When Eating Intuitively Is Not Always a Positive Response: Using Machine Learning to Better Unravel Eaters Profiles
Abstract
:1. Introduction
1.1. Holistic Portrait of Eaters
1.2. Eating during the COVID-19 Pandemic
1.3. Using Machine Learning to Provide a New Empirical Perspective on Data about Eaters Profiles
2. Materials and Methods
2.1. Sample
2.2. Assessment Measures
2.3. Procedure
2.4. Statistical Analyses
3. Results
3.1. Identification of the Number of Clusters
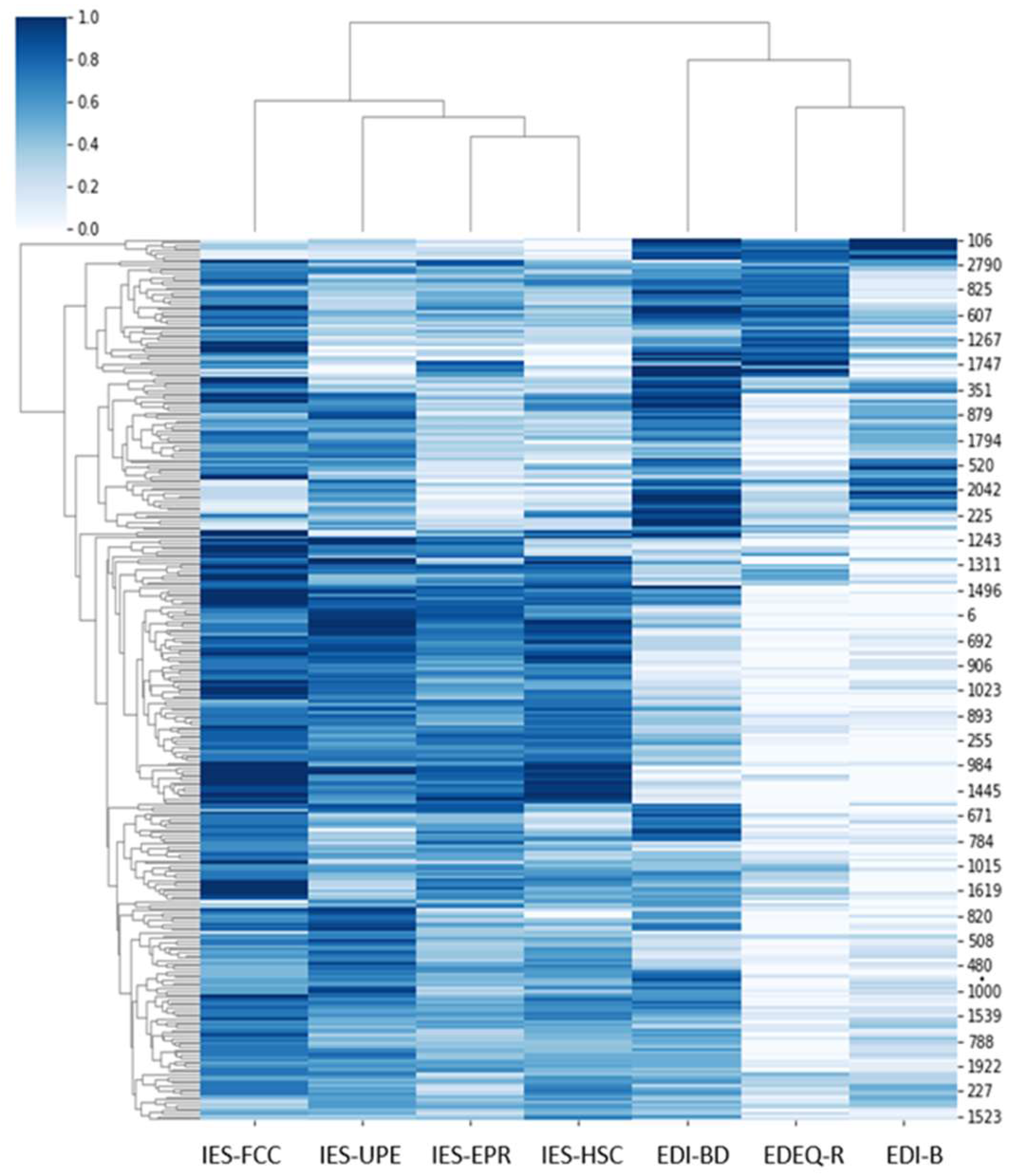
3.2. Validation of the 7-Cluter Model
3.3. Descriptive Interpretation of the Clusters
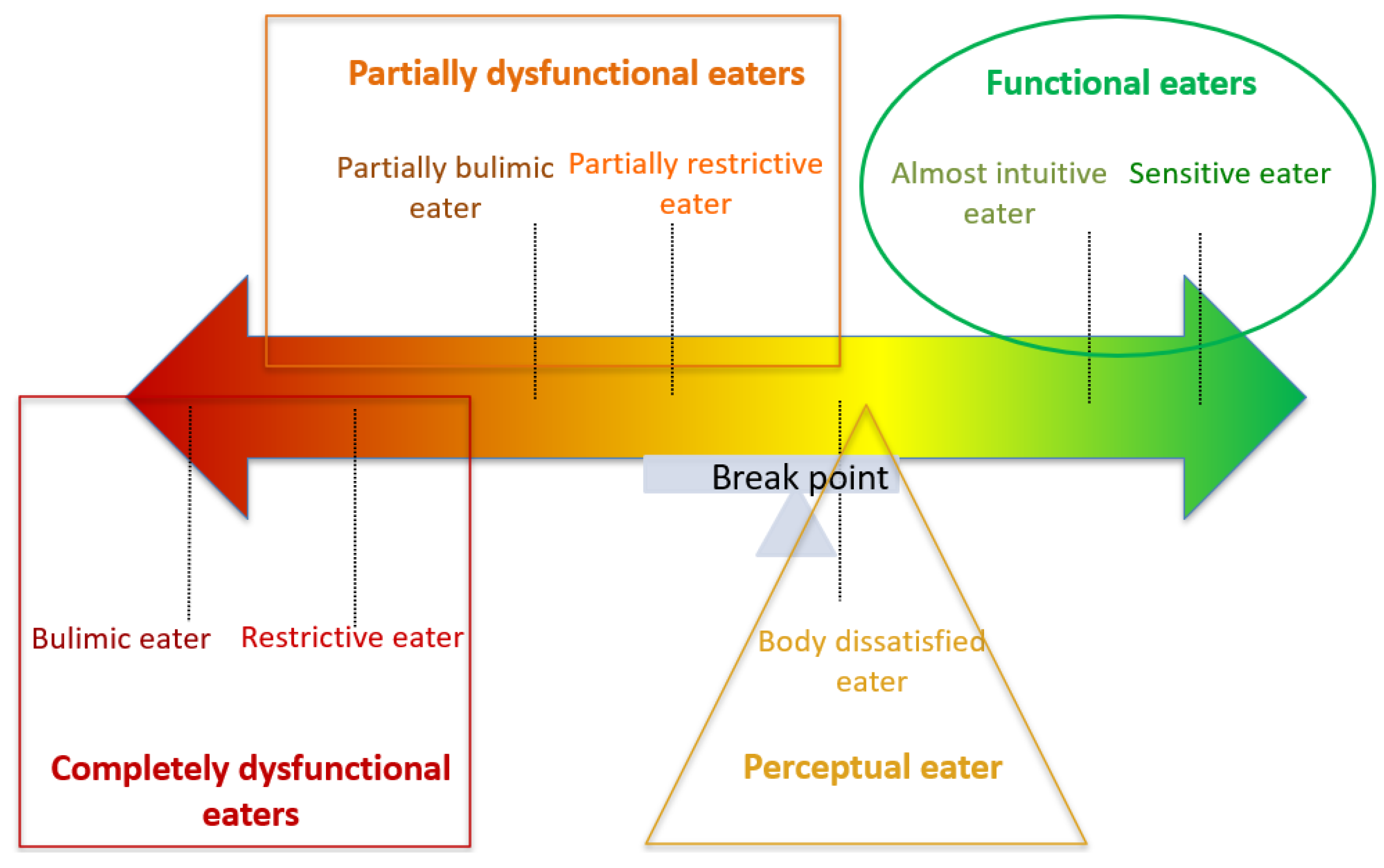
4. Discussion
4.1. Category 1: Completely Dysfunctional Eaters
4.2. Category 2: Partially Dysfunctional Eaters
4.3. Category 3: Perceptual Eater
4.4. Category 4: Functional Eaters
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fischler, C. Food, self and identity. Soc. Sci. Inf. 1988, 27, 275–292. [Google Scholar] [CrossRef]
- Giachetti, I. Identités des Mangeurs, Images des Aliments; Polytechnica: Paris, France, 1996. [Google Scholar]
- Strodl, E.; Markey, C.; Aimé, A.; Rodgers, R.F.; Dion, J.; Coco, G.L.; Gullo, S.; McCabe, M.; Mellor, D.; Granero-Gallegos, A.; et al. A cross-country examination of emotional eating, restrained eating and intuitive eating: Measurement Invariance across eight countries. Body Image 2020, 35, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Stice, E. A review of the evidence for a sociocultural model of bulimia nervosa and an exploration of the mechanisms of action. Clin. Psychol. Rev. 1994, 14, 633–661. [Google Scholar] [CrossRef]
- Van Strien, T. Dieting, dissatisfaction with figure and sex role orientation in women. Int. J. Eat. Disord. 1989, 8, 455–462. [Google Scholar] [CrossRef]
- Kerin, J.L.; Webb, H.J.; Zimmer-Gembeck, M.J. Intuitive, mindful, emotional, external and regulatory eating behaviours and beliefs: An investigation of the core components. Appetite 2019, 132, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Polivy, J.; Herman, C.P. Dieting and binging: A causal analysis. Am. Psychol. 1985, 40, 193–201. [Google Scholar] [CrossRef]
- Polivy, J.; Herman, C.P.; Mills, J.S. What is restrained eating and how do we identify it? Appetite 2020, 155, 104820. [Google Scholar] [CrossRef]
- Stice, E.; Nemeroff, C.; Shaw, H.E. Test of the dual pathway model of bulimia nervosa: Evidence for dietary restraint and affect regulation mechanisms. J. Soc. Clin. Psychol. 1996, 15, 340–363. [Google Scholar] [CrossRef]
- Bruch, H. Psychological aspects in overeating and obesity. Psychosomatics 1964, 5, 269–274. [Google Scholar] [CrossRef]
- Lindeman, M.; Stark, K. Emotional eating and eating disorder psychopathology. Eat. Disord. 2001, 9, 251–259. [Google Scholar] [CrossRef]
- Van Strien, T.; Engels, R.C.; Van Leeuwe, J.; Snoek, H.M. The Stice model of overeating: Tests in clinical and non-clinical samples. Appetite 2005, 45, 205–213. [Google Scholar] [CrossRef]
