SuperPATH—Current Status of Evidence and Further Investigations: A Scoping Review and Quality Assessment
Abstract
1. Introduction
2. Materials and Methods
2.1. Scoping Review
2.2. Search Strategy
2.3. Data Extraction and Quality Assessment
3. Results
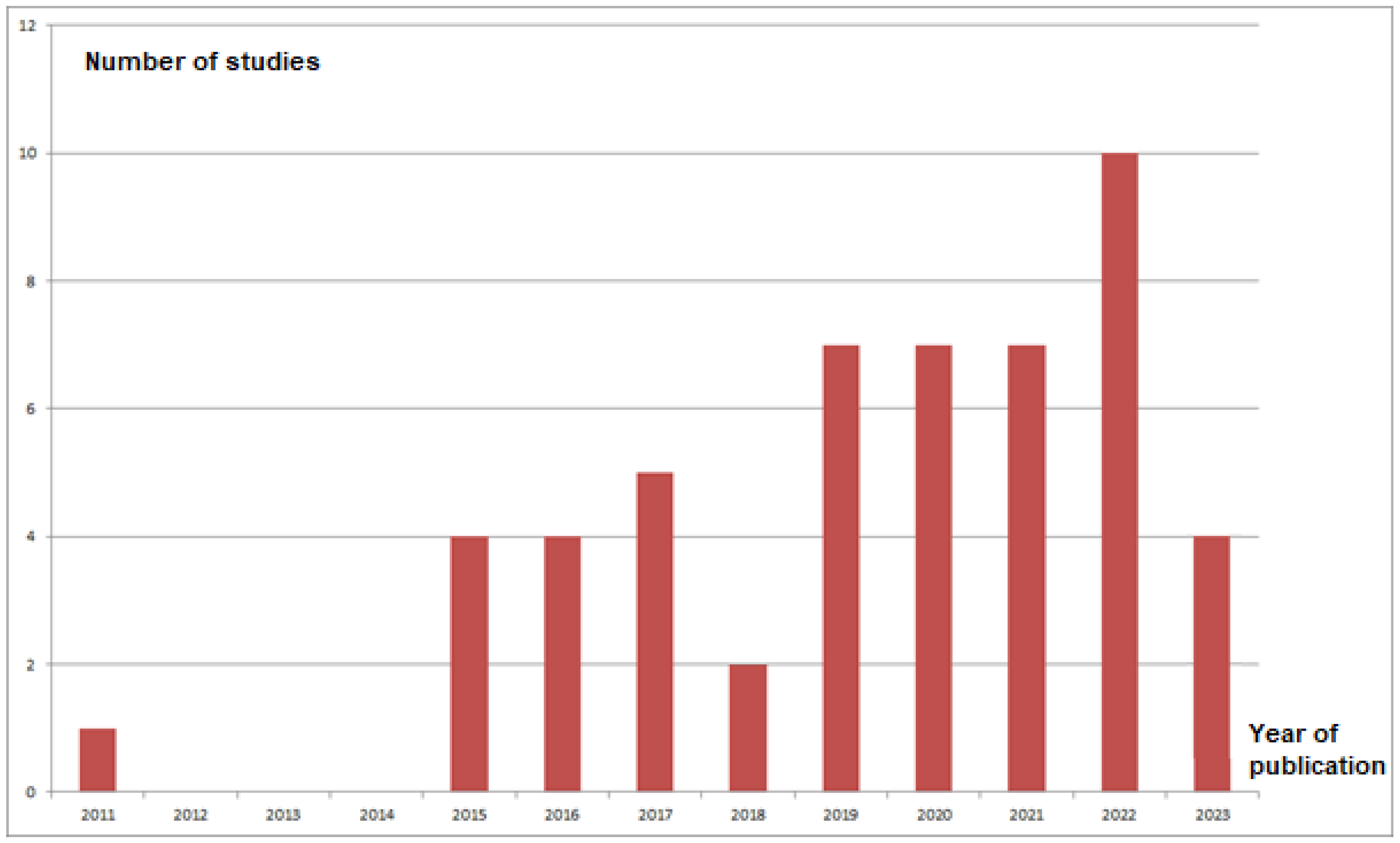
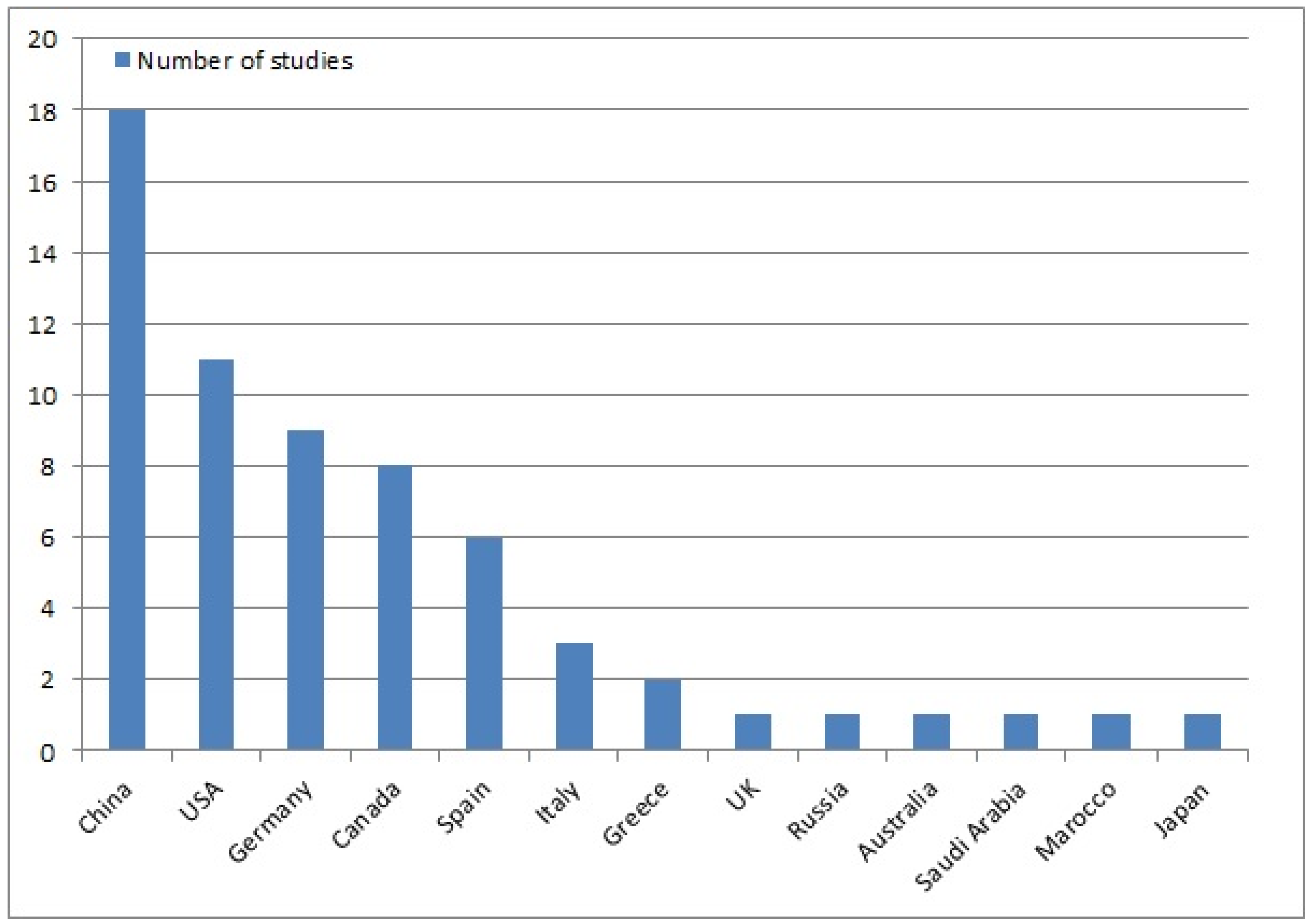
3.1. Search Results
3.2. Meta-Analyses on SuperPATH
3.3. RCTs on SuperPATH
3.4. Prospective Non-RCTs on SuperPATH
3.5. Quality Assessment
4. Discussion
- -
- RCTs and meta-analyses of SuperPATH vs. each CA separately (ALA, LA, PA, PLA);
- -
- RCTs and meta-analyses of SuperPATH vs. DAA in direct comparison;
- -
- RCTs and meta-analyses of SuperPATH vs. other MI techniques (except of DAA) or vs. robotic-assisted techniques;
- -
- Meta-analyses of the laboratory parameters of SuperPATH vs. other techniques;
- -
- RCTs and meta-analyses of SuperPATH HA;
- -
- RCTs and meta-analyses of the stem positioning through SuperPATH;
- -
- RCT and meta-analyses of revision THA through SuperPATH;
- -
- RCTs and meta-analyses of mid- and long-term outcomes of SuperPATH.
- -
- Standardization of terminology: SuperPATH is the designation of a hip replacement technique that uses a direct superior approach (DSA);
- -
- Report the use of bone cement;
- -
- Report information on the additional stab incision:
- -
- Do you report an added incision length of both incisions (additional stab incision + main incision) in SuperPATH THA or just the main incision?
- -
- Did you omit the additional stab incision in SuperPATH HA?
5. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ALMI | anterolateral minimally invasive |
| ALA | anterolateral approach |
| AMIS | anterior minimally invasive surgery |
| AMSTAR | A MeaSurement Tool to Assess Systematic Reviews |
| ANFH | avascular necrosis of the femoral head |
| CA | conventional approach |
| CNKI | China National Knowledge Infrastructure |
| DAA | direct anterior approach |
| DSA | direct superior approach |
| FNF | femoral neck fracture |
| HA | hemiarthroplasty |
| HHS | Harris Hip Score |
| HOOS | Hip disability and osteoarthritis outcome score |
| LA | lateral approach |
| MI | minimally invasive |
| OA | osteoarthritis |
| OHS | Oxford Hip Score |
| PA | posterior approach |
| PATH | Percutaneously assisted total hip |
| PLA | posterolateral approach |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| RCT | randomized controlled trial |
| ROM | range of motion |
| RoB | risk of bias |
| ROBINS-I | risk of bias in non-randomized studies of interventions |
| SF-36 | Short Form 36 |
| SuperCap | Supercapsular approach |
| SuperPATH | Supercapsular percutaneously assisted approach in total hip |
| THA | total hip arthroplasty |
| VAS | visual analog scale |
| WOMAC | Western Ontario and MacMaster Universities Osteoarthritis Index |
References
- Varacallo, M.A.; Herzog, L.; Toossi, N.; Johanson, N.A. Ten-Year Trends and Independent Risk Factors for Unplanned Readmission Following Elective Total Joint Arthroplasty at a Large Urban Academic Hospital. J. Arthroplast. 2017, 32, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Sendtner, E.; Renkawitz, T.; Kramny, P.; Wenzl, M.; Grifka, J. Fractured neck of femur--internal fixation versus arthroplasty. Dtsch. Arztebl. Int. 2010, 107, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Galakatos, G.R. Direct Anterior Total Hip Arthroplasty. Mol. Med. 2018, 115, 537–541. [Google Scholar]
- Walde, T.A.; Blattgerste, D.; Sehmisch, S.; Kuttler, W.; Walde, H.-J.; Köster, G. Early results and patient satisfaction after total hip arthroplasty using a minimally invasive anterolateral approach. Hip Int. 2009, 19, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Chow, J.; Penenberg, B.; Murphy, S. Modified micro-superior percutaneously-assisted total hip: Early experiences & case reports. Curr. Rev. Musculoskelet. Med. 2011, 4, 146–150. [Google Scholar] [CrossRef]
- Murphy, S.B. Tissue-preserving, minimally invasive total hip arthroplasty using a superior capsulotomy. In Minimally Invasive Total Hip and Knee Arthroplasty; Hozack, W., Ed.; Springer: Berlin/Heidelberg, Germany, 2004; pp. 101–107. [Google Scholar]
- Penenberg, B.L.; Bolling, W.S.; Riley, M. Perkutan assistierte Hüftendoprothetik (PATH): Ein vorläufiger Bericht. J. Bone Jt. Surg. Am. 2008, 90, 209–220. [Google Scholar] [CrossRef]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Belinky, F.; Nativ, N.; Stelzer, G.; Zimmerman, S.; Stein, T.I.; Safran, M.; Lancet, D. PathCards: Multi-source consolidation of human biological pathways. Database 2015, 2015, bav006. [Google Scholar] [CrossRef] [PubMed]
- Pevzner, P.A.; Tang, H. Fragment assembly with double-barreled data. Bioinformatics 2001, 17, S225–S233. [Google Scholar] [CrossRef]
- Xu, B.; Gao, J.; Li, C. An efficient algorithm for DNA fragment assembly in MapReduce. Biochem. Biophys Res. Commun. 2012, 426, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Hamzeh, O.; Alkhateeb, A.; Zheng, J.; Kandalam, S.; Rueda, L. Prediction of tumor location in prostate cancer tissue using a machine learning system on gene expression data. BMC Bioinform. 2020, 21, 78. [Google Scholar] [CrossRef]
- Ramadanov, N.; Bueschges, S.; Liu, K.; Klein, R.; Schultka, R. Comparison of short-term outcomes between SuperPATH approach and conventional approaches in hip replacement: A systematic review and meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2020, 15, 420. [Google Scholar] [CrossRef]
- Ramadanov, N.; Bueschges, S.; Liu, K.; Lazaru, P.; Marintschev, I. Comparison of short-term outcomes between direct anterior approach (DAA) and SuperPATH in total hip replacement: A systematic review and network meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2021, 16, 324. [Google Scholar] [CrossRef]
- Ge, Y.; Chen, Z.; Chen, Q.; Fu, Y.; Fan, M.; Li, T.; Shan, L.; Tong, P.; Zhou, L. A Systematic Review and Meta-Analysis of the SuperPATH Approach in Hip Arthroplasty. Biomed. Res. Int. 2021, 2021, 5056291. [Google Scholar] [CrossRef]
