Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders Associated with Tinnitus: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Data Management and Selection of Studies
2.4. Data Extraction
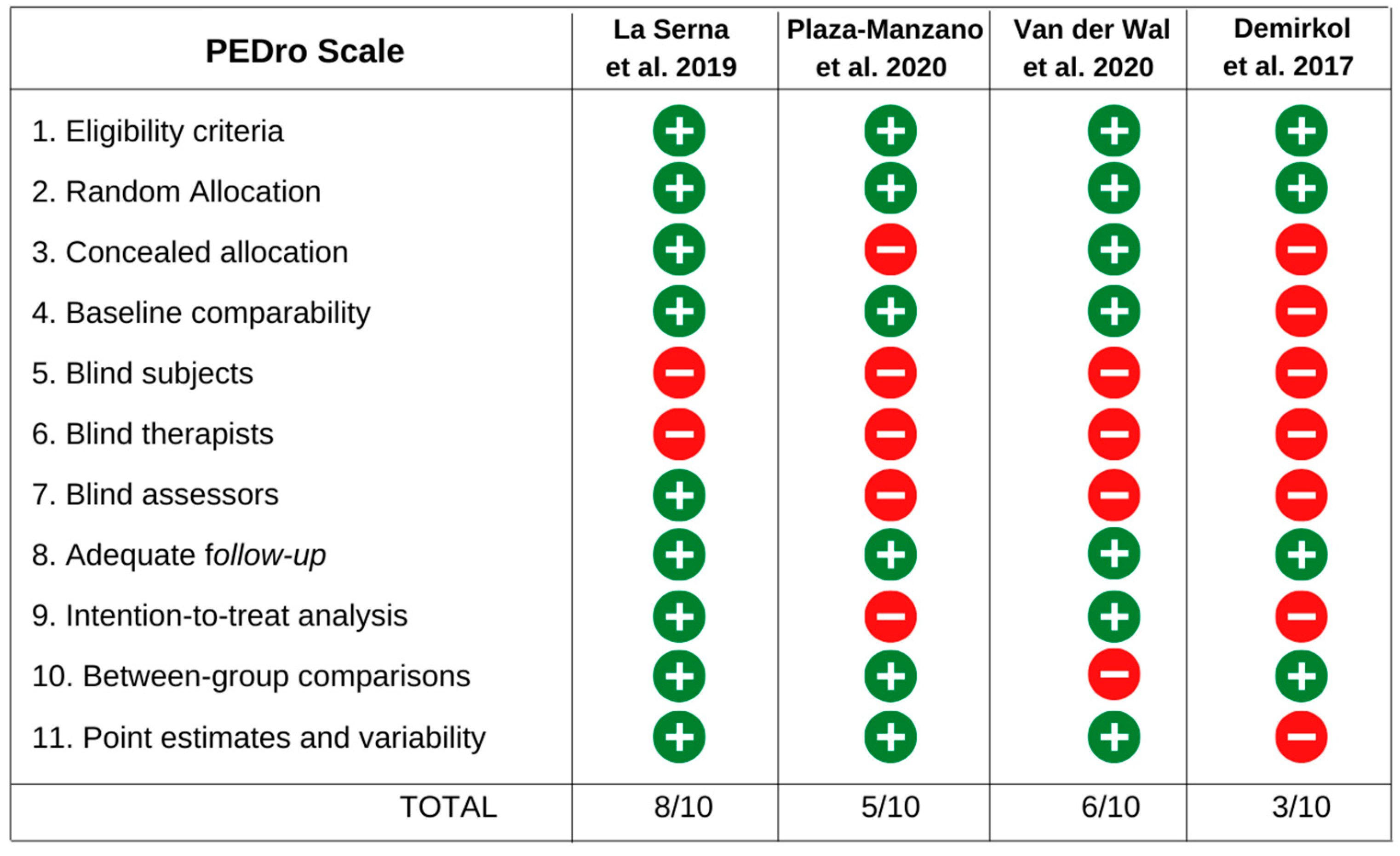
2.5. Assessment of the Risk of Bias in Included Studies
2.6. Data Analysis
2.7. Patients and Public Involvement
3. Results
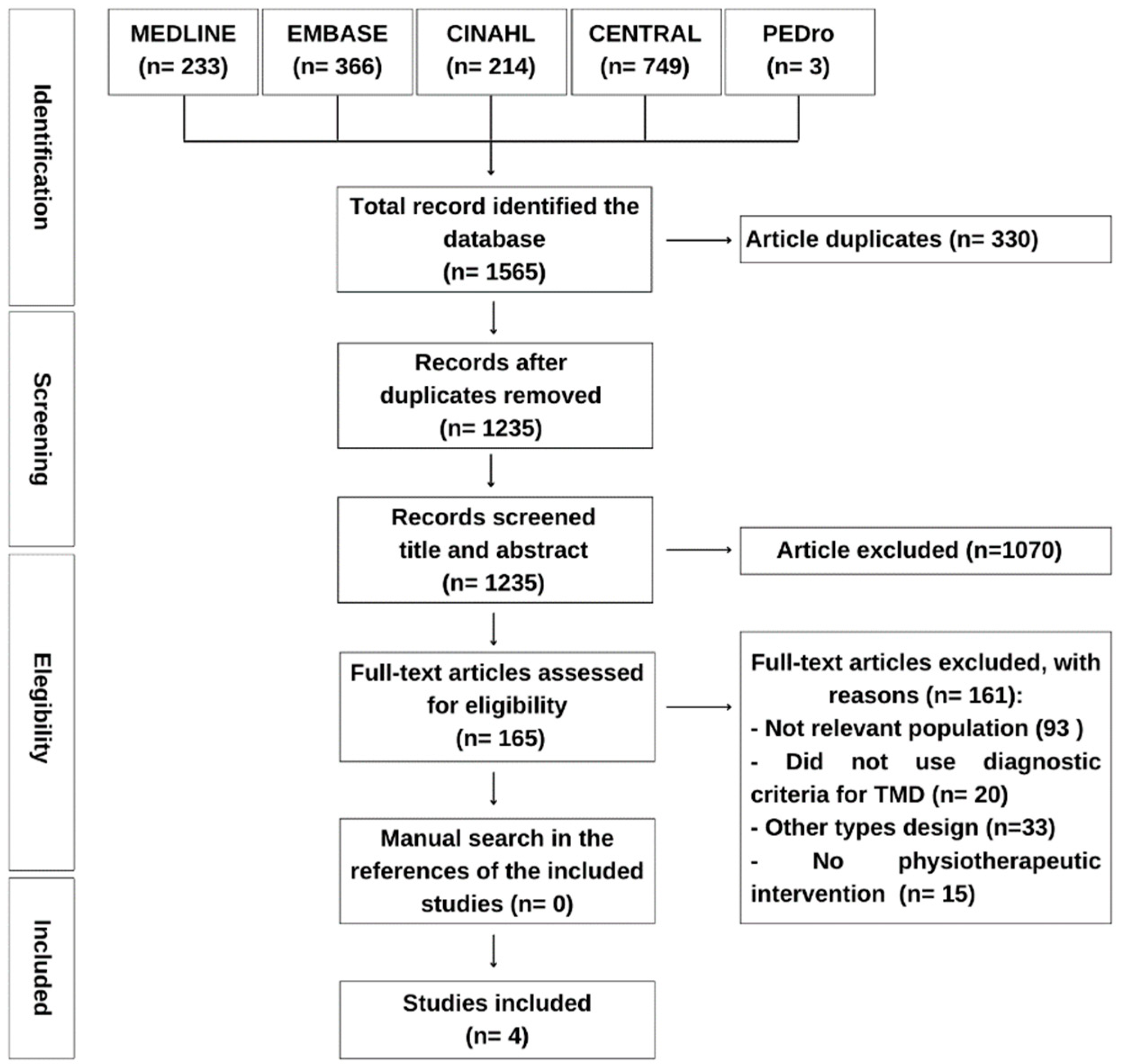
3.1. Study Selection
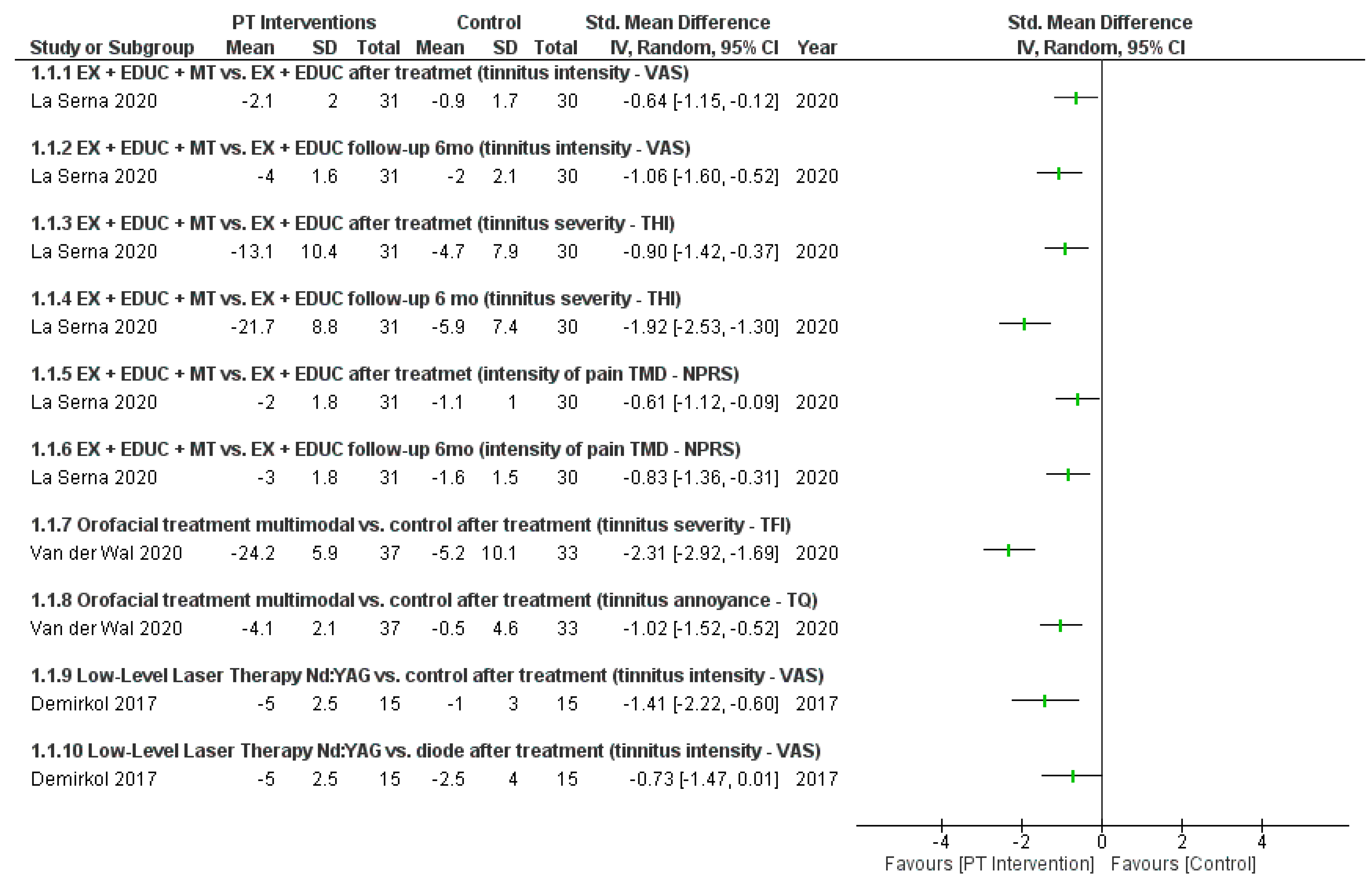
3.2. Interventions
3.3. Methodological Quality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ohrbach, R.; Dworkin, S.F. AAPT Diagnostic Criteria for Chronic Painful Temporomandibular Disorders. J. Pain 2019, 20, 1276–1292. [Google Scholar] [CrossRef] [PubMed]
- Valesan, L.F.; Da-Cas, C.D.; Réus, J.C.; Denardin, A.C.S.; Garanhani, R.R.; Bonotto, D.; Januzzi, E.; de Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Bagis, B.; Ayaz, E.A.; Turgut, S.; Durkan, R.; Özcan, M. Gender Difference in Prevalence of Signs and Symptoms of Temporomandibular Joint Disorders: A Retro-spective Study on 243 Consecutive Patients. Int. J. Med. Sci. 2012, 9, 539–544. [Google Scholar] [CrossRef] [PubMed]
- Conti, P.C.R.; Pinto-Fiamengui, L.M.S.; Cunha, C.O.; Conti, A.C.d.C.F. Orofacial Pain and Temporomandibular Disorders: The Impact on Oral Health and Quality of Life. Braz. Oral Res. 2012, 26, 120–123. [Google Scholar] [CrossRef]
- Costa, Y.M.; Conti, P.C.R.; de Faria, F.A.C.; Bonjardim, L.R. Temporomandibular Disorders and Painful Comorbidities: Clinical Association and Underlying Mechanisms. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 288–297. [Google Scholar] [CrossRef]
- Silveira, A.; Gadotti, I.C.; Armijo-Olivo, S.; Biasotto-Gonzalez, D.A.; Magee, D. Jaw Dysfunction Is Associated with Neck Disability and Muscle Tenderness in Subjects with and without Chronic Temporomandibular Disorders. BioMed Res. Int. 2015, 2015, 512792. [Google Scholar] [CrossRef]
- Porto De Toledo, I.; Stefani, F.M.; Porporatti, A.L.; Mezzomo, L.A.; Peres, M.A.; Flores-Mir, C.; De Luca Canto, G. Prevalence of Otologic Signs and Symptoms in Adult Patients with Temporomandibular Disorders: A Systematic Review and Me-ta-Analysis. Clin. Oral Investig. 2017, 21, 597–605. [Google Scholar] [CrossRef]
- Baguley, D.; McFerran, D.; Hall, D. Tinnitus. Lancet 2013, 382, 1600–1607. [Google Scholar] [CrossRef]
- McCormack, A.; Edmondson-Jones, M.; Somerset, S.; Hall, D. A Systematic Review of the Reporting of Tinnitus Prevalence and Severity. Hear. Res. 2016, 337, 70–79. [Google Scholar] [CrossRef]
