Factors Affecting Transcranial Motor-Evoked Potential Measurements Using Single-Train Stimulation with an Increased Number of Pulses during Adolescent Scoliosis Surgery: A Prospective Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Anesthesia and Monitoring Technique
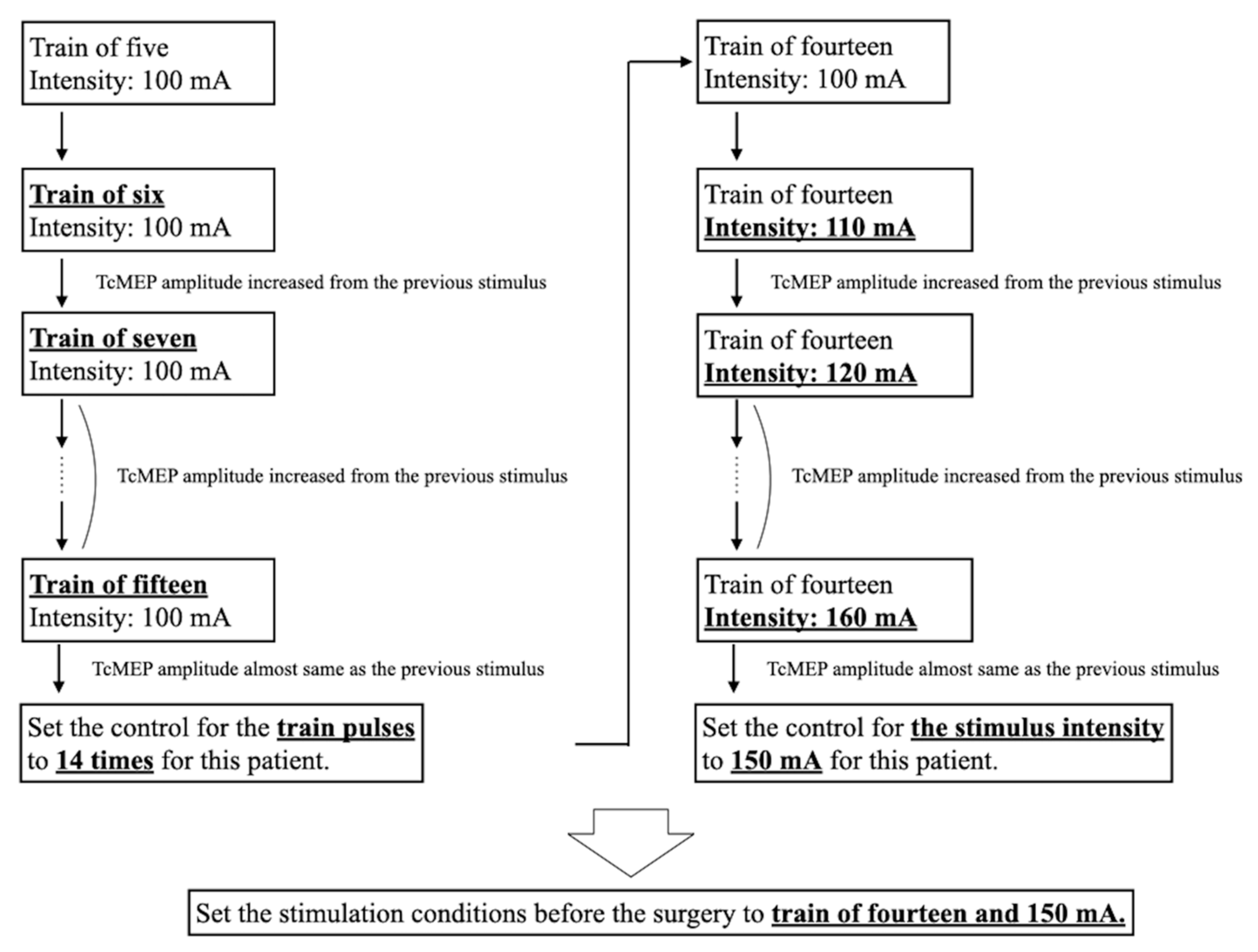
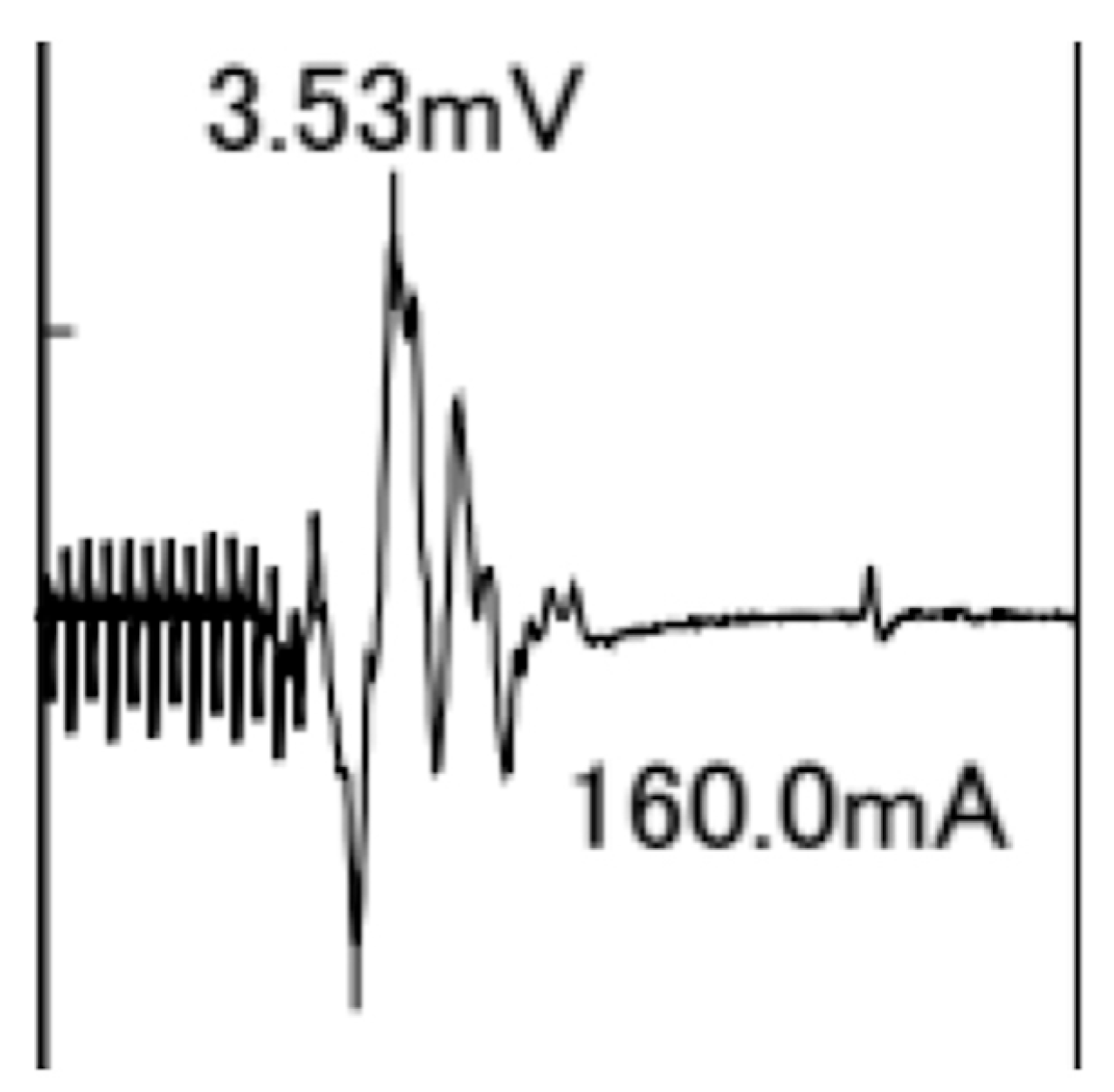
2.3. TcMEP Measurements
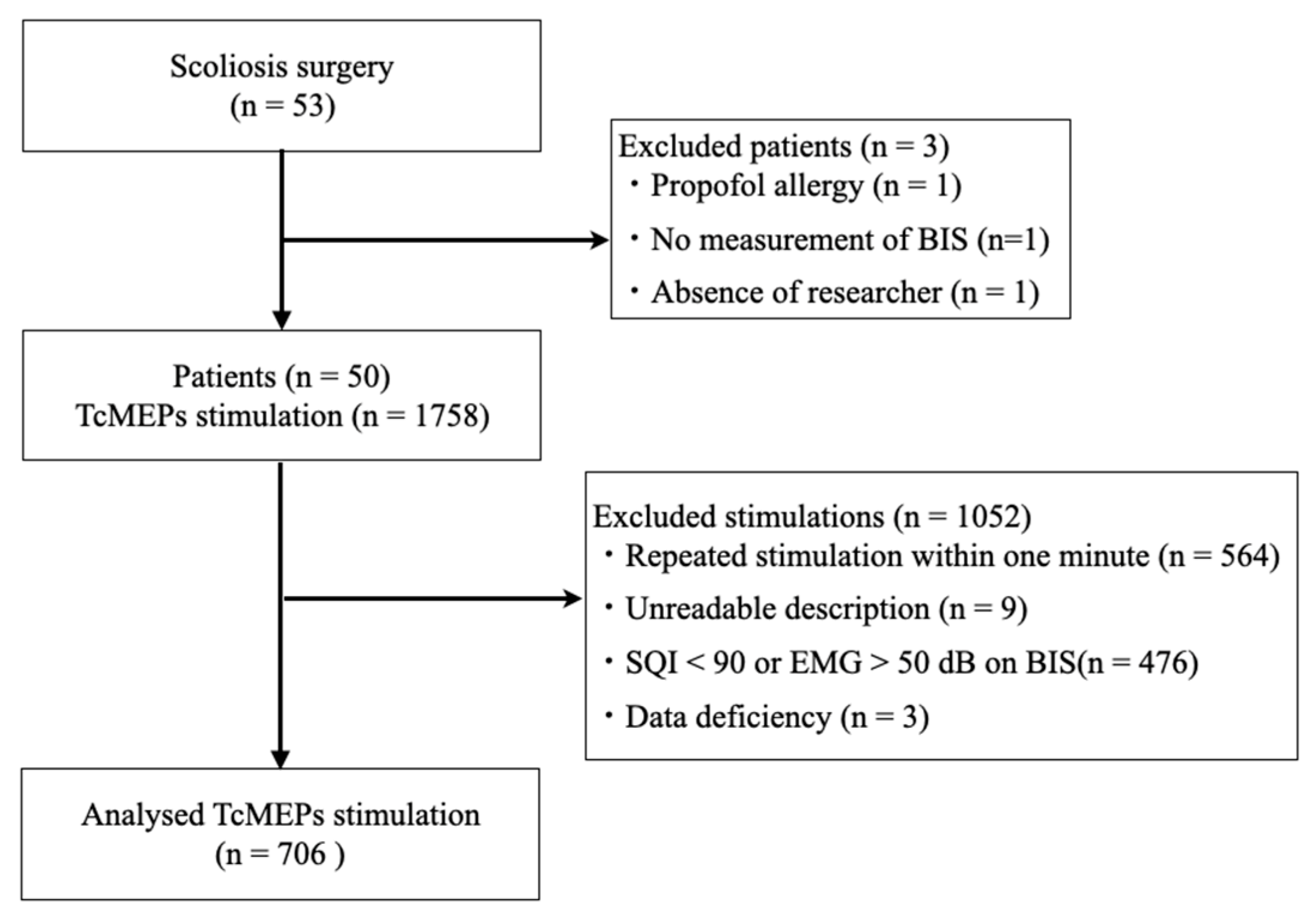
2.4. Rationale for the Number of Cases
2.5. Statistical Analysis
3. Results
3.1. Patient Demographic, Perioperative, and TcMEP Measurement Data
3.2. TcMEP Parameters
3.3. Influence of Physiological, Pharmacological, and Time-Related Factors as Well as Stimulation Conditions on TcMEP Amplitude
3.4. NND and Complications of STS-INP
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koumbourlis, A.C. Scoliosis and the respiratory system. Paediatr. Respir. Rev. 2006, 7, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Weiss, H.R.; Goodall, D. Rate of complications in scoliosis surgery—A systematic review of the Pub Med literature. Scoliosis 2008, 3, 9. [Google Scholar] [CrossRef] [Green Version]
- Reames, D.L.; Smith, J.S.; Fu, K.M.; Polly, D.W., Jr.; Ames, C.P.; Berven, S.H.; Perra, J.H.; Glassman, S.D.; McCarthy, R.E.; Knapp, R.D., Jr.; et al. Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: A review of the Scoliosis Research Society Morbidity and Mortality database. Spine 2011, 36, 1484–1491. [Google Scholar] [CrossRef]
- Divecha, H.M.; Siddique, I.; Breakwell, L.M.; Millner, P.A.; British Scoliosis Society, M. Complications in spinal deformity surgery in the United Kingdom: 5-year results of the annual British Scoliosis Society National Audit of Morbidity and Mortality. Eur. Spine J. 2014, 23 (Suppl. 1), S55–S60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thirumala, P.D.; Crammond, D.J.; Loke, Y.K.; Cheng, H.L.; Huang, J.; Balzer, J.R. Diagnostic accuracy of motor evoked potentials to detect neurological deficit during idiopathic scoliosis correction: A systematic review. J. Neurosurg. Spine 2017, 26, 374–383. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nassef, M.; Splinter, W.; Lidster, N.; Al-Kalbani, A.; Nashed, A.; Ilton, S.; Vanniyasingam, T.; Paul, J. Intraoperative neurophysiologic monitoring in idiopathic scoliosis surgery: A retrospective observational study of new neurologic deficits. Can. J. Anesth. 2021, 68, 477–484. [Google Scholar] [CrossRef]
