.; et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N. Engl. J. Med. 2001, 345, 861–869. [Google Scholar] [CrossRef]
- Lewis, E.J.; Hunsicker, L.G.; Clarke, W.R.; Berl, T.; Pohl, M.A.; Lewis, J.B.; Ritz, E.; Atkins, R.C.; Rohde, R.; Raz, I.; et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N. Engl. J. Med. 2001, 345, 851–860. [Google Scholar] [CrossRef]
- Chaudhuri, A.; Ghanim, H.; Arora, P. Improving the residual risk of renal and cardiovascular outcomes in diabetic kidney disease: A review of pathophysiology; mechanisms; and evidence from recent trials. Diabetes Obes. Metab. 2022, 24, 365–376. [Google Scholar] [CrossRef]
- Erraez, S.; López-Mesa, M.; Gómez-Fernández, P. Mineralcorticoid receptor blockers in chronic kidney disease. Nefrologia 2021, 41, 258–275. [Google Scholar] [CrossRef]
- Bakris, G.L.; Agarwal, R.; Anker, S.D.; Pitt, B.; Ruilope, L.M.; Rossing, P.; Kolkhof, P.; Nowack, C.; Schloemer, P.; Joseph, A.; et al. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2020, 383, 2219–2229. [Google Scholar] [CrossRef]
- Pitt, B.; Filippatos, G.; Agarwal, R.; Anker, S.D.; Bakris, G.L.; Rossing, P.; Joseph, A.; Kolkhof, P.; Nowack, C.; Schloemer, P.; et al. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. N. Engl. J. Med. 2021, 385, 2252–2263. [Google Scholar] [CrossRef]
- Castro., A.; Marzal, D.; Arrarte, V.; Campuzano, R.; Dalmau, R.; Fernández, R.; García-Moll, X.; Gómez Doblas, J.J.; Gorgojo, J.J.; Mazón, P.; et al. Comprehensive approach to the patient with diabetes mellitus and cardiovascular disease or very high cardiovascular risk. REC Cardio Clin. 2019, 54, 183–192. [Google Scholar]
- Campuzano, R.; Castro, A.; Arrarte, V.; de Pablo, C.; Marzal, D.; Fernández, R.; Berenguel Senen, A.; Alarcón Duque, J.A. Selection of the best of 2020 in vascular risk and cardiac rehabilitation. REC Cardio Clin. 2021, 56 (Suppl. S1), 27–34. [Google Scholar]
- Thomas, M.; Magwire, M.; Gosch, K.; Sammour, Y.; Mehta, R.; O’Keefe, J.; Nassif, M.E.; Kosiborod, M. Cardiometabolic Center of Excellence: A Novel Care Delivery Model for Secondary Prevention of Cardiovascular Disease in Type 2 Diabetes. Circ. Cardiovasc. Qual. Outcomes 2021, 14, e007682. [Google Scholar] [CrossRef]
- Arnold, S.V.; Goyal, A.; Inzucchi, S.E.; McGuire, D.K.; Tang, F.; Mehta, S.N.; Sperling, L.S.; Maddox, T.M.; Einhorn, D.; Wong, N.D.; et al. Quality of Care of the Initial Patient Cohort of the Diabetes Collaborative Registry®. J. Am. Heart Assoc. 2017, 6, e005999. [Google Scholar] [CrossRef]
- Weng, W.; Tian, Y.; Kong, S.X.; Ganguly, R.; Hersloev, M.; Brett, J.; Hobbs, T. The prevalence of cardiovascular disease and antidiabetes treatment characteristics among a large type 2 diabetes population in the United States. Endocrinol. Diabetes Metab. 2019, 2, e00076. [Google Scholar] [CrossRef]
- Buse, J.B.; Wexler, D.J.; Tsapas, A.; Rossing, P.; Mingrone, G.; Mathieu, C.; D’Alessio, D.A.; Davies, M.J. 2019 update to: Management of hyperglycaemia in type 2 diabetes; 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020, 63, 221–228. [Google Scholar] [CrossRef]