- Levine, R.A.; Nam, E.C.; Oron, Y.; Melcher, J.R. Evidence for a Tinnitus Subgroup Responsive to Somatosensory Based Treatment Modalities. Prog. Brain Res. 2007, 166, 195–207. [Google Scholar] [CrossRef]
- Buergers, R.; Kleinjung, T.; Behr, M.; Vielsmeier, V. Is There a Link between Tinnitus and Temporomandibular Disorders? J. Prosthet. Dent. 2014, 111, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Olivo, M.; Martini, A. Prevalence of Tinnitus in Patients with Different Temporomandibular Disorders Symptoms. Int. Tinnitus J. 2015, 19, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Bousema, E.J.; Koops, E.A.; van Dijk, P.; Dijkstra, P.U. Association Between Subjective Tinnitus and Cervical Spine or Temporomandibular Disorders: A Systematic Review. Trends Hear. 2018, 22, 2331216518800640. [Google Scholar] [CrossRef] [PubMed]
- Vielsmeier, V.; Strutz, J.; Kleinjung, T.; Schecklmann, M.; Kreuzer, P.M.; Land-grebe, M.; Langguth, B. Temporomandibular Joint Disorder Complaints in Tinnitus: Further Hints for a Putative Tinnitus Subtype. PLoS ONE 2012, 7, e38887. [Google Scholar] [CrossRef]
- Edvall, N.K.; Gunan, E.; Genitsaridi, E.; Lazar, A.; Mehraei, G.; Billing, M.; Tull-berg, M.; Bulla, J.; Whitton, J.; Canlon, B.; et al. Impact of Temporomandibular Joint Complaints on Tinnitus-Related Distress. Front. Neurosci. 2019, 13, 879. [Google Scholar] [CrossRef]
- Ginszt, M.; Szkutnik, J.; Zieliński, G.; Bakalczuk, M.; Stodółkiewicz, M.; Litko-Rola, M.; Ginszt, A.; Rahnama, M.; Majcher, P. Cervical Myofascial Pain Is Associated with an Imbalance of Masticatory Muscle Activity. Int. J. Environ. Res. Public Health 2022, 19, 1577. [Google Scholar] [CrossRef] [PubMed]
- Shore, S.; Zhou, J.; Koehler, S. Neural Mechanisms Underlying Somatic Tinnitus. Prog. Brain Res. 2007, 166, 107–123. [Google Scholar] [CrossRef]
- Rocha, C.B.; Sanchez, T.G. Efficacy of Myofascial Trigger Point Deactivation for Tinnitus Control. Braz. J. Otorhinolaryngol. 2012, 78, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Rocha, C.A.C.; Sanchez, T.G.; Tesseroli De Siqueira, J.T. Myofascial Trigger Point: A Possible Way of Modulating Tinnitus. Audiol. Neurotol. 2008, 13, 153–160. [Google Scholar] [CrossRef]
- Westcott, M.; Sanchez, T.; Diges, I.; Saba, C.; Dineen, R.; McNeill, C.; Chiam, A.; O’Keefe, M.; Sharples, T. Tonic Tensor Tympani Syndrome in Tinnitus and Hyperacusis Patients: A Multi-Clinic Prevalence Study. Noise Health 2013, 15, 117–128. [Google Scholar] [CrossRef]