- Lieberman, J.A.; Lyon, R.; Feiner, J.; Diab, M.; Gregory, G.A. The effect of age on motor evoked potentials in children under propofol/isoflurane anesthesia. Anesth. Analg. 2006, 103, 316–321. [Google Scholar] [CrossRef]
- Kawaguchi, M.; Iida, H.; Tanaka, S.; Fukuoka, N.; Hayashi, H.; Izumi, S.; Yoshitani, K.; Kakinohana, M. A practical guide for anesthetic management during intraoperative motor evoked potential monitoring. J. Anesth. 2020, 34, 5–28. [Google Scholar] [CrossRef]
- Macdonald, D.B.; Skinner, S.; Shils, J.; Yingling, C.; American Society of Neurophysiological Monitoring. Intraoperative motor evoked potential monitoring—A position statement by the American Society of Neurophysiological Monitoring. Clin. Neurophysiol. 2013, 124, 2291–2316. [Google Scholar] [CrossRef]
- Schwartz, D.M.; Sestokas, A.K.; Dormans, J.P.; Vaccaro, A.R.; Hilibrand, A.S.; Flynn, J.M.; Li, P.M.; Shah, S.A.; Welch, W.; Drummond, D.S.; et al. Transcranial electric motor evoked potential monitoring during spine surgery: Is it safe? Spine 2011, 36, 1046–1049. [Google Scholar] [CrossRef]
- Ulkatan, S.; Jaramillo, A.M.; Tellez, M.J.; Kim, J.; Deletis, V.; Seidel, K. Incidence of intraoperative seizures during motor evoked potential monitoring in a large cohort of patients undergoing different surgical procedures. J. Neurosurg. 2017, 126, 1296–1302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yata, S.; Ida, M.; Shimotsuji, H.; Nakagawa, Y.; Ueda, N.; Takatani, T.; Shigematsu, H.; Motoyama, Y.; Nakase, H.; Kirita, T.; et al. Bite injuries caused by transcranial electrical stimulation motor-evoked potentials’ monitoring: Incidence, associated factors, and clinical course. J. Anesth. 2018, 32, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Rice, D.; Barone, S., Jr. Critical periods of vulnerability for the developing nervous system: Evidence from humans and animal models. Environ. Health Perspect. 2000, 108, 511–533. [Google Scholar] [CrossRef] [PubMed]
