Meckel’s Diverticulum as a Cause of Small Bowel Obstruction Complicated with Gangrene in the Third Trimester of Pregnancy: A Case Report
Abstract
1. Introduction
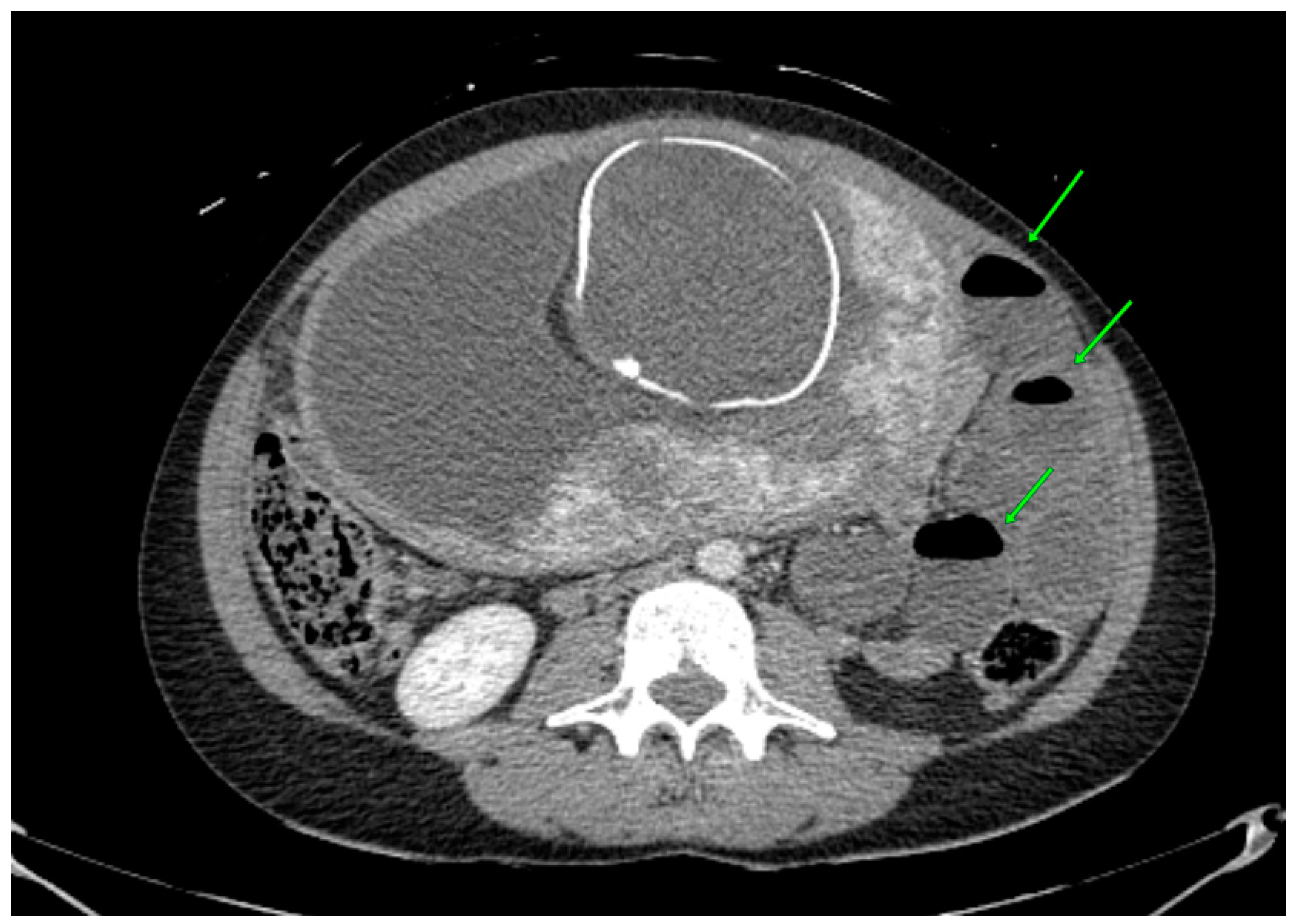
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bouyou, J.; Gaujoux, S.; Marcellin, L.; Leconte, M.; Goffinet, F.; Chapron, C.; Dousset, B. Abdominal emergencies during pregnancy. J. Visc. Surg. 2015, 152 (Suppl. S6), S105–S115. [Google Scholar] [CrossRef] [PubMed]
- Angelini, D.J. Obstetric triage revisited: Update on non-obstetric surgical conditions in pregnancy. J. Midwifery Women’s Health 2003, 48, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Sagar, J.; Kumar, V.; Shah, D.K. Meckel’s diverticulum: A systematic review. J. R. Soc. Med. 2006, 99, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.J.; Conroy, M.; Farkas, N. Systematic review of Meckel’s diverticulum in pregnancy. ANZ J. Surg. 2021, 91, E561–E569. [Google Scholar] [CrossRef] [PubMed]
- Pandeva, I.; Kumar, S.; Alvi, A.; Nosib, H. Meckel’s Diverticulitis as a Cause of an Acute Abdomen in the Second Trimester of Pregnancy: Laparoscopic Management. Case Rep. Obstet. Gynecol. 2015, 2015, 835609. [Google Scholar] [CrossRef]
- Augustin, G.; Majerovic, M. Non-obstetrical acute abdomen during pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2007, 131, 4–12. [Google Scholar] [CrossRef]
- Khan, N.A.; Chandramohan, M.; McDonald, S. Meckel divertculum. Radiol. Pediatr. 2008, 110, 213–217. [Google Scholar]
- Botezatu, R.; Marian, R.; Gica, N.; Iancu, G.; Peltecu, G.; Panaitescu, A.M. Axial Torsion and Infarction of Meckel’s Diverticulum in the 3rd Trimester of Pregnancy. Chirurgia 2018, 113, 266–269. [Google Scholar] [CrossRef]
- Limas, C.; Seretis, K.; Soultanidis, C.; Anagnostoulis, S. Axial Torsion and Gangrene of a Giant Meckel’s Diverticulum. J. Gastrointestin Liver Dis. 2006, 15, 67–68. [Google Scholar]
- Dumper, J.; Mackenzie, S.; Mitchell, P.; Sutherland, F.; Quan, M.L.; Mew, D. Complications of Meckel’s diverticula in adults. Can. J. Surg. J. Can. Chir. 2006, 49, 353–357. [Google Scholar]