- Parker, W.S.; Chole, R.A. Tinnitus, Vertigo, and Temporomandibular Disorders. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Mottaghi, A.; Menéndez-Díaz, I.; Cobo, J.L.; González-Serrano, J.; Cobo, T. Is There a Higher Prevalence of Tinnitus in Patients with Temporomandibular Disorders? A Systematic Review and Meta-Analysis. J. Oral Rehabil. 2019, 46, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Vielsmeier, V.; Kleinjung, T.; Strutz, J.; Bürgers, R.; Kreuzer, P.M.; Langguth, B. Tinnitus with Temporomandibular Joint Disorders: A Specific Entity of Tinnitus Patients? Otolaryngol.-Head Neck Surg. 2011, 145, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Gauer, R.L.; Semidey, M.J. Diagnosis and Treatment of Temporomandibular Disorders. Am. Fam. Physician 2015, 91, 378–386. [Google Scholar]
- Gil-Martinez, A.; Paris-Alemany, A.; López-de-Uralde-Villanueva, I.; La Touche, R. Management of Pain in Patients with Temporomandibular Disorder (TMD): Challenges and Solutions. J. Pain Res. 2018, 11, 571–587. [Google Scholar] [CrossRef]
- McNeely, M.L.; Armijo Olivo, S.; Magee, D.J. A Systematic Review of the Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders. Phys. Ther. 2006, 86, 710–725. [Google Scholar] [CrossRef]
- Feitoza, C.C.; de Lemos Menezes, P. Prognosis of Conservative Treatment in Individuals with Temporomandibular Disorders and Tinnitus: A Systematic Review. Muscle Ligaments Tendons J. 2019, 8, 123. [Google Scholar] [CrossRef]
- Michiels, S.; Nieste, E.; Van de Heyning, P.; Braem, M.; Visscher, C.; Topsakal, V.; Gilles, A.; Jacquemin, L.; De Hertogh, W. Does Conservative Temporomandibular Therapy Affect Tinnitus Complaints? A Systematic Review. J. Oral Facial Pain Headache 2019, 33, 308–317. [Google Scholar] [CrossRef]
- Sharma, P.; Singh, G.; Kothiyal, S.; Goyal, M. Effects of Manual Therapy in Somatic Tinnitus Patients Associated with Cervicogenic and Temporomandibular Dysfunction Domain: Systematic Review and Meta Analysis of Randomized Controlled Trials. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 247–253. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Altman, D.; Antes, G.; Atkins, D.; Barbour, V.; Barrowman, N.; Berlin, J.A.; et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Dworkin, S.F.; LeResche, L. Research Diagnostic Criteria for Temporomandibular Disorders: Review, Criteria, Examinations and Specifications, Critique. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Innervations. Version 5; The Cochrane Collaboration. 2011. Available online: https://training.cochrane.org/handbook (accessed on 1 December 2022).
- Staniszewska, S.; Brett, J.; Simera, I.; Seers, K.; Mockford, C.; Goodlad, S.; Altman, D.G.; Moher, D.; Barber, R.; Denegri, S.; et al. GRIPP2 Reporting Checklists: Tools to Improve Reporting of Patient and Public Involvement in Research. BMJ 2017, 358, j3453. [Google Scholar] [CrossRef] [PubMed]