- Ohtaki, S.; Akiyama, Y.; Kanno, A.; Noshiro, S.; Hayase, T.; Yamakage, M.; Mikuni, N. The influence of depth of anesthesia on motor evoked potential response during awake craniotomy. J. Neurosurg. 2017, 126, 260–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fehlings, M.G.; Tator, C.H.; Linden, R.D. The relationships among the severity of spinal cord injury, motor and somatosensory evoked potentials and spinal cord blood flow. Electroencephalogr. Clin. Neurophysiol. 1989, 74, 241–259. [Google Scholar] [CrossRef]
- Sahinovic, M.M.; Gadella, M.C.; Shils, J.; Dulfer, S.E.; Drost, G. Anesthesia and intraoperative neurophysiological spinal cord monitoring. Curr. Opin. Anaesthesiol. 2021, 34, 590–596. [Google Scholar] [CrossRef]
- Haghighi, S.S.; Keller, B.P.; Oro, J.J.; Gibbs, S.R. Motor-evoked potential changes during hypoxic hypoxia. Surg. Neurol. 1993, 39, 399–402. [Google Scholar] [CrossRef]
- Shinzawa, M.; Yoshitani, K.; Minatoya, K.; Irie, T.; Ogino, H.; Ohnishi, Y. Changes of motor evoked potentials during descending thoracic and thoracoabdominal aortic surgery with deep hypothermic circulatory arrest. J. Anesth. 2012, 26, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Kanemaru, E.; Yoshitani, K.; Kato, S.; Tanaka, Y.; Ohnishi, Y. Reappearance of Motor-Evoked Potentials During the Rewarming Phase After Deep Hypothermic Circulatory Arrest. J. Cardiothorac. Vasc. Anesth. 2018, 32, 709–714. [Google Scholar] [CrossRef] [Green Version]
- Kalkman, C.J.; Drummond, J.C.; Ribberink, A.A.; Patel, P.M.; Sano, T.; Bickford, R.G. Effects of propofol, etomidate, midazolam, and fentanyl on motor evoked responses to transcranial electrical or magnetic stimulation in humans. Anesthesiology 1992, 76, 502–509. [Google Scholar] [CrossRef]
- Scheufler, K.M.; Zentner, J. Total intravenous anesthesia for intraoperative monitoring of the motor pathways: An integral view combining clinical and experimental data. J. Neurosurg. 2002, 96, 571–579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nathan, N.; Tabaraud, F.; Lacroix, F.; Moulies, D.; Viviand, X.; Lansade, A.; Terrier, G.; Feiss, P. Influence of propofol concentrations on multipulse transcranial motor evoked potentials. Br. J. Anaesth. 