- Van Strien, T.; van de Laar, F.A.; van Leeuwe, J.F.J.; Lucassen, P.L.B.J.; van den Hoogen, H.J.M.; Rutten, G.E.H.M. The dieting dilemma in patients with newly diagnosed type 2 diabetes: Does dietary restraint predict weight gain 4 years after diagnosis? Health Psychol. 2007, 26, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Adriaanse, M.A.; de Ridder, D.T.; Evers, C. Emotional eating: Eating when emotional or emotional about eating? Psychol. Health 2011, 26, 23–39. [Google Scholar] [CrossRef] [PubMed]
- Ouwens, M.A.; van Strien, T.; van Leeuwe, J.F. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite 2009, 53, 245–248. [Google Scholar] [CrossRef]
- Stice, E.; Marti, C.N.; Durant, S. Risk factors for onset of eating disorders: Evidence of multiple risk pathways from an 8-year prospective study. Behav. Res. Ther. 2011, 49, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Waller, G.; Osman, S. Emotional eating and eating psychopathology among non-eating-disordered women. Int. J. Eat. Disord. 1998, 23, 419–424. [Google Scholar] [CrossRef]
- Bruce, L.; Ricciardelli, L. A systematic review of the psychosocial correlates of intuitive eating among adult women. Appetite 2016, 96, 454–472. [Google Scholar] [CrossRef]
- Richards, P.S.; Crowton, S.; Berrett, M.E.; Smith, M.H.; Passmore, K. Can patients with ED learn to eat intuitively? A 2-year pilot study. J. Treat. Prev. 2017, 25, 99–113. [Google Scholar] [CrossRef]
- Tribole, E.; Resch, E. Intuitive Eating; St. Martin’s Griffin: New York, NY, USA, 1995. [Google Scholar]
- Oswald, A.; Chapman, J.; Wilson, C. Do interoceptive awareness and interoceptive responsiveness mediate the relationship between body appreciation and intuitive eating in young women? Appetite 2017, 109, 66–72. [Google Scholar] [CrossRef]
- Resch, E.; Tylka, T.L. Intuitive eating. In Handbook of Positive Body Image and Embodiment: Constructs, Protective Factors, and Interventions; Tylka, T.L., Piran, N., Eds.; Oxford University Press: Oxford, UK, 2019; pp. 68–79. [Google Scholar]
- Tylka, T.L. Development and psychometric evaluation of a measure of intuitive eating. J. Couns. Psychol. 2006, 53, 226–240. [Google Scholar] [CrossRef]
- Avalos, L.C.; Tylka, T.L. Exploring a model of intuitive eating with college women. J. Couns. Psychol. 2006, 53, 486. [Google Scholar] [CrossRef]
- Christoph, M.; Järvelä-Reijonen, E.; Hooper, L.; Larson, N.; Mason, S.M.; Neumark-Sztainer, D. Longitudinal associations between intuitive eating and weight-related behaviours in a population-based sample of young adults. Appetite 2021, 160, 105093. [Google Scholar] [CrossRef] [PubMed]
- Hazzard, V.M.; Telke, S.E.; Simone, M.; Anderson, L.M.; Larson, N.I.; Neumark-Sztainer, D. Intuitive eating longitudinally predicts better psychological health and lower use of disordered eating behaviours: Findings from EAT 2010–2018. Eat. Weight Disord. 2021, 26, 287–294. [Google Scholar] [CrossRef]
- Linardon, J.; Tylka, T.L.; Fuller-Tyszkiewicz, M. Intuitive eating and its psychological correlates: A meta-analysis. Int. J. Eat. Disord. 2021, 54, 1073–1098. [Google Scholar] [CrossRef] [PubMed]