- Ramadanov, N.; Bueschges, S.; Liu, K.; Lazaru, P.; Marintschev, I. Direct anterior approach vs. SuperPATH vs. conventional approaches in total hip replacement: A network meta-analysis of randomized controlled trials. Orthop. Traumatol. Surg. Res. 2021, 107, 103058. [Google Scholar] [CrossRef]
- Zhao, F.; Xue, Y.; Wang, X.; Zhan, Y. Efficacy of Supercapsular Percutaneously-Assisted Total Hip Arthroplasty in the Elderly With Femoral Neck Fractures: A Meta-analysis. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221074176. [Google Scholar] [CrossRef] [PubMed]
- Ramadanov, N. An Updated Meta-Analysis of Randomized Controlled Trials on Total Hip Arthroplasty through SuperPATH versus Conventional Approaches. Orthop. Surg. 2022, 14, 807–823. [Google Scholar] [CrossRef] [PubMed]
- Joseph, V.M.; Nagy, M.; Board, T.N. Systematic review and meta-analysis on SuperPATH approach versus conventional approaches for hip arthroplasty. Hip Int. 2022, 33, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Ramadanov, N.; Bueschges, S.; Liu, K.; Lazaru, P.; Marintschev, I. Direct and indirect comparisons in network meta-analysis of SuperPATH, direct anterior and posterior approaches in total hip arthroplasty. Sci. Rep. 2022, 12, 16778. [Google Scholar] [CrossRef] [PubMed]
- Yan, L.; Ge, L.; Dong, S.; Saluja, K.; Li, D.; Reddy, K.S.; Wang, Q.; Yao, L.; Li, J.J.; da Costa, B.R.; et al. Evaluation of Comparative Efficacy and Safety of Surgical Approaches for Total Hip Arthroplasty: A Systematic Review and Network Meta-analysis. JAMA Netw. Open 2023, 6, e2253942. [Google Scholar] [CrossRef]
- Yan, T.; Tian, S.; Wang, Y.; Yang, X.; Li, T.; Liu, J.; Pan, P.; Wang, R.; Wang, D.; Sun, K. Comparison of early effectiveness between SuperPATH approach and Hardinge approach in total hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2017, 31, 17–24. (In Chinese) [Google Scholar] [CrossRef]
- Xie, J.; Zhang, H.; Wang, L.; Yao, X.; Pan, Z.; Jiang, Q. Comparison of supercapsular percutaneously assisted approach total hip versus conventional posterior approach for total hip arthroplasty: A prospective, randomized controlled trial. J. Orthop. Surg. Res. 2017, 12, 138. [Google Scholar] [CrossRef]
- Yuan, H.; Zhu, J.; Sun, Z.; Zhang, Z. Comparison of effectiveness between SuperPATH approach and posterolateral approach in total hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2018, 32, 14–19. (In Chinese) [Google Scholar] [CrossRef]
- Ouyang, C.; Wang, H.; Meng, W.; Luo, Z.; Wang, D.; Pei, F.; Zhou, Z. Randomized controlled trial of comparison between the SuperPATH and posterolateral approaches in total hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2018, 32, 1500–1506. (In Chinese) [Google Scholar] [CrossRef]
- Jia, J.; Ji, Y.; Liu, X.; Wu, L.; Yu, B.; Ao, R. Hip hemiarthroplasty for senile femoral neck fractures: Minimally invasive SuperPath approach versus traditional posterior approach. Injury 2019, 50, 1452–1459. [Google Scholar] [CrossRef]
- Meng, W.; Huang, Z.; Wang, H.; Wang, D.; Luo, Z.; Bai, Y.; Gao, L.; Wang, G.; Zhou, Z. Supercapsular percutaneously-assisted total hip (SuperPath) versus posterolateral total hip arthroplasty in bilateral osteonecrosis of the femoral head: A pilot clinical trial. BMC Musculoskelet. Disord. 2019, 21, 2. [Google Scholar] [CrossRef]
- Meng, W.; Gao, L.; Huang, Z.; Wang, H.; Wang, D.; Luo, Z.; Bai, Y.; Wang, G.; Zhou, Z. Supercapsular percutaneously-assisted total hip (SuperPath) versus mini-incision posterolateral total hip arthroplasty for hip osteoarthritis: A prospective randomized controlled trial. Ann. Transl. Med. 2021, 9, 392. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Ma, L.; Wang, Q.; Rong, K. Comparison of total hip arthroplasty with minimally invasive SuperPath approach vs. conventional posterolateral approach in elderly patients: A one-year follow-up randomized controlled research. Asian J. Surg. 2020, 44, 531–536. [Google Scholar] [CrossRef] [PubMed]
- Khoja, Y.T.M.; Habis, A.A.M.; Wood, G.C.A.M. The Supercapsular Percutaneously Assisted Total Hip Approach Does Not Provide Any Clinical Advantage Over the Conventional Posterior Approach for THA in a Randomized Clinical Trial. Clin. Orthop. Relat. Res. 2022, 481, 1116–1125. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Ji, W.; Shen, Y.; He, S.; Lin, Y.; Ye, Z.; Wang, B. Comparison of the early clinical efficacy of the SuperPath approach versus the modified Hardinge approach in total hip arthroplasty for femoral neck fractures in elderly patients: A randomized controlled trial. J. Orthop. Surg. Res. 2023, 18, 215. [Google Scholar] [CrossRef]