2003, 91, 493–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ushirozako, H.; Yoshida, G.; Hasegawa, T.; Yamato, Y.; Yasuda, T.; Banno, T.; Arima, H.; Oe, S.; Yamada, T.; Ide, K.; et al. Characteristics of false-positive alerts on transcranial motor evoked potential monitoring during pediatric scoliosis and adult spinal deformity surgery: An “anesthetic fade” phenomenon. J. Neurosurg. Spine 2019, 32, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Ando, K.; Kobayashi, K.; Ito, K.; Tsushima, M.; Morozumi, M.; Tanaka, S.; Machino, M.; Ota, K.; Nishida, Y.; Ishiguro, N.; et al. Wave change of intraoperative transcranial motor-evoked potentials during corrective fusion for syndromic and neuromuscular scoliosis. Oper. Neurosurg. 2019, 16, 53–58. [Google Scholar] [CrossRef]
- Neira, V.M.; Ghaffari, K.; Bulusu, S.; Moroz, P.J.; Jarvis, J.G.; Barrowman, N.; Splinter, W. Diagnostic accuracy of neuromonitoring for identification of new neurologic deficits in pediatric spinal fusion surgery. Anesth. Analg. 2016, 123, 1556–1566. [Google Scholar] [CrossRef] [PubMed]
- Pastorelli, F.; Di Silvestre, M.; Plasmati, R.; Michelucci, R.; Greggi, T.; Morigi, A.; Bacchin, M.R.; Bonarelli, S.; Cioni, A.; Vommaro, F.; et al. The prevention of neural complications in the surgical treatment of scoliosis: The role of the neurophysiological intraoperative monitoring. Eur. Spine J. 2011, 20, S105–S114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kundnani, V.K.; Zhu, L.; Tak, H.; Wong, H. Multimodal intraoperative neuromonitoring in corrective surgery for adolescent idiopathic scoliosis: Evaluation of 354 consecutive cases. Indian J. Orthop. 2010, 44, 64–72. [Google Scholar] [CrossRef]
- Schwartz, D.M.; Auerbach, J.D.; Dormans, J.P.; Flynn, J.; Drummond, D.S.; Bowe, J.A.; Laufer, S.; Shah, S.A.; Bowen, J.R.; Pizzutillo, P.D.; et al. Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J. Bone Joint Surg. Am. 2007, 89, 2440–2449. [Google Scholar] [CrossRef]
- Liu, Q.; Wang, Q.; Liu, H.; Wu, W.K.K.; Chan, M.T.V. Warning criteria for intraoperative neurophysiologic monitoring. Curr. Opin. Anaesthesiol. 2017, 30, 557–562. [Google Scholar] [CrossRef]
