Validity of the Central Sensitization Inventory to Address Human Assumed Central Sensitization: Newly Proposed Clinically Relevant Values and Associations
Abstract
1. Introduction
2. Materials and Methods
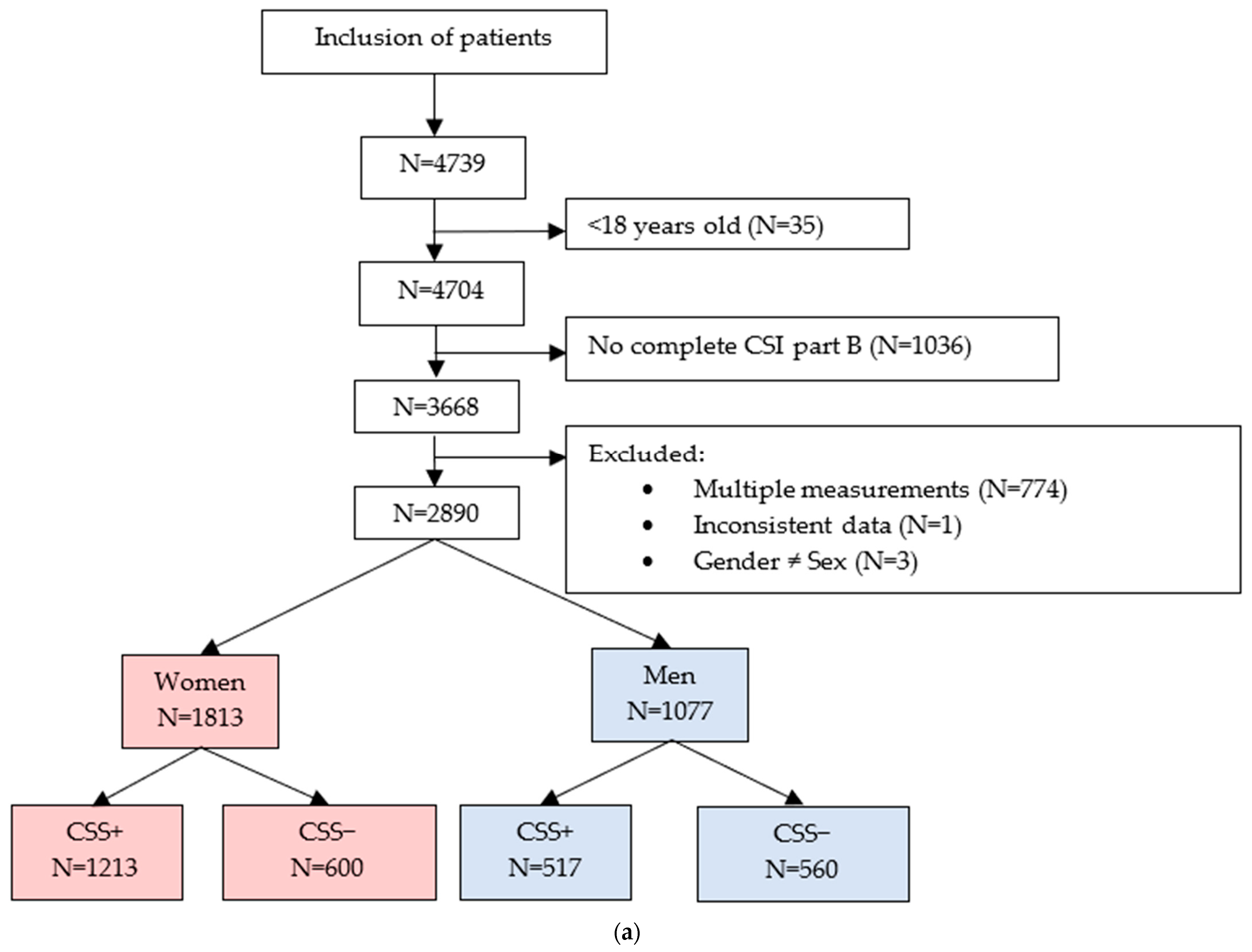
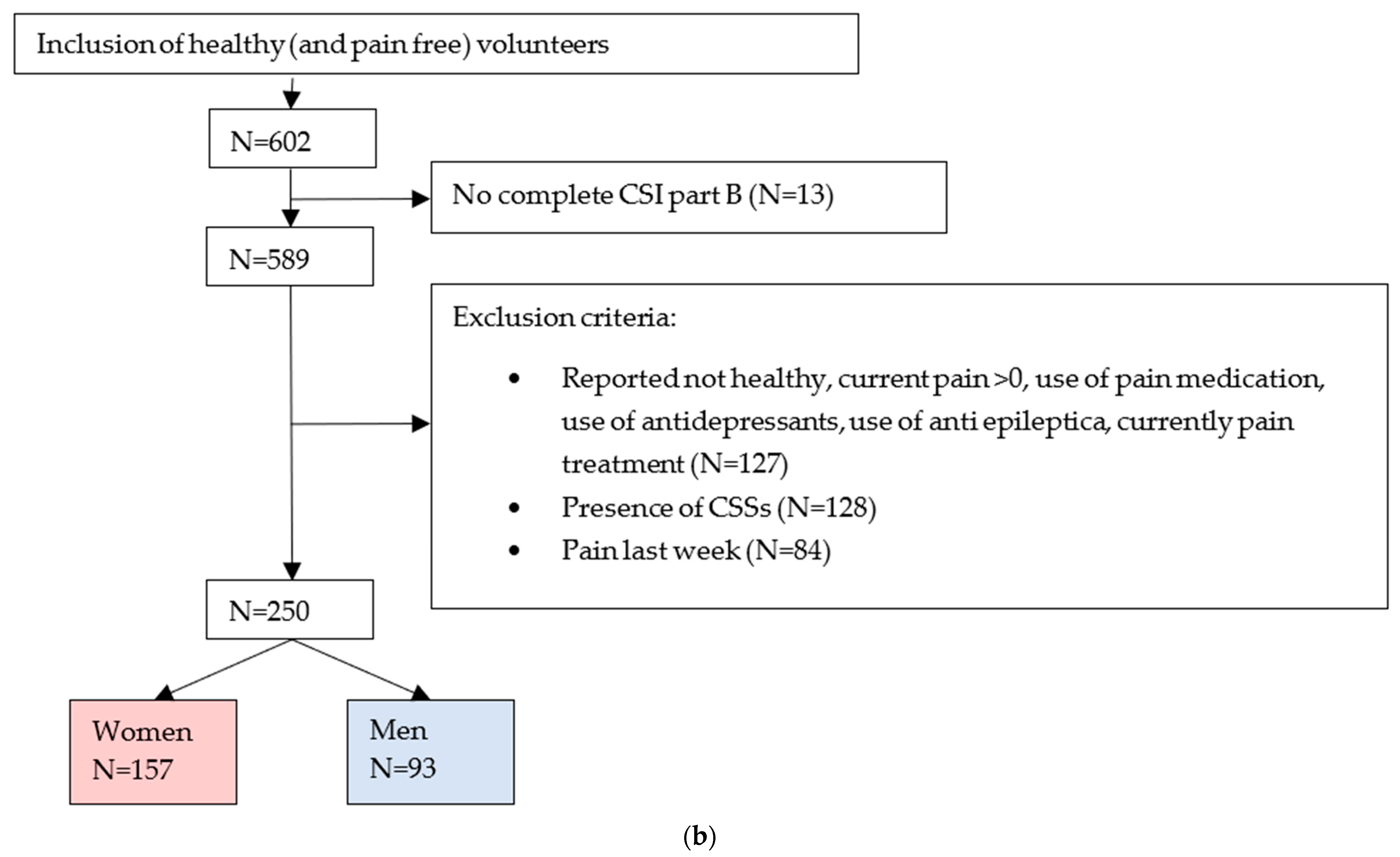
2.1. Participants
2.2. Measures
2.2.1. Central Sensitization Inventory (CSI)
2.2.2. Pain Catastrophizing Scale (PCS)
2.2.3. Pain Disability Index (PDI)
2.2.4. SF-12 Health Survey (SF-12)
2.2.5. Numeric Rating Scale (NRS) for Pain
2.2.6. Pain Location
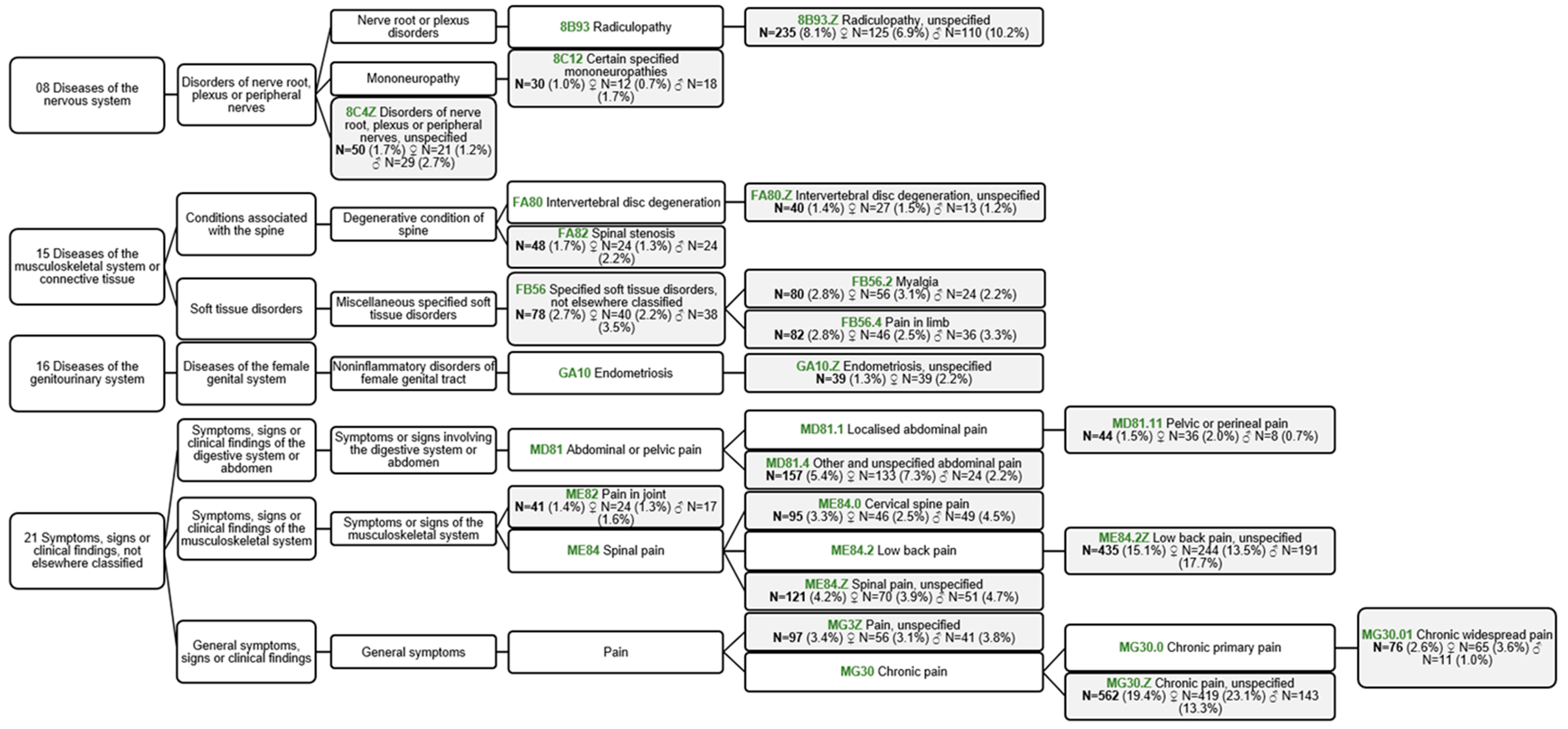
2.2.7. Pain Disorder
2.3. Sample Size Calculation for the Number of Healthy Volunteers
2.4. Data Analysis
3. Results
3.1. Cutoff Scores for the CSI
3.2. Differences between Groups
3.3. Associated Factors with the CSI Score
4. Discussion
4.1. Limitations and Strengths
4.2. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Loeser, J.D.; Treede, R.-D. The Kyoto protocol of IASP basic pain Terminology. Pain 2008, 137, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Woolf, C.J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 2011, 152, S2–S15. [Google Scholar] [CrossRef] [PubMed]
