Investigation of the Influence of Roughness and Dental Implant Design on Primary Stability via Analysis of Insertion Torque and Implant Stability Quotient: An In Vitro Study
Abstract
:1. Introduction
2. Methods
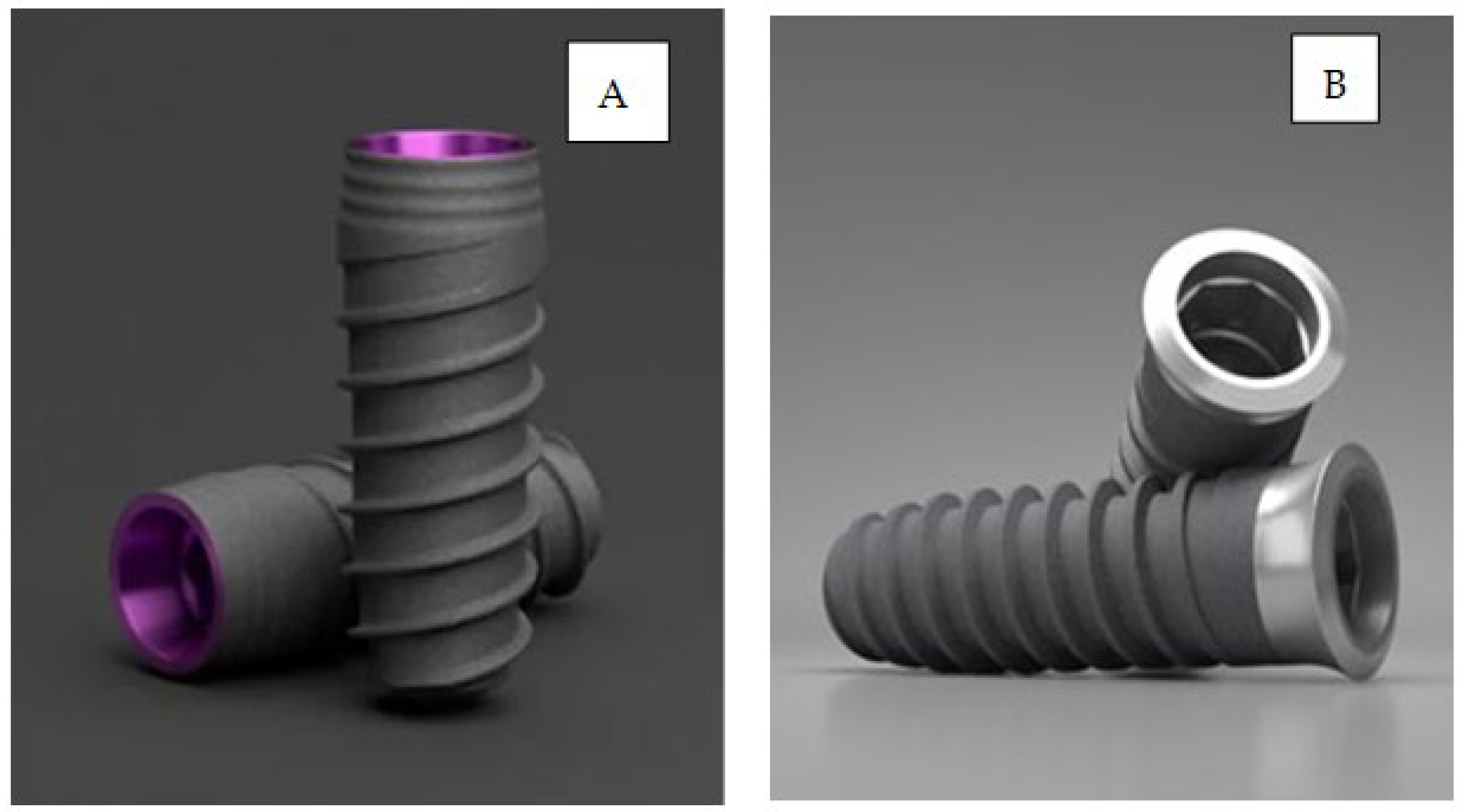
2.1. Dental Implants
2.2. Surface Treatments
- Minimally rough surfaces: Sa values 0.5–1 µm.