- Korytkin, A.A.; El Moudni, Y.M.; Novikova, Y.S.; Kovaldov, K.A.; Morozova, E.A. A prospective randomised comparison of earlier function after total hip arthroplasty with a mini posterior approach or supercapsular percutaneously-assisted total hip approach: A gait analysis study. Hip Int. 2023, 33, 169–177. [Google Scholar] [CrossRef]
- Qurashi, S.; Chinnappa, J.; Lord, S.J.; Nazha, A.; Gordon, J.; Chow, J. Driving After Microinvasive Total Hip Arthroplasty. J. Arthroplast. 2017, 32, 1525–1529. [Google Scholar] [CrossRef]
- Martínez, J.M.; Sanz-Reig, J.; Morales-Santías, M.; de Puga, D.B.S.; Roman, C.V.; Gimenez, E.M. Comparative cohort study of the SuperPath approach and the conventional posterior approach in primary cementless hip replacement surgery. Rev. Esp. Cir. Ortop. Traumatol. Engl. Ed. 2019, 63, 346–354, (In English, In Spanish). [Google Scholar] [CrossRef]
- Wang, X.; Lan, H.; Hu, Z.; Li, K.; Wang, Z.; Luo, J.; Long, X. SuperPATH Minimally Invasive Approach to Total Hip Arthroplasty of Femoral Neck Fractures in the Elderly: Preliminary Clinical Results. Orthop. Surg. 2019, 12, 74–85. [Google Scholar] [CrossRef]
- Tottas, S.; Tsigalou, C.; Ververidis, A.; Kougioumtzis, I.E.; Karaglani, M.; Tilkeridis, K.; Chatzipapas, C.; Drosos, G.I. Supercapsular Percutaneously Assisted total hip arthroplasty versus lateral approach in Total Hip Replacement. A prospective comparative study. J. Orthop. 2020, 21, 406–415. [Google Scholar] [CrossRef]
- Rasuli, K.J.; Gofton, W. Percutaneously assisted total hip (PATH) and Supercapsular percutaneously assisted total hip (SuperPATH) arthroplasty: Learning curves and early outcomes. Ann. Transl. Med. 2015, 3, 179. [Google Scholar] [CrossRef] [PubMed]
- Gofton, W.; Fitch, D.A. In-hospital cost comparison between the standard lateral and supercapsular percutaneously-assisted total hip surgical techniques for total hip replacement. Int. Orthop. 2016, 40, 481–485. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chow, J.; Fitch, D.A. In-hospital costs for total hip replacement performed using the supercapsular percutaneously-assisted total hip replacement surgical technique. Int. Orthop. 2017, 41, 1119–1123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Xu, K.; Anwaier, D.; He, R.; Zhang, X.; Qin, S.; Wang, G.; Duan, X.; Tong, D.; Ji, F. Hidden blood loss after hip hemiarthroplasty using the superPATH approach: A retrospective study. Injury 2019, 50, 2282–2286. [Google Scholar] [CrossRef] [PubMed]
- LeRoy, T.E.; Hayden, B.L.; Desmarais, J.; Menendez, M.E.; Ward, D. Early Outcome Comparison of the Posterior Approach and the Superior Approach for Primary Total Hip Arthroplasty. Arthroplast. Today 2020, 6, 508–512. [Google Scholar] [CrossRef] [PubMed]
- Lei, P.; Liao, Z.; Peng, J.; Li, G.; Zhou, Q.; Xiao, X.; Yang, C. Assessment of the Learning Curve of Supercapsular Percutaneously Assisted Total Hip Arthroplasty in an Asian Population. Biomed. Res. Int. 2020, 2020, 5180458. [Google Scholar] [CrossRef]
- Jiang, H.; Wang, L.H.; Jin, Y.X.; Liu, Z.M.; Xu, L.F.; Chen, X.Y. Supercapsular percutaneously assisted total hip arthroplasty versus conventional posterior approach: Comparison of early functional results. Acta Orthop. Traumatol. Turc. 2020, 54, 511–515. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, M.-C.; Wang, T.; Meng, Y.; Chao, X.-M.; Zhu, H.-F.; Li, C.-G.; Pan, C.-L.; He, H.-B. Less blood loss in supercapsular percutaneously assisted versus posterolateral total hip arthroplasty. J. Orthop. Surg. Res. 2021, 16, 217. [Google Scholar] [CrossRef]
- Di Maro, A.; Creaco, S.; Albini, M.; Latiff, M.; Merlo, M. Radiographic results on acetabular cup placement with the SuperPath technique: A retrospective study of 756 cases. BMC Musculoskelet. Disord. 2022, 23, 101. [Google Scholar] [CrossRef]
- McGoldrick, N.P.; Antoniades, S.; El Meniawy, S.; Kreviazuk, C.; Beaulé, P.E.; Grammatopoulos, G. Supine versus lateral position for total hip replacement: Accuracy of biomechanical reconstruction. Arch. Orthop. Trauma Surg. 2022, 142, 2945–2955. [Google Scholar] [CrossRef]
- Cecere, A.B.; De Cicco, A.; Bruno, G.; Toro, G.; Errico, G.; Braile, A.; Panni, A.S. SuperPath approach is a recommendable option in frail patients with femoral neck fractures: A case-control study. Arch. Orthop. Trauma Surg. 2022, 142, 3265–3270. [Google Scholar] [CrossRef]
- Busch, A.; Wegner, A.; Wassenaar, D.; Brandenburger, D.; Haversath, M.; Jäger, M. SuperPath® vs. direct anterior approach: A retrospective comparison between two minimally invasive approaches in total hip arthroplasty. Die Orthopädie 2022, 51, 986–995. [Google Scholar] [CrossRef]