- Delgado de la Serna, P.; Plaza-Manzano, G.; Cleland, J.; Fernández-de-las-Peñas, C.; Martín-Casas, P.; Díaz-Arribas, M.J. Effects of Cervico-Mandibular Manual Therapy in Patients with Temporomandibular Pain Disorders and Associated Somatic Tinnitus: A Randomized Clinical Trial. Pain Med. 2020, 21, 613–624. [Google Scholar] [CrossRef]
- Demirkol, N.; Usumez, A.; Demirkol, M.; Sari, F.; Akcaboy, C. Efficacy of Low-Level Laser Therapy in Subjective Tinnitus Patients with Temporomandibular Disorders. Photomed. Laser Surg. 2017, 35, 427–431. [Google Scholar] [CrossRef]
- Plaza-Manzano, G.; Delgado-de-la-Serna, P.; Diaz-Arribas, M.J.; Rodrigues-de-Souza, D.P.; Fernandez-de-las-Penas, C.; Alburquerque-Sendin, F. Influence of Clinical, Physical, Psychological, and Psychophysical Variables on Treatment Out-comes in Somatic Tinnitus Associated With Temporomandibular Pain: Evidence From a Randomized Clinical Trial. Pain Pract. 2020, 21, 8–17. [Google Scholar] [CrossRef]
- Van der Wal, A.; Michiels, S.; Van de Heyning, P.; Braem, M.; Visscher, C.M.; Top-sakal, V.; Gilles, A.; Jacquemin, L.; Van Rompaey, V.; De Hertogh, W. Treatment of Somatosensory Tinnitus: A Randomized Controlled Trial Studying the Effect of Orofacial Treatment as Part of a Multidisciplinary Program. J. Clin. Med. 2020, 9, 705. [Google Scholar] [CrossRef] [PubMed]
- Lomas, J.; Gurgenci, T.; Jackson, C.; Campbell, D. Temporomandibular Dysfunction. Aust. J. Gen. Pract. 2018, 47, 212–215. [Google Scholar] [CrossRef]
- Hilgenberg, P.B.; Saldanha, A.D.D.; Cunha, C.O.; Rubo, J.H.; Conti, P.C.R. Temporomandibular Disorders, Otologic Symptoms and Depression Levels in Tinnitus Patients. J. Oral Rehabil. 2012, 39, 239–244. [Google Scholar] [CrossRef]
- Nascimento, I.d.P.; Almeida, A.A.; Diniz, J.; Martins, M.L.; de Freitas, T.M.M.W.C.; da Rosa, M.R.D. Tinnitus Evaluation: Relationship between Pitch Matching and Loudness, Visual Analog Scale and Tinnitus Handicap Inventory. Braz. J. Otorhino-laryngol. 2019, 85, 611–616. [Google Scholar] [CrossRef]
- Adamchic, I.; Langguth, B.; Hauptmann, C.; Alexander Tass, P. Psychometric Evaluation of Visual Analog Scale for the Assessment of Chronic Tinnitus. Am. J. Audiol. 2012, 21, 215–225. [Google Scholar] [CrossRef]