- Yang, J.; Skaggs, D.L.; Chan, P.; Shah, S.A.; Vitale, M.G.; Neiss, G.; Feinberg, N.; Andras, L.M. Raising mean arterial pressure alone restores 20% of intraoperative neuromonitoring losses. Spine 2018, 43, 890–894. [Google Scholar] [CrossRef]
- Acharya, S.; Palukuri, N.; Gupta, P.; Kohli, M. Transcranial motor evoked potentials during spinal deformity corrections-safety, efficacy, limitations, and the role of a checklist. Front. Surg. 2017, 4, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sakamoto, T.; Kawaguchi, M.; Kakimoto, M.; Inoue, S.; Takahashi, M.; Furuya, H. The effect of hypothermia on myogenic motor-evoked potentials to electrical stimulation with a single pulse and a train of pulses under propofol/ketamine/fentanyl anesthesia in rabbits. Anesth. Analg. 2003, 96, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, D.B. Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J. Clin. Neurophysiol. 2002, 19, 416–429. [Google Scholar] [CrossRef] [PubMed]
- Tamkus, A.; Rice, K. The incidence of bite injuries associated with transcranial motor-evoked potential monitoring. Anesth. Analg. 2012, 115, 663–667. [Google Scholar] [CrossRef] [PubMed]

| Demographic Data | Radiographic and Laboratory Data | ||
|---|---|---|---|
| Age (years) | 14 [13, 17] | Diagnosis | |
| Sex | Idiopathic scoliosis | 41 (82%) | |
| Female/Male | 41 (82%)/9 (18%) | Symptomatic scoliosis | 7 (14%) |
| Height (m) | 1.59 [1.55, 1.63] | Congenital scoliosis | 2 (4%) |
| Weight (kg) | 48 [44, 54] | Cobb angle | |
| Body mass index (kg/m2) | 18.92 [17.37, 21.30] | Main curve (°) | 54 [50, 62] |
| Body surface area (m2) | 1.44 [1.36, 1.52] | Bending main curve (°) | 16 [11, 26] |
| ASA-PS class | Flexibility of main curve (%) | 70 [56, 80] | |
| 1/2 | 39 (78%)/11 (22%) | Kyphosis (°) | 14 [9, 23] |
| Complication | Hemoglobin (mg/dL) | 12.20 [11.62, 13.10] | |
| None | 35 (70%) | Hematocrit (%) | 37.00 [35.82, 39.77] |
| Chiari malformation | 3 (20%) | ||
| Marfan syndrome | 3 (20%) | Intraoperative data | |
| ADHD | 1 (6.7%) | Operation time (min) | 252 [212, 283] |