- Gofton, W.; Chow, J.; Olsen, K.D.; Fitch, D.A. Thirty-day readmission rate and discharge status following total hip arthroplasty using the supercapsular percutaneously-assisted total hip surgical technique. Int. Orthop. 2015, 39, 847–851. [Google Scholar] [CrossRef] [PubMed]
- Della Torre, P.K.; Fitch, D.A.; Chow, J.C. Supercapsular percutaneously-assisted total hip arthroplasty: Radiographic outcomes and surgical technique. Ann. Transl. Med. 2015, 3, 180. [Google Scholar] [CrossRef] [PubMed]
- Cardenas-Nylander, C.; Bellotti, V.; Astarita, E.; Gomez, E.M.; Fernandez, M.R. Innovative approach in total hip arthroplasty: Supercapsular percutaneously-assisted. Hip Int. 2016, 26, S34–S37. [Google Scholar] [CrossRef]
- Bodrogi, A.W.; Sciortino, R.; Fitch, D.A.; Gofton, W. Use of the supercapsular percutaneously assisted total hip approach for femoral neck fractures: Surgical technique and case series. J. Orthop. Surg. Res. 2016, 11, 113. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mitchell, R.J.; Kay, A.B.; Smith, K.M.; Murphy, S.B.; Le, D.T. Early results of displaced femoral neck fragility fractures treated with supercapsular percutaneous-assisted total hip arthroplasty. Arthroplast. Today 2019, 5, 193–196. [Google Scholar] [CrossRef] [PubMed]
- Quitmann, H. Supercapsular percutaneously assisted (SuperPath) approach in total hip arthroplasty: Surgical technique and preliminary results. Oper. Orthop. Traumatol. 2019, 31, 536–546. [Google Scholar] [CrossRef]
- Scaglione, M.; Casella, F.; Giuntoli, M.; Celli, F.; Fabbri, L.; Marchetti, S. The role of superior capsular approach (SuperPATH) in the treatment of femoral neck fractures with hemiarthroplasty implantation: Our experience and review of literature. Acta Biomed. 2020, 91, e2020114. [Google Scholar] [CrossRef]
- Kay, A.; Klavas, D.; Haghshenas, V.; Phan, M.; Le, D. Two year follow up of supercapsular percutaneously assisted total hip arthroplasty. BMC Musculoskelet. Disord. 2021, 22, 478. [Google Scholar] [CrossRef]
- Flevas, D.A.; Tsakotos, G.A.; Benakis, L.N.; Sasalos, G.G.; Tokis, A.V. The Supercapsular Percutaneously Assisted Total Hip (SuperPATH) Approach Revisited: Technique Improvements after the Perioperative Experience of 344 Cases. Life 2022, 12, 981. [Google Scholar] [CrossRef] [PubMed]
- Hagio, K.; Aikawa, K. Minimally invasive surgery supercapsular percutaneously-assisted total hip (SuperPath) arthroplasty. Acta Biomed. 2023, 94, e2023069. [Google Scholar] [CrossRef]
- Yao, J.; Ding, H. Research progress of supercapsular percutaneously assisted total hip in minimally invasive total hip arthroplasty. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016, 30, 1170–1173. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Chow, J. SuperPath: The Direct Superior Portal-Assisted Total Hip Approach. JBJS Essent. Surg. Tech. 2017, 7, e23. [Google Scholar] [CrossRef] [PubMed]
- Barrett, A.A.; Ezzibdeh, R.M.; Horst, P.K.; Roger, D.J.; Amanatullah, D.F. Direct Superior Approach to the Hip for Total Hip Arthroplasty. JBJS Essent. Surg. Tech. 2019, 9, e17. [Google Scholar] [CrossRef] [PubMed]
- Cronin, M.D.; Gofton, W.; Erwin, L.; Fitch, D.A.; Chow, J. Early surgical and functional outcomes comparison of the supercapsular percutaneously-assisted total hip and traditional posterior surgical techniques for total hip arthroplasty: Protocol for a randomized, controlled study. Ann. Transl. Med. 2015, 3, 335. [Google Scholar] [CrossRef]

| First Author | Year of Publication | Origin | Language | Journal (ISSN) | Study Design | Study Protocol | Operation | Compared with: | Surgical Indication | Databases Searched | Included Studies | Quality Assessment | Number of Patients | Outcome Parameters | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ramadanov N et al. [18] | 2020 | Germany/ Spain | English | Journal of Orthopedic Surgery and Research (1749–799X) | Meta-analysis | Yes | THA, HA | CAs | OA, ANFH, FNF | PubMed, Cochrane Library, Clinical Trials, CNKI, Google Scholar | 12 RCTs | RoB, LoE, | 726 | 1, 2, 3, 4, 5, 6, 7, 8 | First meta-analysis of SuperPATH in the English-language literature; HA subgroup analysis |
| Ramadanov N et al. [19] | 2021 | Germany/ Spain | English | Journal of Orthopedic Surgery and Research (1749–799X) | Network meta-analysis | Yes | THA | DAA | OA, ANFH, FNF | PubMed, Cochrane Library, Clinical Trials, CNKI, Google Scholar | 16 RCTs | RoB, LoE | 1392 | 1, 2, 3, 4, 5, 6 | First meta-analysis of SuperPATH vs. DAA |
| Ge Y et al. [20] | 2021 | China | English | BioMed Research International (2314–6141) | Meta-analysis | Yes | THA, HA | CAs | OA, FNF | PubMed, Embase, Cochrane Library | 3 RCTs, 3 non-RCTs | RoB, NOS | 526 | 1, 2, 3, 4, 5, 6, 7 | Limitation: both THA, HA |
