Intrauterine Tamponade Balloon for Management of Severe Postpartum Haemorrhage: Does Early Insertion Change the Outcome? A Retrospective Study on Blood Loss
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Outcome
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Say, L.; Chou, D.; Gemmill, A.; Tunçalp, Ö.; Moller, A.-B.; Daniels, J.; Gülmezoglu, A.M.; Temmerman, M.; Alkema, L. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health 2014, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- CNGOF_2014_Hémorragie du Post-Partum. Available online: https://cngof.fr/app/pdf/RPC//1-RPC%20DU%20CNGOF/2014/CNGOF_2014_HPP.pdf?x72671 (accessed on 7 July 2023).
- Borovac-Pinheiro, A.; Pacagnella, R.C.; Cecatti, J.G.; Miller, S.; El Ayadi, A.M.; Souza, J.P.; Durocher, J.; Blumenthal, P.D.; Winikoff, B. Postpartum hemorrhage: New insights for definition and diagnosis. Am. J. Obstet. Gynecol. 2018, 219, 162–168. [Google Scholar] [CrossRef]
- Knight, M.; Kurinczuk, J.J.; Spark, P.; Brocklehurst, P. Cesarean Delivery and Peripartum Hysterectomy. Obstet. Gynecol. 2008, 111, 97–105. [Google Scholar] [CrossRef]
- Maternal Morbidity Data in Australia: An Assessment of the Feasibility of Standardised Collection; Australian Institute of Health and Welfare: Canberra, Australia, 2012.
- Zwart, J.; Richters, J.; Öry, F.; De Vries, J.; Bloemenkamp, K.; Van Roosmalen, J. Severe maternal morbidity during pregnancy, delivery and puerperium in the Netherlands: A nationwide population-based study of 371 000 pregnancies. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 842–850. [Google Scholar] [CrossRef]
- Bonnet, M.P.; Basso, O.; Bouvier-Colle, M.H.; Dupont, C.; Rudigoz, R.C.; Fuhrer, R.; Deneux-Tharaux, C. Postpartum Haemorrhage in Canada and France: A Population-Based Comparison. PLoS ONE 2013, 8, e66882. [Google Scholar] [CrossRef] [PubMed]
- Chandraharan, E.; Arulkumaran, S. Surgical aspects of postpartum haemorrhage. Best Pract. Res. Clin. Obstet. Gynaecol. 2008, 22, 1089–1102. [Google Scholar] [CrossRef] [PubMed]
- Russell, R.T. WHO guidelines for the management of postpartum haemorrhage and retained placenta. Hum. Fertil. 2011, 14, 129. [Google Scholar] [CrossRef]
- Driessen, M.; Bouvier-Colle, M.H.; Dupont, C.; Khoshnood, B.; Rudigoz, R.C.; Deneux-Tharaux, C. Postpartum Hemorrhage Resulting From Uterine Atony After Vaginal Delivery. Obstet. Gynecol. 2011, 117, 11. [Google Scholar] [CrossRef]
