Efficacy of Cardiopulmonary Resuscitation Using Automatic Compression—Defibrillation Apparatus: An Animal Study and A Manikin-Based Simulation Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Automated Compression–Defibrillation Apparatus
2.2. Study Design
2.3. Animal Experiments
2.3.1. Animal Preparation
2.3.2. Randomization and Experimental Protocol
2.3.3. Measurements and Outcomes
2.4. Simulation Study
2.4.1. Participants and Simulation Scenario
2.4.2. Measurements
2.5. Sample Size
2.5.1. Animal Experiment
2.5.2. Simulation Study
2.6. Statistical Analysis
2.7. Statement of Ethical Approval
3. Results
3.1. Results of the Animal Experiments
3.1.1. Comparison of Hemodynamic Effects and Quality of CPR
3.1.2. Comparison of Time Variables
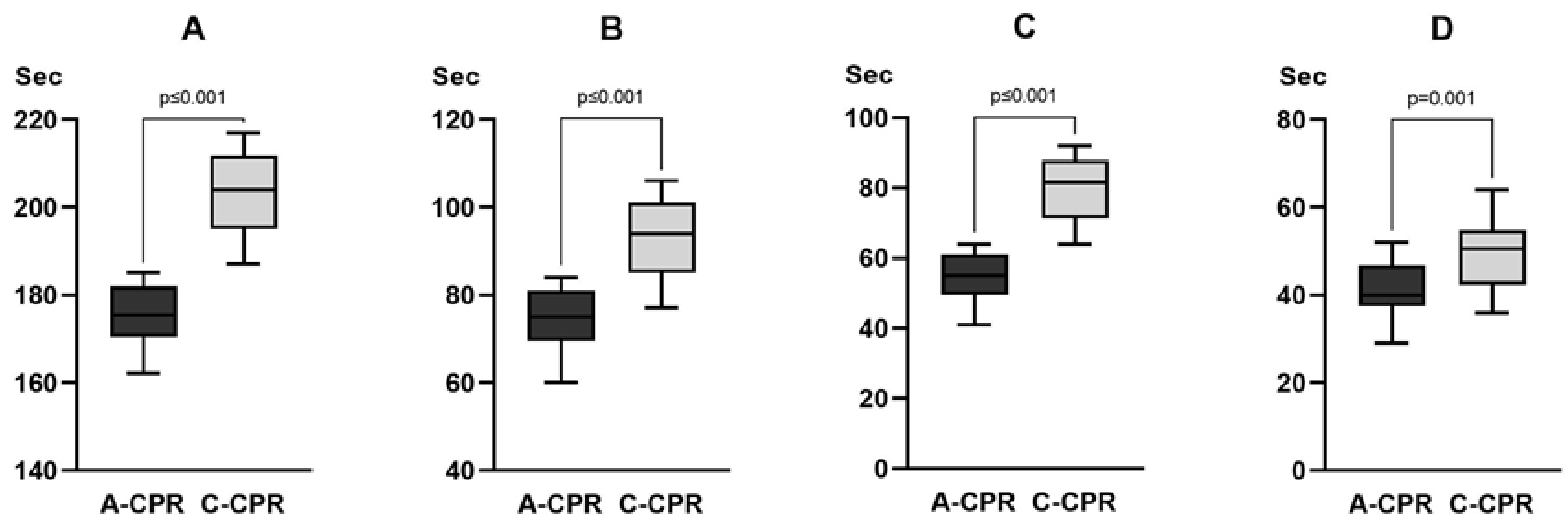
3.2. Results of the Simulation Study
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blom, M.T.; Beesems, S.G.; Homma, P.C.; Zijlstra, J.A.; Hulleman, M.; van Hoeijen, D.A.; Bardai, A.; Tijssen, J.G.; Tan, H.L.; Koster, R.W. Improved survival after out-of-hospital cardiac arrest and use of automated external defibrillators. Circulation 2014, 130, 1868–1875. [Google Scholar] [CrossRef] [PubMed]
- Pijls, R.W.; Nelemans, P.J.; Rahel, B.M.; Gorgels, A.P. A text message alert system for trained volunteers improves out-of-hospital cardiac arrest survival. Resuscitation 2016, 105, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Wissenberg, M.; Lippert, F.K.; Folke, F.; Weeke, P.; Hansen, C.M.; Christensen, E.F.; Jans, H.; Hansen, P.A.; Lang-Jensen, T.; Olesen, J.B.; et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA 2013, 310, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Hasselqvist-Ax, I.; Riva, G.; Herlitz, J.; Rosenqvist, M.; Hollenberg, J.; Nordberg, P.; Ringh, M.; Jonsson, M.; Axelsson, C.; Lindqvist, J.; et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N. Engl. J. Med. 2015, 372, 2307–2315. [Google Scholar] [CrossRef]
- Harve, H.; Jokela, J.; Tissari, A.; Saukko, A.; Räsänen, P.; Okkolin, T.; Pettilä, V.; Silfvast, T. Can untrained laypersons use a defibrillator with dispatcher assistance? Acad. Emerg. Med. 2007, 14, 624–628. [Google Scholar] [CrossRef]
- Asai, H.; Fukushima, H.; Bolstad, F.; Okuchi, K. Quality of dispatch-assisted cardiopulmonary resuscitation by lay rescuers following a standard protocol in Japan: An observational simulation study. Acute Med. Surg. 2018, 5, 133–139. [Google Scholar] [CrossRef]
- Hanisch, J.R.; Counts, C.R.; Latimer, A.J.; Rea, T.D.; Yin, L.; Sayre, M.R. Causes of chest compression interruptions during out-of-hospital cardiac arrest resuscitation. J. Am. Heart Assoc. 2020, 9, e015599. [Google Scholar] [CrossRef]
