Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Clinical Evaluations
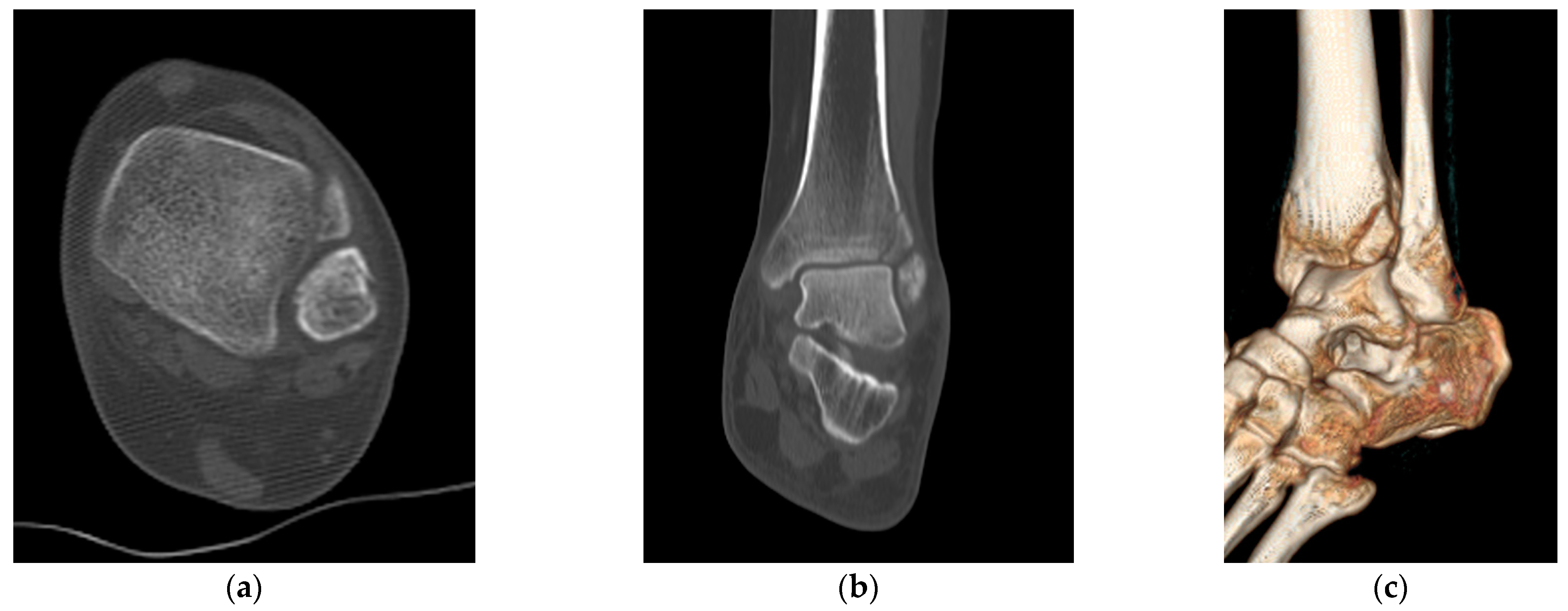
2.3. Radiological Evaluations
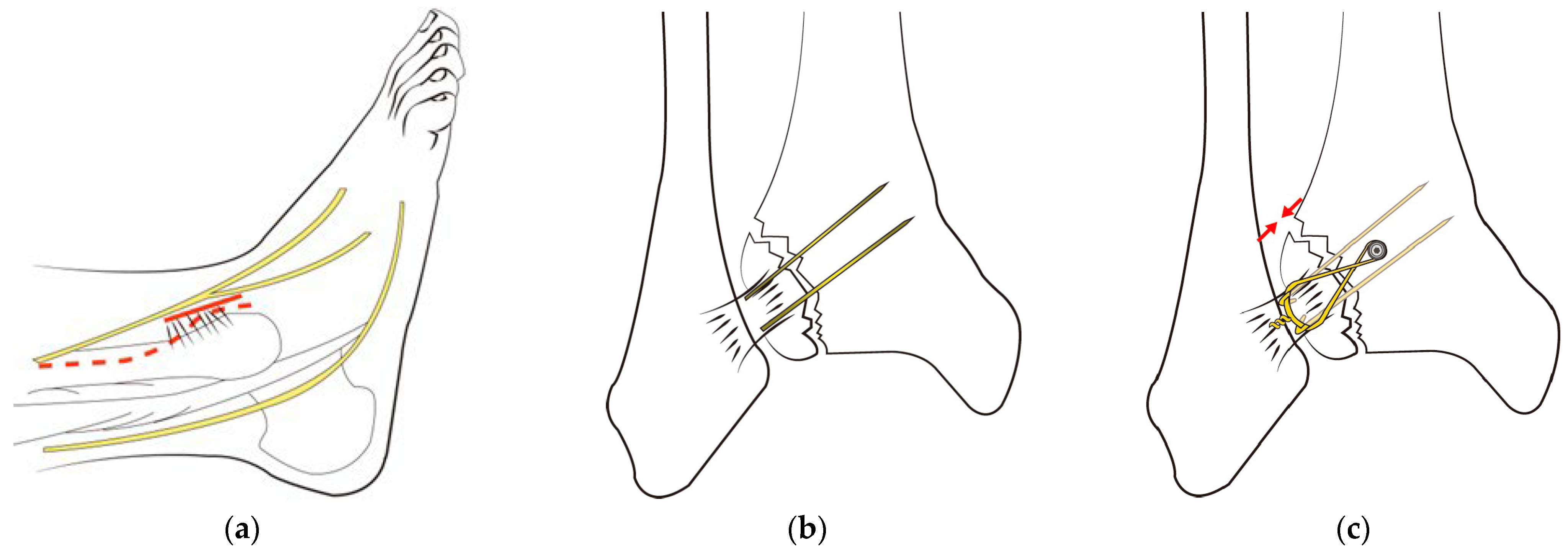
2.4. Surgery
2.5. Statistical Analysis
3. Results
3.1. Clinical Outcomes
3.2. Radiologic Outcomes
3.3. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kannus, P.; Palvanen, M.; Niemi, S.; Parkkari, J.; Järvinen, M. Increasing number and incidence of low-trauma ankle fractures in elderly people: Finnish statistics during 1970–2000 and projections for the future. Bone 2002, 31, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Scheer, R.C.; Newman, J.M.; Zhou, J.J.; Oommen, A.J.; Naziri, Q.; Shah, N.V.; Pascal, S.C.; Penny, G.S.; McKean, J.M.; Tsai, J.; et al. Ankle Fracture Epidemiology in the United States: Patient-Related Trends and Mechanisms of Injury. J. Foot Ankle Surg. 2020, 59, 479–483. [Google Scholar] [CrossRef]
- Delco, M.L.; Kennedy, J.G.; Bonassar, L.J.; Fortier, L.A. Post-traumatic osteoarthritis of the ankle: A distinct clinical entity requiring new research approaches. J. Orthop. Res. 2017, 35, 440–453. [Google Scholar] [CrossRef]
- Pogliacomi, F.; De Filippo, M.; Casalini, D.; Longhi, A.; Tacci, F.; Perotta, R.; Pagnini, F.; Tocco, S.; Ceccarelli, F. Acute syndesmotic injuries in ankle fractures: From diagnosis to treatment and current concepts. World J. Orthop. 2021, 12, 270–291. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie-Harris, D.J.; Reed, S.C.; Hedman, T.P. Disruption of the ankle syndesmosis: Biomechanical study of the ligamentous restraints. Arthroscopy 1994, 10, 558–560. [Google Scholar] [CrossRef] [PubMed]
- Xenos, J.S.; Hopkinson, W.J.; Mulligan, M.E.; Olson, E.J.; Popovic, N.A. The tibiofibular syndesmosis. Evaluation of the ligamentous structures, methods of fixation, and radiographic assessment. J. Bone Jt. Surg. Am. 1995, 77, 847–856. [Google Scholar] [CrossRef]
- Mishra, P.K.; Patidar, V.; Singh, S.P. Chaput Tubercle Fracture in an Adult- A Rare Case Report. J. Clin. Diagn. Res. 2017, 11, rd01–rd02. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.J.; Bae, S.Y.; Kim, M.Y. Treatment of Anteroinferior Tibiofibular Ligament Avulsion Fracture Accompanied with Ankle Fracture. JKFAS 2011, 15, 13–17. [Google Scholar]
- Birnie, M.F.N.; van Schilt, K.L.J.; Sanders, F.R.K.; Kloen, P.; Schepers, T. Anterior inferior tibiofibular ligament avulsion fractures in operatively treated ankle fractures: A retrospective analysis. Arch. Orthop. Trauma Surg. 2019, 139, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Bae, K.J.; Kang, S.B.; Kim, J.; Lee, J.; Go, T.W. Reduction and fixation of anterior inferior tibiofibular ligament avulsion fracture without syndesmotic screw fixation in rotational ankle fracture. J. Int. Med. Res. 2020, 48, 300060519882550. [Google Scholar] [CrossRef] [PubMed]