- Moderately rough surfaces: Sa values 1–2 µm.
- Rough surfaces: Sa values > 2 µm.
2.3. Roughness
2.4. Wettability
2.5. Implant Stability Analysis
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wennerberg, A.; Albrektsson, T. Effects of titanium surface topography on bone integration: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. S4), 172–184. [Google Scholar] [CrossRef] [PubMed]
- Feller, L.; Jadwat, Y.; Khammissa, R.A.G.; Meyerov, R.; Schechter, I.; Lemmer, J. Cellular responses evoked by different surface characteristics of intra osseous titanium implants. BioMed Res. Int. 2015, 2015, 171945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, G.R. Surface roughness of dental implant and osseointegration. J. Maxillofac. Oral Surg. 2021, 20, 1–4. [Google Scholar]
- Heitzer, M.; Kniha, K.; Katz, M.; Winnand, P.; Peters, F.; Möhlhenrich, S.; Hölzle, F.; Modabber, A. The primary stability of two dental implant systems in low-density bone. Int. J. Oral Maxillofac. Surg. 2022, 51, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.-S.; Namgung, C.; Lee, J.-H.; Lim, Y.-J. The influence of thread geometry on implant osseointegration under immediate loading: A literature review. J. Adv. Prosthodont. 2014, 6, 547–554. [Google Scholar] [CrossRef] [Green Version]
- Feller, L.; Chandran, R.; Khammissa, R.A.G.; Meyerov, R.; Jadwat, Y.; Bouckaert, M.; Schechter, I.; Lemmer, J. Osseointegration: Biological events in relation to characteristics of the implant surface. S. Afr. Dent. J. 2014, 69, 112–117. [Google Scholar]
- Gil, F.J.; Aparicio, C.; Manero, J.M.; Padros, A. Influence of the height of the external hexagon and surface treatment on fatigue life of commercially pure titanium dental implants. Int. J. Oral Maxillofac. Implant. 2009, 24, 583–590. [Google Scholar]
- Abuhussein, H.; Pagni, G.; Rebaudi, A.; Wang, H.-L. The effect of thread pattern upon implant osseointegration. Clin. Oral Implant. Res. 2010, 21, 129–136. [Google Scholar] [CrossRef] [Green Version]
- Al-Thobity, A.M.; Kutkut, A.; Almas, K. Micro threaded implants and crestal bone loss: A systematic review. J. Oral Implantol. 2017, 43, 157–166. [Google Scholar] [CrossRef]
- Stacchi, C.; Lamazza, L.; Rapani, A.; Troiano, G.; Messina, M.; Antonelli, A.; Giudice, A.; Lombardi, T. Marginal bone changes around platform-switching conical connection implants placed 1 or 2 mm subcrestally: A multicenter crossover randomized controlled trial. Clin. Implant. Dent. Relat. Res. 2023, 25, 398–408. [Google Scholar] [CrossRef]
- Dagorne, C.; Malet, J.; Bizouard, G.; Mora, F.; Rangé, H.; Bouchard, P. Clinical evaluation of two dental implant macrostructures on peri-implant bone loss: A comparative, retrospective study. Clin. Oral Implant. Res. 2014, 26, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Boggan, R.; Strong, J.; Misch, C.E.; Bidez, M.W. Influence of hex geometry and prosthetic table width on static and fatigue strength of dental implants. J. Prosthet. Dent. 1999, 82, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Velasco, E.; Monsalve-Guil, L.; Jimenez, A.; Ortiz, I.; Moreno-Muñoz, J.; Nuñez-Marquez, E.; Pegueroles, M.; Perez, R.; Gil, F.J. Importance of the Roughness and Residual Stresses of Dental Implants on Fatigue and Osseointegration Behavior. In Vivo Study in Rabbits. J. Oral Investig. 2016, 42, 469–476. [Google Scholar] [CrossRef]
