1. Introduction
Maxillofacial trauma is still the most common area treated within oral and maxillofacial surgery departments. In Poland, like in other European countries, most of the fractures affect males (from 3.6:1 to 9.4:1, in Poland 5.1:1) with a mean age of 33 years. Among the etiological factors of the injury, there are mainly assaults, traffic accidents, falls, accidents at work, and sports-related injuries. [
1]. In the presented study, the factors of greatest significance were falls, with a representation of 42%, then road traffic accidents (39%), and assaults (18%).
According to literature [
2], the most common fracture of the condylar process is a basal fracture (54% of condylar fractures), and the second most common fracture is mandibular head fracture (34% of condylar process fractures). Among all of the mandibular head fractures, there is 8% of type A fracture, 34% of type B, and 73% of type C.
The pathomechanism of the injury most often leads to the antero-medial displacement of the proximal fragment of mandibular head. It follows the contracting lateral pterygoid muscle, eventually reaching the infratemporal fossa. Currently, there are two main ways to reach the proximal fragment and its anatomical reduction [
3,
4,
5,
6,
7,
8]: preauricular access and retroauricular access. Both are percutaneous accesses and allow the direct visualization of the displaced fragment to the infratemporal region. Thus, it is possible to move the inner part of the mandibular head (the proximal fragment in diacapitular fracture) by supporting it from the front, i.e., in the pterygoid fovea. In this way, moving the mandibular head achieves its original anatomical position in glenoid fossa and contact with the distal fragment of mandible. It usually takes more than one manual attempt to accomplish a reduction, even though the muscle relaxant application and the caudal ramus of the mandible is pulled down. It appears that this may affect the postoperative appearance of the lateral pterygoid muscle. However, the extent to which its presentation changes is unknown, as the appearance of this muscle has not previously been studied after surgical treatment of mandibular head fracture. And there is an issue of importance, because it is the muscle that causes the mandibular contralaterotrusion, so it is largely responsible for the patient’s functional recovery [
9,
10].
The aim of this study was to evaluate the appearance of the pterygoid lateral muscle on computed tomography after surgical treatment of mandibular head fracture and its impact on muscle range of motion.
2. Materials and Methods
Sixty-six patients with unilateral mandibular head fractures were included in the study (classification according to Neff was applied [
11]—there were 5% of mandibular head fracture type A discovered, 21% of type B, and 74% of type C).
Most of the patients reported to the Emergency Department shortly after the injury and were included in the department’s operational schedule as a priority, as soon as possible. Due to their late reporting to the hospital, 8 patients were treated surgically more than 2 weeks after the injury.
The criterion for patient eligibility for this prospective study was the fact that the mandibular head on the opposite side was not injured, because the reference group consisted of the muscles of the healthy side.
Patients (
Table 1) were divided into two groups—51 of them were treated surgically with ORIF (open reduction and internal fixation) and 15 of them conservatively (i.e., closed treatment). Conservative treatment consisted of maxillomandibular ligation for a week, then elastic guide and mouth-opening exercises for another week, followed by 6 weeks of physiotherapy. Qualification for surgical or conservative treatment was not randomized, but dictated by clinical indications. Due to the medical staff special interest in mandibular condyle fractures, indications for surgical treatment were more restrictive than in other centers (shortening of the mandibular ramus of more than 2 mm and rotation of the proximal fragment of more than 30 degrees, versus shortening of the mandibular ramus of more than 5 mm and rotation of more than 50 degrees in other clinics).
The size of lateral pterygoid muscles was then evaluated in spiral computed tomography (CT). A standard protocol in Lodz’s department is to order a CT scan just after a surgery to assess the accuracy of bone fragment fixation, and 3, 6, 12, and 24 months later to assess the progress of a bone consolidation. All computed tomography images were assessed in RadiAnt DICOM viewer (Medixant, Poland, Poznań,
www.radiantviewer.com, accessed on 5 July 2023). The examinations were performed at the same window settings for each case: window height of 60 and width of 400 HU, which are the values that can be adopted for viewing soft tissues in CT images.