- Shbaklo, N.; Lupia, T.; De Rosa, F.G.; Corcione, S. Infection control in the era of COVID-19: A narrative review. Antibiotics 2021, 10, 1244. [Google Scholar] [CrossRef]
- Kramer, D.B.; Lo, B.; Dickert, N.W. CPR in the Covid-19 rra—An ethical framework. N. Engl. J. Med. 2020, 383, e6. [Google Scholar] [CrossRef]
- Fragkou, P.C.; Dimopoulou, D.; Latsios, G.; Koudounis, P.; Synetos, A.; Dimopoulou, A.; Tsioufis, K.; Papaevangelou, V.; Tsiodras, S. Transmission of infections during cardiopulmonary resuscitation. Clin. Microbiol. Rev. 2021, 34, e0001821. [Google Scholar] [CrossRef]
- Chan-Yeung, M. Severe acute respiratory syndrome (SARS) and healthcare workers. Int. J. Occup. Environ. Health 2004, 10, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Edelson, D.P.; Sasson, C.; Chan, P.S.; Atkins, D.L.; Aziz, K.; Becker, L.B.; Berg, R.A.; Bradley, S.M.; Brooks, S.C.; Cheng, A.; et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: From the Emergency Cardiovascular Care Committee and Get with The Guidelines-Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation 2020, 141, e933–e943. [Google Scholar] [CrossRef]
- Secrest, K.M.; Anderson, T.M.; Trumpower, B.; Harrod, M.; Krein, S.L.; Guetterman, T.C.; Chan, P.S.; Nallamothu, B.K. Early changes in hospital resuscitation practices during the COVID-19 pandemic. Resusc. Plus 2022, 12, 100317. [Google Scholar] [CrossRef]
- Ahn, J.Y.; Ryoo, H.W.; Cho, J.W.; Kim, J.H.; Lee, S.H.; Jang, T.C. Impact of the COVID-19 outbreak on adult out-of-hospital cardiac arrest outcomes in Daegu, South Korea: An observational study. Clin. Exp. Emerg. Med. 2021, 8, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Lee, S.H.; Lim, H.J.; Hong, W.P. Impact of COVID-19 on out-of-hospital cardiac arrest in Korea. J. Korean Med. Sci. 2023, 38, e92. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.; Cha, K.C.; Lee, J.H.; Park, S.; Kim, D.H.; Lee, B.K.; Park, J.S.; Jung, W.J.; Lee, D.K.; Roh, Y.I.; et al. 2020 Korean Guidelines for Cardiopulmonary Resuscitation. Part 4. Adult advanced life support. Clin. Exp. Emerg. Med. 2021, 8, S26–S40. [Google Scholar] [CrossRef] [PubMed]
- Roh, Y.I.; Jung, W.J.; Im, H.Y.; Lee, Y.; Im, D.; Cha, K.C.; Hwang, S.O. Development of an automatic device performing chest compression and external defibrillation: An animal-based pilot study. PLoS ONE 2023, 18, e0288688. [Google Scholar] [CrossRef]
- Hwang, S.O.; Lee, K.H.; Lee, J.W.; Lee, S.Y.; Yoo, B.S.; Yoon, J.; Choe, K.H. Simultaneous sterno-thoracic cardiopulmonary resuscitation improves short-term survival rate in canine cardiac arrests. Resuscitation 2002, 53, 209–216. [Google Scholar] [CrossRef]
- Cunningham, L.M.; Mattu, A.; O’Connor, R.E.; Brady, W.J. Cardiopulmonary resuscitation for cardiac arrest: The importance of uninterrupted chest compressions in cardiac arrest resuscitation. Am. J. Emerg. Med. 2012, 30, 1630–1638. [Google Scholar] [CrossRef]