- Zachariah, S.K.; Fenn, M.; Jacob, K.; Arthungal, S.A.; Zachariah, S.A. Management of acute abdomen in pregnancy: Current perspectives. Int. J. Womens Health 2019, 11, 119–134. [Google Scholar] [CrossRef]
- Tan, E.K.; Tan, E.L. Alterations in physiology and anatomy during pregnancy. Crit. Illn. Obstet. 2013, 27, 791–802. [Google Scholar] [CrossRef] [PubMed]
- Stefanopol, I.A.; Miulescu, M.; Baroiu, L.; Anghele, A.D.; Danila, D.M.; Tiron, Z. An Unusual Case of Meckel Diverticulitis Misdiagnosed as an Infected Urachal Cyst. Medicina 2021, 57, 495. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, M.; Salman, B.; Yilmaz, T.U.; Oguz, M. A quality of life comparison of laparoscopic and open approaches in acute appendicitis: A randomised prospective study. Acta Chir. Belg. 2009, 109, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Fatum, M.; Rojansky, N. Laparoscopic Surgery During Pregnancy. Obstet. Gynecol. Surv. 2001, 56, 50–59. [Google Scholar] [CrossRef]
- Acute Abdomen and Pregnancy. Obstetric Concerns. Available online: https://emedicine.medscape.com/article/195976-overview#a11 (accessed on 4 April 2023).
- Mazzocco, M.I.; Donati, S.; Maraschini, A.; Corsi, E.; Colciago, E.; Guelfi, F.; Cetin, I. Spontaneous hemoperitoneum in pregnancy: Italian prospective population-based cohort study. Acta Obstet. Gynecol. Scand. 2022, 101, 1220–1226. [Google Scholar] [CrossRef]
- Ahmed, Z.; Chhabra, S.; Kankaria, J.; Jenaw, R.K. Meckel’s diverticular perforation presenting as acute abdomen in the second trimester of pregnancy. BMJ Case Rep. 2016, 2016, bcr2016216643. [Google Scholar] [CrossRef] [PubMed]
- Orlandini, C.; Conti, N.; Pizzo, A.; Guerrini, E.; Verre, L. A Rare Case of Mekel’s Diverticulum Perforation by the Gangrenous Appendicitis during Pregnancy. Obstet. Gynecol. Cases Rev. 2016, 3, 074. [Google Scholar] [CrossRef]
- Li, Y.; Wu, S. Rare Cases of Two Types of Meckel’s Diverticulum. CRSLS 2018, e2017.00082. Available online: http://crsls.sls.org/2017-00082/ (accessed on 4 April 2023).