- Al-Zirqi, I.; Vangen, S.; Forsen, L.; Stray-Pedersen, B. Prevalence and risk factors of severe obstetric haemorrhage. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 1265–1272. [Google Scholar] [CrossRef]
- Ahonen, J.; Stefanovic, V.; Lassila, R. Management of post-partum haemorrhage: Management of PPH. Acta Anaesthesiol. Scand. 2010, 54, 1164–1178. [Google Scholar] [CrossRef]
- Bakri, Y.; B-Lynch, C.; Alouini, S. Second generation of intrauterine balloon tamponade: New perspective. BMJ Innov. 2020, 6, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Bakri, Y.N.; Amri, A.; Abdul Jabbar, F. Tamponade-balloon for obstetrical bleeding. Int. J. Gynecol. Obstet. 2001, 74, 139–142. [Google Scholar] [CrossRef]
- Clinical Management Guidelines for Obstetrician-Gynecologists. Number 47, October 2003: Prophylactic Antibiotics in Labor and Delivery. Obstet. Gynecol. 2003, 102, 875–882. [Google Scholar]
- Georgiou, C. Balloon tamponade in the management of postpartum haemorrhage: A review. BJOG Int. J. Obstet. Gynaecol. 2009, 116, 748–757. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.S.; Faraag, E.; Mohammed, M.; Elmarghany, Z.; Helaly, M.; Gadallah, A.; Taymour, M.A.; Ahmad, Y.; Eissa, A.I.; Ogila, A.I.; et al. The safety and effectiveness of Bakri balloon in the management of postpartum hemorrhage: A systematic review. J. Matern.-Fetal Neonatal Med. 2021, 34, 300–307. [Google Scholar]
- Revert, M.; Cottenet, J.; Raynal, P.; Cibot, E.; Quantin, C.; Rozenberg, P. Intrauterine balloon tamponade for management of severe postpartum haemorrhage in a perinatal network: A prospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2017, 124, 1255–1262. [Google Scholar] [CrossRef]
- Lo, A.; St. Marie, P.; Yadav, P.; Belisle, E.; Markenson, G. The impact of Bakri balloon tamponade on the rate of postpartum hysterectomy for uterine atony. J. Matern.-Fetal Neonatal Med. 2017, 30, 1163–1166. [Google Scholar] [CrossRef]
- Doumouchtsis, S.K.; Papageorghiou, A.T.; Arulkumaran, S. Systematic Review of Conservative Management of Postpartum Hemorrhage: What to Do When Medical Treatment Fails. Obstet. Gynecol. Surv. 2007, 62, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Habib, N.; Luton, D.; Centini, G.; Renuit, I.; Birbarah, C.; Ceccaldi, P.F. Advanced Interventional Procedures after Intrauterine Tamponade Balloon Insertion in a Tertiary Care Center. J. Investig. Surg. 2021, 34, 373–379. [Google Scholar] [CrossRef]
