Correlation between Power Elbow Flexion and Physical Performance Test: A Potential Predictor for Assessing Physical Performance in Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Calculation
2.3. Participants
2.4. Outcomes
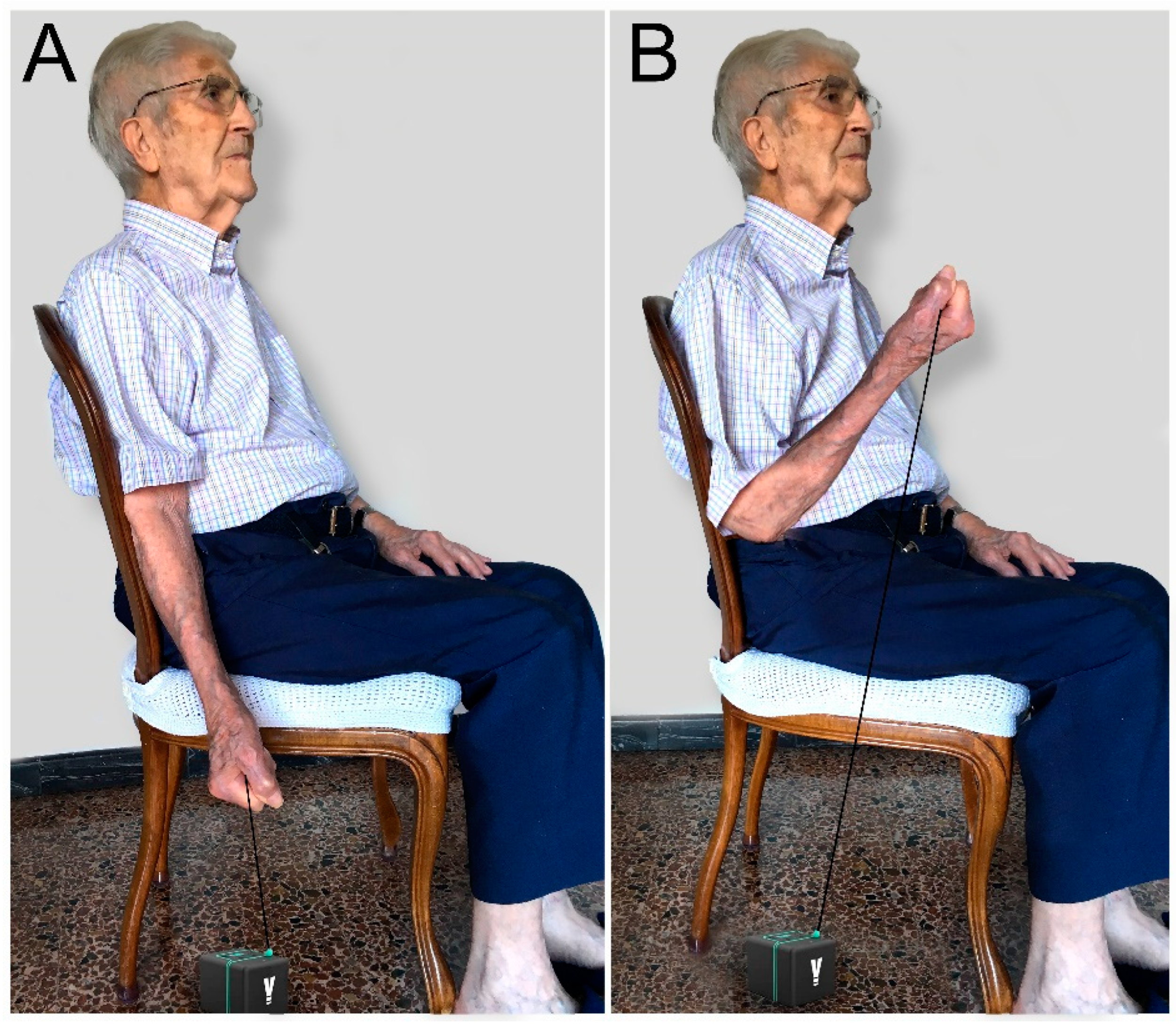
2.4.1. Power Elbow Flexion (PEF)
2.4.2. Short Physical Performance Battery (SPPB)
2.4.3. The 4 Meter Walk Test (4mWT)
2.4.4. Timed Up and Go Test (TUG)
2.4.5. Barthel Index (BI)
2.4.6. Handgrip Strength
2.5. Statistical Analysis
3. Results
3.1. Barthel Index
3.2. SPPB
3.3. The 4mWT
3.4. TUG
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ouchi, Y.; Rakugi, H.; Arai, H.; Akishita, M.; Ito, H.; Toba, K.; Kai, I. Redefining the elderly as aged 75 years and older: Proposal from the joint Committee of Japan Gerontological Society and the Japan geriatrics society. Geriatr. Gerontol. Int. 2017, 17, 1045–1047. [Google Scholar] [CrossRef]
- Christensen, K.; Doblhammer, G.; Rau, R.; Vaupel, J.W. Aging populations: The challenges ahead. Lancet 2009, 374, 1196–1208. [Google Scholar] [CrossRef]
- Cai, Y.; Tian, Q.; Gross, A.L.; Wang, H.; E, J.Y.; Agrawal, Y.; Simonsick, E.M.; Ferrucci, L.; Schrack, J.A. Motor and Physical Function Impairments as Contributors to Slow Gait Speed and Mobility Difficulty in Middle-Aged and Older Adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2022, 77, 1620–1628. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef]
- Matsumoto, K.; Gondo, Y.; Masui, Y.; Yasumoto, S.; Yoshida, Y.; Ikebe, K.; Arai, Y.; Kabayama, M.; Kamide, K.; Akasaka, H.; et al. Physical performance reference values for Japanese oldest old: A SONIC study. BMC Geriatr. 2022, 22, 748. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Kim, M.J.; Yabushita, N.; Tanaka, K. Exploring effective items of physical function in slow walking speed and self-reported mobility limitation in community-dwelling older adults. Geriatr. Gerontol. Int. 2012, 12, 50–58. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical perform-nce battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Labata-Lezaun, N.; González-Rueda, V.; Rodríguez-Sanz, J.; López-de-Celis, C.; Llurda-Almuzara, L.; Rodríguez-Rubio, P.R.; Pérez-Bellmunt, A. Correlation between Physical Performance and Stabilometric Parameters in Older Adults. Medicina 2022, 58, 1211. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Rodrigues, B.; Gonçalves, I.O.; Asano, R.Y.; Uchida, M.C.; Marzetti, E. The physical capabilities underlying timed “Up and Go” tests are time-dependent in community-dwelling older women. Exp. Gerontol. 2018, 104, 138–146. [Google Scholar] [CrossRef]
- Kwan, M.M.; Lin, S.I.; Chen, C.H.; Close, J.C.; Lord, S.R. Sensorimotor function, balance abilities and pain influence Timed Up and Go performance in older community-living people. Aging Clin. Exp. Res. 2011, 23, 196–201. [Google Scholar] [CrossRef]
- Lusardi, M.; Pellecchia, G.; Schulman, M. Functional performance in community living older adults. J. Geriatr. Phys. Ther. 2003, 26, 14–22. [Google Scholar] [CrossRef]
- Fritz, S.; Lusardi, M. White paper: “Walking speed: The sixth vital sign”. J. Geriatr. Phys. Ther. 2009, 32, 46–49. [Google Scholar] [CrossRef]