- Messer, M.; McClure, Z.; Lee, S.; Linardon, J. Bidirectional relationships between intuitive eating and shape and weight overvaluation, dissatisfaction, preoccupation, and fear of weight gain: A prospective study. Body Image 2021, 39, 227–231. [Google Scholar] [CrossRef]
- Monthuy-Blanc, J.; Corno, G.; Bouchard, S.; St-Pierre, M.J.; Bourbeau, F.; Mostefa-Kara, L.; Therrien, É.; Rousseau, M. Body perceptions, occupations, eating attitudes, and behaviors emerged during the pandemic: An exploratory cluster analysis of eaters profiles. Front. Psychol. 2022, 13, 949373. [Google Scholar] [CrossRef]
- Ruzanska, U.A.; Warschburger, P. Intuitive eating mediates the relationship between self-regulation and BMI-Results from a cross-sectional study in a community sample. Eat. Behav. 2019, 33, 23–29. [Google Scholar] [CrossRef]
- Tylka, T.L.; Wood-Barcalow, N.L. The body appreciation scale-2: Item refinement and psychometric evaluation. Body Image 2015, 12, 53–67. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Withnell, S.J.; Kinnear, A.; Masson, P.; Bodell, L.P. How different are threshold and other specified feeding and eating disorders? Comparing severity and treatment outcome. Front. Psychol. 2022, 13, 784512. [Google Scholar] [CrossRef]
- Fairweather-Schmidt, A.K.; Wade, T.D. DSM-5 eating disorders and other specified eating and feeding disorders: Is there a meaningful differentiation? Int. J. Eat. Disord. 2014, 47, 524–533. [Google Scholar] [CrossRef]
- Mustelin, L.; Lehtokari, V.L.; Keski-Rahkonen, A. Other specified and unspecified feeding or eating disorders among women in the community. Int. J. Eat. Disord. 2016, 49, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Tribole, E.; Resch, E. Intuitive Eating, 3rd ed.; St. Martin’s Press: New York, NY, USA, 2012. [Google Scholar]
- Marquis, M.; Talbot, A.; Sabourin, A.; Riopel, C. Exploring the environmental, personal and behavioural factors as determinants for university students’ food behaviour. Int. J. Consum. Stud. 2018, 43, 113–122. [Google Scholar] [CrossRef]
- Acosta, A.; Camilleri, M.; Abu Dayyeh, B.; Calderon, G.; Gonzalez, D.; McRae, A.; Rossini, W.; Singh, S.; Burton, D.; Clark, M.M. Selection of Antiobesity Medications Based on Phenotypes Enhances Weight Loss: A Pragmatic Trial in an Obesity Clinic. Obesity 2021, 29, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and implications for eating disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- Miskovic-Wheatley, J.; Koreshe, E.; Kim, M.; Simeone, R.; Maguire, S. The impact of the COVID-19 pandemic and associated public health response on people with eating disorder symptomatology: An Australian study. J. Eat. Disord. 2022, 10, 9. [Google Scholar] [CrossRef]