- Cayrol, T.; Draper-Rodi, J.; Fabre, L.; Pitance, L.; Van Den Broeke, E.N. Stuck in the middle with you: Why a broad-brush approach to defining central sensitization does not help clinicians and patients. J. Orthop. Sports Phys. Ther. 2021, 51, 204–206. [Google Scholar] [CrossRef]
- van den Broeke, E.N. Central sensitization and pain hypersensitivity: Some critical considerations. F1000Research 2018, 7, 1325. [Google Scholar] [CrossRef]
- Schuttert, I.; Timmerman, H.; Petersen, K.K.; McPhee, M.E.; Arendt-Nielsen, L.; Reneman, M.F.; Wolff, A.P. The Definition, Assessment, and Prevalence of (Human Assumed) Central Sensitisation in Patients with Chronic Low Back Pain: A Systematic Review. J. Clin. Med. 2021, 10, 5931. [Google Scholar] [CrossRef] [PubMed]
- Mayer, T.G.; Neblett, R.; Cohen, H.; Howard, K.J.; Choi, Y.H.; Williams, M.J.; Perez, Y.; Gatchel, R.J. The development and psychometric validation of the central sensitization inventory. Pain Pract. 2012, 12, 276–285. [Google Scholar] [CrossRef]
- PRIDEDALLAS.COM. Central Sensitisation Inventory. Available online: https://www.pridedallas.com/questionnaires/ (accessed on 25 February 2023).