- Tornero-Quiñones, I.; Sáez-Padilla, J.; Espina Díaz, A.; Abad Robles, M.T.; Sierra Robles, Á. Functional Ability, Frailty and Risk of Falls in the Elderly: Relations with Autonomy in Daily Living. Int. J. Environ. Res. Public Health 2020, 17, 1006. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Morishita, L.; Boult, C.; Ebbitt, B.; Rambel, M.; Fallstrom, K.; Gooden, T. Concurrent validity of administering the Geriatric Depression Scale and the physical functioning dimension of the SIP by telephone. J. Am. Geriatr. Soc. 1995, 43, 680–683. [Google Scholar] [CrossRef]
- Bohannon, R.W. Are hand-grip and knee extension strength reflective of common constructs? Percept. Mot. Ski. 2012, 114, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Amaral, C.A.; Amaral, T.L.M.; Monteiro, G.T.R.; Vasconcellos, M.T.L.; Portela, M.C. Hand grip strength: Reference values for adults and elderly people of Rio Branco, Acre, Brazil. PLoS ONE 2019, 14, e0211452. [Google Scholar] [CrossRef] [PubMed]
- Bean, J.F.; Leveille, S.G.; Kiely, D.K.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. A comparison of leg power and leg strength within the InCHIANTI study: Which influences mobility more? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2003, 58, M728–M733. [Google Scholar] [CrossRef]
- Izquierdo, M.; Ibañez, J.; Gorostiaga, E.; Garrues, M.; Zúñiga, A.; Antón, A.; Larrión, J.L.; Häkkinen, K. Maximal strength and power characteristics in isometric and dynamic actions of the upper and lower extremities in middle-aged and older men. Acta Physiol. Scand. 1999, 167, 57–68. [Google Scholar] [CrossRef]
- Herman, S.; Kiely, D.K.; Leveille, S.; O’Neill, E.; Cyberey, S.; Bean, J.F. Upper and lower limb muscle power relationships in mobility-limited older adults. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 476–480. [Google Scholar] [CrossRef]
- Stagsted, R.A.W.; Ramari, C.; Skjerbaek, A.G.; Thrue, C.; Dalgas, U.; Hvid, L.G. Lower extremity muscle power—A critical determinant of physical function in aging and multiple sclerosis. Exp. Gerontol. 2021, 150, 111347. [Google Scholar] [CrossRef]
- Alcazar, J.; Rodriguez-Lopez, C.; Ara, I.; Alfaro-Acha, A.; Mañas-Bote, A.; Guadalupe-Grau, A. The force-velocity relationship in older people: Reliability and validity of a systematic procedure. Int. J. Sports Med. 2017, 38, 1097–1104. [Google Scholar] [CrossRef]
- Lindemann, U.; Farahmand, P.; Klenk, J.; Blatzonis, K.; Becker, C. Validity of linear encoder measurement of sit-to-stand performance power in older people. Physiotherapy 2015, 101, 298–302. [Google Scholar] [CrossRef]
- Lohne-Seiler, H.; Torstveit, M.K.; Anderssen, S.A. Traditional versus functional strength training: Effects on muscle strength and power in the elderly. J. Aging Phys. Act. 2013, 21, 51–70. [Google Scholar] [CrossRef]
- Sayers, S.P. High-speed power training: A novel approach to resistance training in older men and women. A brief review and pilot study. J. Strength Cond. Res. 2007, 21, 518–526. [Google Scholar] [CrossRef]