- Albertini, M.; Yagüe, M.F.; Lazaro, P.; Herrero-Climent, M.; Ríos-Santos, J.; Bullon, P.; Gil, F. Advances in surfaces and osseointegration in implantology. Biomimetic surfaces. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e316–e325. [Google Scholar] [CrossRef] [Green Version]
- Gil, F.J.; Herrero, M.; Lázaro, P.; Rios, J.V. Implant-abutment connections: Influence of the design on the microgap and their fatigue and fracture behavior of dental implants. J. Mater. Sci. Mater. Med. 2014, 25, 1825–1830. [Google Scholar] [CrossRef]
- Aragoneses, J.; Valverde, N.L.; Fernandez-Dominguez, M.; Mena-Alvarez, J.; Rodriguez, C.; Gil, J.; Aragoneses, J.M. Relevant Aspects of Titanium and Zirconia Dental Implants for Their Fatigue and Osseointegration Behaviors. Materials 2022, 15, 4036. [Google Scholar] [CrossRef] [PubMed]
- Gil, J.; Sandino, C.; Cerrolaza, M.; Pérez, R.; Herrero-Climent, M.; Rios-Carrasco, B.; Rios-Santos, J.V.; Brizuela, A. Influence of Bone-Level Dental Implants Placement and of Cortical Thickness on Osseointegration: In Silico and In Vivo Analyses. J. Clin. Med. 2022, 11, 1027. [Google Scholar] [CrossRef]
- Elias, C.N.; Oshida, Y.; Lima, J.H.C.; Muller, C.A. Relationship between surface properties (roughness, wettability and morphology) of titanium and dental implant removal torque. J. Mech. Behav. Biomed. Mater. 2008, 1, 234–242. [Google Scholar] [CrossRef] [Green Version]
- Gittens, R.A.; Scheideler, L.; Rupp, F.; Hyzy, S.L.; Geis-Gerstorfer, J.; Schwartz, Z.; Boyan, B.D. A review on the wettability of dental implant surfaces II: Biological and clinical aspects. Acta Biomater. 2014, 10, 2907–2918. [Google Scholar] [CrossRef] [Green Version]
- Kim, I.-H.; Kwon, T.-Y.; Kim, K.-H. Wetting behavior of dental implants, wetting and wettability. IntechOpen 2015, 9, 253–270. [Google Scholar] [CrossRef] [Green Version]
- Rupp, F.; Scheideler, L.; Eichler, M.; Geis-Gerstorfer, J. Wetting behavior of dental implants. Int. J. Oral Maxillofac. Implant. 2011, 26, 1256–1266. [Google Scholar]
- Herrero-Climent, M.; Lemos, B.F.; Herrero-Climent, F.; Falcao, C.; Oliveira, H.; Herrera, M.; Gil, F.J.; Ríos-Carrasco, B.; Ríos-Santos, J.V. Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. Int. J. Environ. Res. Public Health 2020, 17, 4436. [Google Scholar] [CrossRef] [PubMed]
- De Bruyn, H.; Christiaens, V.; Doornewaard, R.; Jacobsson, M.; Cosyn, J.; Jacquet, W.; Vervaeke, S. Implant surface roughness and patient factors on long-term peri-implant bone loss. Periodontology 2000 2017, 73, 218–227. [Google Scholar] [CrossRef]
- Al-Sabbagh, M.; Eldomiaty, W.; Khabbaz, Y. Can osseointegration be achieved without primary stability? Dent. Clin. N. Am. 2019, 63, 461–473. [Google Scholar] [CrossRef]
- Tabassum, A.; Meijer, G.J.; Wolke, J.G.; Jansen, J.A. Influence of surgical technique and surface roughness on the primary stability of an implant in artificial bone with different cortical thickness: A laboratory study. Clin. Oral Implant. Res. 2010, 21, 213–220. [Google Scholar] [CrossRef]