- Ray, K.K.; Seshasai, S.R.; Wijesuriya, S.; Sivakumaran, R.; Nethercott, S.; Preiss, D.; Erqou, S.; Sattar, N. Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: A meta-analysis of randomised controlled trials. Lancet 2009, 373, 1765–1772. [Google Scholar] [CrossRef]
- Bonds, D.E.; Miller, M.E.; Bergenstal, R.M.; Buse, J.B.; Byington, R.P.; Cutler, J.A.; Dudl, R.J.; Ismail-Beigi, F.; Kimel, A.R.; Hoogwerf, B.; et al. The association between symptomatic; severe hypoglycaemia and mortality in type 2 diabetes: Retrospective epidemiological analysis of the ACCORD study. BMJ 2010, 340, b4909. [Google Scholar] [CrossRef]
- Zinman, B.; Marso, S.P.; Christiansen, E.; Calanna, S.; Rasmussen, S.; Buse, J.B.; LEADER Publication Committee on behalf of the LEADER Trial Investigators. Hypoglycemia; Cardiovascular Outcomes; and Death: The LEADER Experience. Diabetes Care 2018, 41, 1783–1791. [Google Scholar] [CrossRef]
- Cai, X.; Zhang, Y.; Li, M.; Wu, J.H.; Mai, L.; Li, J.; Yang, Y.; Hu, Y.; Huang, Y. Association between prediabetes and risk of all-cause mortality and cardiovascular disease: Updated meta-analysis. BMJ 2020, 370, m2297. [Google Scholar] [CrossRef] [PubMed]
- Garber, A.J.; Handelsman, Y.; Grunberger, G.; Einhorn, D.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bush, M.A.; DeFronzo, R.A.; Garber, J.R.; et al. Consensus Statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the Comprehensive Type 2 Diabetes Management Algorithm—2020 Executive Summary. Endocr. Pract. 2020, 26, 107–139. [Google Scholar] [CrossRef] [PubMed]
- Battelino, T.; Danne, T.; Bergenstal, R.M.; Amiel, S.A.; Beck, R.; Biester, T.; Bosi, E.; Buckingham, B.A.; Cefalu, W.T.; Close, K.L.; et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations from the International Consensus on Time in Range. Diabetes Care 2019, 42, 1593–1603. [Google Scholar] [CrossRef]
- Garvey, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr. Pract. 2016, 22 (Suppl. S3), 1–203. [Google Scholar] [CrossRef]
- Gorgojo Martínez, J.J. Relevance of weight in the management of patients with type 2 diabetes mellitus: Towards an adipocentric approach to diabetes. Med. Clin. 2016, 147 (Suppl. S1), 8–16. [Google Scholar] [CrossRef]
- Al-Mrabeh, A.; Zhyzhneuskaya, S.V.; Peters, C.; Barnes, A.C.; Melhem, S.; Jesuthasan, A.; Aribisala, B.; Hollingsworth, K.G.; Lietz, G.; Mathers, J.C.; et al. Hepatic Lipoprotein Export and Remission of Human Type 2 Diabetes after Weight Loss. Cell Metab. 2020, 31, 233–249.e4. [Google Scholar] [CrossRef] [PubMed]
- Gregg, E.W.; Jakicic, J.M.; Blackburn, G.; Bloomquist, P.; Bray, G.A.; Clark, J.M.; Coday, M.; Curtis, J.M.; Egan, C.; Evans, M.; et al. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: A post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol. 2016, 4, 913–921. [Google Scholar]