- Hazell, T.; Kenno, K.; Jakobi, J. Functional benefit of power training for older adults. J. Aging Phys. Act. 2007, 15, 349–359. [Google Scholar] [CrossRef]
- Beaudart, C.; Rolland, Y.; Cruz-Jentoft, A.J.; Bauer, J.M.; Sieber, C.; Cooper, C.; Al-Daghri, N.; Araujo de Carvalho, I.; Bautmans, I.; Bernabei, R.; et al. Assessment of Muscle Function and Physical Performance in Daily Clinical Practice: A position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif. Tissue Int. 2019, 105, 1–14. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar] [CrossRef]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the reliability and validity of a shorter walk test compared with the 10-Meter Walk Test for measurements of gait speed in healthy, older adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef]
- Pophal da Silva, L.; Boneti-Moreira, N.; Barbosa de Freitas, P.; Pereira, G.; Rodacki, A.L.F. Gait Parameters of Older Adults according to Their Fall History and Functional Capacity While Walking at Different Speeds. Gerontology 2021, 67, 532–543. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Bouwstra, H.; Smit, E.B.; Wattel, E.M.; Van der Wouden, J.C.; Hertogh, C.M.; Terluin, B.; Terwee, C.B. Measurement Properties of the Barthel Index in Geriatric Rehabilitation. J. Am. Med. Dir. Assoc. 2019, 20, 420–425.e1. [Google Scholar] [CrossRef]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Labata-Lezaun, N.; Canet-Vintró, M.; López-De-Celis, C.; Rodríguez-Sanz, J.; Aiguadé, R.; Cuadra-Llopart, L.; Jovell-Fernández, E.; Bosch, J.; Pérez-Bellmunt, A. Effectiveness of a Multicomponent Training Program on Physical Performance and Muscle Quality in Older Adults: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2022, 20, 222. [Google Scholar] [CrossRef]
- Velasco, R.; Bejines, M.; Sánchez, R.; Mora, A.B.; Benítez, V.; García, L. Envejecimiento y capacidad funcional en adultos mayores institucionalizados del occidente de México. NURE Investig. Rev. Científica Enfermería 2015, 12, 1–11. [Google Scholar]
- Mañas, A.; del Pozo-Cruz, B.; García-García, F.J.; Guadalupe-Grau, A.; Ara, I. Role of objectively measured sedentary behavior in physical performance, frailty and mortality among older adults: A short systematic review. Eur. J. Sport Sci. 2017, 17, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Cid-Ruzafa, J.; Damián-Moreno, J. Valoración de la discapacidad física: El índice de Barthel [Disability evaluation: Barthel’s index]. Rev. Española Salud Pública 1997, 71, 127–137. Erratum in Rev. Española De Salud Pública 1997, 71, 411(In Spanish) [Google Scholar] [CrossRef]
- De Fátima Ribeiro Silva, C.; Ohara, D.G.; Matos, A.P.; Pinto, A.C.P.N.; Pegorari, M.S. Short Physical Performance Battery as a Measure of Physical Performance and Mortality Predictor in Older Adults: A Comprehensive Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 10612. [Google Scholar] [CrossRef]
- Boreskie, K.F.; Hay, J.L.; Boreskie, P.E.; Arora, R.C.; Duhamel, T.A. Frailty-aware care: Giving value to frailty assessment across different healthcare settings. BMC Geriatr. 2022, 22, 13. [Google Scholar] [CrossRef]
