Sleep Apnea Combined with Pulmonary Hypertension in a Veteran Patient Population
Abstract
1. Introduction
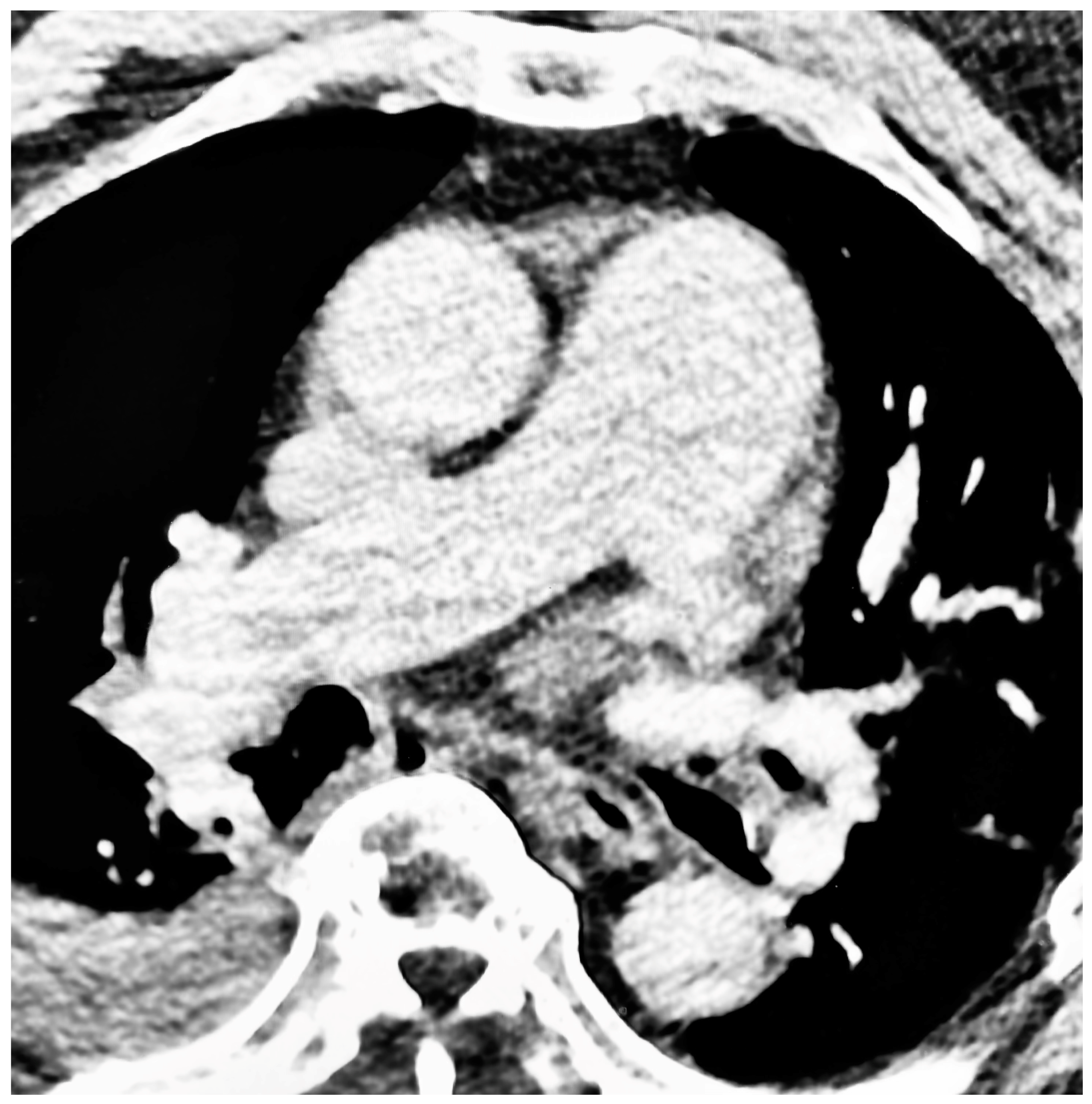
2. Materials and Methods
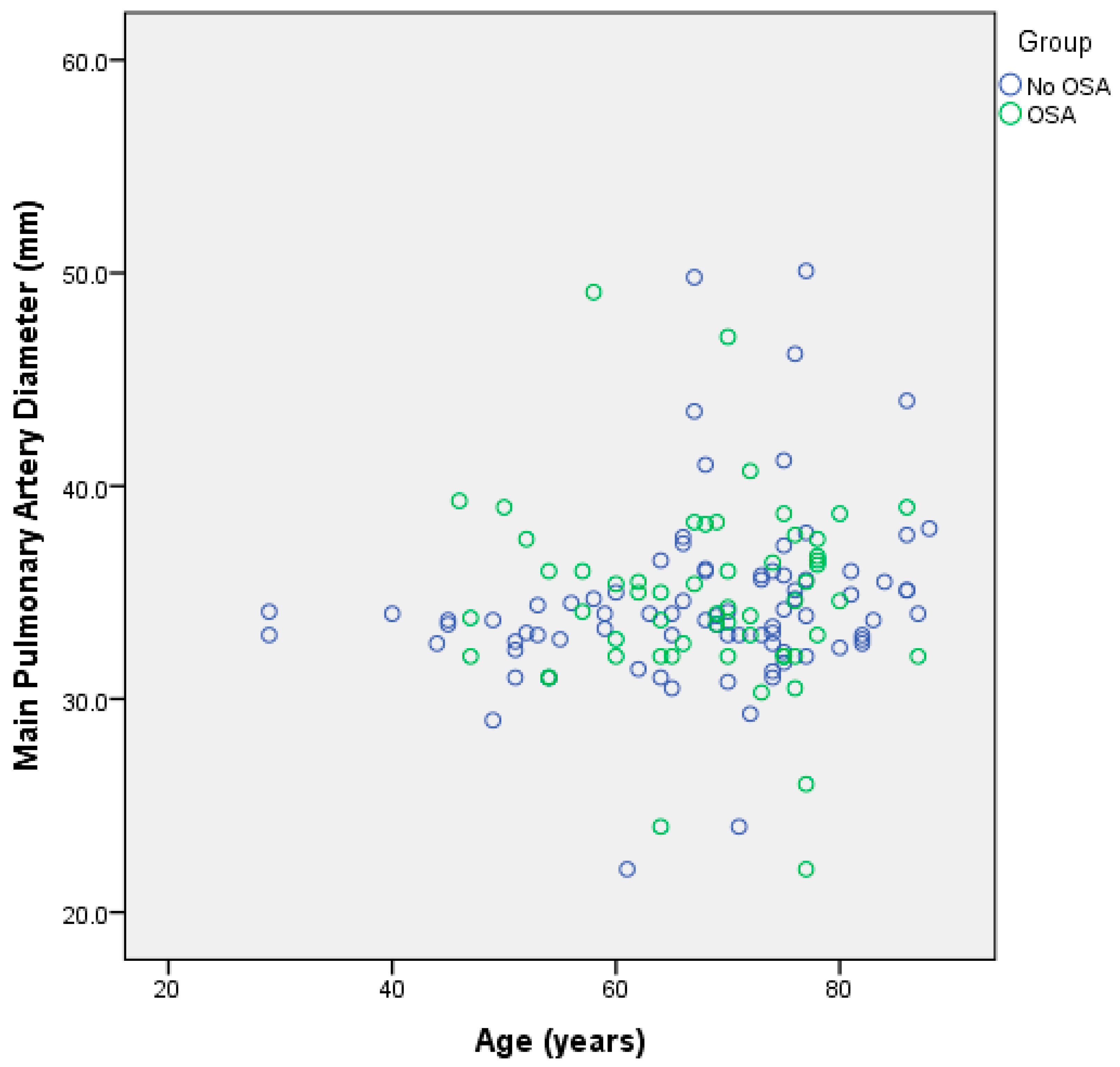
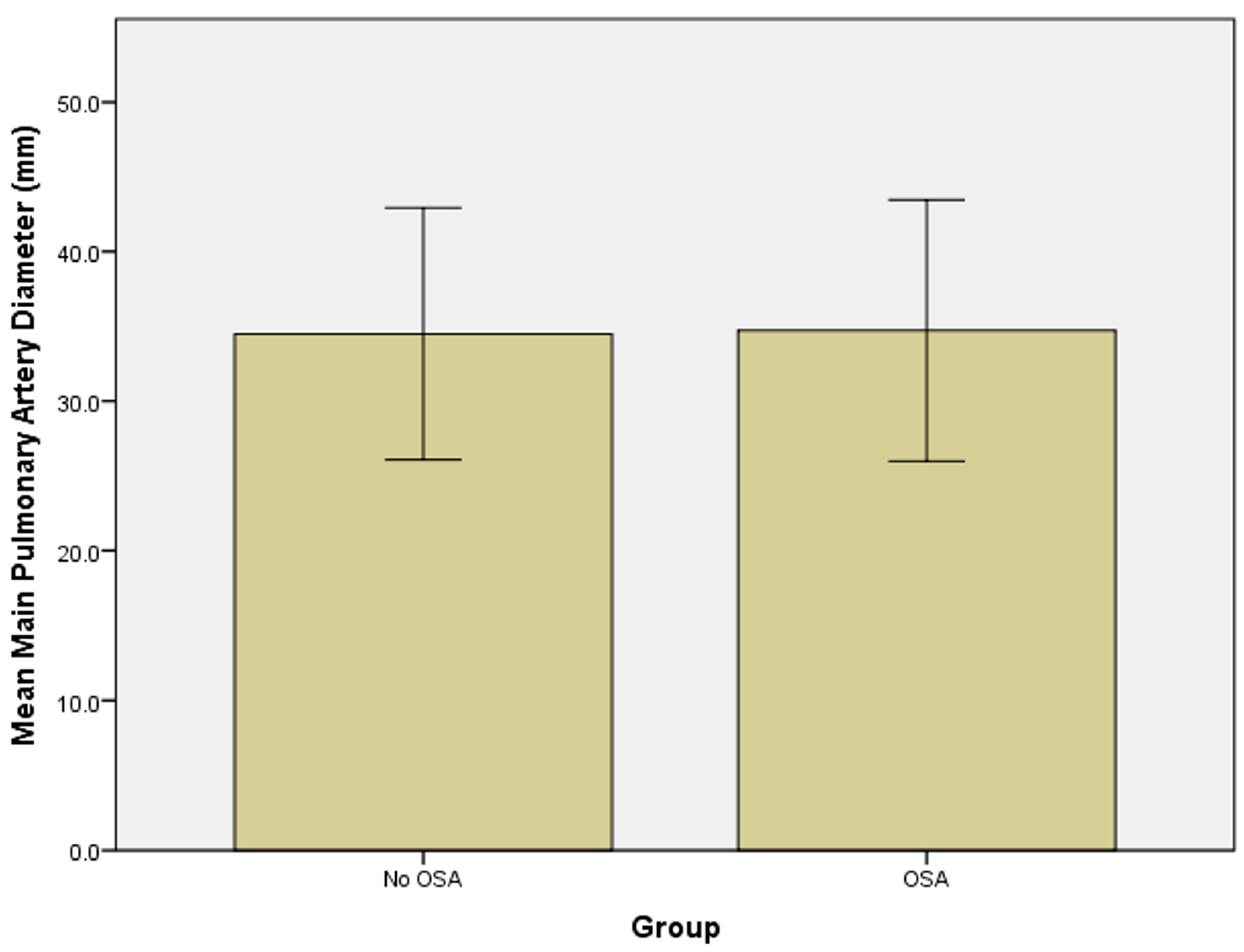
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eckert, D.J.; Malhotra, A. Pathophysiology of adult obstructive sleep apnea. Proc. Am. Thorac. Soc. 2008, 5, 144–153. [Google Scholar] [CrossRef] [PubMed]
- Sommer, N.; Dietrich, A.; Schermuly, R.T.; Ghofrani, H.A.; Gudermann, T.; Schulz, R.; Seeger, W.; Grimminger, F.; Weissmann, N. Regulation of hypoxic pulmonary vasoconstriction: Basic mechanisms. Eur. Respir. J. 2008, 32, 1639–1651. [Google Scholar] [CrossRef] [PubMed]
- Kholdani, C.; Fares, W.H.; Mohsenin, V. Pulmonary hypertension in obstructive sleep apnea: Is it clinically significant? A critical analysis of the association and pathophysiology. Pulm. Circ. 2015, 5, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Hassoun, P.M. Pulmonary Arterial Hypertension. N. Engl. J. Med. 2021, 385, 2361–2376. [Google Scholar] [CrossRef] [PubMed]