| Autism | 1 (6.7%) | Anesthesia time (min) | 358 [305, 400] |
| Asthma | 1 (6.7%) | Number of fused levels | 10 [8, 11] |
| Depression | 1 (6.7%) | Number of facetectomies | 9 [7, 10] |
| Developmental disorder | 1 (6.7%) | Total fluid intake (mL) | 3000 [2278, 4068] |
| Kawasaki disease | 1 (6.7%) | Total transfusion (mL) | 295 [0, 648] |
| Migraine | 1 (6.7%) | Urine output (mL) | 532 [340, 1008] |
| Multiple osteochondroma | 1 (6.7%) | Water balance (mL) | 1765 [1178, 2304] |
| Renal dysfunction | 1 (6.7%) | ||
| Vital signs at admission | |||
| Pulse rate (waves/min) | 84 [74, 93] | ||
| Mean NIBP (mmHg) | 107 [99, 113] | ||
| All (n = 1412) | Age 10–14 Years (n = 760) | Age 15–19 Years (n = 652) | |
|---|---|---|---|
| TcMEP stimulation settings | |||
| Number of pulses | 13 [11, 14] | 13 [12, 15] | 12 [11, 13] |
| Stimulation intensity (mA) | 150 [140, 160] | 150 [140, 170] | 140 [130, 150] |
| TcMEP amplitude (mV) | |||
| Abductor pollicis brevis muscle | 3.25 [2.50, 4.18] | 3,20 [2.44, 4.10] | 3.30 [2.55, 4.30] |
| Tibialis anterior muscle | 1.36 [0.89, 1.91] | 1.16 [0.72, 1.59] | 1.59 [1.12, 2.40] |
| Abductor hallucis muscle | 1.96 [1.39, 2.70] | 1.78 [1.18, 2.53] | 2.15 [1.61, 2.80] |
| Author | Patients | Number of Pulses | Stimulus Intensity |
|---|---|---|---|
| Ushirozako et al. [23] | Adult spinal deformity: 282 | 5 | 200 mA |
| Adolescent idiopathic scoliosis: 100 | |||
| Other types of scoliosis: 11 | |||
| Ando et al. [24] | Syndromic and neuromuscular scoliosis: 23 | 4 to 5 | 300 to 600 V |
| Neira et al. [25] | Pediatric scoliosis: 296 | 5 | Not mentioned |
| Pastorelli et al. [26] | Congenital scoliosis/kyphoscoliosis: 15 | 5 to 7 | up to 200 mA |
| Adolescent idiopathic scoliosis/kyphoscoliosis: 76 | |||
| Adult idiopathic scoliosis/kyphoscoliosis: 52 | |||
| Other spine deformities: 29 | |||
| Kundnani et al. [27] | Adolescent idiopathic scoliosis (aged 8 to 18 years): 354 | 2 to 7 | 250 to 500 V |
| Physiological factors | |
| Mean arterial blood pressure (mmHg) | 55 [51, 61] |
| Percutaneous oxygen saturation (%) | 100 [100, 100] |
| Core temperature (°C) | 36.70 [36.40, 37.00] |
| Pulse rate (waves/min) | 78 [69, 85] |