- Mingrone, G.; Panunzi, S.; De Gaetano, A.; Guidone, C.; Iaconelli, A.; Capristo, E.; Chamseddine, G.; Bornstein, S.R.; Rubino, F. Metabolic surgery versus conventional medical therapy in patients with type 2 diabetes: 10-year follow-up of an open-label; single-centre; randomised controlled trial. Lancet 2021, 397, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Chumakova-Orin, M.; Vanetta, C.; Moris, D.P.; Guerron, A.D. Diabetes remission after bariatric surgery. World J. Diabetes 2021, 12, 1093–1101. [Google Scholar] [CrossRef]
- Kalra, S.; Singal, A.; Lathia, T. What’s in a Name? Redefining Type 2 Diabetes Remission. Diabetes Ther. 2021, 12, 647–654. [Google Scholar] [CrossRef]
- Cahn, A.; Wiviott, S.D.; Mosenzon, O.; Murphy, S.A.; Goodrich, E.L.; Yanuv, I.; Rozenberg, A.; Wilding, J.P.H.; Leiter, L.A.; Bhatt, D.L.; et al. Cardiorenal outcomes with dapagliflozin by baseline glucose-lowering agents: Post hoc analyses from DECLARE-TIMI 58. Diabetes Obes. Metab. 2021, 23, 29–38. [Google Scholar] [CrossRef]
- Lam, C.S.P.; Ramasundarahettige, C.; Branch, K.R.H.; Sattar, N.; Rosenstock, J.; Pratley, R.; Del Prato, S.; Lopes, R.D.; Niemoeller, E.; Khurmi, N.S.; et al. Efpeglenatide and Clinical Outcomes with and without Concomitant Sodium-Glucose Cotransporter-2 Inhibition Use in Type 2 Diabetes: Exploratory Analysis of the AMPLITUDE-O Trial. Circulation 2022, 145, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Jabbour, S.A.; Frías, J.P.; Hardy, E.; Ahmed, A.; Wang, H.; Öhman, P.; Guja, C. Safety and Efficacy of Exenatide Once Weekly Plus Dapagliflozin Once Daily versus Exenatide or Dapagliflozin Alone in Patients with Type 2 Diabetes Inadequately Controlled with Metformin Monotherapy: 52-Week Results of the DURATION-8 Randomized Controlled Trial. Diabetes Care 2018, 41, 2136–2146. [Google Scholar] [PubMed]
- Frías, J.P.; Auerbach, P.; Bajaj, H.S.; Fukushima, Y.; Lingvay, I.; Macura, S.; Søndergaard, A.L.; Tankova, T.I.; Tentolouris, N.; Buse, J.B. Efficacy and safety of once-weekly semaglutide 2·0 mg versus 1·0 mg in patients with type 2 diabetes (SUSTAIN FORTE): A double-blind; randomised; phase 3B trial. Lancet Diabetes Endocrinol. 2021, 9, 563–574. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.; Færch, L.; Jeppesen, O.K.; Pakseresht, A.; Pedersen, S.D.; Perreault, L.; Rosenstock, J.; Shimomura, I.; Viljoen, A.; Wadden, T.A.; et al. Semaglutide 2·4 mg once a week in adults with overweight or obesity; and type 2 diabetes (STEP 2): A randomised; double-blind; double-dummy; placebo-controlled; phase 3 trial. Lancet 2021, 397, 971–984. [Google Scholar] [CrossRef]
- Frias, J.P.; Bonora, E.; Nevarez Ruiz, L.; Li, Y.G.; Yu, Z.; Milicevic, Z.; Malik, R.; Bethel, M.A.; Cox, D.A. Efficacy and Safety of Dulaglutide 3.0 mg and 4.5 mg versus Dulaglutide 1.5 mg in Metformin-Treated Patients with Type 2 Diabetes in a Randomized Controlled Trial (AWARD-11). Diabetes Care 2021, 44, 765–773. [Google Scholar] [CrossRef]
- Gorgojo-Martínez, J.J.; Gargallo-Fernández, M.A.; Galdón Sanz-Pastor., A.; Antón-Bravo, T.; Brito-Sanfiel, M.; Wong-Cruz, J. Real-World Clinical Outcomes Associated with Canagliflozin in Patients with Type 2 Diabetes Mellitus in Spain: The Real-Wecan Study. J. Clin. Med. 2020, 9, 2275. [Google Scholar] [CrossRef]