- Truong, Q.A.; Bhatia, H.S.; Szymonifka, J.; Zhou, Q.; Lavender, Z.; Waxman, A.B.; Semigran, M.J.; Malhotra, R. A four-tier classification system of pulmonary artery metrics on computed tomography for the diagnosis and prognosis of pulmonary hypertension. J. Cardiovasc. Comput. Tomogr. 2018, 12, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Sirajuddin, A.; Mirmomen, S.M.; Henry, T.S.; Kandathil, A.; Kelly, A.M.; King, C.S.; Kuzniewski, C.T.; Lai, A.R.; Lee, E.; Expert Panel on Thoracic Imaging; et al. ACR Appropriateness Criteria(R) Suspected Pulmonary Hypertension: 2022 Update. J. Am. Coll. Radiol. 2022, 19, S502–S512. [Google Scholar] [CrossRef] [PubMed]
- Aluja Jaramillo, F.; Gutierrez, F.R.; Diaz Telli, F.G.; Yevenes Aravena, S.; Javidan-Nejad, C.; Bhalla, S. Approach to Pulmonary Hypertension: From CT to Clinical Diagnosis. Radiographics 2018, 38, 357–373. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, B.V.; Basner, R.C. Sleep Disorders In Goldman-Cecil Medicine, 26th ed.; Goldman, L., Schafer, A.I., Cecil, R.L., Eds.; Elsevier: Philadelphia, PA, USA, 2020; pp. 2376–2386.e2372. [Google Scholar]
- Lau, E.M.; Godinas, L.; Sitbon, O.; Montani, D.; Savale, L.; Jais, X.; Lador, F.; Gunther, S.; Celermajer, D.S.; Simonneau, G.; et al. Resting pulmonary artery pressure of 21-24 mmHg predicts abnormal exercise haemodynamics. Eur. Respir. J. 2016, 47, 1436–1444. [Google Scholar] [CrossRef]