- Kregel, J.; Vuijk, P.J.; Descheemaeker, F.; Keizer, D.; van der Noord, R.; Nijs, J.; Cagnie, B.; Meeus, M.; van Wilgen, P. The Dutch Central Sensitization Inventory (CSI): Factor analysis, discriminative power, and test-retest reliability. Clin. J. Pain 2016, 32, 624–630. [Google Scholar] [CrossRef]
- Kregel, J.; Schumacher, C.; Dolphens, M.; Malfliet, A.; Goubert, D.; Lenoir, D.; Cagnie, B.; Meeus, M.; Coppieters, I. Convergent validity of the Dutch central sensitization inventory: Associations with psychophysical pain measures, quality of life, disability, and pain cognitions in patients with chronic spinal pain. Pain Pract. 2018, 18, 777–787. [Google Scholar] [PubMed]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The Central Sensitization Inventory (CSI): Establishing clinically significant values for identifying central sensitivity syndromes in an outpatient chronic pain sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef]
- Mibu, A.; Nishigami, T.; Tanaka, K.; Manfuku, M.; Yono, S. Difference in the impact of central sensitization on pain-related symptoms between patients with chronic low back pain and knee osteoarthritis. J. Pain Res. 2019, 12, 1757–1765. [Google Scholar] [CrossRef]
- Neblett, R.; Hartzell, M.M.; Cohen, H.; Mayer, T.G.; Williams, M.; Choi, Y.; Gatchel, R.J. Ability of the central sensitization inventory to identify central sensitivity syndromes in an outpatient chronic pain sample. Clin. J. Pain 2015, 31, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Falling, C.; Stebbings, S.; Baxter, G.D.; Gearry, R.B.; Mani, R. Criterion validity and discriminatory ability of the central sensitization inventory short form in individuals with inflammatory bowel diseases. Scand. J. Pain 2021, 21, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Orr, N.L.; Wahl, K.J.; Lisonek, M.; Joannou, A.; Noga, H.; Albert, A.; Bedaiwy, M.A.; Williams, C.; Allaire, C.; Yong, P.J. Central sensitization inventory in endometriosis. Pain 2022, 163, e234–e245. [Google Scholar] [CrossRef] [PubMed]
- van Wilgen, C.P.; Vuijk, P.J.; Kregel, J.; Voogt, L.; Meeus, M.; Descheemaeker, F.; Keizer, D.; Nijs, J. Psychological Distress and Widespread Pain Contribute to the Variance of the Central Sensitization Inventory: A Cross-Sectional Study in Patients with Chronic Pain. Pain Pract. 2018, 18, 239–246. [Google Scholar] [CrossRef]
- Nijs, J.; Leysen, L.; Vanlauwe, J.; Logghe, T.; Ickmans, K.; Polli, A.; Malfliet, A.; Coppieters, I.; Huysmans, E. Treatment of central sensitization in patients with chronic pain: Time for change? Expert Opin. Pharmacother. 2019, 20, 1961–1970. [Google Scholar] [CrossRef]
- Graven-Nielsen, T.; Arendt-Nielsen, L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat. Rev. Rheumatol. 2010, 6, 599–606. [Google Scholar] [CrossRef]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef]
- Berkley, K.J. Sex differences in pain. Behav. Brain Sci. 1997, 20, 371–380. [Google Scholar]
- Sorge, R.E.; Totsch, S.K. Sex differences in pain. J. Neurosci. Res. 2017, 95, 1271–1281. [Google Scholar] [CrossRef]
- Wiesenfeld-Hallin, Z. Sex differences in pain perception. Gend. Med. 2005, 2, 137–145. [Google Scholar] [CrossRef]
- Roldan-Jimenez, C.; Perez-Cruzado, D.; Neblett, R.; Gatchel, R.; Cuesta-Vargas, A. Central Sensitization in Chronic Musculoskeletal Pain Disorders in Different Populations: A Cross-Sectional Study. Pain Med. 2020, 21, 2958–2963. [Google Scholar] [CrossRef]
- Sharma, S.; Jha, J.; Pathak, A.; Neblett, R. Translation, cross-cultural adaptation, and measurement properties of the Nepali version of the central sensitization inventory (CSI). BMC Neurol. 2020, 20, 286. [Google Scholar] [CrossRef]
- Walankar, P.P.; Panhale, V.P.; Patil, M.M. Psychosocial factors, disability and quality of life in chronic shoulder pain patients with central sensitization. Health Psychol. Res. 2020, 8, 8874. [Google Scholar] [CrossRef] [PubMed]
- Gervais-Hupe, J.; Pollice, J.; Sadi, J.; Carlesso, L.C. Validity of the central sensitization inventory with measures of sensitization in people with knee osteoarthritis. Clin. Rheumatol. 2018, 37, 3125–3132. [Google Scholar] [CrossRef]
- Andias, R.; Silva, A.G. Cross-Cultural Adaptation and Psychometric Properties of the European Portuguese Version of the Central Sensitization Inventory in Adolescents With Musculoskeletal Chronic Pain. Pain Pract. 2020, 20, 480–490. [Google Scholar] [CrossRef]
- Madi, M.; Hamzeh, H.; Abujaber, S.; Altubasi, I. Cross cultural adaptation, validity, and reliability of Central Sensitization Inventory in Arabic language. Disabil. Rehabil. 2022, 44, 8075–8083. [Google Scholar] [CrossRef]