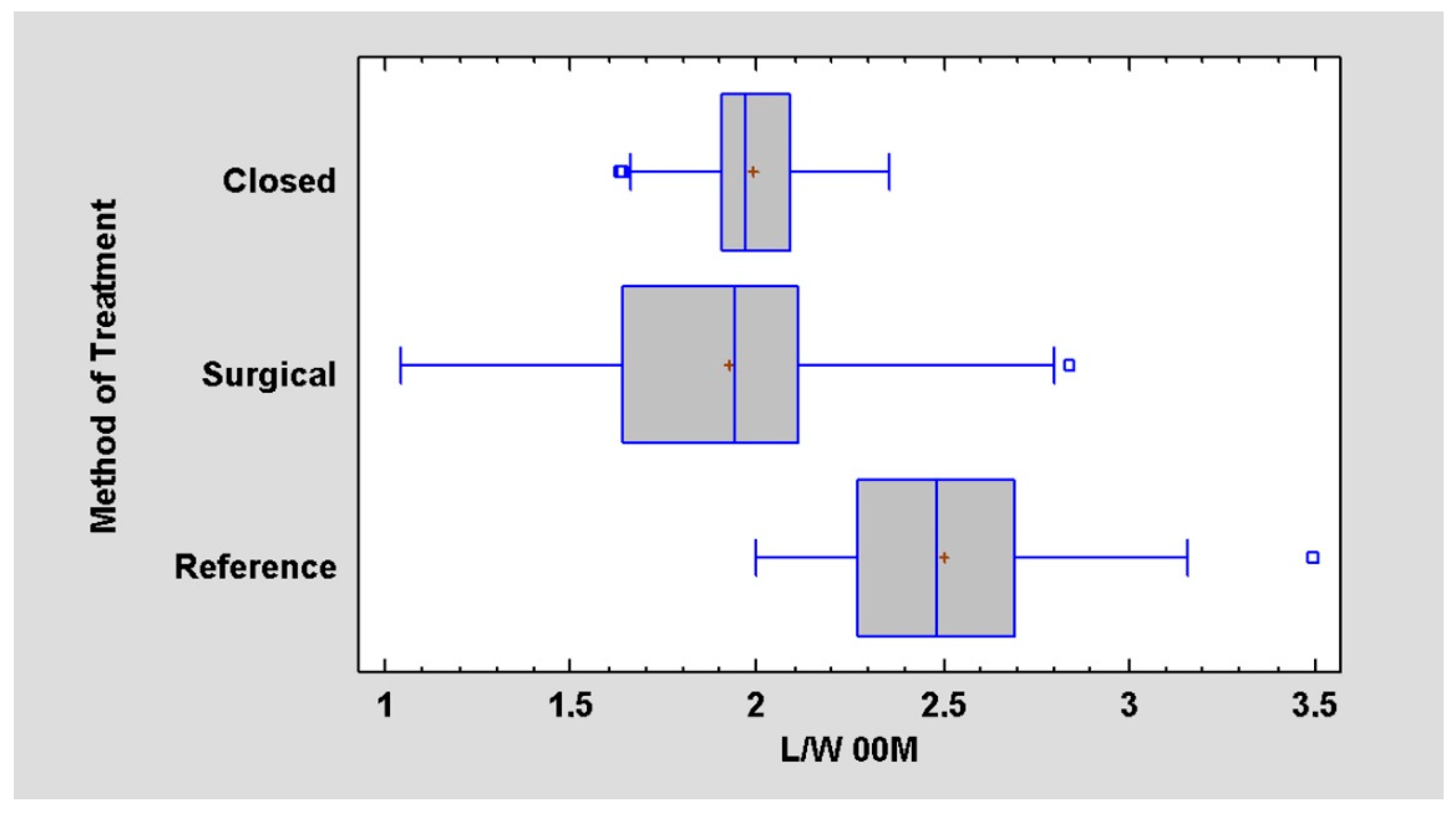
The fractured/operated side and the non-fractured/reference side were studied in both groups. The measurements of the greatest length and width of the lateral pterygoid muscle on both fractured and non-fractured sides were taken. Then, the calculation of length-to-width ratio was performed. The reference points (
Figure 1) for the measurements were the center of the mandibular pterygoid fovea (pterygoid pit) and the angle between the outer surface of the lateral plate of the pterygoid processus of the sphenoid bone and the posterior wall of the maxilla. In sagittal dimension of the lateral pterygoid muscle, the measurements were made from the central point in the pterygoid depression in an axis directed to the base of the lemma (which may also correspond to the center of the palate). Measurements of the muscle size in CT images were taken at regular time intervals—just after surgery (or during the first visit after fracture in case of conservative treatment), and 3, 6, 12, and 24 months after.
In addition, the focus was on the functional evaluation of surgically treated patients. Measurements of mandibular movements such as maximal interincisal opening, and ipsilateral and contralateral movement were taken. They were made one day after surgery, and then 6 months after and 12 months after, which is a standard protocol for clinic’s postoperative care.
The effect of the time that elapsed between injury and treatment, the effect of the duration of the surgical procedure, as well as age, gender, the cause of the injury, and the material of the screws used for osteosynthesis were also examined.