- Sattar, N.; Lee, M.M.Y.; Kristensen, S.L.; Branch, K.R.H.; Del Prato, S.; Khurmi, N.S.; Lam, C.S.P.; Lopes, R.D.; McMurray, J.J.V.; Pratley, R.E.; et al. Cardiovascular; mortality; and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: A systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021, 9, 653–662. [Google Scholar] [CrossRef]
- Salah, H.M.; Al’Aref, S.J.; Khan, M.S.; Al-Hawwas, M.; Vallurupalli, S.; Mehta, J.L.; Mounsey, J.P.; Greene, S.J.; McGuire, D.K.; Lopes, R.D.; et al. Effects of sodium-glucose cotransporter 1 and 2 inhibitors on cardiovascular and kidney outcomes in type 2 diabetes: A meta-analysis update. Am. Heart J. 2021, 233, 86–91. [Google Scholar] [CrossRef]
- Giugliano, D.; Longo, M.; Caruso, P.; Maiorino, M.I.; Bellastella, G.; Esposito, K. Sodium-glucose co-transporter-2 inhibitors for the prevention of cardiorenal outcomes in type 2 diabetes: An updated meta-analysis. Diabetes Obes. Metab. 2021, 23, 1672–1676. [Google Scholar] [CrossRef]
- Tsapas, A.; Karagiannis, T.; Avgerinos, I.; Liakos, A.; Bekiari, E. GLP-1 receptor agonists for cardiovascular outcomes with and without metformin. A systematic review and meta-analysis of cardiovascular outcomes trials. Diabetes Res. Clin. Pract. 2021, 177, 108921. [Google Scholar] [CrossRef] [PubMed]
- Neuen, B.L.; Arnott, C.; Perkovic, V.; Figtree, G.; de Zeeuw, D.; Fulcher, G.; Jun, M.; Jardine, M.J.; Zoungas, S.; Pollock, C.; et al. Sodium-glucose co-transporter-2 inhibitors with and without metformin: A meta-analysis of cardiovascular; kidney and mortality outcomes. Diabetes Obes. Metab. 2021, 23, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Escobar, C.; Barrios, V.; Cosín, J.; Gámez Martínez, J.M.; Huelmos Rodrigo, A.I.; Ortíz Cortés, C.; Llergo, J.T.; Requeijo, C.; Solà, I.; Zapata, M.J.M. SGLT2 inhibitors and GLP1 agonists administered without metformin compared to other glucose-lowering drugs in patients with type 2 diabetes mellitus to prevent cardiovascular events: A systematic review. Diabet. Med. 2021, 38, e14502. [Google Scholar] [CrossRef]
- Davis, S.N.; Johns, D.; Maggs, D.; Xu, H.; Northrup, J.H.; Brodows, R.G. Exploring the substitution of exenatide for insulin in patients with type 2 diabetes treated with insulin in combination with oral antidiabetes agents. Diabetes Care 2007, 30, 2767–2772. [Google Scholar] [CrossRef] [PubMed]
- Tuttle, K.R.; Lakshmanan, M.C.; Rayner, B.; Busch, R.S.; Zimmermann, A.G.; Woodward, D.B.; Botros, F.T. Dulaglutide versus insulin glargine in patients with type 2 diabetes and moderate-to-severe chronic kidney disease (AWARD-7): A multicentre; open-label; randomised trial. Lancet Diabetes Endocrinol. 2018, 6, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Rodbard, H.W.; Lingvay, I.; Reed, J.; de la Rosa, R.; Rose, L.; Sugimoto, D.; Araki, E.; Chu, P.L.; Wijayasinghe, N.; Norwood, P. Semaglutide Added to Basal Insulin in Type 2 Diabetes (SUSTAIN 5): A Randomized; Controlled Trial. J. Clin. Endocrinol. Metab. 2018, 103, 2291–2301. [Google Scholar] [CrossRef]