| Factors related to the depth of anesthesia | |
| Bispectral index | 44 [39, 49] |
| Signal quality index | 95.5 [94.2, 98.7] |
| Electromyogram activity (dB) | 28.3 [27.5, 29.4] |
| Suppression ratio (%) | 0 [0, 0] |
| Pharmacological factors | |
| Estimated blood concentration of propofol (µg/mL) | 3.40 [3.00, 3.91] |
| Surgical factors | |
| Surgical elapsed time at TcMEP stimulation (min) | 144 [98, 199] |
| Abductor Pollicis Brevis Muscle Amplitude (n = 1412) | ||
|---|---|---|
| Regression Coefficient [95% CI] | Predicted Mean Difference [95% CI *] | |
| Mean arterial blood pressure (mmHg) | 0.004 [−0.005, 0.012] | 0.036 [−0.049, 0.121] |
| Bispectral index | 0.003 [−0.007, 0.014] | 0.033 [−0.070, 0.136] |
| Estimated blood concentration of propofol (µg/mL) | −0.217 [−0.501, 0.068] | −0.198 [−0.456, 0.062] |
| Core temperature (°C) | −0.140 [−0.432, 0.150] | −0.084 [−0.259, 0.090] |
| Oxygen saturation (%) | 0.122 [−0.027, 0.269] | ** |
| Number of pulses (times) | 0.035 [−0.039, 0.108] | 0.105 [−0.117, 0.325] |
| Stimulus intensity (×10 mA) | −0.076 [−0.171, 0.019] | −0.153 [−0.343, 0.039] |
| Surgical elapsed time at TcMEP stimulation (min) | 0.000 [−0.001, 0.002] | 0.050 [−0.095, 0.197] |
| Tibialis Anterior Muscle Amplitude (n = 1412) | ||
| Regression Coefficient [95% CI] | Predicted Mean Difference [95% CI *] | |
| Mean arterial blood pressure (mmHg) | −0.005 [−0.012, 0.002] | −0.054 [−0.124, 0.016] |
| Bispectral index | 0.003 [−0.006, 0.012] | 0.030 [−0.055, 0.115] |
| Estimated blood concentration of propofol (µg/mL) | −0.031 [−0.285, 0.217] | −0.028 [−0.259, 0.198] |
| Core temperature (°C) | 0.185 [−0.057, 0.431] | 0.111 [−0.034, 0.258] |
| Oxygen saturation (%) | 0.080 [−0.042, 0.204] | ** |
| Number of pulses (times) | −0.074 [−0.138, −0.012] | −0.223 [−0.413, −0.036] |
| Stimulus intensity (×10 mA) | −0.044 [−0.128, 0.038] | −0.088 [−0.256, 0.077] |
| Surgical elapsed time at TcMEP stimulation (min) | −0.001 [−0.002, 0.001] | −0.055 [−0.176, 0.066] |
| Abductor Hallucis Muscle Amplitude (n = 1412) | ||
| Regression Coefficient [95% CI] | Predicted Mean Difference [95% CI *] | |
| Mean arterial blood pressure (mmHg) | −0.003 [−0.011, 0.004] | −0.035 [−0.107, 0.037] |