- Nisticò, V.; Bertelli, S.; Tedesco, R.; Anselmetti, S.; Priori, A.; Gambini, O.; Demartini, B. The psychological impact of COVID-19-related lockdown measures among a sample of Italian patients with eating disorders: A preliminary longitudinal study. Eat. Weight Disord. 2021, 26, 2771–2777. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, S.; Meule, A.; Favreau, M.; Voderholzer, U. Bulimia nervosa in times of the COVID-19 pandemic—Results from an online survey of former inpatients. Eur. Eat. Disord. Rev. 2020, 28, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, S.; Maier, J.; Meule, A.; Voderholzer, U. Eating disorders in times of the COVID-19 pandemic—Results from an online survey of patients with anorexia nervosa. Int. J. Eat. Disord. 2020, 53, 1791–1800. [Google Scholar] [CrossRef]
- Termorshuizen, J.D.; Watson, H.J.; Thornton, L.M.; Borg, S.; Flatt, R.E.; MacDermod, C.M.; Harper, L.E.; van Furth, E.F.; Peat, C.M.; Bulik, C.M. Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ~1000 individuals in the United States and the Netherlands. Int. J. Eat. Disord. 2020, 53, 1780–1790. [Google Scholar] [CrossRef]
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int. J. Eat. Disord. 2020, 53, 1855–1862. [Google Scholar] [CrossRef]
- Graell, M.; Morón-Nozaleda, M.G.; Camarneiro, R.; Villaseñor, Á.; Yáñez, S.; Muñoz, R.; Martínez-Núñez, B.; Miguélez-Fernández, C.; Muñoz, M.; Faya, M. Children and adolescents with eating disorders during COVID-19 confinement: Difficulties and future challenges. Eur. Eat. Disord. Rev. 2020, 28, 864–870. [Google Scholar] [CrossRef] [PubMed]
- Emmelkamp, P.M.G. Psychological consequences of COVID-19. Clin. Psychol. Psychother. 2021, 28, 1315–1316. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 Home Confinement on Eating Behaviour and Physical Activity: Results of the ECLB-COVID19 International Online Survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef]
- Choukas-Bradley, S.; Maheux, A.J.; Roberts, S.R.; Hutchinson, E.A.; Lu, C.; Ladouceur, C.D.; Silk, J.S. Picture perfect during a pandemic? Body imageconcerns and depressive symptoms in US adolescent girls during the COVID-19 lockdown. J. Child. Media 2022, 16, 481–492. [Google Scholar] [CrossRef]
- Corno, G.; Paquette, A.; Monthuy-Blanc, J.; Ouellet, M.; Bouchard, S. The relationship between Women’s negative body image and disordered eatingbehaviors during the COVID-19 pandemic: A cross-sectional study. Front. Psychol. 2022, 13, 856933. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Flaudias, V.; Iceta, S.; Zerhouni, O.; Rodgers, R.F.; Billieux, J.; Llorca, P.M.; Boudesseul, J.; de Chazeron, I.; Romo, L.; Maurage, P.; et al. COVID-19 pandemic lockdown and problematic eating behaviors in astudent population. J. Behav. Addict. 2020, 9, 826–835. [Google Scholar] [CrossRef]
- Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Saleh, S.T.; Al Daour, R.; Osaili, T.M.; Al Dhaheri, A.S. Eating habits and lifestyle during COVID-19lockdown in the United Arab Emirates: A cross-sectional study. Nutrients 2021, 12, 3314. [Google Scholar] [CrossRef]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Rossell, S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef]