- Brown, R.E.; Bech, P.G.; Aronson, R. Semaglutide once weekly in people with type 2 diabetes: Real-world analysis of the Canadian LMC diabetes registry (SPARE study). Diabetes Obes. Metab. 2020, 22, 2013–2020. [Google Scholar] [CrossRef]
- Naing, S.; Ramesh, G.; Garcha, J.; Poliyedath, A.; Khandelwal, S.; Mills, P.K. Is the stepping-down approach a better option than multiple daily injections in obese patients with poorly controlled Type 2 diabetes on advanced insulin therapy? Endocrinol. Diabetes Metab. 2020, 4, e00204. [Google Scholar] [CrossRef]
- Morillas, C.; D’Marco, L.; Puchades, M.J.; Solá-Izquierdo, E.; Gorriz-Zambrano, C.; Bermúdez, V.; Gorriz, J.L. Insulin Withdrawal in Diabetic Kidney Disease: What Are We Waiting for? Int. J. Environ. Res. Public Health 2021, 18, 5388. [Google Scholar] [CrossRef]
- Vitale, M.; Haxhi, J.; Cirrito, T.; Pugliese, G. Renal protection with glucagon-like peptide-1 receptor agonists. Curr. Opin. Pharmacol. 2020, 54, 91–101. [Google Scholar] [CrossRef]
- Jacobsen, L.V.; Hindsberger, C.; Robson, R.; Zdravkovic, M. Effect of renal impairment on the pharmacokinetics of the GLP-1 analogue liraglutide. Br. J. Clin. Pharmacol. 2009, 68, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Górriz, J.L.; Romera, I.; Cobo, A.; O’Brien, P.D.; Merino-Torres, J.F. Glucagon-Like Peptide-1 Receptor Agonist Use in People Living with Type 2 Diabetes Mellitus and Chronic Kidney Disease: A Narrative Review of the Key Evidence with Practical Considerations. Diabetes Ther. 2022, 13, 389–421. [Google Scholar] [CrossRef] [PubMed]
- Idorn, T.; Knop, F.K.; Jørgensen, M.B.; Jensen, T.; Resuli, M.; Hansen, P.M.; Christensen, K.B.; Holst, J.J.; Hornum, M.; Feldt-Rasmussen, B. Safety and Efficacy of Liraglutide in Patients with Type 2 Diabetes and End-Stage Renal Disease: An Investigator-Initiated; Placebo-Controlled; Double-Blind; Parallel-Group; Randomized Trial. Diabetes Care 2016, 39, 206–213. [Google Scholar] [CrossRef]
- Bakris, G.; Oshima, M.; Mahaffey, K.W.; Agarwal, R.; Cannon, C.P.; Capuano, G.; Charytan, D.M.; de Zeeuw, D.; Edwards, R.; Greene, T.; et al. Effects of Canagliflozin in Patients with Baseline eGFR <30 mL/min per 1.73 m2: Subgroup Analysis of the Randomized CREDENCE Trial. Clin. J. Am. Soc. Nephrol. 2020, 15, 1705–1714. [Google Scholar] [PubMed]
- Aldekhail, N.M.; Logue, J.; McLoone, P.; Morrison, D.S. Effect of orlistat on glycaemic control in overweight and obese patients with type 2 diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials. Obes. Rev. 2015, 16, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee; Draznin, B.; Aroda, V.R.; Bakris, G.; Benson, G.; Brown, F.M.; Freeman, R.; Green, J.; Huang, E.; Isaacs, D.; et al. 8. Obesity and Weight Management for the Prevention and Treatment of Type 2 Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care 2022, 45 (Suppl. S1), S113–S124. [Google Scholar]
- Rubino, F.; Nathan, D.M.; Eckel, R.H.; Schauer, P.R.; Alberti, K.G.; Zimmet, P.Z.; Del Prato, S.; Ji, L.; Sadikot, S.M.; Herman, W.H.; et al. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Diabetes Care 2016, 39, 861–877. [Google Scholar] [CrossRef]