- Stacchi, C.; Troiano, G.; Montaruli, G.; Mozzati, M.; Lamazza, L.; Antonelli, A.; Giudice, A.; Lombardi, T. Changes in implant stability using different site preparation techniques: Osseodensification drills versus piezoelectric surgery. A multi-center prospective randomized controlled clinical trial. Clin. Implant. Dent. Relat. Res. 2023, 25, 133–140. [Google Scholar] [CrossRef]
- Smeets, R.; Stadlinger, B.; Schwarz, F.; Beck-Broichsitter, B.; Jung, O.; Precht, C.; Kloss, F.; Gröbe, A.; Heiland, M.; Ebker, T. Impact of dental implant surface modifications on osseointegration. BioMed Res. Int. 2016, 2016, 6285620. [Google Scholar] [CrossRef] [Green Version]
- Meredith, N.; Alleyne, D.; Cawley, P. Quantitative determination of the stability of the implant-tissue interface using resonance frequency analysis. Clin. Oral Implant. Res. 1996, 7, 261–267. [Google Scholar] [CrossRef]
- Brizuela-Velasco, A.; Álvarez-Arenal, Á.; Gil-Mur, F.J.; Herrero-Climent, M.; Chávarri-Prado, D.; Chento-Valiente, Y.; Dieguez-Pereira, M. Relationship between insertion torque and resonance frequency measurements, performed by resonance frequency analysis, in micromobility of dental implants. Implant. Dent. 2015, 24, 607–611. [Google Scholar] [CrossRef]
- Romero–Ruiz, M.M.; Gil-Mur, F.J.; Ríos, J.V.; Lázaro, P.; Ríos, B.; Herrero, M. Influence of a novel surface of bioacti ve implants on osseointegration: A comparative and histomorphometric correlation and implant stability study in mini pigs. Int. J. Mol. Sci. 2019, 20, 2307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implication. Periodontology 2000 2008, 47, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Rompen, E.; Da Silva, D.; Lundgren, A.; Gottlow, J.; Sennerby, L. Stability measurements of a double-threaded titanium implant design with turned or oxidised surface. Appl. Osseointegr. Res. 2000, 1, 18–20. [Google Scholar]
- Glauser, R.; Portmann, M.; Ruhstaller, P.; Lundgren, A.; Hammerle, C.; Gottlow, J. Stability measurements of immediately loaded machined and oxidized implants in the posterior maxilla. A comparative study using resonance frequency analysis. Appl. Osseointegr. Res. 2001, 2, 27–29. [Google Scholar]
- Al-Nawas, B.; Groetz, K.A.; Goetz, H.; Duschner, H.; Wagner, W. Comparative histomorphometry and resonance frequency analysis of implants with moderately rough surfaces in a loaded animal model. Clin. Oral Implant. Res. 2007, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Al-Nawas, B.; Hangen, U.; Duschner, H.; Krummenauer, F.; Wagner, W. Turned, machined versus double-etched dental implants in vivo. Clin. Implant. Dent. Relat. Res. 2007, 9, 71–78. [Google Scholar] [CrossRef]
- Sennerby, L.; Persson, L.G.; Berglundh, T.; Wennerberg, A.; Lindhe, J. Implant stability during initiation and resolution of experimental periimplantitis: An experimental study in the dog. Clin. Implant. Dent. Relat. Res. 2005, 7, 136–140. [Google Scholar] [CrossRef]