- Ramalho, S.M.; Trovisqueira, A.; de Lourdes, M.; Gonçalves, S.; Ribeiro, I.; Vaz, A.R.; Machado, P.P.P.; Conceição, E. The impact of COVID-19 lockdown on disordered eating behaviors: The mediation role of psychological distress. Eat. Weight Disord. 2022, 27, 179–188. [Google Scholar] [CrossRef]
- Khan, M.A.; Smith, J.E.M. “Covibesity”, a new pandemic. Obes. Med. 2020, 19, 100282. [Google Scholar] [CrossRef] [PubMed]
- Lucibello, K.M.; Vani, M.F.; Koulanova, A.; DeJonge, M.L.; Ashdown-Franks, G.; Sabiston, C.M. #quarantine15: A content analysis of Instagram posts during COVID-19. Body Image 2021, 38, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L. Weight stigma and the “Quarantine-15”. Obesity 2020, 28, 1180–1181. [Google Scholar] [CrossRef] [PubMed]
- Monthuy-Blanc, J.; Corno, G.; Abou Chabake, S. Exploring the impact of the COVID-19 pandemic on perceptual disturbances and dysfunctional eating attitudes and behaviors: A review of the literature. Front. Psychol. 2023, 14, 1139261. [Google Scholar] [CrossRef]
- Fardouly, J.; Crosby, R.D.; Sukunesan, S. Potential benefits and limitations of machine learning in the field of eating disorders: Current research and future directions. J. Eat. Disord. 2022, 10, 66. [Google Scholar] [CrossRef]
- Haynos, A.F.; Wang, S.B.; Lipson, S.; Peterson, C.B.; Mitchell, J.E.; Halmi, K.A.; Agras, W.S.; Crow, S.J. Machine learning enhances prediction of illness course: A longitudinal study in eating disorders. Psychol. Med. 2021, 51, 1392–1402. [Google Scholar] [CrossRef]
- Ren, Y.; Lu, C.; Yang, H.; Ma, Q.; Barnhart, W.R.; Zhou, J.; Heet, J. Using machine learning to explore core risk factors associated with the risk of eating disorders among non-clinical young women in China: A decision-tree classification analysis. J. Eat. Disord. 2022, 10, 19. [Google Scholar] [CrossRef]
- Faghihi, U.; Kalantarpour, C.; Saki, A. Causal Probabilistic Based Variational Autoencoders Capable of Handling Noisy Inputs Using Fuzzy Logic Rules. In Intelligent Computing. SAI 2022. Lecture Notes in Networks and Systems; Arai, K., Ed.; Springer: Cham, Switzerland, 2022; Volume 507. [Google Scholar] [CrossRef]
- Rubin, D.B. Inference and missing data. Biometrika 1976, 63, 581–592. [Google Scholar] [CrossRef]
- Maïano, C.; Morin, A.J.; Monthuy-Blanc, J.; Garbarino, J.M.; Ninot, G. Development and validity of a very short form of the eating disorder inventory. Compr. Psychiatry 2016, 65, 141–149. [Google Scholar] [CrossRef]
- Cicchetti, D.V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994, 6, 284. [Google Scholar] [CrossRef]
- Carbonneau, E.; Carbonneau, N.; Lamarche, B.; Provencher, V.; Bégin, C.; Bradette-Laplante, M.; Laramée, C.; Lemieux, S. Validation of a French-Canadian adaptation of the intuitive eating Scale-2 for the adult population. Appetite 2016, 105, 37–45. [Google Scholar] [CrossRef]
- Tylka, T.L.; Kroon Van Diest, A.M. The intuitive eating Scale-2: Item refinement and psychometric evaluation with college women and men. J. Couns. Psychol. 2013, 60, 137–153. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Wilson, G.T.; Schleimer, K. Binge Eating: Nature, Assessment, and Treatment; Guilford Press: New York, NY, USA, 1993. [Google Scholar]