| Cardiovascular Risk Factor | Action | |||
|---|---|---|---|---|
| Dietetic pattern | Mediterranean diet | |||
| Smoking | Stop smoking | |||
| Physical activity | >150 min a week of aerobic physical activity + resistance exercise twice a week | |||
| HbA1c | ≤7.0%, ≤6.5% if possible without hypoglycemia (individualization) | |||
| Weight | Reduction in body weight ≥10% if BMI ≥ 25 Kg/m2 or waist circumference at risk | |||
| Lipids | Primary objective | Secondary objectives | ||
| CV risk | LDLc | Non-HDL cholesterol | ApoB | |
| Moderate | <100 mg/dL | <130 mg/dL | <100 mg/dL | |
| High | <70 mg/dL and a reduction ≥50% from baseline levels | <100 mg/dL | <80 mg/dL | |
| Very high | <55 mg/dL and a reduction ≥50% from baseline levels | <85 mg/dL | <65 mg/dL | |
| Blood pressure | • Systolic: 120 -< 130 mmHg • Diastolic: 70 -< 80 mmHg | |||
| Drugs with CV Benefit in Specific Study Populations | Clinical Trial | Primary and Secondary Endpoints with a Significant Risk Reduction | |
|---|---|---|---|
| Major CV Events † | HF Hospitalization | ||
| Established CVD | |||
| GLP-1 receptor agonists | |||
| Liraglutide | Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results (LEADER) [89] | Primary endpoint ‡ | |
| Semaglutide | Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes (SUSTAIN-6) [90] | Primary endpoint ‡ | |
| Dulaglutide | Researching Cardiovascular Events with a Weekly Incretin in Diabetes (REWIND) [94] | Primary endpoint ‡ | |
| SGLT2 inhibitors | |||
| Empagliflozin | Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients (EMPA-REG) [72] | Primary endpoint ‡ | Secondary endpoint |
| Canagliflozin | Canagliflozin Cardiovascular Assessment Study (CANVAS) [74] | Primary endpoint ‡ | Secondary endpoint |
| Dapagliflozin | Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE-TIMI 58) [75] | Primary endpoint ‡ | |
| Ertugliflozin | Evaluation of Ertugliflozin Efficacy and Safety Cardiovascular Outcomes Trial (VERTIS CV) [76] | Secondary endpoint | |
| Multiple CV risk factors | |||
| GLP-1 receptor agonist, dulaglutide | Researching Cardiovascular Events with a Weekly Incretin in Diabetes (REWIND) [94] | Primary endpoint ‡ | |
| SGLT2 inhibitor, dapagliflozin | Dapagliflozin Effect on Cardiovascular Events–Thrombolysis in Myocardial Infarction 58 (DECLARE-TIMI 58) [75] | Primary endpoint ‡ | |
| Heart failure with reduced ejection fractionǁ | |||
| SGLT2 inhibitors | |||
| Dapagliflozin | Dapagliflozin and Prevention of Adverse Outcomes in Heart Failure (DAPA-HF) [81] ‡ | Primary endpoint ‡ | |
| Empagliflozin | Empagliflozin Outcome Trial in Patients with Chronic Heart Failure and a Reduced Ejection Fraction (EMPEROR-Reduced) [82] | Primary endpoint ‡ | |
| Chronic kidney disease with albuminuria ** | |||
| SGLT2 inhibitors | |||
| Canagliflozin | Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) [77] | Secondary endpoint | Secondary endpoint ‡ |
| Dapagliflozin | Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) [78] | Secondary endpoint | Secondary endpoint |
| Heart failure with preserved ejection fraction | |||