- Klute, M.; Laekeman, M.; Kuss, K.; Petzke, F.; Dieterich, A.; Leha, A.; Neblett, R.; Ehrhardt, S.; Ulma, J.; Schafer, A. Cross-cultural adaptation and validation of the German Central Sensitization Inventory (CSI-GE). BMC Musculoskelet. Disord. 2021, 22, 708. [Google Scholar] [CrossRef] [PubMed]
- Chiarotto, A.; Viti, C.; Sulli, A.; Cutolo, M.; Testa, M.; Piscitelli, D. Cross-cultural adaptation and validity of the Italian version of the Central Sensitization Inventory. Musculoskelet. Sci. Pract. 2018, 37, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Mikkonen, J.; Luomajoki, H.; Airaksinen, O.; Neblett, R.; Selander, T.; Leinonen, V. Cross-cultural adaptation and validation of the Finnish version of the central sensitization inventory and its relationship with dizziness and postural control. BMC Neurol. 2021, 21, 141. [Google Scholar] [CrossRef]
- Ide, K.; Yasuda, T.; Hasegawa, T.; Yamato, Y.; Yoshida, G.; Banno, T.; Arima, H.; Oe, S.; Mihara, Y.; Ushirozako, H.; et al. Evaluation of the Central Sensitization Inventory Score in elderly adults with musculoskeletal examination. Mod. Rheumatol. 2021, 31, 885–889. [Google Scholar] [CrossRef]
- Tanaka, K.; Nishigami, T.; Mibu, A.; Manfuku, M.; Yono, S.; Shinohara, Y.; Tanabe, A.; Ono, R. Validation of the Japanese version of the Central Sensitization Inventory in patients with musculoskeletal disorders. PLoS ONE 2017, 12, e0188719. [Google Scholar] [CrossRef] [PubMed]
- Ohashi, Y.; Fukushima, K.; Inoue, G.; Uchida, K.; Koyama, T.; Tsuchiya, M.; Uchiyama, K.; Takahira, N.; Takaso, M. Central sensitization inventory scores correlate with pain at rest in patients with hip osteoarthritis: A retrospective study. BMC Musculoskelet. Disord. 2020, 21, 595. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, E.; Voogt, L.; Lenoir, D.; Coppieters, I.; Ickmans, K. Convergent validity of the Central Sensitization Inventory in chronic whiplash-associated disorders; associations with quantitative sensory testing, pain intensity, fatigue, and psychosocial factors. Pain Med. 2020, 21, 3401–3412. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Osman, A.; Barrios, F.X.; Kopper, B.A.; Hauptmann, W.; Jones, J.; O’Neill, E. Factor structure, reliability, and validity of the Pain Catastrophizing Scale. J. Behav. Med. 1997, 20, 589–605. [Google Scholar] [CrossRef]
- Pollard, C.A. Preliminary validity study of the pain disability index. Percept. Mot. Ski. 1984, 59, 974. [Google Scholar] [CrossRef]
- Soer, R.; Koke, A.J.A.; Vroomen, P.C.A.J.; Stegeman, P.; Smeets, R.J.E.M.; Coppes, M.H.; Reneman, M.F. Extensive Validation of the Pain Disability Index in 3 Groups of Patients With Musculoskeletal Pain. Spine 2013, 38, E562–E568. [Google Scholar] [CrossRef]
- Tait, R.C.; Pollard, C.A.; Margolis, R.B.; Duckro, P.N.; Krause, S.J. The Pain Disability Index—Psychometric and Validity Data. Arch. Phys. Med. Rehabil. 1987, 68, 438–441. [Google Scholar]
- Gronblad, M.; Hupli, M.; Wennerstrand, P.; Jarvinen, E.; Lukinmaa, A.; Kouri, J.P.; Karaharju, E.O. Intercorrelation and Test-Retest Reliability of the Pain Disability Index (Pdi) and the Oswestry Disability Questionnaire (Odq) and Their Correlation with Pain Intensity in Low-Back-Pain Patients. Clin. J. Pain 1993, 9, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Hays, R.D.; Sherbourne, C.D.; Mazel, R.M. The RAND 36-items Health Survey 1.0. Health Econ. 1993, 2, 10. [Google Scholar] [CrossRef] [PubMed]
- van der Zee, K.I.; Sanderman, R. Het Meten van de Algemene Gezondheidstoestand met de RAND-36: Een Handleiding; University of Groningen: Groningen, The Netherlands, 1993. [Google Scholar]
- Luo, X.M.; George, M.L.; Kakouras, I.; Edwards, C.L.; Pietrobon, R.; Richardson, W.; Hey, L. Reliability, validity, and responsiveness of the short form 12-item survey (SF-12) in patients with back pain. Spine 2003, 28, 1739–1745. [Google Scholar] [CrossRef]
- Ibrahim, A.A.; Akindele, M.O.; Ganiyu, S.O.; Kaka, B.; Abdullahi, B.B.; Sulaiman, S.K.; Fatoye, F. The Hausa 12-item short-form health survey (SF-12): Translation, cross-cultural adaptation and validation in mixed urban and rural Nigerian populations with chronic low back pain. PLoS ONE 2020, 15, e0232223. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef]
- World Health Organization. ICD-11; International Classification of Diseases 11th Revision: The global Standard for Diagnostic Health Information. Available online: https://icd.who.int/en (accessed on 25 February 2023).