- Schaffer, M.; Bonel, H.; Sroka, R.; Schaffer, P.; Busch, M.; Reiser, M.; Dühmke, E. Effects of 780 Nm Diode Laser Irradiation on Blood Microcirculation: Preliminary Findings on Time-Dependent T1-Weighted Contrast-Enhanced Magnetic Resonance Imaging (MRI). J. Photochem. Photobiol. B Biol. 2000, 54, 55–60. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Huang, C.Y.; Chang, C.Y.; Cheng, Y.F. Efficacy of Low-Level Laser Therapy for Tinnitus: A Systematic Review with Meta-Analysis and Trial Sequential Analysis. Brain Sci. 2020, 10, 931. [Google Scholar] [CrossRef] [PubMed]
- Tullberg, M.; Ernberg, M. Long-Term Effect on Tinnitus by Treatment of Temporomandibular Disorders: A Two-Year Follow-up by Questionnaire. Acta Odontol. Scand. 2006, 64, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Jacquemin, L.; Mertens, G.; Van de Heyning, P.; Vanderveken, O.M.; Topsakal, V.; De Hertogh, W.; Michiels, S.; Van Rompaey, V.; Gilles, A. Sensitivity to Change and Convergent Validity of the Tinnitus Functional Index (TFI) and the Tinnitus Questionnaire (TQ): Clinical and Research Perspectives. Hear. Res. 2019, 382, 107796. [Google Scholar] [CrossRef]
- Ebrahim, S.; Montoya, L.; Busse, J.W.; Carrasco-Labra, A.; Cuyatt, C.H. The Effectiveness of Splint Therapy in Patients with Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Am. Dent. Assoc. 2012, 143, 847–857. [Google Scholar] [CrossRef]
- Racine, M.; Tousignant-Laflamme, Y.; Kloda, L.A.; Dion, D.; Dupuis, G.; Choinière, M. A Systematic Literature Review of 10 Years of Research on Sex/Gender and Experimental Pain Perception—Part 1: Are There Really Differences between Women and Men? Pain 2012, 153, 602–618. [Google Scholar] [CrossRef]
- La Touche, R.; Martínez García, S.; Serrano García, B.; Proy Acosta, A.; Adraos Juárez, D.; Fernández Pérez, J.J.; Angulo-Díaz-Parreño, S.; Cuenca-Martínez, F.; Par-is-Alemany, A.; Suso-Martí, L. Effect of Manual Therapy and Therapeutic Exercise Ap-plied to the Cervical Region on Pain and Pressure Pain Sensitivity in Patients with Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Pain Med. 2020, 21, 2373–2384. [Google Scholar] [CrossRef]
- Calixtre, L.B.; Moreira, R.F.C.; Franchini, G.H.; Alburquerque-Sendín, F.; Oliveira, A.B. Manual Therapy for the Management of Pain and Limited Range of Motion in Subjects with Signs and Symptoms of Temporomandibular Disorder: A Systematic Re-view of Randomised Controlled Trials. J. Oral Rehabil. 2015, 42, 847–861. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Pitance, L.; Singh, V.; Neto, F.; Thie, N.; Michelotti, A. Effectiveness of Manual Therapy and Therapeutic Exercise for Temporomandibular Disorders: Systematic Review and Meta-Analysis. Phys. Ther. 2016, 96, 9–25. [Google Scholar] [CrossRef]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sports Phys. Ther. 2018, 48, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.G. Understanding Effective Treatments of Myofascial Trigger Points. J. Bodyw. Mov. Ther. 2002, 6, 81–88. [Google Scholar] [CrossRef]