- Uygur, E.; Poyanli, O.; Mutlu, İ.; Çelik, T.; Akpinar, F. Medial malleolus fractures: A biomechanical comparison of tension band wiring fixation methods. Orthop. Traumatol. Surg. Res. 2018, 104, 1259–1263. [Google Scholar] [CrossRef]
- Yeo, E.D.; Jung, K.J.; Hong, Y.C.; Hong, C.H.; Lee, H.S.; Won, S.H.; Yoon, S.J.; Kim, S.H.; Ji, J.Y.; Lee, D.W.; et al. A Tension-Band Wiring Technique for Direct Fixation of a Chaput Tubercle Fracture: Technical Note. Medicina 2022, 58, 1005. [Google Scholar] [CrossRef] [PubMed]
- McKeown, R.; Parsons, H.; Ellard, D.R.; Kearney, R.S. An evaluation of the measurement properties of the Olerud Molander Ankle Score in adults with an ankle fracture. Physiotherapy 2021, 112, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, M.E.; Hagemeijer, N.; Guss, D.; El-Hawary, A.; El-Mowafi, H.; DiGiovanni, C.W. Evaluation of Syndesmosis Reduction on CT Scan. Foot Ankle Int. 2019, 40, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Yeung, T.W.; Chan, C.Y.; Chan, W.C.; Yeung, Y.N.; Yuen, M.K. Can pre-operative axial CT imaging predict syndesmosis instability in patients sustaining ankle fractures? Seven years’ experience in a tertiary trauma center. Skelet. Radiol. 2015, 44, 823–829. [Google Scholar] [CrossRef] [PubMed]
- Nault, M.L.; Hébert-Davies, J.; Laflamme, G.Y.; Leduc, S. CT scan assessment of the syndesmosis: A new reproducible method. J. Orthop. Trauma 2013, 27, 638–641. [Google Scholar] [CrossRef]
- Kocadal, O.; Yucel, M.; Pepe, M.; Aksahin, E.; Aktekin, C.N. Evaluation of Reduction Accuracy of Suture-Button and Screw Fixation Techniques for Syndesmotic Injuries. Foot Ankle Int. 2016, 37, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Elgafy, H.; Semaan, H.B.; Blessinger, B.; Wassef, A.; Ebraheim, N.A. Computed tomography of normal distal tibiofibular syndesmosis. Skelet. Radiol. 2010, 39, 559–564. [Google Scholar] [CrossRef]
- Dikos, G.D.; Heisler, J.; Choplin, R.H.; Weber, T.G. Normal tibiofibular relationships at the syndesmosis on axial CT imaging. J. Orthop. Trauma 2012, 26, 433–438. [Google Scholar] [CrossRef]