- Concha-Cisternas, Y.; Petermann-Rocha, F.; Castro-Piñero, J.; Parra, S.; Albala, C.; Wyngard, V.V.; Vásquez, J.; Cigarroa, I.; Celis-Morales, C. Fuerza de prensión manual. Un sencillo, pero fuerte predictor de salud en población adulta y personas mayores [Handgrip strength as a predictor of adverse health outcomes]. Rev. Médica Chile 2022, 150, 1075–1086. (In Spanish) [Google Scholar] [CrossRef]
- Labott, B.K.; Donath, L. Agility performance in healthy older adults is associated with handgrip strength and force development: Results from a 1-year randomized controlled trial. Eur. Geriatr. Med. 2023, 14, 547–555. [Google Scholar] [CrossRef]
- Gray, M.; Paulson, S. Developing a measure of muscular power during a functional task for older adults. BMC Geriatr. 2014, 14, 145. [Google Scholar] [CrossRef]
- Foldager, F.; Jørgensen, P.B.; Tønning, L.U.; Petersen, E.T.; Jakobsen, S.S.; Vainorius, D.; Homilius, M.; Hansen, T.B.; Stilling, M.; Mechlenburg, I. The relationship between muscle power, functional performance, accelerometer-based measurement of physical activity and patient-reported outcomes in patients with hip osteoarthritis: A cross-sectional study. Musculoskelet. Sci. Pract. 2022, 62, 102678. [Google Scholar] [CrossRef]
- Toosizadeh, N.; Wendel, C.; Hsu, C.H.; Zamrini, E.; Mohler, J. Frailty assessment in older adults using upper-extremity function: Index development. BMC Geriatr. 2017, 17, 117. [Google Scholar] [CrossRef]
- Lindemann, U.; Klenk, J.; Becker, C. Assessment of fatigability of older women during sit-to-stand performance. Aging Clin. Exp. Res. 2016, 28, 889–893. [Google Scholar] [CrossRef] [PubMed]
- Toosizadeh, N.; Joseph, B.; Heusser, M.R.; Jokar, T.O.; Mohler, J.; Phelan, H.A.; Najafi, B. Assessing Upper-Extremity Motion: An Innovative, Objective Method to Identify Frailty in Older Bed-Bound Trauma Patients. J. Am. Coll. Surg. 2016, 223, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Luc, B.A.; Murray, A.M.; Pietrosimone, B.G.; Tevald, M.A. The relationships between strength, power, and physical function in older adults with knee osteoarthritis. Osteoarthr. Cartil. 2013, 21, S276–S277. [Google Scholar] [CrossRef]
- Kozicka, I.; Kostka, T. Handgrip strength, quadriceps muscle power, and optimal shortening velocity roles in maintaining functional abilities in older adults living in a long-term care home: A 1-year follow-up study. Clin. Interv. Aging 2016, 11, 739–747. [Google Scholar] [CrossRef]
- Kang, G.E.; Naik, A.D.; Ghanta, R.K.; Rosengart, T.K.; Najafi, B. A Wrist-Worn Sensor-Derived Frailty Index Based on an Upper-Extremity Functional Test in Predicting Functional Mobility in Older Adults. Gerontology 2021, 67, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Bottaro, M.; Machado, S.N.; Nogueira, W.; Scales, R.; Veloso, J. Effect of high versus low-velocity resistance training on muscular fitness and functional performance in older men. Eur. J. Appl. Physiol. 2007, 99, 257–264. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD or n (%) |
|---|---|
| Sex | |
| Women | 35 (85.4%) |
| Men | 6 (14.6%) |
| Age (years) | 82.0 ± 9.6 |