- Shalabi, M.M.; Wolke, J.G.; Jansen, J.A. The effects of implant surface roughness and surgical technique on implant fixation in an in vitro model. Clin. Oral Implant. Res. 2006, 17, 172–178. [Google Scholar] [CrossRef]
- Rasmusson, L.; Meredith, N.; Kahnberg, K.; Sennerby, L. Effects of barrier membranes on bone resorption and implant stability in onlay bone grafts. An experimental study. Clin. Oral Implant. Res. 1999, 10, 267–277. [Google Scholar] [CrossRef]
- Buser, D.; Mericske-stern, R.; Pierre Bernard, J.P.; Behneke, A.; Behneke, N.; Hirt, H.P.; Belser, U.C.; Lang, N.P. Long term evaluation of non-submerged ITI implants. Part 1; 8-year life table analysis of a prspective multi-center study with 2359 implants. Clin. Oral Implant. Res. 1997, 8, 161–172. [Google Scholar] [CrossRef]
- Pera, F.; Pesce, P.; Menini, M.; Fanelli, F.; Kim, B.-C.; Zhurakivska, K.; Mayer, Y.; Isola, G.; Cianciotta, G.; Crupi, A.; et al. Immediate loading full-arc rehabilitation using transmucosal tissue-level implants with different variables associated: A observational study. Minerva Dent. Oral Sci. 2023; Online ahead of print. [Google Scholar] [CrossRef]
- Lekholm, U.; Zarb, G.A. Patient selection and preparation. In Tissue Integrated Prostheses: Osseointegration in Clinical Dentistry; Branemark, P.I., Zarb, G.A., Albrektsson, T., Eds.; Quintessence Publishing Company: Chicago, IL, USA; Gothenburg, Sweden, 1985; pp. 199–209. [Google Scholar]
- Shapiro, S.; Wilk, M. An analysis of variance test for normality (complete samples). Biometrika 1965, 52, 591–611. [Google Scholar] [CrossRef]
- Mann, H.; Whitney, D. On a Test of Whether one of Two Random Variables is Stochastically Larger than the Other. Ann. Math. Stat. 1947, 18, 50–60. [Google Scholar] [CrossRef]
- Kruskal, W.; Wallis, W. Use of ranks in one-criterion variance analysis. J. Am. Stat. Assoc. 1952, 47, 583–621. [Google Scholar] [CrossRef]
- Dunn, O. Multiple comparisons using rank sums. Technometrics 1964, 6, 241–252. [Google Scholar] [CrossRef]
- Holm, S. Simple sequentially rejective multiple test procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Gil, J.; Pérez, R.; Herrero-Climent, M.; Rizo-Gorrita, M.; Torres-Lagares, D.; Gutiérrez, J.L. Benefits of residual aluminium oxide for sand blasting titanium dental implants: Osseointegration and bactericidal effects. Materials 2022, 15, 178. [Google Scholar] [CrossRef]
- Berglundh, T.; Armitage, G.; Araujo, M.G.; Avila-Ortiz, G.; Blanco, J.; Camargo, P.M.; Chen, S.; Cochran, D.; Derks, J.; Figuero, E.; et al. Peri-Implant Diseases and Conditions: Consensus Report of Workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J. Periodontol. 2018, 89, S313–S318. [Google Scholar] [CrossRef]
- Sul, Y.; Jonsson, J.; Yoon, G.; Johansson, C. Resonance frequency measurements in vivo and related surface properties of magnesium-incorporated micropatterned and magnesium-incorporated TiUnite, Osseotite, SLA and TiOblast implants. Clin. Oral Implant. Res. 2009, 20, 1146–1155. [Google Scholar] [CrossRef]
- Rakic, M.; Galindo-Moreno, P.; Monje, A.; Radovanovic, S.; Wang, H.L.; Cochran, D.; Sculean, A.; Canullo, L. How Frequent Does Peri-Implantitis Occur? A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2018, 22, 1805–1816. [Google Scholar] [CrossRef]