Statistical analysis was performed in Statgraphics Centurion 18 (Statgraphics Technologies Inc., The Plains City, VA, USA). A p value of less than 0.05 was considered statistically significant. One-way analysis of variance and regression analysis and independence χ2 test were done.
4. Discussion
In a growing number of centers, mandibular head fractures are treated surgically. The goal of this treatment is to restore anatomical conditions; however, as we notice, it also carries other implications. They are related, for example, with the lateral pterygoid muscle which is inserted into the pterygoid fovea on the mandible. Basing on CT images and measurements of the muscles, permanent morphological alterations in the lateral pterygoid muscle are observed.
The core of the research is to evaluate the condition of the muscle at the operated site and its evolution over a long period of time. A reference group is needed to understand the significance of this data. The split-mouth method used in the paper may be insufficient for some readers, because the mandible is, however, one bone and both condylar processes act as a functional unit. Thus, simply operating on one condyle causes some degree of dysfunction on the opposite side of the mandible. In order to understand how this degree of dysfunction may be caused by the surgical procedure itself, an extra refereed group was used, i.e., 15 patients with single condylar fractures, but treated only in a closed fashion. There is no impact of surgery in this control. It seems that such a double reference group gives a good frame of reference for the results obtained.
During the study, it was noted that muscle on the operated side becomes permanently wider and shorter, which suggests its more spherical image. Apart from morphological changes, functional changes were also observed.
According to different studies, it is established that the proper range of MIO (the greatest distance between the incisal edge of the maxillary central incisor to the incisal edge of the mandibular central incisor, when the mouth is opened as wide as possible painlessly [
12]) is 44–54 mm, whilst the normal range of lateral movements is 10 mm [
13,
14]. During the study, it was noted that the range of lateral movement to the contralateral side is permanently reduced. Can we do something to influence the distant functional outcome? It was noted that fixed factors such as patient’s gender or age do not statistically significantly affect the results. The factor that can be changed by the operator such as the fixing material used also does not affect the functional outcome. Fixation is mostly done with two or three screws. It is thought that two-screw fixation may be sufficient for the correct rigidity of the bone union [
15]. In some cases, omitting the third screw application would not change the osseous outcome of osteosynthesis, but would reduce the invasiveness observable in the condition of the lateral pterygoid muscle. Shortening the operation time and reducing the number of bores should support the return of activity in the musculoskeltal system.
On the contrary, a significant relationship was noted between the range of contralateral motion and the time from injury to treatment. The earlier the patient visits the ER and the earlier the treatment is initiated, the better the results will be. The distant functional outcome absolutely indicates the great importance of early surgical treatment. Taking into consideration authors’ clinical experiences, it was noted that, at the current stage of development of surgical techniques, late treatment (osteotomies) of the mandibular head unfortunately lead to poor results.
Taking all of the above into account, this question should be reconsidered: what does the surgical treatment offer the patient for the cost of permanent morphological and functional changes in the lateral pterygoid muscle? According to Neff’s 2020 publication [
16], surgical treatment may lead to omitting temporomandibular joint dysfunction (TMD), craniomandibular dysfunction (CMD), osteoarthrosis, pain, and, most importantly, ankylosis. The last complication may even lead to the necessity of TMJ replacement. Even though modern rapid TMJ prototyping techniques that are used nowadays make it possible to avoid some complications [
17], it is natural that the position of the muscle will change and, therefore, impact the mandible position.
Given the appropriate indications, both treatment options show acceptable results in most cases; however, it is crucial for therapeutic decision making that the long-term results of conservative treatment are much less predictable and may highly affect the health-related quality of life. According to researchers, closed reduction via intermaxillary fixation or solely functional training will not lead to physiological or anatomic recovery and can, at best, offer neuromuscular adaption of the affected joints [
18].
In terms of disturbing poor functional results, the reason seems to be that qualification for surgical treatment is not randomized, but dictated by clinical indications (e.g., patient with mandibular head dislocation will never qualify for conservative treatment, which leads to the conclusion that patients treated surgically are those, whose muscles were more affected by the injury from the beginning). As mentioned before, indications for surgical treatment were restrictive (shortening of the mandibular ramus of more than 2 mm and angulation of the proximal fragment of more than 30 degrees), which suggests that patients treated conservatively were the ones with a better initial state of the muscle.
A weakness of the study is the lack of data when it comes to the functional outcome of the patient treated with closed reduction. Following Skroch [
19], further investigation concerning the relationship between remodeling and flaring and alterations of the muscle pull would also help us to understand the issue more thoroughly. For the time being, it is not possible to state with the current study results if they could be generalised to other mandibular condyle fractures.