- Eisdorfer, J.; Zinkin, N.T.; Rivadeneira, D.E. Meckel’s diverticulitis: A rare cause of abdominal pain during pregnancy. ANZ J. Surg. 2018, 88, 800–802. [Google Scholar] [CrossRef]
- Hu, W.T.; Zhang, Q.Y.; Cheng, H.D. Perforated Meckel’s Diverticulitis Complicating Pregnancy at 28 Weeks’ Gestation Misdiagnosed as Appendicitis. Reprod. Dev. Med. 2018, 2, 187–189. [Google Scholar] [CrossRef]
- Nagata, H.; Nishizawa, H.; Mashima, S.; Shimahara, Y. Axial torsion of Meckel’s diverticulum causing acute peritonitis in the first trimester of pregnancy: A case report. Surg. Case Rep. 2019, 5, 190. [Google Scholar] [CrossRef] [PubMed]
- Combes, A.D.; Limmer, A.M.; Verschuer, K. Small bowel intussusception secondary to Meckel’s diverticulum containing polypoid lesion in pregnancy. ANZ J. Surg. 2020, 90, 1774–1776. [Google Scholar] [CrossRef] [PubMed]
- Féria, B.; Trindade, M.; Palma, M.J.; Figueiredo, J.; Passos, F. Meckel’s Diverticulum: The “Great Mimic” but Often a Forgotten Cause of Acute Abdomen during Pregnancy. Case Rep. Obstet. Gynecol. 2022, 2022, 2383075. [Google Scholar] [CrossRef]
- He, Y.; Wang, L.; Cao, W. Case report: Emergency presentation of Meckel’s diverticulum in the 3rd trimester of pregnancy. Front. Surg. 2023, 10, 1051158. [Google Scholar] [CrossRef]
- Fu, P.-H.; Yu, C.-H.; Chen, Y.-C.; Chu, C.-C.; Chen, J.-Y.; Liang, F.-W. Risk of adverse fetal outcomes following nonobstetric surgery during gestation: A nationwide population-based analysis. BMC Pregnancy Childbirth 2022, 22, 406. [Google Scholar] [CrossRef] [PubMed]


| Author | Year | Patient’s Age | Gestational Age during Diagnosis | Imaging | Management | Preoperative Diagnosis | Postoperative Diagnosis |
|---|---|---|---|---|---|---|---|
| Ahmed et al. [18] | 2016 | 24 | 24 | US 1 (free fluid in the abdomen with multiple septa) | Exploratory laparotomy | Appendicular perforation peritonitis | Perforated Meckel’s diverticulum |
| Orlandini et al. [19] | 2016 | 24 | 30 | US (monolateral hydronephrosis) | Exploratory laparotomy and Cesarean section | Not reported | Perforated Meckel’s diverticulum |
| Li et al. [20] | 2017 | 28 | 30 | US (signs of general small-bowel expansion and ascites). MRI scan (intraperitoneal bowel expansion with effusion) | Exploratory laparoscopy | Gastroenteritis | Small bowel obstruction |
| Botezatu et al. [8] | 2018 | 30 | 34 | US (no findings) | Clinical observation and symptomatic medication | Bowel obstruction and/or perforation | Perforated Meckel’s diverticulum |
| Eisdorfer et al. [21] | 2018 | 30 | 22 | MRI 2 scan | Conservative treatment | Meckel’s diverticulitis | Not reported |
| Hu et al. [22] | 2018 | 28 | 28 | US | Conservative treatment | Appendicitis | Perforated Meckel’s diverticulum |
| Nagata et al. [23] | 2019 | 31 | 15 | CT 3 scan (dilated small bowel loops with multiple air–fluid levels) | Emergency laparotomy | Gastroenteritis | Gangrenous Meckel’s diverticulum |
| Combes et al. [24] | 2020 | 27 | 21 | US (target sign consistent with intussusception) | Emergency laparoscopy | Intussusception | Intussusception |
| Beatriz Féria et al. [25] | 2022 | 40 | 33 | US (not informative), CT scan (showed densification of pericolic fat tissue) | Urgent Cesarean section followed by a laparotomy | Appendicitis, bowel obstruction, perforated ulcer, inflammatory bowel disease, and diverticulitis | Perforated necrotic Meckel’s diverticulum |
| Yantao He et al. [26] | 2023 | 23 | 22 | US (not informative), CT scan (left lower abdominal part of the small intestine in a vortex shape, local intestinal lumen dilated) | Exploratory laparotomy and small-bowel resection | Acute gastroenteritis and preterm labor | Meckel’s diverticulum, with a 360° twist and local necrosis without perforation |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Šiaudinytė, M.; Vankevičienė, K.; Povilaitienė, R.; Domža, G.; Paliulytė, V.; Ramašauskaitė, D. Meckel’s Diverticulum as a Cause of Small Bowel Obstruction Complicated with Gangrene in the Third Trimester of Pregnancy: A Case Report. J. Clin. Med. 2023, 12, 4569. https://doi.org/10.3390/jcm12144569
Šiaudinytė M, Vankevičienė K, Povilaitienė R, Domža G, Paliulytė V, Ramašauskaitė D. Meckel’s Diverticulum as a Cause of Small Bowel Obstruction Complicated with Gangrene in the Third Trimester of Pregnancy: A Case Report. Journal of Clinical Medicine. 2023; 12(14):4569. https://doi.org/10.3390/jcm12144569
Chicago/Turabian StyleŠiaudinytė, Monika, Karolina Vankevičienė, Rasa Povilaitienė, Gintautas Domža, Virginija Paliulytė, and Diana Ramašauskaitė. 2023. "Meckel’s Diverticulum as a Cause of Small Bowel Obstruction Complicated with Gangrene in the Third Trimester of Pregnancy: A Case Report" Journal of Clinical Medicine 12, no. 14: 4569. https://doi.org/10.3390/jcm12144569
APA StyleŠiaudinytė, M., Vankevičienė, K., Povilaitienė, R., Domža, G., Paliulytė, V., & Ramašauskaitė, D. (2023). Meckel’s Diverticulum as a Cause of Small Bowel Obstruction Complicated with Gangrene in the Third Trimester of Pregnancy: A Case Report. Journal of Clinical Medicine, 12(14), 4569. https://doi.org/10.3390/jcm12144569