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic pain as a symptom or a disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A classification of chronic pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef]
- World Health Organization. ICD 10 to 11 Mapping. Available online: https://icd.who.int/browse11/Downloads/Download?fileName=mapping.zip (accessed on 30 December 2022).
- Advisors, T.R.A. Sample Size Table. Available online: https://www.research-advisors.com/tools/SampleSize.htm (accessed on 25 February 2023).
- Zweig, M.H.; Campbell, G. Receiver Operating Characteristic (Roc) Plots—A Fundamental Evaluation Tool in Clinical Medicine (Vol 39, Pg 561, 1993). Clin. Chem. 1993, 39, 1589. [Google Scholar] [CrossRef]
- Habibzadeh, F.; Habibzadeh, P.; Yadollahie, M. On determining the most appropriate test cut-off value: The case of tests with continuous results. Biochem. Medica 2016, 26, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Brenner, H.; Gefeller, O. Variation of sensitivity, specificity, likelihood ratios and predictive values with disease prevalence. Stat. Med. 1997, 16, 981–991. [Google Scholar] [CrossRef]
- Fluss, R.; Faraggi, D.; Reiser, B. Estimation of the Youden Index and its associated cutoff point. Biom. J. J. Math. Methods Biosci. 2005, 47, 458–472. [Google Scholar] [CrossRef]
- Greiner, M.; Pfeiffer, D.; Smith, R.D. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev. Vet. Med. 2000, 45, 23–41. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; Sage Publications Ltd.: London, UK, 2018. [Google Scholar]
- Larsen, D.B.; Laursen, M.; Edwards, R.R.; Simonsen, O.; Arendt-Nielsen, L.; Petersen, K.K. The combination of preoperative pain, conditioned pain modulation, and pain catastrophizing predicts postoperative pain 12 Months after total knee arthroplasty. Pain Med. 2021, 22, 1583–1590. [Google Scholar] [CrossRef]
- Heinze, G.; Dunkler, D. Five myths about variable selection. Transpl. Int. 2017, 30, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Holm, L.A.; Nim, C.G.; Lauridsen, H.H.; Filtenborg, J.B.; O’Neill, S.F. Convergent validity of the central sensitization inventory and experimental testing of pain sensitivity. Scand. J. Pain 2022, 22, 597–613. [Google Scholar] [CrossRef]
- Echeita, J.A.; Dekker, R.; Preuper, H.R.S.; Reneman, M.F. Maximal cardiopulmonary exercise test in patients with chronic low back pain: Feasibility, tolerance and relation with central sensitization. An observational study. Disabil. Rehabil. 2022, 44, 6287–6294. [Google Scholar] [CrossRef] [PubMed]
- Hassett, A.L.; Radvanski, D.C.; Vaschillo, E.G.; Vaschillo, B.; Sigal, L.H.; Karavidas, M.K.; Buyske, S.; Lehrer, P.M. A pilot study of the efficacy of heart rate variability (HRV) biofeedback in patients with fibromyalgia. Appl. Psychophysiol. Biofeedback 2007, 32, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zafereo, J.; Wang-Price, S.; Kandil, E. Quantitative Sensory Testing Discriminates Central Sensitization Inventory Scores in Participants with Chronic Musculoskeletal Pain: An Exploratory Study. Pain Pract. 2021, 21, 547–556. [Google Scholar] [CrossRef]
- Perkins, N.J.; Schisterman, E.F. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am. J. Epidemiol. 2006, 163, 670–675. [Google Scholar] [CrossRef]
- Bezerra, M.C.; Bittencourt, J.V.; Reis, F.J.J.; de Almeida, R.S.; Meziat, N.A.M.; Nogueira, L.A.C. Central Sensitization Inventory is a useless instrument for detection of the impairment of the conditioned pain modulation in patients with chronic musculoskeletal pain. Jt. Bone Spine 2021, 88, 105127. [Google Scholar] [CrossRef] [PubMed]
- Kendall, P.C.; Marrs-Garcia, A.; Nath, S.R.; Sheldrick, R.C. Normative comparisons for the evaluation of clinical significance. J. Consult. Clin. Psychol. 1999, 67, 285–299. [Google Scholar] [CrossRef] [PubMed]
- Kendall, P.C.; Sheldrick, R.C. Normative data for normative comparisons. J. Consult. Clin. Psychol. 2000, 68, 767–773. [Google Scholar] [CrossRef]