- Van Alem, A.P.; Sanou, B.T.; Koster, R.W. Interruption of cardiopulmonary resuscitation with the use of the automated external defibrillator in out-of-hospital cardiac arrest. Ann. Emerg. Med. 2003, 42, 449–457. [Google Scholar] [CrossRef]
- Berg, R.A.; Sanders, A.B.; Kern, K.B.; Hilwig, R.W.; Heidenreich, J.W.; Porter, M.E.; Ewy, G.A. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 2001, 104, 2465–2470. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, T.F.; Walker, R.G.; Chapman, F.W.; Koster, R.W. Association between chest compression interruptions and clinical outcomes of ventricular fibrillation out-of-hospital cardiac arrest. Circulation 2015, 132, 1030–1037. [Google Scholar] [CrossRef] [PubMed]
- Sugerman, N.T.; Edelson, D.P.; Leary, M.; Weidman, E.K.; Herzberg, D.L.; Vanden Hoek, T.L.; Becker, L.B.; Abella, B.S. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: A prospective multicenter study. Resuscitation 2009, 80, 981–984. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | A-CPR (n = 12) | C-CPR (n = 12) | p-Value |
|---|---|---|---|
| Male, n (%) | 10 (83.3) | 7 (58.3) | 0.178 |
| Body weight (kg) | 36.5 (36–37.75) | 38.0 (36.25–39.50) | 0.167 |
| Systolic blood pressure (mmHg) | 105 (94–118) | 97 (92–106) | 0.128 |
| Diastolic blood pressure (mmHg) | 69 (60–78) | 67 (57–72) | 0.185 |
| Mean aortic pressure (mmHg) | 82 (70–92) | 77 (68–83) | 0.154 |
| Mean right atrial pressure (mmHg) | 2.2 (1.0–3.5) | 4.2 (3.1–5.4) | 0.039 |
| CPP (mmHg) | 86 (68–95) | 80 (60–86) | 0.396 |
| CBF (mL/min) | 206 (165–264) | 186 (149–232) | 0.382 |
| ETCO2 (mmHg) | 49 (46–53) | 49 (44–50) | 0.248 |
| pH | 7.473 (7.439–7.498) | 7.493 (7.462–7.533) | 0.141 |
| PaCO2 (mmHg) | 35 (28–41) | 31 (29–37) | 0.488 |
| PaO2 (mmHg) | 111 (100–134) | 118 (96–141) | 0.954 |
| Bicarbonate (mmol/L) | 27.8 (20.2–29.4) | 25.4 (22.2–29.9) | 0.885 |
| SaO2 (%) | 99 (98–99) | 99 (98–99) | 0.570 |
| Lactate (mg/dl) | 1.3 (1.0–2.5) | 0.3 (0.7–1.5) | 0.106 |
| Hemodynamic Parameters | Elapsed Time after CPR | 2 min | 4 min | 8 min | 12 min | 16 min | 20 min | p-Value |
|---|---|---|---|---|---|---|---|---|
| Aortic pressure, compression (mmHg) | A-CPR | 94 (89–101) | 92 (14–105) | 91 (68–103) | 131 (85–161) | 102 (78–133) | 71 (35–106) | 0.186 |
| C-CPR | 86 (81–105) | 96 (76–102) | 99 (90–107) | 107 (105–122) | 166 (104–276) | 104 (75–134) | ||
| Aortic pressure, relaxation (mmHg) | A-CPR | 27 (22–32) | 18 (15–22) | 18 (13–22) | 35 (32–41) | 30 (17–33) | 24 (3–45) | 0.256 |
| C-CPR | 14 (11–21) | 16 (9–21) | 20 (13–26) | 34 (16–42) | 64 (26–126) | 26 (24–28) | ||
| Mean aortic pressure (mmHg) | A-CPR | 47 (46–50) | 42 (39–48) | 42 (39–48) | 67 (56–75) | 54 (38–66) | 39 (14–65) | 0.168 |