- Davidovitch, R.I.; Weil, Y.; Karia, R.; Forman, J.; Looze, C.; Liebergall, M.; Egol, K. Intraoperative syndesmotic reduction: Three-dimensional versus standard fluoroscopic imaging. J. Bone Jt. Surg. Am. 2013, 95, 1838–1843. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Warner, S.J.; Fabricant, P.D.; Garner, M.R.; Schottel, P.C.; Helfet, D.L.; Lorich, D.G. The Measurement and Clinical Importance of Syndesmotic Reduction After Operative Fixation of Rotational Ankle Fractures. J. Bone Jt. Surg. Am. 2015, 97, 1935–1944. [Google Scholar] [CrossRef] [PubMed]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Narain, F.; Van Zwieten, K.J.; Lippens, P.; Schmidt, K.; Gervois, P.; Colla, P.; Palmers, Y.; Vandersteen, M.; Reyskens, A.; Robeyns, I. Foot inversion and eversion movements in stance and swing-some comparative-anatomical and functional morphological aspects. Mater. Fourth All Russ. Sci. Pract. Conf. Int. Particip. 335 Health Base Hum. Potential Probl. Ways Their Solut. 2009, 4, 428–429. [Google Scholar]
- Kapandji, I.A. Physiology of the Joints, 6th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2016; Volume 2. [Google Scholar]
- Norkus, S.A.; Floyd, R.T. The anatomy and mechanisms of syndesmotic ankle sprains. J. Athl. Train. 2001, 36, 68–73. [Google Scholar]
- Lee, H.S.; Park, S.S.; Kim, J.W.; Shin, M.J.; Kim, S.M.; Lee, S.H.; Lee, S.M. Diagnostic Value of Ultrasonography for Acute Tear of Tibiofibular Syndesmosis in Ankle. JKFAS 2004, 8, 1–6. [Google Scholar]
- Broos, P.; Bisschop, A. Operative treatment of ankle fractures in adults: Correlation between types of fracture and final results. Injury 1991, 22, 403–406. [Google Scholar] [CrossRef]
- Park, J.W.; Kim, S.K.; Hong, J.S.; Park, J.H. Anterior tibiofibular ligament avulsion fracture in weber type B lateral malleolar fracture. J. Trauma Acute Care Surg. 2002, 52, 655–659. [Google Scholar] [CrossRef] [PubMed]
- Court-Brown, C.M.; Heckman, J.D.; McQueen, M.M.; Ricci, W.M.; Tornetta, P.; McKee, M.D. Rockwood and Green’s Fractures in Adults, 8th ed.; Wolters Kluwer Health Philadelphia: Philadelphia, PA, USA, 2015. [Google Scholar]
- Elsoe, R.; Ostgaard, S.E.; Larsen, P. Population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg. 2018, 24, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Juto, H.; Nilsson, H.; Morberg, P. Epidemiology of Adult Ankle Fractures: 1756 cases identified in Norrbotten County during 2009–2013 and classified according to AO/OTA. BMC Musculoskelet. Disord. 2018, 19, 441. [Google Scholar] [CrossRef]
- Seeley, D.G.; Browner, W.S.; Nevitt, M.C.; Genant, H.K.; Scott, J.C.; Cummings, S.R. Which fractures are associated with low appendicular bone mass in elderly women? The Study of Osteoporotic Fractures Research Group. Ann. Intern. Med. 1991, 115, 837–842. [Google Scholar] [CrossRef]