- Gille, T.; Didier, M.; Boubaya, M.; Moya, L.; Sutton, A.; Carton, Z.; Baran-Marszak, F.; Sadoun-Danino, D.; Israel-Biet, D.; Cottin, V.; et al. Obstructive sleep apnoea and related comorbidities in incident idiopathic pulmonary fibrosis. Eur. Respir. J. 2017, 49, 1601934. [Google Scholar] [CrossRef] [PubMed]
- Carratu, P.; Ventura, V.A.; Maniscalco, M.; Dragonieri, S.; Berardi, S.; Ria, R.; Quaranta, V.N.; Vacca, A.; Devito, F.; Ciccone, M.M.; et al. Echocardiographic findings and plasma endothelin-1 levels in obese patients with and without obstructive sleep apnea. Sleep Breath. 2016, 20, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Zhao, Z.; Zhao, Q.; Jin, Q.; Zhang, Y.; Li, X.; Duan, A.; Luo, Q.; Liu, Z. The clinical characteristics of patients with pulmonary hypertension combined with obstructive sleep apnoea. BMC Pulm. Med. 2021, 21, 378. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.; Parthasarathy, S. Obesity Hypoventilation Syndrome. Curr. Pulmonol. Rep. 2015, 4, 42–55. [Google Scholar] [CrossRef] [PubMed]
- Sajkov, D.; McEvoy, R.D. Obstructive sleep apnea and pulmonary hypertension. Prog. Cardiovasc. Dis. 2009, 51, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Ulmer, C.S.; McCant, F.; Stechuchak, K.M.; Olsen, M.; Bosworth, H.B. Prevalence of insomnia