- Hou, C.; Tsai, L.; Cheng, K.; Chung, K.; Hong, C. Immediate Effects of Various Physical Therapeutic Modalities on Cervical Myofascial Pain and Trigger-Point Sensitivity. Arch. Phys. Med. Rehabil. 2002, 83, 1406–1414. [Google Scholar] [CrossRef]
- Shimada, A.; Ishigaki, S.; Matsuka, Y.; Komiyama, O.; Torisu, T.; Oono, Y.; Sato, H.; Naganawa, T.; Mine, A.; Yamazaki, Y.; et al. Effects of Exercise Therapy on Painful Temporomandibular Disorders. J. Oral Rehabil. 2019, 46, 475–481. [Google Scholar] [CrossRef]
- Häggman-Henrikson, B.; Liv, P.; Ilgunas, A.; Visscher, C.M.; Lobbezoo, F.; Durham, J.; Lövgren, A. Increasing Gender Differences in the Prevalence and Chronification of Orofacial Pain in the Population. Pain 2020, 161, 1768–1775. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The Efficacy of Pain Neuroscience Education on Musculoskeletal Pain: A Systematic Review of the Literature. Physiother. Theory Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef] [PubMed]
- Langguth, B.; Kreuzer, P.M.; Kleinjung, T.; De Ridder, D. Tinnitus: Causes and Clinical Management. Lancet Neurol. 2013, 12, 920–930. [Google Scholar] [CrossRef]
| Study and Country | Sample | Average Age (years) | Intervention Group | Comparison Group | Frequency and Duration of Intervention | Outcomes and Evaluation Measures | Follow-Up | Results |
|---|---|---|---|---|---|---|---|---|
| La Serna et al. (2020) [35] Spain Plaza-Manzano et al. (2020) [37] Spain | GI: 31 (12 M e 19 W) GC: 30 (13 M e 17 W) | GI: 42.5 (±12.0) GC: 44 (±10.5) | Education based on pain mechanisms, coping strategies and changing habits. Mobility, posture, TMJ motor control, tongue and neck exercises. Mandibular mobilization and soft tissue techniques in the massater, temporalis, SCOM and upper trapezius. | Education based on pain mechanisms, coping strategies and changing habits. Mobility, posture, TMJ motor control, tongue and neck exercises. | 6 sessions of 30 min in 4 weeks. | Intensity of TMDs pain (NPRS), PPT (algometry), tinnitus severity (VAS), tinnitus report (THI), incapacity (CF-PDI) and quality of life (SF-12). | 3 months 6 months | The exercise/education plus manual therapy group showed better outcomes in intensity of TMDs pain, tinnitus severity, PPT and incapacity. The follow-up three and six months theses outcomes proved significantly better. However, similar changes for the quality of life as the exercise/education alone group. In Both groups of treatment higher scores of tinnitus severity predicted better outcomes 3 and 6 months pos-intervention (p = 0.001). In addition, lower PPTs in the temporalis muscle predicted poorer clinical outcomes (p < 0.005). In group with manual therapy higher scores THI predicted better outcomes post-intervention (p < 0.005). |