- Hasselman, C.T.; Vogt, M.T.; Stone, K.L.; Cauley, J.A.; Conti, S.F. Foot and ankle fractures in elderly white women. Incidence and risk factors. J. Bone Jt. Surg. Am. 2003, 85, 820–824. [Google Scholar] [CrossRef]
- Ramsey, P.L.; Hamilton, W. Changes in tibiotalar area of contact caused by lateral talar shift. J. Bone Jt. Surg. Am. 1976, 58, 356–357. [Google Scholar] [CrossRef]
- Lauge-Hansen, N. Fractures of the ankle. II. Combined experimental-surgical and experimental-roentgenologic investigations. Arch. Surg. 1950, 60, 957–985. [Google Scholar] [CrossRef]
- Rasmussen, O. Stability of the ankle joint. Analysis of the function and traumatology of the ankle ligaments. Acta Orthop. Scand. Suppl. 1985, 211, 1–75. [Google Scholar] [CrossRef] [PubMed]
- Gougoulias, N.; Khanna, A.; Sakellariou, A.; Maffulli, N. Supination-external rotation ankle fractures: Stability a key issue. Clin. Orthop. Relat. Res. 2010, 468, 243–251. [Google Scholar] [CrossRef]
- Wagstaffe, W. An unusual form of fracture of the fibula. St. Thomas Hosp. Rep. 1875, 6, 43–49. [Google Scholar]
- Pankovich, A.M. Fractures of the fibula at the distal tibiofibular syndesmosis. Clin. Orthop. Relat. Res. 1979, 143, 138–147. [Google Scholar] [CrossRef]
- Danis, R. Les Fractures Malleolaires; Theorie et Pratique de l’Osteosynthese Masson: Paris, France, 1949; pp. 133–165. [Google Scholar]
- Yuen, C.P.; Lui, T.H. Distal Tibiofibular Syndesmosis: Anatomy, Biomechanics, Injury and Management. Open Orthop. J. 2017, 11, 670–677. [Google Scholar] [CrossRef]
- Akseki, D.; Pinar, H.; Bozkurt, M.; Yaldiz, K.; Arag, S. The distal fascicle of the anterior inferior tibiofibular ligament as a cause of anterolateral ankle impingement: Results of arthroscopic resection. Acta Orthop. Scand. 1999, 70, 478–482. [Google Scholar] [CrossRef]
- Bassett, F., 3rd; Gates, H., 3rd; Billys, J.; Morris, H.; Nikolaou, P. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. JBJS 1990, 72, 55–59. [Google Scholar] [CrossRef]
- Haraguchi, N.; Toga, H.; Shiba, N.; Kato, F. Avulsion fracture of the lateral ankle ligament complex in severe inversion injury: Incidence and clinical outcome. Am. J. Sport. Med. 2007, 35, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Shu, H.; Li, W.; Liu, Y.; Shi, B.; Zheng, G. Clinical features and surgical effectiveness of ankle fractures involving Tillaux-Chaput in adults. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi Zhongguo Xiufu Chongjian Waike Zazhi Chin. J. Reparative Reconstr. Surg. 2015, 29, 288–291. [Google Scholar]
- Rammelt, S.; Boszczyk, A. Computed tomography in the diagnosis and treatment of ankle fractures: A critical analysis review. JBJS Rev. 2018, 6, e7. [Google Scholar] [CrossRef]