| Height (cm) | 155.2 ± 9.1 |
| Weight | 66.5 ± 11.8 |
| Dominant Limb | |
| Right | 39 (95.1%) |
| Left | 2 (4.9%) |
| Variable | Mean ± SD or n (%) |
|---|---|
| Encoder EF (power) | 398.4 ± 291.6 |
| Handgrip (Kg) | 11.5 ± 8.4 |
| Barthel Index (points) | 84.4 ± 18.4 |
| Barthel | |
| Independent | 17 (41.5%) |
| Mildly independent | 20 (48.8%) |
| Moderately independent | 4 (9.8%) |
| SPPB (points) | 6.8 ± 4.4 |
| SPPB | |
| Good performance | 13 (39.4%) |
| Moderate performance | 5 (15.2%) |
| Poor Performance | 2 (6.1%) |
| Disabled | 13 (39.4%) |
| 4mWT (m/s) | 0.8 ± 0.6 |
| 4mWT | |
| No frailty | 10 (25.6%) |
| Frailty | 29 (75.5%) |
| TUG (points) | 22.2 ± 13.3 |
| TUG | |
| No risk of falling | 7 (17.9%) |
| Risk of falling | 13 (33.3%) |
| High risk of falling | 1 (48.7%) |
| Encoder | Handgrip | |||||
|---|---|---|---|---|---|---|
| Variable | n | Mean ± SD | p | n | Mean ± SD | p |
| Barthel | ||||||
| Independent | 17 | 549.47 ± 350 78 | 0.011 | 14 | 15.91 ± 9.97 | 0.006 |
| Mildly independent | 20 | 312.55 ± 187 15 | 18 | 7.29 ± 4.30 | ||
| Moderately independent | 4 | 185.50 ± 128.44 | 3 | 16.11 ± 7.71 | ||
| n = 41 | n = 35 | |||||
| SPPB | ||||||
| Good performance | 13 | 645.77 ± 367 13 | 0.010 | 11 | 17.81 ± 9.93 | 0.066 |
| Moderate performance | 5 | 400.00 ± 164.87 | 4 | 8.42 ± 5.10 | ||
| Poor performance | 2 | 437.00 ± 22.63 | 2 | 13.00 ± 1.41 | ||
| Disabled | 13 | 272.15 ± 138.82 | 11 | 8.61 ± 7.24 | ||
| n = 33 | n = 28 | |||||
| 4mWT | ||||||
| No frailty | 10 | 681.10 ± 400.38 | 0.000 | 8 | 20.30 ± 10.06 | 0.000 |
| Frailty | 29 | 308.10 ± 175.42 | 25 | 8.91 ± 5.49 | ||
| n = 39 | n = 33 | |||||
| TUG | ||||||
| No risk of falling | 7 | 788.71 ± 435.38 | 0.000 | 5 | 21.53 ± 12.36 | 0.001 |
| Risk of falling | 13 | 434.69 ± 161.19 | 11 | 13.96 ± 6.95 | ||
| High risk of falling | 19 | 240.74 ± 136.44 | 17 | 7.29 ± 3.99 | ||
| n = 39 | n = 33 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Rodríguez, S.; Jovell-Fernández, E.; Cuadra-Llopart, L.; Rodríguez-Sanz, J.; Labata-Lezaun, N.; López-de-Celis, C.; Bosch, J.; Pérez-Bellmunt, A. Correlation between Power Elbow Flexion and Physical Performance Test: A Potential Predictor for Assessing Physical Performance in Older Adults. J. Clin. Med. 2023, 12, 5560. https://doi.org/10.3390/jcm12175560
Rodríguez-Rodríguez S, Jovell-Fernández E, Cuadra-Llopart L, Rodríguez-Sanz J, Labata-Lezaun N, López-de-Celis C, Bosch J, Pérez-Bellmunt A. Correlation between Power Elbow Flexion and Physical Performance Test: A Potential Predictor for Assessing Physical Performance in Older Adults. Journal of Clinical Medicine. 2023; 12(17):5560. https://doi.org/10.3390/jcm12175560
Chicago/Turabian StyleRodríguez-Rodríguez, Sergi, Esther Jovell-Fernández, Leonor Cuadra-Llopart, Jacobo Rodríguez-Sanz, Noé Labata-Lezaun, Carlos López-de-Celis, Joan Bosch, and Albert Pérez-Bellmunt. 2023. "Correlation between Power Elbow Flexion and Physical Performance Test: A Potential Predictor for Assessing Physical Performance in Older Adults" Journal of Clinical Medicine 12, no. 17: 5560. https://doi.org/10.3390/jcm12175560