| Van der Wal et al. (2020) [38] Belgium | GI: 40 (18 M e 22 W) GC: 40 (24 M e 16 W) | GI: 46 (±13) GC: 45 (±15) | Counselling, stretching, masticatory muscle massage and relaxation therapy. For patients with cervical dysfunctions, mobilizations and exercises for the region were added (early-started group). | Participants remained on the waiting list for 9 weeks, after which they also underwent the same intervention (delayed-started group). | 18 sessions in 9 weeks. | Tinnitus annoyance (TQ) and tinnitus severity (TFI). | 9 weeks 18 weeks | There was a clinically important and statistically significant (p < 0.005) reduction in the TQ and TFI score immediately after the intervention and at follow-up. |
| Demirkol et al. (2017) [36] Turkey | GI: 15 (7 M e 8 W) GC: 16 (10 M e 6 W) GP: 15 (6 M e 9 W) | GI: 36.6 (±14. 7) GC: 40.1 (±14.6) GP: 37.7 (±13.8) | Application of the Nd:YAG laser, 20 s continuously in the external acoustic meatus, with output power of 0.25 W, pulse duration 1000 ls (VLP mode), frequency of 10 Hz, pulse energy of 25 mJ, 25 W of power of peak and energy density of 8 J/cm2. | Application of 810 mn diode laser, 9 s continuously in the external acoustic meatus, with energy density of 8 J/cm2 and output power of 0.25 W. Placebo laser was applied anteromedially to the external acoustic meatus, without irradiation. | 10 sessions in 2 weeks. | Tinnitus intensity (VAS) | 1 month | In the two groups that received the laser, there was a reduction in tinnitus intensity after one month of treatment (p < 0.001). The group receiving Nd:YAG showed greater percentage improvement in tinnitus severity (p < 0.001). |
| Certainty Assessment | No. of Patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Manual Therapy, Exercise and Education | Exercise and Education | Relative (95% CI) | Absolute (95% CI) | |
| Intensity of pain after treatment (follow-up: mean 6 months; assessed with NPRS: scale from 0 to 10) | |||||||||||
| 1 | Randomized trials | Not serious | Not serious | Not serious | Serious a | None | 30 | 31 | - | SMD 0.61 SD lower (1.12 lower to 0.09 lower) | ⊕⊕⊕◯ Moderate |
| Tinnitus intensity after treatment (follow-up: mean 6 months; assessed with VAS: scale from 0 to 10) | |||||||||||