- Gasparova, M.; Falougy, H.; Kubikova, E.; Almasi, J. Isolated “Tillaux” fracture in adulthood: Rarity where the key of success is not to miss it. Bratisl. Lek. Listy 2020, 121, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Perren, S.M.; Allgöwer, M.; Müller, M.E.; Schneider, R.; Willenegger, H. Manual of Internal Fixation: Techniques Recommended by the AO-ASIF Group; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1991. [Google Scholar]
- Kanakis, T.; Papadakis, E.; Orfanos, A.; Andreadakis, A.; Xylouris, E. Figure eight tension band in the treatment of fractures and pseudarthroses of the medial malleolus. Injury 1990, 21, 393–397. [Google Scholar] [CrossRef]




| Method | Description |
|---|---|
| Direct Anterior Difference | This is the perpendicular distance measured from the incisura to the anterior end of the fibular orientation line. |
| Direct Posterior Difference | This refers to the perpendicular distance from the incisura to the posterior end of the line representing the fibular orientation. |
| Fibular Translation | This is the distance measured between the anterior border of the tibial incisura and a line representing the direct anterior difference. It is considered positive when the fibula is situated behind the anterior border of the incisura. |
| Fibular Rotation | This is the angle formed between a line connecting the anterior and posterior borders of the tibial incisura and another line on the fibula indicating its orientation. This angle is deemed positive when the fibula is internally rotated relative to the incisura. |
| Pt. No. | Age | Sex | Cause | Lauge-Hansen Classification | Injured Side | OMAS | VAS Score | ||
|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||||||
| 1 | 57 | F | S | SER IV | Left | 30 | 80 | 8 | 1 |
| 2 | 76 | F | S | SER IV | Left | 25 | 85 | 7 | 0 |
| 3 | 56 | F | S | SER II | Right | 30 | 90 | 8 | 0 |
| 4 | 39 | M | S | SER IV | Left | 35 | 95 | 8 | 0 |
| 5 | 58 | F | S | SER IV | Left | 0 | 80 | 9 | 1 |
| 6 | 79 | F | TA | PER IV | Left | 0 | 70 | 8 | 0 |
| 7 | 53 | F | S | SER IV | Left | 0 | 60 | 9 | 0 |
| 8 | 67 | M | TA | PER IV | Right | 0 | 95 | 8 | 0 |
| 9 | 19 | M | TA | PER II | Right | 0 | 90 | 7 | 0 |
| 10 | 47 | F | S | SER II | Left | 0 | 80 | 8 | 0 |
| 11 | 57 | M | S | PER III | Left | 0 | 90 | 8 | 0 |
| 12 | 68 | F | S | SER IV | Left | 0 | 75 | 7 | 0 |
| 13 | 61 | M | TA | SER IV | Right | 0 | 90 | 7 | 0 |
| 14 | 62 | F | S | SER II | Left | 0 | 85 | 8 | 1 |
| 15 | 31 | F | S | SER III | Right | 0 | 85 | 8 | 0 |
| 16 | 85 | M | TA | SER IV | Right | 0 | 80 | 9 | 0 |