- Menini, M.; Pesce, P.; Delucchi, F.; Ambrogio, G.; Canepa, C.; Carossa, M.; Pera, F. One-stage versus two-stage technique using two splinted extra-short implants: A multicentric split-mouth study with a one-year follow-up. Clin. Implant. Dent. Relat. Res. 2022, 24, 602–610. [Google Scholar] [CrossRef]
- Hänggi, M.P.; Hänggi, D.C.; Schoolfield, J.D.; Meyer, J.; Cochran, D.L.; Hermann, J.S. Crestal bone changes around titanium implants. Part I: A retrospective radiographic evaluation in humans comparing two non-submerged implant designs with different machined collar lengths. J. Periodontol. 2005, 76, 791–802. [Google Scholar] [CrossRef] [Green Version]
- Hermann, J.S.; Buser, D.; Schenk, R.K.; Cochran, D.L. Crestal bone changes around titanium implants. A histometric evaluation of unloaded non-submerged and submerged implants in the canine mandible. J. Periodontol. 2000, 71, 1412–1424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buxadera-Palomero, J.; Godoy-Gallardo, M.; Molmeneu, M.; Punset, M.; Gil, F.J. Antibacterial Properties of Triethoxysilylpropyl Succinic Anhydride Silane (TESPSA) on Titanium Dental Implants. Polymers 2020, 12, 773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Godoy-Gallardo, M.; Guillem-Marti, J.; Sevilla, P.; Manero, J.M.; Gil, F.J.; Rodriguez, D. Anhydride-Functional Silane Immobilized onto Titanium Surfaces Induces Osteoblast Cell Differentiation and Reduces Bacterial Adhesion and Biofilm Formation. Mater. Sci. Eng. C 2016, 59, 524–532. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hotchkiss, K.M.; Reddy, G.B.; Hyzy, S.L.; Schwartz, Z.; Boyan, B.D.; Olivares-Navarrete, R. Titanium surface characteristics, including topography and wettability, alter macrophage activation. Acta Biomater. 2016, 31, 425–434. [Google Scholar] [CrossRef] [Green Version]
- Shalabi, M.; Gortemaker, A.; Hof, M.V.; Jansen, J.; Creugers, N. Implant surface roughness and bone healing: A systematic review. J. Dent. Res. 2006, 85, 496–500. [Google Scholar] [CrossRef]
- Robles, D.; Brizuela, A.; Fernández-Domínguez, M.; Gil, J. Corrosion Resistance and Titanium Ion Release of Hybrid Dental Implants. Materials 2023, 16, 3650. [Google Scholar] [CrossRef]
- Camps-Font, O.; Toledano-Serrabona, J.; Juiz-Camps, A.; Gil, J.; Sánchez-Garcés, M.A.; Figueiredo, R.; Gay-Escoda, C.; Valmaseda-Castellón, E. Effect of Implantoplasty on Roughness, Fatigue and Corrosion Behavior of Narrow Diameter Dental Implants. J. Funct. Biomater. 2023, 14, 61. [Google Scholar] [CrossRef]
- Toledano-Serrabona, J.; Bosch, B.M.; Diez-Tercero, L.; Gil, F.J.; Camps-Font, O.; Valmaseda-Castellón, E.; Gay-Escoda, C.; Sanchez-Garcés, M.A. Evaluation of the inflammatory and osteogenic response induced by titanium particles released during implantoplasty of dental implants. Sci. Rep. 2022, 12, 15790. [Google Scholar] [CrossRef]






| Samples | Sa (µm) | Sz (µm) | S Area Index | |||
|---|---|---|---|---|---|---|
| Average | Desv.est. | Average | Desv.est. | Average | Desv.est. | |
| A | 0.55 | 0.01 | 3.47 | 1.53 | 1.04 | 0.01 |