- Gouvernement du Québec. Ligne du Temps COVID-19 au Québec; Institut National de Santé Publique du Québec: Québec, QC, Canada, 2021; Available online: https://inspq.qc.ca/covid-19/donnees/ligne-du-temps (accessed on 1 October 2022).
- Sun, J.; Kabán, A.; Garibaldi, J.M. Robust mixture clustering using Pearson type VII distribution. Pattern Recognit. Lett. 2010, 31, 2447–2454. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Christopher, G.; Cooper, Z.; O’Connor, M. The eating disorder examination. Int. J. Eat. Disord. 1993, 6, 1–8. [Google Scholar]
- Fairburn, C.G. Cognitive Behavior Therapy and Eating Disorders; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Piran, N.; Neumark-Sztainer, D. Yoga and the experience of embodiment: A discussion of possible links. Eat. Disord. 2020, 28, 330–348. [Google Scholar] [CrossRef]
- Monthuy-Blanc, J.; Lemieux, V.; Thériault, J.; Rousseau, M. Exploratory study: A blind integrated school-based prevention program on eating disorders and obesity. Can. J. Commun. Ment. Health 2021, 39, 61–84. [Google Scholar] [CrossRef]
- Andrieu, B. Sentir sa santé. In Les Sensations de Santé: Pour une Épistémologie des Pratiques Corporelles du Sujet de Santé; Klein, A., Ed.; Presses Universitaires de Nancy: Nancy, France, 2011; pp. 259–282. [Google Scholar]
- Neumark-Sztainer, D.; Paxton, S.; Hannan, P.; Haines, J.; Story, M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J. Adolesc. Health 2006, 39, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Stice, E. A prospective test of the dual-pathway model of bulimic pathology: Mediating effects of dieting and negative affect. J. Abnorm. Psychol. 2001, 110, 124–135. [Google Scholar] [CrossRef]
- Lewis-Smith, H.; Diedrichs, P.C.; Halliwell, E. Cognitive-behavioral roots of body image therapy and prevention. Body Image 2019, 31, 309–320. [Google Scholar] [CrossRef]
- Lattimore, P. Mindfulness-based emotional eating awareness training: Taking the emotional out of eating. Eat. Weight Disord. 2020, 25, 649–657. [Google Scholar] [CrossRef]
- Leme, A.C.B.; Philippi, S.T. Home food availability, parents’/caregivers’ support, and family meals influence on dietary servings of low-income urban adolescent girls from Brazil. Nutrire 2017, 42, 30. [Google Scholar] [CrossRef]
- Stice, E.; Shaw, H. Eating disorder prevention programs: A meta-analytic review. Psychol. Bull. 2004, 130, 206–227. [Google Scholar] [CrossRef] [PubMed]
- Noordenbos, G. How to block the ways to eating disorders. Eat. Disord. 2016, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Monthuy-Blanc, J. Fondements Approfondis des Troubles du Comportement Alimentaire; Editions JFD: Montreal, QC, Canada, 2018. [Google Scholar]
- Ovejero, O.J.; Guzmán, P.E.; González, M.G.; Pérez, I.S.; Castro, A.B.; Escursell, R.M.R.; Giral, M.M. Universal prevention program of eating, weight and body image problems in adolescents: A 12-month follow-up. Psicothema 2020, 32, 204–213. [Google Scholar] [CrossRef]