| C-CPR | 52 (36–52) | 45 (37–49) | 46 (41–50) | 59 (48–65) | 98 (52–176) | 52 (41–63) | ||
| Right atrial pressure, compression (mmHg) | A-CPR | 113 (76–149) | 155 (55–254) | 159 (119–198) | 131 (95–167) | 113 (77–149) | 121 (87–155) | 0.023 |
| C-CPR | 160 (115–206) | 139 (114–163) | 128 (119–138) | 106 (91–121) | 90 (73–106) | 65 (24–105) | ||
| Right atrial pressure, relaxation (mmHg) | A-CPR | 4 (3–4) | 5 (5–6) | 6 (5–7) | 6 (6–6) | 8 (8–8) | 7 (6–7) | 0.099 |
| C-CPR | 4 (3–5) | 3 (3–3) | 3 (2–4) | 5 (4–5) | 5 (3–6) | 4 (2–5) | ||
| CPP (mmHg) | A-CPR | 43 (36–49) | 35 (26–47) | 34 (28–45) | 45 (36–78) | 45 (32–55) | 34 (11–56) | 0.385 |
| C-CPR | 13 (5–17) | 14 (6–19) | 17 (5–22) | 35 (21–39) | 72 (21–132) | 48 (37–59) | ||
| CBF (mL/min) | A-CPR | 298 (226–360) | 318 (240–390) | 293 (230–351) | 215 (175–266) | 252 (185–292) | 253 (113–393) | 0.768 |
| C-CPR | 361 (258–407) | 357 (329–434) | 381 (295–398) | 194 (113–239) | 149 (94–247) | 78 (65–90) | ||
| ETCO2 (mmHg) | A-CPR | 30 (26–31) | 20 (17–29) | 25 (23–34) | 34 (30–44) | 33 (30–35) | 33 (24–41) | 0.591 |
| C-CPR | 24 (22–28) | 21 (18–27) | 25 (22–41) | 28 (24–37) | 37 (28–47) | 26 (24–29) |
| Outcomes | A-CPR (n = 12) | C-CPR (n = 12) | p-Value |
|---|---|---|---|
| Total number of defibrillations | 2.5 (1.0–5.3) | 3 (1.0–4.8) | 0.893 |
| CCF (%) | 93.4 (90.4–97.4) | 91.5 (87.2–96.8) | 0.322 |
| ROSC | 11 (91.7%) | 12 (100%) | 0.262 |
| 2 h survival | 11 (91.7%) | 12 (100%) | 0.262 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, W.J.; Roh, Y.-I.; Im, H.; Lee, Y.; Im, D.; Cha, K.-C.; Hwang, S.O. Efficacy of Cardiopulmonary Resuscitation Using Automatic Compression—Defibrillation Apparatus: An Animal Study and A Manikin-Based Simulation Study. J. Clin. Med. 2023, 12, 5333. https://doi.org/10.3390/jcm12165333
Jung WJ, Roh Y-I, Im H, Lee Y, Im D, Cha K-C, Hwang SO. Efficacy of Cardiopulmonary Resuscitation Using Automatic Compression—Defibrillation Apparatus: An Animal Study and A Manikin-Based Simulation Study. Journal of Clinical Medicine. 2023; 12(16):5333. https://doi.org/10.3390/jcm12165333
Chicago/Turabian StyleJung, Woo Jin, Young-Il Roh, Hyeonyoung Im, Yujin Lee, Dahye Im, Kyoung-Chul Cha, and Sung Oh Hwang. 2023. "Efficacy of Cardiopulmonary Resuscitation Using Automatic Compression—Defibrillation Apparatus: An Animal Study and A Manikin-Based Simulation Study" Journal of Clinical Medicine 12, no. 16: 5333. https://doi.org/10.3390/jcm12165333
APA StyleJung, W. J., Roh, Y.-I., Im, H., Lee, Y., Im, D., Cha, K.-C., & Hwang, S. O. (2023). Efficacy of Cardiopulmonary Resuscitation Using Automatic Compression—Defibrillation Apparatus: An Animal Study and A Manikin-Based Simulation Study. Journal of Clinical Medicine, 12(16), 5333. https://doi.org/10.3390/jcm12165333