| Ramadanov et al. [21] | 2021 | Germany/ Spain | English | Orthopedics and Traumatology: Surgery and Research (1877–0568) | Network meta-analysis | Yes | THA | DAA, CAs | OA, ANFH, FNF | PubMed, Scopus, Web of Science, Cochrane Library, Clinical Trials Cinahl, CNKI, | 24 RCTs | RoB, LoE | 2074 | 1, 2, 3, 4, 5, 6 | Update of Ramadanov N et al. [19] |
| Zhao F et al. [22] | 2022 | China | English | Geriatric Orthopedic Surgery and Rehabilitation (2151–4593) | Meta-analysis | No | THA | CAs | FNF | PubMed, Embase, Scopus, Web of Science, Cochrane Library, CNKI, Wanfan | 9 Non-RCTs | RoB, MINORS, PB | 694 | 1, 2, 3, 4, 5, 7, 8 | First meta-analysis of SuperPATH THA in FNFs |
| Ramadanov N [23] | 2022 | Germany | English | Orthopedic Surgery (1757–7861) | Meta-analysis | Yes | THA | CAs | OA, ANFH, FNF | PubMed, Cochrane Library, Clinical Trials, CNKI, Google Scholar | 14 RCTs | RoB, LoE, PB | 1021 | 1, 2, 3, 4, 5, 6, 8 | Update of Ramadanov N et al. [18] |
| Joseph VM et al. [24] | 2022 | United Kingdom | English | HIP International (1724–6067) | Meta-analysis | No | THA, HA | CAs | OA | PubMed, Embase, Scopus, Web of Science, Cochrane Library, Cinahl EMCare | 3 RCTs,4 non-RCTs | RoB | 730 | 1, 2, 3, 4, 5, 6, 7, 8 | Limitation: both THA, HA |
| Ramadanov N et al. [25] | 2022 | Germany/ Spain | English | Scientific Reports (2045–2322) | Network meta-analysis | Yes | THA | DAA, PA | OA, ANFH, FNF, Dysplasia | PubMed, Embase, Cochrane Library, Clinical trials, CNKI | 20 RCTs | RoB, LoE | 1501 | 1, 2, 3, 5, 6 | First meta-analysis of SuperPATH vs. PA |
| Yan L et al. [26] | 2023 | China/ Canada | English | JAMA Network Open (2574–3805) | Network meta-analysis | Yes | THA | 2-incision approach, DAA, LA, MI LA, MI ALA, PA, MI PA | Any indication | PubMed, Embase, Cochrane Library, Clinical Trials | 63 RCTs | RoB, LoE, PB | 4859 | 1, 3, 4, 5, 6, 7, 8, 9 | Highest sample size |
| First Author | Year of Publication | Origin | Language | Journal (ISSN) | Study Design | THA or HA | Cement | Compared with: | Surgical Indication | Number of Patients | Outcome Parameters | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yan T et al. [27] | 2017 | China | Chinese/ English | Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (1002–1892) | RCT | THA | NR | LA | OA, ANFH, FNF, Dysplasia | 154 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8 | Uni- and bilateral THA |
| Xie J et al. [28] | 2017 | China | English | Journal of Orthopedic Surgery and Research (1749–799X) | RCT | THA | Cementless | PA | OA | 92 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8 | No blinding |
| Yuan H et al. [29] | 2018 | China | Chinese/ English | Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (1002–1892) | RCT | THA | NR | PLA | OA, ANFH, FNF, Dysplasia | 84 | 1, 2, 3, 5 (HHS), 9 | - |
| Ouyang C et al. [30] | 2018 | China | Chinese | Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi (1002–1892) | RCT | THA | NR | PLA | OA, ANFH | 24 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10, 12 | Low sample size |
| Jianbo J et al. [31] | 2019 | China | English | Injury (0020–1383) | RCT | HA | NR | PA | FNF | 100 | 1, 2, 3, 4, 5 (HHS), 11 | First RCT on SuperPATH HA in FNF; no blinding |
| Meng W et al. [32] | 2019 | China/ Germany | English | Musculoskeletal Disorders (1471–2474) | RCT | THA | NR | PLA | ANFH | 4 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10, 12 | Bilateral; very low sample size |
| Meng W et al. [33] | 2021 | China/ Germany | English | Annals of Translational Medicine (2305–5847) | RCT | THA | NR | Mini-incision PLA | OA | 40 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10, 12 | - |
| Li X et al. [34] | 2021 | China | English | Asian Journal of Surgery (1015–9584/) | RCT | THA | NR | PLA | ANFH, FNF | 96 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10 | - |
| Khoja YT et al. [35] | 2022 | Canada/ Saudi Arabia | English | Clinical Orthopedics and Related Research (0009–921X) | RCT | THA | Cementless | PA | OA | 46 | 1, 3, 4, 5 (OHS), 6, 7, 8, 10 | - |
| Shen J et al. [36] | 2023 | China | English | Journal of Orthopedic Surgery and Research (1749–799X) | RCT | THA | NR | LA | FNF | 120 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10 | No blinding |
| Korytkin AA et al. [37] | 2023 | Russia/ Marocco | English | HIP International (1724–6067) | RCT | THA | Cementless | Mini-incision PA | OA | 49 | 1, 3, 4, 5 (HHS, HOOS), 6, 7, 8, 10, 12 | - |