- Garner, D.M. Eating Disorder Inventory-3. Professional Manual; Psychological Assessment Resources, Inc.: Lutz, FL, USA, 2004. [Google Scholar]
- Clausen, L.; Rosenvinge, J.H.; Friborg, O.; Rokkedal, K. Validating the Eating Disorder Inventory-3 (EDI-3): A comparison between 561 female eating disorders patients and 878 females from the general population. J. Psychopathol. Behav. Assess. 2011, 33, 101–110. [Google Scholar] [CrossRef]
- Segura-García, C.; Aloi, M.; Rania, M.; Ciambrone, P.; Palmieri, A.; Pugliese, V.; Ruiz Moruno, A.J.; De Fazio, P. Ability of EDI-2 and EDI-3 to correctly identify patients and subjects at risk for eating disorders. Eat. Behav. 2015, 19, 20–23. [Google Scholar] [CrossRef]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ 2007, 335, 194. [Google Scholar] [CrossRef]
- Chwyl, C.; Berry, M.P.; Manasse, S.M.; Forman, E.M. Rethinking emotional eating: Retrospective and momentary indices of emotional eating represent distinct constructs. Appetite 2021, 167, 105604. [Google Scholar] [CrossRef]
| Silhouette | NMI_Score | |
|---|---|---|
| Agglomerative Clustering with t-SNE | 0.175 | 0.223 * |
| Gaussian Mixture Clustering with t-SNE | 0.173 | 0.222 |
| Agglomerative Clustering with Original Dataframe | 0.197 | 0.220 |
| Gaussian Mixture Clustering with PCA | 0.120 | 0.218 |
| Agglomerative Clustering with PCA | 0.205 * | 0.214 |
| Gaussian Mixture Clustering with Original Dataframe | 0.042 | 0.205 |
| Cluster#1 | Cluster#2 | Cluster#3 | Cluster#4 | Cluster#5 | Cluster#6 | Cluster#7 | |
|---|---|---|---|---|---|---|---|
| n (%) or M ± SD | n (%) or M ± SD | n (%) or M ± SD | n (%) or M ± SD | n (%) or M ± SD | n (%) or M ± SD | n (%) or M ± SD | |
| N (%) | 44 (13.9) | 39 (12.34) | 49 (15.56) | 34 (10.7) | 47 (14.8) | 30 (9.5) | 74 (23.3) |
| Females | 42 (95.5) | 36 (92.3) | 44 (89.8) | 32 (94.1) | 42 (89.4) | 26 (86.7) | 59 (79.7) |
| Males | 2 (4.5) | 2 (5.1) | 5 (10.2) | 2 (5.9) | 4 (8.5) | 2 (6.7) | 15 (20.3) |
| Other a | / | 1 (2.6) | / | / | 1 (2.1) | 2 (6.6) | / |
| Age | 37.72 ± 14.27 | 35.68 ± 14.03 | 32.06 ± 11.48 | 41.03 ± 14.55 | 36.74 ± 15.15 | 37.57 ± 12.64 | 37.35 ± 16.52 |
| BMI | 37.97 ± 17.44 | 27.36 ± 9.52 | 26.62 ± 8.42 | 31.08 ± 8.42 | 25.68 ± 6.66 | 26.86 ± 7.23 | 25.27 ± 9.10 |
| Cluster#1 | Cluster#2 | Cluster#3 | Cluster#4 | Cluster#5 | Cluster#6 | Cluster#7 | |
|---|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | M ± SD | |
| EDI-BD | 9.2 ± 1.47 | 8.4 ± 2.06 | 5.9 ± 1.61 | 9.4 ± 1.14 | 6.1 ± 1.05 | 5.5 ± 1.17 | 2.9 ± 0.98 |
| EDI-B | 7.0 ± 1.80 | 2.5 ± 1.63 | 3.4 ± 1.05 | 1.1 ± 1.06 | 0.7 ± 0.71 | 0.4 ± 0.65 | 0.8 ± 1.00 |
| EDE-Q-R | 1.9 ± 1.69 | 4.7 ± 0.78 | 1.1 ± 1.03 | 0.8 ± 0.83 | 0.3 ± 0.36 | 2.0 ± 0.99 | 0.3 ± 0.50 |
| IES-UPE | 3.0 ± 0.88 | 2.2 ± 0.74 | 3.3 ± 0.55 | 3.3 ± 0.96 | 3.8 ± 0.68 | 3.0 ± 0.73 | 4.0 ± 0.67 |
| IES-FCC | 3.1 ± 1.06 | 3.8 ± 0.81 | 3.7 ± 0.72 | 3.8 ± 0.83 | 4.0 ± 0.63 | 4.3 ± 0.65 | 4.3 ± 0.63 |