- Adams, G.R.; Gandhi, W.; Harrison, R.; van Reekum, C.M.; Wood-Anderson, D.; Gilron, I.; Salomons, T.V. Do “central sensitization” questionnaires reflect measures of nociceptive sensitization or psychological constructs? A systematic review and meta-analyses. Pain 2023, 164, 1222–1239. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Roldan-Jimenez, C.; Neblett, R.; Gatchel, R.J. Cross-cultural adaptation and validity of the Spanish central sensitization inventory. Springerplus 2016, 5, 1837. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Vargas, A.I.; Neblett, R.; Chiarotto, A.; Kregel, J.; Nijs, J.; van Wilgen, C.P.; Pitance, L.; Knezevic, A.; Gatchel, R.J.; Mayer, T.G.; et al. Dimensionality and Reliability of the Central Sensitization Inventory in a Pooled Multicountry Sample. J. Pain 2018, 19, 317–329. [Google Scholar] [CrossRef] [PubMed]
- Akeda, K.; Takegami, N.; Yamada, J.; Fujiwara, T.; Nishimura, A.; Sudo, A. Central Sensitization in Chronic Low Back Pain: A Population-Based Study of a Japanese Mountain Village. J. Pain Res. 2021, 14, 1271–1280. [Google Scholar] [CrossRef]
- Falling, C.; Stebbings, S.; Baxter, G.D.; Siegel, C.A.; Gearry, R.B.; Nijs, J.; Mani, R. Symptoms of central sensitization in patients with inflammatory bowel diseases: A case-control study examining the role of musculoskeletal pain and psychological factors. Scand. J. Pain 2021, 21, 283–295. [Google Scholar] [CrossRef]
- Wang, D.; Frey-Law, L.A. Multisensory sensitivity differentiates between multiple chronic pain conditions and pain-free individuals. Pain 2023, 164, e91–e102. [Google Scholar] [CrossRef]
- Shraim, M.A.; Massé-Alarie, H.; Hodges, P.W. Methods to discriminate between mechanism-based categories of pain experienced in the musculoskeletal system: A systematic review. Pain 2021, 162, 1007–1037. [Google Scholar] [CrossRef]
- Cuesta-Vargas, A.I.; Neblett, R.; Nijs, J.; Chiarotto, A.; Kregel, J.; van Wilgen, C.P.; Pitance, L.; Knezevic, A.; Gatchel, R.J.; Mayer, T.G. Establishing Central Sensitization–Related Symptom Severity Subgroups: A Multicountry Study Using the Central Sensitization Inventory. Pain Med. 2020, 21, 2430–2440. [Google Scholar] [CrossRef]
- Neblett, R.; Hartzell, M.M.; Mayer, T.G.; Cohen, H.; Gatchel, R.J. Establishing clinically relevant severity levels for the central sensitization inventory. Pain Pract. 2017, 17, 166–175. [Google Scholar] [CrossRef]
- van der Noord, R.; Paap, D.; van Wilgen, C.P. Convergent validity and clinically relevant categories for the Dutch Central Sensitization Inventory in patients with chronic pain. J. Appl. Biobehav. Res. 2018, 23, e12119. [Google Scholar] [CrossRef]
| Patients | Total Group | Women | Men | CSS+ | CSS− | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CSS+ | CSS− | CSS+ | CSS− | CSS+ | CSS− | Women vs. Men | Women vs. Men | ||||||||||||
| N | Mean ± SD % | N | Mean ± SD % | p | N | Mean ± SD % | N | Mean ± SD % | p | N | Mean ± SD % | N | Mean ± SD % | p | p | p | |||
| Age (years) | 1730 | 49.5 ± 15.2 | 1160 | 50.8 ± 17.1 | 0.028 * | 1213 | 47.9 ± 15.2 | 600 | 47.9 ± 17.9 | 0.947 | 517 | 53.1 ± 14.5 | 560 | 54.1 ± 15.7 | 0.326 | <0.001 * | <0.001 * | ||
| Height (cm) | 1370 | 173.2 ± 9.5 | 992 | 175.2 ± 10.1 | <0.001 * | 955 | 169.2 ± 7.2 | 508 | 168.7 ± 7.2 | 0.287 | 415 | 182.6 ± 7.1 | 484 | 182.0 ± 8.0 | 0.210 | <0.001 * | <0.001 * | ||
| Weight (kg) | 1370 | 82.4 ± 18.5 | 992 | 82.2 ± 17.9 | 0.882 | 955 | 78.3 ± 17.1 | 508 | 74.8 ± 16.2 | <0.001 * | 415 | 91.8 ± 18.3 | 484 | 90.0 ± 16.3 | 0.135 | <0.001 * | <0.001 * | ||
| BMI (kg/cm²) | 1369 | 27.4 ± 5.5 | 992 | 26.7 ± 5.1 | 0.002 * | 954 | 27.4 ± 5.8 | 508 | 26.3 ± 5.7 | 0.001 * | 415 | 27.5 ± 5.0 | 484 | 27.1 ± 4.3 | 0.286 | 0.717 | 0.008 * | ||
| CSI (0−100) | 1730 | 44.8 ± 14.5 | 1160 | 33.3 ± 14.2 | <0.001 * | 1213 | 46.0 ± 14.4 | 600 | 34.6 ± 14.4 | <0.001 * | 517 | 42.0 ± 14.3 | 560 | 31.9 ± 13.9 | <0.001 * | <0.001 * | 0.001 * | ||
| Pain now (0−10) | 1147 | 6.3 ± 2.2 | 919 | 6.1 ± 2.3 | 0.026 * | 785 | 6.3 ± 2.2 | 463 | 6.0 ± 2.3 | 0.060 | 362 | 6.3 ± 2.2 | 456 | 6.1 ± 2.3 | 0.198 | 0.853 | 0.651 | ||
| Mean pain last 7 days (0–10) | 1430 | 6.7 ± 1.8 | 1024 | 6.7 ± 1.8 | 0.680 | 991 | 6.7 ± 1.8 | 523 | 6.6 ± 1.8 | 0.382 | 439 | 6.7 ± 1.8 | 501 | 6.7 ± 1.8 | 0.826 | 0.958 | 0.296 | ||
| Worst pain (0–10) | 1430 | 8.5 ± 1.4 | 1024 | 8.4 ± 1.5 | 0.155 | 991 | 8.5 ± 1.3 | 523 | 8.4 ± 1.5 | 0.085 | 439 | 8.4 ± 1.5 | 501 | 8.4 ± 1.4 | 0.978 | 0.237 | 0.667 | ||