| Qurashi S et al. [38] | 2017 | Australia/ USA | English | Journal of Arthroplasty (0883–5403) | Prospective non-RCT | THA | Cementless | SuperPATH | OA, ANFH, Dysplasia | 100 | Brake reaction time after SuperPATH THA | - |
| Más Martínez J et al. [39] | 2019 | Spain | English/ Spanish | Revista Espanola de Cirugia Ortopedica y Traumatologia (1988–8856) | Prospective non-RCT | THA | Cementless | PA | OA | 90 | 1, 3, 5 (HHS, WOMAC), 6, 7, 9 | - |
| Wang XD et al. [40] | 2020 | China | English | Orthopedic Surgery (1757–7861) | Prospective non-RCT | THA | NR | PLA | FNF | 110 | 1, 2, 3, 4, 5 (HHS), 7, 8 | - |
| Tottas S et al. [41] | 2020 | Greece | English | Journal of Orthopedics (0972–978X) | Prospective non-RCT | THA | Cementless | LA | OA, ANFH, Dysplasia | 48 | 1, 2, 3, 4, 5 (HHS), 6, 7, 8, 10 | - |
| Author | Protocol Registered before Commencement of the Review | Adequacy of the Literature Search | Justification for Excluding Individual Studies | RoB from Individual Studies Being Included in the Review | Appropriateness of Meta-Analytical Methods | Consideration of RoB When Interpreting the Results of the Review | Assessment of Presence and Likely Impact of Publication Bias | Overall Quality |
|---|---|---|---|---|---|---|---|---|
| Ramadanov N et al. [18] | High | High | Moderate | High | High | Moderate | Low | Low |
| Ramadanov N et al. [19] | High | High | Moderate | High | High | Moderate | Low | Low |
| Ge Y et al. [20] | High | High | High | High | High | Moderate | Low | Low |
| Ramadanov et al. [21] | High | High | Moderate | High | High | Moderate | Low | Low |
| Zhao F et al. [22] | Low | High | High | High | High | Moderate | High | Low |
| Ramadanov N [23] | High | High | Moderate | High | High | High | High | Moderate |
| Joseph VM et al. [24] | Low | Low | Moderate | High | High | Moderate | Low | Critically low |
| Ramadanov N et al. [25] | High | High | Moderate | High | High | Moderate | Low | Low |
| Yan L et al. [26] | High | Moderate | High | High | High | Moderate | High | Moderate |
| Author | Bias Arising from the Randomization Process | Bias Due to Deviation from Intended Interventions | Bias Due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Result | Overall RoB |
|---|---|---|---|---|---|---|
| Yan T et al. [27] | Some concerns | High RoB | Low RoB | Low RoB | Low RoB | High RoB |
| Xie J et al. [28] | High RoB | Low RoB | Low RoB | Low RoB | Low RoB | High RoB |
| Yuan H et al. [29] | Some concerns | Low RoB | Low RoB | Low RoB | Low RoB | Some concerns |
| Ouyang C et al. [30] | Some concerns | Low RoB | Low RoB | Low RoB | Low RoB | Some concerns |
| Jianbo J et al. [31] | High RoB | Low RoB | Low RoB | Low RoB | Low RoB | High RoB |
| Meng W et al. [32] | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB |
| Meng W et al. [33] | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB |
| Li X et al. [34] | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB |
| Khoja YT et al. [35] | Some concerns | Low RoB | Low RoB | Low RoB | Low RoB | Some concerns |
| Shen J et al. [36] | High RoB | Low RoB | Low RoB | Low RoB | Low RoB | High RoB |
| Korytkin AA et al. [37] | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB |
| First Author | Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Result | Overall RoB |
|---|---|---|---|---|---|---|---|---|
| Qurashi S et al. [38] | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB |
| Más Martínez J et al. [39] | Low RoB | Serious RoB | Low RoB | Low RoB | Low RoB | Moderate RoB | Low RoB | Serious RoB |
| Wang XD et al. [40] | Low RoB | Moderate RoB | Low RoB | Low RoB | Low RoB | Moderate RoB | Low RoB | Moderate RoB |
| Tottas S et al. [41] | Moderate RoB | Serious RoB | Low RoB | Low RoB | Low RoB | Low RoB | Low RoB | Serious RoB |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramadanov, N. SuperPATH—Current Status of Evidence and Further Investigations: A Scoping Review and Quality Assessment. J. Clin. Med. 2023, 12, 5395. https://doi.org/10.3390/jcm12165395
Ramadanov N. SuperPATH—Current Status of Evidence and Further Investigations: A Scoping Review and Quality Assessment. Journal of Clinical Medicine. 2023; 12(16):5395. https://doi.org/10.3390/jcm12165395
Chicago/Turabian StyleRamadanov, Nikolai. 2023. "SuperPATH—Current Status of Evidence and Further Investigations: A Scoping Review and Quality Assessment" Journal of Clinical Medicine 12, no. 16: 5395. https://doi.org/10.3390/jcm12165395
APA StyleRamadanov, N. (2023). SuperPATH—Current Status of Evidence and Further Investigations: A Scoping Review and Quality Assessment. Journal of Clinical Medicine, 12(16), 5395. https://doi.org/10.3390/jcm12165395