| Bispectral index | 0.005 [−0.004, 0.013] | 0.045 [−0.043, 0.133] |
| Estimated blood concentration of propofol (µg/mL) | −0.036 [−0.289, 0.216] | −0.033 [−0.263, 0.196] |
| Core temperature (°C) | 0.118 [−0.132, 0.370] | 0.071 [−0.079, 0.222] |
| Oxygen saturation (%) | −0.082 [−0.208, 0.044] | ** |
| Number of pulses (times) | −0.034 [−0.099, 0.031] | −0.103 [−0.297, 0.092] |
| Stimulus intensity (×10 mA) | 0.126 [0.040, 0.210] | 0.251 [0.080, 0.420] |
| Surgical elapsed time at TcMEP stimulation (min) | −0.001 [−0.003, −0.000] | −0.137 [−0.262, −0.013] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toki, T.; Fujita, N.; Ichikawa, T.; Ochi, N.; Yokota, I.; Sudo, H.; Morimoto, Y. Factors Affecting Transcranial Motor-Evoked Potential Measurements Using Single-Train Stimulation with an Increased Number of Pulses during Adolescent Scoliosis Surgery: A Prospective Observational Study. J. Clin. Med. 2023, 12, 4433. https://doi.org/10.3390/jcm12134433
Toki T, Fujita N, Ichikawa T, Ochi N, Yokota I, Sudo H, Morimoto Y. Factors Affecting Transcranial Motor-Evoked Potential Measurements Using Single-Train Stimulation with an Increased Number of Pulses during Adolescent Scoliosis Surgery: A Prospective Observational Study. Journal of Clinical Medicine. 2023; 12(13):4433. https://doi.org/10.3390/jcm12134433
Chicago/Turabian StyleToki, Takayuki, Noriaki Fujita, Tomohiro Ichikawa, Noriki Ochi, Isao Yokota, Hideki Sudo, and Yuji Morimoto. 2023. "Factors Affecting Transcranial Motor-Evoked Potential Measurements Using Single-Train Stimulation with an Increased Number of Pulses during Adolescent Scoliosis Surgery: A Prospective Observational Study" Journal of Clinical Medicine 12, no. 13: 4433. https://doi.org/10.3390/jcm12134433
APA StyleToki, T., Fujita, N., Ichikawa, T., Ochi, N., Yokota, I., Sudo, H., & Morimoto, Y. (2023). Factors Affecting Transcranial Motor-Evoked Potential Measurements Using Single-Train Stimulation with an Increased Number of Pulses during Adolescent Scoliosis Surgery: A Prospective Observational Study. Journal of Clinical Medicine, 12(13), 4433. https://doi.org/10.3390/jcm12134433