disorder and sleep apnea in a sample of veterans at risk for cardiovascular disease. J. Clin. Sleep. Med. 2021, 17, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Carratu, P.; Di Ciaula, A.; Dragonieri, S.; Ranieri, T.; Matteo Ciccone, M.; Portincasa, P.; Resta, O. Relationships between Obstructive Sleep Apnea Syndrome and cardiovascular risk in a naive population of southern Italy. Int. J. Clin. Pract. 2021, 75, e14952. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stark, P.; Chang, E.Y. Sleep Apnea Combined with Pulmonary Hypertension in a Veteran Patient Population. J. Clin. Med. 2023, 12, 4634. https://doi.org/10.3390/jcm12144634
Stark P, Chang EY. Sleep Apnea Combined with Pulmonary Hypertension in a Veteran Patient Population. Journal of Clinical Medicine. 2023; 12(14):4634. https://doi.org/10.3390/jcm12144634
Chicago/Turabian StyleStark, Paul, and Eric Y. Chang. 2023. "Sleep Apnea Combined with Pulmonary Hypertension in a Veteran Patient Population" Journal of Clinical Medicine 12, no. 14: 4634. https://doi.org/10.3390/jcm12144634
APA StyleStark, P., & Chang, E. Y. (2023). Sleep Apnea Combined with Pulmonary Hypertension in a Veteran Patient Population. Journal of Clinical Medicine, 12(14), 4634. https://doi.org/10.3390/jcm12144634