- ElFarra, J.; Matias-Gomes, S.; Shevell, T.; Tamim, H.; Bobby, P. 554: The effect of postgraduate training level on the accuracy of clinically estimated fetal weights. Am. J. Obstet. Gynecol. 2013, 208, S238. [Google Scholar] [CrossRef]
- Alkış, İ.; Karaman, E.; Han, A.; Ark, H.C.; Büyükkaya, B. The fertility sparing management of postpartum hemorrhage: A series of 47 cases of Bakri balloon tamponade. Taiwan. J. Obstet. Gynecol. 2015, 54, 232–235. [Google Scholar] [CrossRef] [PubMed]
- Niola, R.; Giurazza, F.; Torbica, A.; Schena, E.; Silvestre, M.; Maglione, F. Predelivery uterine arteries embolization in patients with placental implant anomalies: A cost-effective procedure. Radiol Med. 2017, 122, 77–79. [Google Scholar] [CrossRef]
- Schmitz, T.; Tararbit, K.; Dupont, C.; Rudigoz, R.C.; Bouvier-Colle, M.H.; Deneux-Tharaux, C. Prostaglandin E2 Analogue Sulprostone for Treatment of Atonic Postpartum Hemorrhage. Obstet. Gynecol. 2011, 118, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Grillo-Ardila, C.F.; Ruiz-Parra, A.I.; Gaitán, H.G.; Rodriguez-Malagon, N. Prostaglandins for management of retained placenta. In Cochrane Database of Systematic Reviews; The Cochrane Collaboration, Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2013; p. CD010312. [Google Scholar] [CrossRef]
- Doumouchtsis, S.K.; Papageorghiou, A.T.; Vernier, C.; Arulkumaran, S. Management of postpartum hemorrhage by uterine balloon tamponade: Prospective evaluation of effectiveness. Acta Obs. Gynecol. Scand. 2008, 87, 849–855. [Google Scholar] [CrossRef]
- Yang, H.; Sun, G.; Cheng, Y.; Cao, D.; Zhao, Y. Bakri balloon tamponade to treat postpartum hemorrhage. Chin. Med. J. 2022, 135, 2258–2260. [Google Scholar] [CrossRef]
- Rocher, G.; Panel, P.; Rollin, I.; Wormser, A.; Souiai-Hidoussi, A.; Raynal, P.; Niro, J. Massive hemoperitoneum due to uterine perforation by the Bakri Balloon, during the treatment of postpartum hemorrhage. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 75–76. [Google Scholar] [CrossRef]
- Leparco, S.; Viot, A.; Benachi, A.; Deffieux, X. Migration of Bakri balloon through an unsuspected uterine perforation during the treatment of secondary postpartum hemorrhage. Am. J. Obstet. Gynecol. 2013, 208, e6–e7. [Google Scholar] [CrossRef]
- Howard, T.F.; Grobman, W.A. The relationship between timing of postpartum hemorrhage interventions and adverse outcomes. Am. J. Obstet. Gynecol. 2015, 213, 239.e1–239.e3. [Google Scholar] [CrossRef]