| PCS (0–52) | 1686 | 22.1 ± 11.6 | 1145 | 21.8 ± 11.4 | 0.445 | 1171 | 21.3 ± 11.3 | 586 | 20.9 ± 11.4 | 0.533 | 515 | 24.0 ± 11.9 | 559 | 22.7 ± 11.3 | 0.059 | <0.001 * | 0.009 * | ||
| PDI (0–70) | 1170 | 40.4 ± 13.0 | 800 | 38.4 ± 14.7 | 0.001 * | 797 | 40.4 ± 12.9 | 388 | 37.9 ± 15.0 | 0.005 * | 373 | 40.5 ± 13.3 | 412 | 38.9 ± 14.4 | 0.092 | 0.878 | 0.349 | ||
| Number of pain locations | 1730 | 2.5 ± 2.1 | 1160 | 1.8 ± 1.3 | <0.001 * | 1213 | 2.6 ± 2.2 | 600 | 1.8 ± 1.3 | <0.001 * | 517 | 2.3 ± 1.9 | 560 | 1.7 ± 1.3 | <0.001 * | 0.001 * | 0.159 | ||
| Number of CSSs (0–10) | 1730 | 2.0 ± 1.2 | 1160 | 0 | <0.001 * | 1213 | 2.1 ± 1.2 | 600 | 0 | <0.001 * | 517 | 1.7 ± 1.0 | 560 | 0 | <0.001 * | <0.001 * | NA | ||
| Physical component SF-12 (0–100) | 1582 | 38.9 ± 5.6 | 1090 | 39.3 ± 5.9 | 0.090 | 1104 | 38.7 ± 5.5 | 566 | 39.0 ± 5.7 | 0.303 | 478 | 39.3 ± 5.9 | 524 | 39.6 ± 6.1 | 0.463 | 0.085 | 0.154 | ||
| Mental component SF-12 (0–100) | 1582 | 45.2 ± 7.3 | 1090 | 47.4 ± 7.3 | <0.001 * | 1104 | 45.4 ± 7.1 | 566 | 47.5 ± 7.3 | <0.001 * | 478 | 44.6 ± 7.8 | 524 | 47.2 ± 7.4 | <0.001 * | 0.060 | 0.615 | ||
| Pain locations | <0.001 * | <0.001 * | 0.003 * | 0.008 * | <0.001 * | ||||||||||||||
| Head | 35 | 2.0% | 24 | 2.1% | 23 | 1.9% | 12 | 2.0% | 12 | 2.3% | 12 | 2.1% | |||||||
| Neck, shoulders, high back and arms | 102 | 5.9% | 66 | 5.7% | 59 | 4.9% | 24 | 4.0% | 43 | 8.3% | 42 | 7.5% | |||||||
| Elbow, wrist, hand | 14 | 0.8% | 6 | 0.5% | 8 | 0.7% | 3 | 0.5% | 6 | 1.2% | 3 | 0.5% | |||||||
| Lower back | 323 | 18.7% | 315 | 27.2% | 213 | 17.6% | 155 | 25.8% | 110 | 21.3% | 160 | 28.6% | |||||||
| Hip, knee | 30 | 1.7% | 20 | 1.7% | 19 | 1.6% | 9 | 1.5% | 11 | 2.1% | 11 | 2.0% | |||||||
| Foot, ankle | 24 | 1.4% | 40 | 3.4% | 16 | 1.3% | 12 | 2.0% | 8 | 1.5% | 28 | 5.0% | |||||||
| Chest, abdomen | 93 | 5.4% | 72 | 6.2% | 72 | 5.9% | 47 | 7.8% | 21 | 4.1% | 25 | 4.5% | |||||||
| Pelvis | 61 | 3.5% | 39 | 3.4% | 49 | 4.0% | 29 | 4.8% | 12 | 2.3% | 10 | 1.8% | |||||||
| Other | 121 | 7.0% | 104 | 9.0% | 79 | 6.5% | 49 | 8.2% | 42 | 8.1% | 55 | 9.8% | |||||||
| Multiple locations | 927 | 53.6% | 474 | 40.9% | 675 | 55.6% | 260 | 43.3% | 252 | 48.7% | 214 | 38.2% | |||||||
| Healthy Volunteers | Total Group | Women | Men | Women vs. Men | CSS+ vs. Healthy Volunteers | CSS− vs. Healthy Volunteers | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total group | Women | Men | Total group | Women | Men | ||||||||
| N | Mean ± SD | N | Mean ± SD | N | Mean ± SD | p | p | p | p | p | p | p | |
| Age (years) | 250 | 43.2 ± 16.1 | 157 | 41.6 ± 14.2 | 93 | 45.9 ± 18.6 | 0.056 | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| Height (cm) | 250 | 175.8 ± 9.2 | 157 | 170.9 ± 6.2 | 93 | 184.0 ± 7.2 | <0.001 * | <0.001 * | 0.004 * | 0.093 | 0.412 | 0.001 * | 0.025 * |
| Weight (kg) | 250 | 75.2 ± 14.9 | 157 | 69.9 ± 12.7 | 93 | 84.2 ± 14.1 | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | 0.001 * |
| BMI (kg/cm²) | 250 | 24.2 ± 3.8 | 157 | 23.9 ± 4.0 | 93 | 24.8 ± 3.3 | 0.067 | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| CSI (0–100) | 250 | 16.4 ± 8.6 | 157 | 17.3 ± 8.7 | 93 | 15.1 ± 8.3 | 0.049 * | <0.001* | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| Total Group (N = 1730) vs. Healthy Volunteers (N = 250); AUC: 0.953 | |||
|---|---|---|---|
| Cutoff Score | Youden Index | Sensitivity | Specificity |
| 28 | 0.7775 | 0.8855 | 0.8920 |
| 29 | 0.7785 | 0.8705 | 0.9080 |
| 30 | 0.7818 | 0.8538 | 0.9280 |
| 31 | 0.7701 | 0.8341 | 0.9360 |
| 32 | 0.7648 | 0.8208 | 0.9440 |
| Women (N = 1213) vs. Healthy Female Volunteers (N = 157) AUC: 0.956 | |||
| Cutoff Score | Youden Index | Sensitivity | Specificity |
| 30 | 0.7913 | 0.8805 | 0.9108 |
| 31 | 0.7851 | 0.8615 | 0.9236 |
| 32 | 0.7782 | 0.8483 | 0.9299 |
| 33 | 0.7934 | 0.8252 | 0.9682 |
| 34 | 0.7736 | 0.8054 | 0.9682 |
| 35 | 0.7505 | 0.7824 | 0.9682 |
| Men (N = 517) vs. Healthy Male Volunteers (N = 93) AUC: 0.947 | |||
| Cutoff Score | Youden Index | Sensitivity | Specificity |
| 23 | 0.7497 | 0.9110 | 0.8387 |
| 24 | 0.7674 | 0.9072 | 0.8602 |
| 25 | 0.8037 | 0.8897 | 0.9140 |
| 26 | 0.7883 | 0.8743 | 0.9140 |
| 27 | 0.7708 | 0.8569 | 0.9140 |