| IES-EPR | 2.3 ± 0.55 | 3.1 ± 0.67 | 2.9 ± 0.54 | 3.2 ± 0.73 | 3.6 ± 0.58 | 3.6 ± 0.61 | 3.8 ± 0.60 |
| IES-HSC | 2.0 ± 0.72 | 2.2 ± 0.77 | 2.8 ± 0.71 | 3.1 ± 0.9 | 3.7 ± 0.78 | 3.0 ± 0.74 | 3.9 ± 0.82 |
| Cluster#1 | Cluster#2 | Cluster#3 | Cluster#6 | Cluster#4 | Cluster#5 | Cluster#7 | |
|---|---|---|---|---|---|---|---|
| EDI-BD Co: 7.48 (6.38) Cl: 15.55 (3.87) | 9.2 (1.47) >Community <Clinical | 8.4 (2.06) >Community <Clinical | 5.9 (1.61) <Community <Clinical | 5.5 (1.17) <Community <Clinical | 9.4 (1.14) >Community <Clinical | 6.1 (1.05) <Community <Clinical | 2.9 (0.98) <Community <Clinical |
| EDI-B Co: 1.94 (3.05) Cl: 4.62 (6.02) | 7.0 (1.80) >Community >Clinical | 2.5 (1.63) >Community <Clinical | 3.4 (1.05) >Community <Clinical | 0.4 (0.65) <Community <Clinical | 1.1 (1.06) <Community <Clinical | 0.7 (0.71) <Community <Clinical | 0.8 (1.00) <Community <Clinical |
| EDE-Q-R Co: 1.25 (1.32) Cl: ≥4 | 1.9 (1.69) >Community <Clinical | 4.7 (0.78) >Community >Clinical | 1.1 (1.03) <Community <Clinical | 2.0 (0.99) >Community <Clinical | 0.8 (0.83) <Community <Clinical | 0.3 (0.36) <Community <Clinical | 0.3 (0.50) <Community <Clinical |
| IES-UPE Co:3.46 (0.76)–3.70 (0.80) | 3.0 (0.88) <Community | 2.2 (0.74) <Community | 3.3 (0.55) <Community | 3.0 (0.73) <Community | 3.3 (0.96) <Community | 3.8 (0.68) >Community | 4.0 (0.67) >Community |
| IES-FCC Co: 3.29 (0.80)–3.48 (0.77) | 3.1 (1.06) <Community | 3.8 (0.81) >Community | 3.7 (0.72) >Community | 4.3 (0.65) >Community | 3.8 (0.83) >Community | 4.0 (0.63) >Community | 4.3 (0.63) >Community |
| IES-EPR Co: 3.17 (0.90)–3.77 (0.85) | 2.3 (0.55) <Community | 3.1 (0.67) <Community | 2.9 (0.54) <Community | 3.6 (0.61) =Community | 3.2 (0.73) =Community | 3.6 (0.58) =Community | 3.8 (0.60) =Community |
| IES-HSC Co: 3.52 (0.70)–3.72 (0.71) | 2.0 (0.72) <Community | 2.2 (0.77) <Community | 2.8 (0.71) <Community | 3.0 (0.74) <Community | 3.1 (0.9) <Community | 3.7 (0.78) =Community | 3.9 (0.82) >Community |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monthuy-Blanc, J.; Faghihi, U.; Fardshad, M.N.G.; Corno, G.; Iceta, S.; St-Pierre, M.-J.; Bouchard, S. When Eating Intuitively Is Not Always a Positive Response: Using Machine Learning to Better Unravel Eaters Profiles. J. Clin. Med. 2023, 12, 5172. https://doi.org/10.3390/jcm12165172
Monthuy-Blanc J, Faghihi U, Fardshad MNG, Corno G, Iceta S, St-Pierre M-J, Bouchard S. When Eating Intuitively Is Not Always a Positive Response: Using Machine Learning to Better Unravel Eaters Profiles. Journal of Clinical Medicine. 2023; 12(16):5172. https://doi.org/10.3390/jcm12165172
Chicago/Turabian StyleMonthuy-Blanc, Johana, Usef Faghihi, Mahan Najafpour Ghazvini Fardshad, Giulia Corno, Sylvain Iceta, Marie-Josée St-Pierre, and Stéphane Bouchard. 2023. "When Eating Intuitively Is Not Always a Positive Response: Using Machine Learning to Better Unravel Eaters Profiles" Journal of Clinical Medicine 12, no. 16: 5172. https://doi.org/10.3390/jcm12165172