| Empagliflozin | EMPEROR PRESERVED (EMPagliflozin outcomE tRial in Patients with chrOnic heaRt Failure with Preserved Ejection Fraction) [85] | Primary endpoint | |
| Dapagliflozin | DELIVER (Dapagliflozin Evaluation to Improve the LIVEs of Patients with PReserved Ejection Fraction Heart Failure) [86] | Primary endpoint | |
| Acute heart failure | |||
| Empagliflozin | EMPULSE (A Study to Test the Effect of Empagliflozin in Patients Who Are in Hospital for Acute Heart Failure) [84] | Primary endpoint | |
| Dapagliflozin | DAPA-HF (Efficacy and Safety of Dapagliflozin in Acute Heart Failure) [81] | Primary endpoint | |
| Sotagliflozin | SOLOIST-WHF (Effect of Sotagliflozin on Cardiovascular Events in Patients with Type 2 Diabetes Post Worsening Heart Failure) [83] | ||
| Chronic kidney disease with or without albuminuria | |||
| Sotagliflozin | SCORED (Effect of Sotagliflozin on Cardiovascular and Renal Events in Patients with Type 2 Diabetes and Moderate Renal Impairment Who Are at Cardiovascular Risk) [79] | Secondary endpoint | Primary endpoint |
| Empagliflozin | EMPA-KIDNEY (The Study of Heart and Kidney Protection with Empagliflozin) [80] | Secondary endpoint | Secondary endpoint |
| Dapagliflozin | DAPA-CKD (Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease) [78] | Secondary endpoint | Secondary endpoint |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro Conde, A.; Marzal Martín, D.; Campuzano Ruiz, R.; Fernández Olmo, M.R.; Morillas Ariño, C.; Gómez Doblas, J.J.; Gorriz Teruel, J.L.; Mazón Ramos, P.; García-Moll Marimon, X.; Soler Romeo, M.J.; et al. Comprehensive Cardiovascular and Renal Protection in Patients with Type 2 Diabetes. J. Clin. Med. 2023, 12, 3925. https://doi.org/10.3390/jcm12123925
Castro Conde A, Marzal Martín D, Campuzano Ruiz R, Fernández Olmo MR, Morillas Ariño C, Gómez Doblas JJ, Gorriz Teruel JL, Mazón Ramos P, García-Moll Marimon X, Soler Romeo MJ, et al. Comprehensive Cardiovascular and Renal Protection in Patients with Type 2 Diabetes. Journal of Clinical Medicine. 2023; 12(12):3925. https://doi.org/10.3390/jcm12123925
Chicago/Turabian StyleCastro Conde, Almudena, Domingo Marzal Martín, Raquel Campuzano Ruiz, Maria Rosa Fernández Olmo, Carlos Morillas Ariño, Juan José Gómez Doblas, Jose Luis Gorriz Teruel, Pilar Mazón Ramos, Xavier García-Moll Marimon, Maria Jose Soler Romeo, and et al. 2023. "Comprehensive Cardiovascular and Renal Protection in Patients with Type 2 Diabetes" Journal of Clinical Medicine 12, no. 12: 3925. https://doi.org/10.3390/jcm12123925
APA StyleCastro Conde, A., Marzal Martín, D., Campuzano Ruiz, R., Fernández Olmo, M. R., Morillas Ariño, C., Gómez Doblas, J. J., Gorriz Teruel, J. L., Mazón Ramos, P., García-Moll Marimon, X., Soler Romeo, M. J., León Jiménez, D., Arrarte Esteban, V., Obaya Rebollar, J. C., Escobar Cervantes, C., & Gorgojo Martínez, J. J. (2023). Comprehensive Cardiovascular and Renal Protection in Patients with Type 2 Diabetes. Journal of Clinical Medicine, 12(12), 3925. https://doi.org/10.3390/jcm12123925