- Jauniaux, E.; Alfirevic, Z.; Bhide, A.G.; Belfort, M.A.; Burton, G.J.; Collins, S.L.; Dornan, S.; Jurkovic, D.; Kayem, G.; Kingdom, J.; et al. Placenta Praevia and Placenta Accreta: Diagnosis and Management: Green-top Guideline No. 27a. BJOG Int. J. Obstet. Gynaecol. 2019, 126, e1–e48. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.C.; To, W.W. Balloon tamponade for postpartum haemorrhage: Case series and literature review. Hong Kong Med. J. 2013, 19, 484–490. Available online: http://www.hkmj.org/abstracts/v19n6/484.htm (accessed on 16 August 2022). [CrossRef] [PubMed]
- Poujade, O.; Grossetti, A.; Mougel, L.; Ceccaldi, P.; Ducarme, G.; Luton, D. Risk of synechiae following uterine compression sutures in the management of major postpartum haemorrhage: Uterine compression suture for PPH: Efficiency and risk of synechiae. BJOG Int. J. Obstet. Gynaecol. 2011, 118, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Dorkham, M.C.; Epee-Bekima, M.J.; Sylvester, H.C.; White, S.W. Experience of Bakri balloon tamponade at a single tertiary centre: A retrospective case series. J. Obstet. Gynaecol. 2021, 41, 854–859. [Google Scholar] [CrossRef] [PubMed]
- Alouini, S.; Bedouet, L.; Ramos, A.; Ceccaldi, C.; Evrard, M.L.; Khadre, K. Évaluation du ballon de Bakri dans les hémorragies graves du post-partum et fertilité ultérieure. J. Gynécol. Obs. Biol. Reprod. 2015, 44, 171–175. [Google Scholar] [CrossRef]
- Kong, C.W.; To, W.W.K. Menstrual and reproductive outcomes after use of balloon tamponade for severe postpartum hemorrhage. BMC Pregnancy Childbirth 2018, 18, 451. [Google Scholar] [CrossRef]
- Serres-Cousine, O.; Kuijper, F.M.; Curis, E.; Atashroo, D. Clinical investigation of fertility after uterine artery embolization. Am. J. Obstet. Gynecol. 2021, 225, 403.e1–403.e22. [Google Scholar] [CrossRef]
- McLucas, B.; Voorhees Iii, W.D.; Elliott, S. Fertility after uterine artery embolization: A review. Minim. Invasive Ther. Allied Technol. 2016, 25, 1–7. [Google Scholar] [CrossRef]
- Einerson, B.D.; Son, M.; Schneider, P.; Fields, I.; Miller, E.S. The association between intrauterine balloon tamponade duration and postpartum hemorrhage outcomes. Am. J. Obstet. Gynecol. 2017, 216, 300.e1–300.e5. [Google Scholar] [CrossRef]
- Wong, M.S.; Dellapiana, G.; Greene, N.; Gregory, K.D. Antibiotics during Intrauterine Balloon Tamponade Is Associated with a Reduction in Endometritis. Amer. J. Perinatol. 2019, 36, 1211–1215. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Sethi, A. Endometritis—Diagnosis, Treatment and its impact on fertility—A Scoping Review. JBRA 2022, 26, 538. Available online: https://www.jbra.com.br/trab/pub/download_trabalho.php?fileSource=/var/www/vhosts/jbra.com.br/media/trab/arq_3532&fileName=22%20-%201858%20-%20Endometritis.pdf&id_trabalho=1280 (accessed on 5 August 2023). [CrossRef] [PubMed]