| B | 0.54 | 0.07 | 16.74 | 1.11 | 1.03 | 0.01 |
| C | 3.85 | 0.18 | 20.96 | 1.65 | 1.74 | 0.05 |
| D | 2.76 | 0.21 | 19.65 | 2.00 | 1.13 | 0.07 |
| E | 1.60 | 0.22 | 13.42 | 2.54 | 1.66 | 0.10 |
| F | 1.67 | 0.19 | 19.72 | 3.02 | 1.88 | 0.09 |
| Samples | A | B | C | D | E | F |
|---|---|---|---|---|---|---|
| Mean | 90.88 | 92.34 | 76.70 | 78.45 | 80.92 | 82.32 |
| Standard Dev. | 5.90 | 6.00 | 3.09 | 2.90 | 1.85 | 1.97 |
| Implants | Sa | IT | ISQ | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Median | Mean | SD | Median | |
| A | 0.55 | 0.01 | 25.85 | 10.44 | 24 | 64.13 | 5.40 | 65.50 |
| B | 0.54 | 0.07 | 29.41 | 11.84 | 28 | 70.77 | 8.59 | 74.00 |
| C | 3.85 | 0.18 | 28.44 | 11.40 | 26 | 63.08 | 8.12 | 64.00 |
| D | 2.76 | 0.21 | 14.69 | 4.35 | 15 | 73.04 | 4.43 | 74.00 |
| E | 1.60 | 0.22 | 29.00 | 11.01 | 27 | 59.68 | 9.51 | 62.00 |
| F | 1.67 | 0.19 | 15.28 | 7.40 | 14 | 72.03 | 5.73 | 72.50 |
| Essential Moderately Rough Surface | Essential Rough Surface | VEGA Minimally Rough Surface | VEGA Moderately Rough Surface | VEGA Rough Surface | |
|---|---|---|---|---|---|
| Essential minimally rough surface | |||||
| Essential moderately rough surface | |||||
| Essential rough surface | 1 | ||||
| VEGA minimally rough surface | |||||
| VEGA moderately rough surface |
| Essential Moderately Rough Surface | Essential Rough Surface | VEGA Minimally Rough Surface | VEGA Moderately Rough Surface | VEGA Rough Surface | |
|---|---|---|---|---|---|
| Essential minimally rough surface | |||||
| Essential moderately rough surface | |||||
| Essential rough surface | |||||
| VEGA minimally rough surface | 1 | ||||
| VEGA moderately rough surface |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero, M.; Herrero-Climent, M.; Ríos-Carrasco, B.; Brizuela, A.; Romero, M.M.; Gil, J. Investigation of the Influence of Roughness and Dental Implant Design on Primary Stability via Analysis of Insertion Torque and Implant Stability Quotient: An In Vitro Study. J. Clin. Med. 2023, 12, 4190. https://doi.org/10.3390/jcm12134190
Romero M, Herrero-Climent M, Ríos-Carrasco B, Brizuela A, Romero MM, Gil J. Investigation of the Influence of Roughness and Dental Implant Design on Primary Stability via Analysis of Insertion Torque and Implant Stability Quotient: An In Vitro Study. Journal of Clinical Medicine. 2023; 12(13):4190. https://doi.org/10.3390/jcm12134190
Chicago/Turabian StyleRomero, Marta, Mariano Herrero-Climent, Blanca Ríos-Carrasco, Aritza Brizuela, Manuel María Romero, and Javier Gil. 2023. "Investigation of the Influence of Roughness and Dental Implant Design on Primary Stability via Analysis of Insertion Torque and Implant Stability Quotient: An In Vitro Study" Journal of Clinical Medicine 12, no. 13: 4190. https://doi.org/10.3390/jcm12134190
APA StyleRomero, M., Herrero-Climent, M., Ríos-Carrasco, B., Brizuela, A., Romero, M. M., & Gil, J. (2023). Investigation of the Influence of Roughness and Dental Implant Design on Primary Stability via Analysis of Insertion Torque and Implant Stability Quotient: An In Vitro Study. Journal of Clinical Medicine, 12(13), 4190. https://doi.org/10.3390/jcm12134190