| Total Group | Women | Men | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | R | adj. R2 | I | β | p | N | R | adj. R2 | I | β | p | N | R | adj. R2 | I | β | p | |
| Sex | 2890 | 0.171 | 0.029 | 31.314 | 5.450 | <0.001 | ||||||||||||
| Age | 2890 | 0.158 | 0.025 | 47.803 | −0.152 | <0.001 | 1813 | 0.133 | 0.017 | 48.266 | −0.126 | <0.001 | 1077 | 0.132 | 0.016 | 43.746 | −0.130 | <0.001 |
| BMI | 2361 | 0.088 | 0.007 | 32.450 | 0.251 | <0.001 | 1462 | 0.120 | 0.014 | 32.834 | 0.318 | <0.001 | 899 | 0.043 | 0.001 | 32.085 | 0.134 | 0.201 |
| Pain severity | 2454 | 0.212 | 0.045 | 27.321 | 1.784 | <0.001 | 1514 | 0.192 | 0.036 | 30.609 | 1.608 | <0.001 | 940 | 0.260 | 0.067 | 21.574 | 2.134 | <0.001 |
| PCS | 2831 | 0.328 | 0.107 | 30.512 | 0.440 | <0.001 | 1757 | 0.318 | 0.101 | 33.209 | 0.429 | <0.001 | 1074 | 0.406 | 0.164 | 24.570 | 0.521 | <0.001 |
| PDI | 1970 | 0.401 | 0.160 | 22.876 | 0.449 | <0.001 | 1185 | 0.383 | 0.146 | 25.989 | 0.428 | <0.001 | 785 | 0.446 | 0.198 | 18.161 | 0.481 | <0.001 |
| Number of Pain locations | 2890 | 0.400 | 0.160 | 32.730 | 3.344 | <0.001 | 1813 | 0.410 | 0.168 | 34.580 | 3.225 | <0.001 | 1077 | 0.353 | 0.125 | 30.255 | 3.262 | <0.001 |
| Number of CSSs | 2890 | 0.467 | 0.218 | 33.764 | 5.332 | <0.001 | 1813 | 0.459 | 0.210 | 35.160 | 4.935 | <0.001 | 1077 | 0.429 | 0.183 | 32.027 | 5.745 | <0.001 |
| PC SF-12 | 2672 | 0.215 | 0.046 | 62.279 | −0.574 | <0.001 | 1670 | 0.205 | 0.041 | 63.320 | −0.558 | <0.001 | 1002 | 0.219 | 0.047 | 57.835 | −0.545 | <0.001 |
| MC SF-12 | 2672 | 0.518 | 0.268 | 89.414 | −1.076 | <0.001 | 1670 | 0.515 | 0.264 | 91.992 | −1.086 | <0.001 | 1002 | 0.549 | 0.301 | 85.461 | −1.068 | <0.001 |
| Group | Total Group | Women | Men | |||
|---|---|---|---|---|---|---|
| unadjusted R2 | 0.580 | 0.579 | 0.550 | |||
| adjusted R2 | 0.577 | 0.576 | 0.545 | |||
| β | CI 95% | β | CI 95% | β | CI 95% | |
| Constant | 69.71 | 60.88–78.53 | 79.43 | 68.35–90.52 | 65.38 | 53.67–77.08 |
| Sex | 2.79 | 1.72–3.86 | - | - | - | - |
| Age(years) | −0.07 | −0.10–−0.03 | −0.10 | −0.15–−0.05 | - | - |
| BMI | 0.10 | 0.01–0.20 | 0.13 | 0.01–0.24 | - | - |
| Pain severity (NRS) | −0.36 | −0.72–−0.01 | - | - | - | - |
| Pain catastrophizing (PCS) | 0.16 | 0.11–0.21 | 0.09 | 0.02–0.16 | 0.23 | 0.16–0.31 |
| Pain disability (PDI) | 0.13 | 0.08–0.18 | 0.10 | 0.04–0.16 | 0.12 | 0.05–0.19 |
| Number of pain locations | 2.18 | 1.91–2.44 | 2.24 | 1.91–2.56 | 2.05 | 1.59–2.50 |
| Number of CSSs (CSI part B) | 3.24 | 2.83–3.66 | 3.21 | 2.71–3.71 | 3.23 | 2.50–3.96 |
| Physical component (SF-12) | −0.40 | −0.50–−0.30 | −0.40 | −0.54–−0.25 | −0.44 | −0.60–−0.29 |
| Mental component (SF-12) | −0.73 | −0.82–−0.64 | −0.80 | −0.92–−0.67 | −0.63 | −0.76–−0.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schuttert, I.; Wolff, A.P.; Schiphorst Preuper, R.H.R.; Malmberg, A.G.G.A.; Reneman, M.F.; Timmerman, H. Validity of the Central Sensitization Inventory to Address Human Assumed Central Sensitization: Newly Proposed Clinically Relevant Values and Associations. J. Clin. Med. 2023, 12, 4849. https://doi.org/10.3390/jcm12144849
Schuttert I, Wolff AP, Schiphorst Preuper RHR, Malmberg AGGA, Reneman MF, Timmerman H. Validity of the Central Sensitization Inventory to Address Human Assumed Central Sensitization: Newly Proposed Clinically Relevant Values and Associations. Journal of Clinical Medicine. 2023; 12(14):4849. https://doi.org/10.3390/jcm12144849
Chicago/Turabian StyleSchuttert, Ingrid, André P. Wolff, Rita H. R. Schiphorst Preuper, Alec G. G. A. Malmberg, Michiel F. Reneman, and Hans Timmerman. 2023. "Validity of the Central Sensitization Inventory to Address Human Assumed Central Sensitization: Newly Proposed Clinically Relevant Values and Associations" Journal of Clinical Medicine 12, no. 14: 4849. https://doi.org/10.3390/jcm12144849
APA StyleSchuttert, I., Wolff, A. P., Schiphorst Preuper, R. H. R., Malmberg, A. G. G. A., Reneman, M. F., & Timmerman, H. (2023). Validity of the Central Sensitization Inventory to Address Human Assumed Central Sensitization: Newly Proposed Clinically Relevant Values and Associations. Journal of Clinical Medicine, 12(14), 4849. https://doi.org/10.3390/jcm12144849