| Group < 15 min (52 Patients) | Group > 15 min (29 Patients) | p Value | |
|---|---|---|---|
| Age (years) | 31.98 ± 5.46 | 31.01 ± 5.28 | 0.2176 |
| Gestation | 2.60 ± 2.00 | 2.17 ± 1.31 | 0.3097 |
| Parity | 1.85 ± 1.38 | 1.76 ± 1.02 | 0.7658 |
| Gestation age at birth (WG) | 39.03 ± 2.05 | 38.86 ± 3.25 | 0.7727 |
| Foetal weight (g) | 3642.98 ± 586.79 | 3692.24 ± 752.25 | 0.7446 |
| Haemoglobin at the time PPH diagnosis (g/dL) | 9.33 ± 1.77 | 8.39 ± 1.86 | 0.0274 |
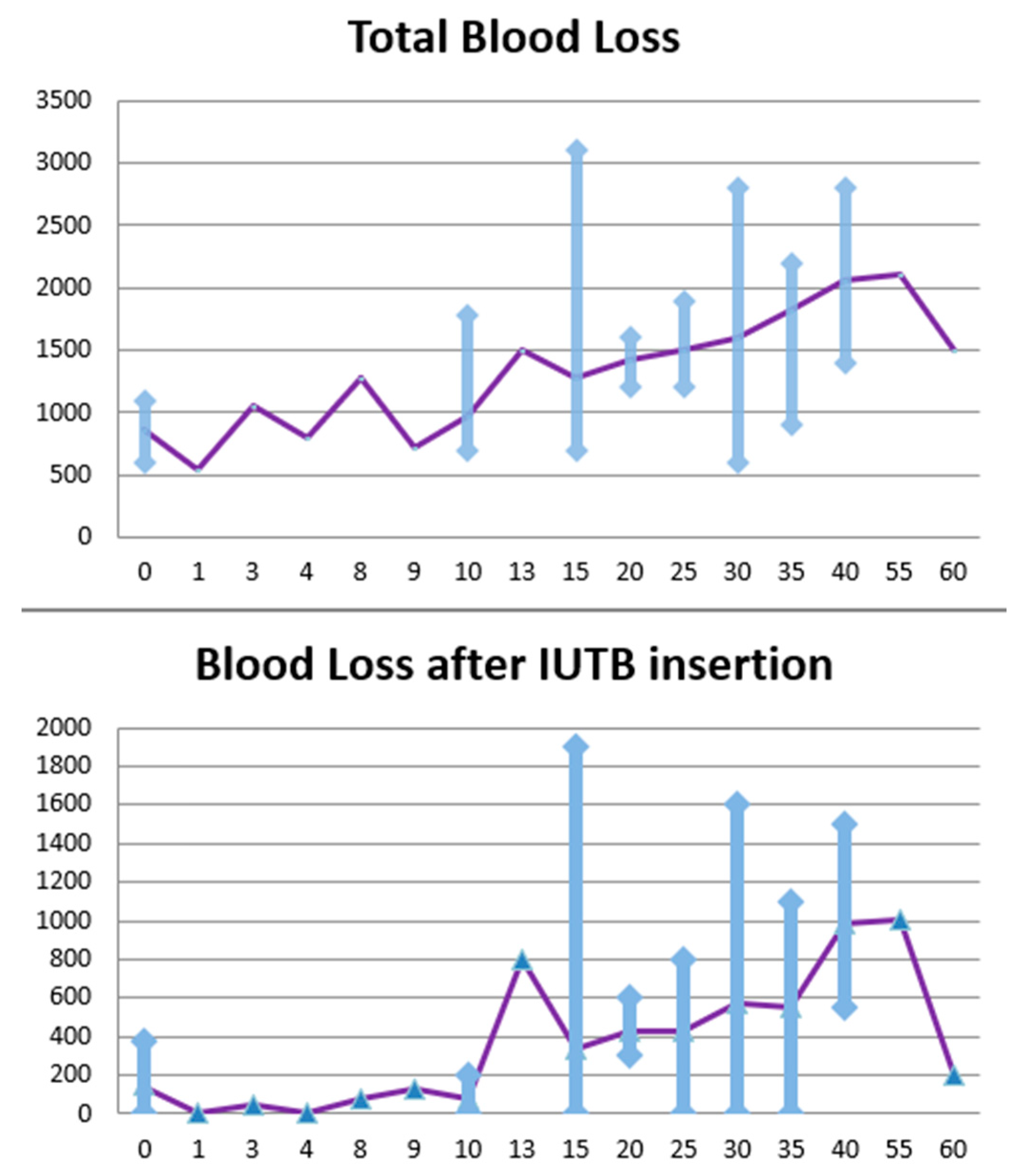
| Mean blood loss before IUTB insertion (mL) | 899.04 ± 225.89 | 1087 ± 237.04 | 0.0007 |
| Total blood loss (mL) | 1150.96 ± 485.02 | 1627.59 ± 498.90 | 0.00001 |
| Mean blood loss after IUTB insertion (mL) | 251.92 ± 344.56 | 540.52 ± 414.06 | 0.0012 |
| No. of red blood cell units | 1.61 ± 1.79 | 3.79 ± 3.23 | 0.00002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Futcher, F.; Moufawad, G.; Centini, G.; Hayek, J.; Tarchichi, J.; Bakar, J.; Habib, N. Intrauterine Tamponade Balloon for Management of Severe Postpartum Haemorrhage: Does Early Insertion Change the Outcome? A Retrospective Study on Blood Loss. J. Clin. Med. 2023, 12, 5439. https://doi.org/10.3390/jcm12175439
Futcher F, Moufawad G, Centini G, Hayek J, Tarchichi J, Bakar J, Habib N. Intrauterine Tamponade Balloon for Management of Severe Postpartum Haemorrhage: Does Early Insertion Change the Outcome? A Retrospective Study on Blood Loss. Journal of Clinical Medicine. 2023; 12(17):5439. https://doi.org/10.3390/jcm12175439
Chicago/Turabian StyleFutcher, Françoise, Graziella Moufawad, Gabriele Centini, Jad Hayek, Jana Tarchichi, Joseph Bakar, and Nassir Habib. 2023. "Intrauterine Tamponade Balloon for Management of Severe Postpartum Haemorrhage: Does Early Insertion Change the Outcome? A Retrospective Study on Blood Loss" Journal of Clinical Medicine 12, no. 17: 5439. https://doi.org/10.3390/jcm12175439
APA StyleFutcher, F., Moufawad, G., Centini, G., Hayek, J., Tarchichi, J., Bakar, J., & Habib, N. (2023). Intrauterine Tamponade Balloon for Management of Severe Postpartum Haemorrhage: Does Early Insertion Change the Outcome? A Retrospective Study on Blood Loss. Journal of Clinical Medicine, 12(17), 5439. https://doi.org/10.3390/jcm12175439