| 1 | Randomized trials | Not serious | Not serious | Not serious | Serious a | None | 30 | 31 | - | SMD 0.64 SD lower (1.15 lower to 0.12 lower) | ⊕⊕⊕◯ Moderate |
| Tinnitus severity after treatment (assessed with THI: scale from 0 to 100) | |||||||||||
| 1 | Randomized trials | Not serious | Not serious | Not serious | Serious a | None | 31 | 30 | - | SMD 0.9 SD lower (1.42 lower to 0.37 lower) | ⊕⊕⊕◯ Moderate |
| Certainty Assessment | No. of Patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Orofacial Treatment Multimodal | Control | Relative (95% CI) | Absolute (95% CI) | |
| Tinnitus annoyance after treatment (assessed with TQI: scale from 0 to 84) | |||||||||||
| 1 | Randomized trials | Serious | Not serious | Not serious | Serious a | None | 33 | 33 | - | SMD 1.02 SD lower (1.52 lower to 0.52 lower) | ⊕⊕◯◯ Low |
| Tinnitus severity after treatment (assessed with TFI: scale from 0 to 100) | |||||||||||
| 1 | Randomized trials | Serious | Not serious | Not serious | Serious a | None | 33 | 33 | - | SMD 2.31 SD lower (2.92 lower to 1.69 lower) | ⊕⊕◯◯ Low |
| Certainty Assessment | No. of Patients | Effect | Certainty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Low-Level Laser Therapy Nd:Yag | Control | Relative (95% CI) | Absolute (95% CI) | |
| Tinnitus intensity (follow-up: median 1 months; assessed with VAS: scale from 0 to 10) | |||||||||||
| 1 | Randomized trials | Serious | Not serious | Not serious | Serious a | None | 15 | 15 | - | SMD 1.41 SD lower (2.22 lower to 0.6 lower) | ⊕⊕◯◯ Low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, M.T.; Silva, C.; Silva, J.; Costa, M.; Gadotti, I.; Ribeiro, K. Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders Associated with Tinnitus: A Systematic Review. J. Clin. Med. 2023, 12, 4329. https://doi.org/10.3390/jcm12134329
da Silva MT, Silva C, Silva J, Costa M, Gadotti I, Ribeiro K. Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders Associated with Tinnitus: A Systematic Review. Journal of Clinical Medicine. 2023; 12(13):4329. https://doi.org/10.3390/jcm12134329
Chicago/Turabian Styleda Silva, Marianne Trajano, Carlos Silva, Jade Silva, Mateus Costa, Inae Gadotti, and Karyna Ribeiro. 2023. "Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders Associated with Tinnitus: A Systematic Review" Journal of Clinical Medicine 12, no. 13: 4329. https://doi.org/10.3390/jcm12134329
APA Styleda Silva, M. T., Silva, C., Silva, J., Costa, M., Gadotti, I., & Ribeiro, K. (2023). Effectiveness of Physical Therapy Interventions for Temporomandibular Disorders Associated with Tinnitus: A Systematic Review. Journal of Clinical Medicine, 12(13), 4329. https://doi.org/10.3390/jcm12134329