| 17 | 64 | F | S | SER II | Left | 5 | 85 | 8 | 0 |
| 18 | 54 | F | S | PER IV | Right | 0 | 85 | 7 | 1 |
| 19 | 55 | F | S | SER II | Right | 0 | 90 | 8 | 0 |
| 20 | 42 | M | S | SER IV | Left | 0 | 85 | 9 | 0 |
| 21 | 56 | F | S | SER IV | Left | 0 | 80 | 8 | 0 |
| Mean | 56.48 | NA | NA | NA | NA | 5.95 | 83.57 | 7.95 | 0.19 |
| SD | 15.39 | NA | NA | NA | NA | 12.11 | 8.24 | 0.67 | 0.40 |
| p value | <0.001 | <0.001 | |||||||
| Evaluation Method | Observer 1 | Observer 2 | ||||
|---|---|---|---|---|---|---|
| Normal Side (n = 21) | Injured Side (n = 21) | p-Value 2 | Normal Side (n = 21) | Injured Side (n = 21) | p-Value 2 | |
| Direct anterior difference, mm | 4.28 (0.84) 1 | 4.84 (1.36) | 0.114 | 4.29 (0.87) | 4.93 (1.38) | 0.082 |
| Direct posterior difference, mm | 7.70 (0.85) | 7.78 (1.31) | 0.830 | 7.71 (0.83) | 7.78 (1.28) | 0.831 |
| Fibular translation, mm | 1.47 (0.52) | 1.61 (0.53) | 0.380 | 1.51 (0.51) | 1.64 (0.57) | 0.430 |
| Fibular rotation, deg | 8.56 (3.96) | 8.48 (4.13) | 0.948 | 8.62 (3.90) | 8.47 (4.06) | 0.902 |
| Evaluation Method | Intraobserver Reliability | Interobserver Reliability | |
|---|---|---|---|
| Observer 1 | Observer 2 | ||
| Direct anterior difference, mm | 0.885 | 0.886 | 0.950 |
| Direct posterior difference, mm | 0.848 | 0.859 | 0.936 |
| Fibular translation, mm | 0.922 | 0.917 | 0.963 |
| Fibular rotation, deg | 0.902 | 0.900 | 0.957 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoon, S.-J.; Yeo, E.-D.; Jung, K.-J.; Hong, Y.-C.; Hong, C.-H.; Won, S.-H.; Lee, K.-J.; Ji, J.-Y.; Byeon, J.-Y.; Lee, D.-W.; et al. Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures. J. Clin. Med. 2023, 12, 5490. https://doi.org/10.3390/jcm12175490
Yoon S-J, Yeo E-D, Jung K-J, Hong Y-C, Hong C-H, Won S-H, Lee K-J, Ji J-Y, Byeon J-Y, Lee D-W, et al. Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures. Journal of Clinical Medicine. 2023; 12(17):5490. https://doi.org/10.3390/jcm12175490
Chicago/Turabian StyleYoon, Sung-Joon, Eui-Dong Yeo, Ki-Jin Jung, Yong-Cheol Hong, Chang-Hwa Hong, Sung-Hun Won, Kyung-Jin Lee, Jae-Young Ji, Je-Yeon Byeon, Dhong-Won Lee, and et al. 2023. "Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures" Journal of Clinical Medicine 12, no. 17: 5490. https://doi.org/10.3390/jcm12175490
APA StyleYoon, S.-J., Yeo, E.-D., Jung, K.-J., Hong, Y.-C., Hong, C.-H., Won, S.-H., Lee, K.-J., Ji, J.-Y., Byeon, J.-Y., Lee, D.-W., & Kim, W.-J. (2023). Evaluating the Efficacy of Tension Band Wiring Fixation for Chaput Tubercle Fractures. Journal of Clinical Medicine, 12(17), 5490. https://doi.org/10.3390/jcm12175490







