Feasibility of Total Endovascular Repair of the Aorta in Patients with Acute Type A Aortic Dissection: Morphological Analysis of 119 Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort and Design
2.2. Endovascular Treatment Eligibility Criteria
- Endovascular Aortic Valve Replacement:Similar to TAVI/TAVR), a catheter would deliver a prosthetic valve to replace the patient’s aortic valve. This part of the procedure is already established and commonly performed for aortic stenosis.
- Endovascular Aortic Root and Ascending Aorta Replacement:This would be the most challenging part. The graft would need to be designed in such a way that it could be anchored securely without risking occlusion of the coronary arteries. It would also need to be constructed in a way that the coronary arteries could be reconnected to the graft.
- Coronary Ostia Reconnection:This remains a significant hurdle for an endovascular Bentall procedure. One potential solution would be some form of branched or fenestrated stent graft that has openings or branches aligned with the coronary ostia. Another option could be hybrid procedures where limited open surgery is used to connect the coronary arteries to the stent graft.
2.3. Data Collection
- Distance between ET and sinotubular junction (STJ).
- Length of ET.
- Diameter of aorta and of true and false lumen.
- Proximal and distal ascending aorta.
- Aortic arch.
- Possible distal landing zone.
- Length and diameter of the supra-aortic arteries.
- Diameter of the aortic annulus.
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
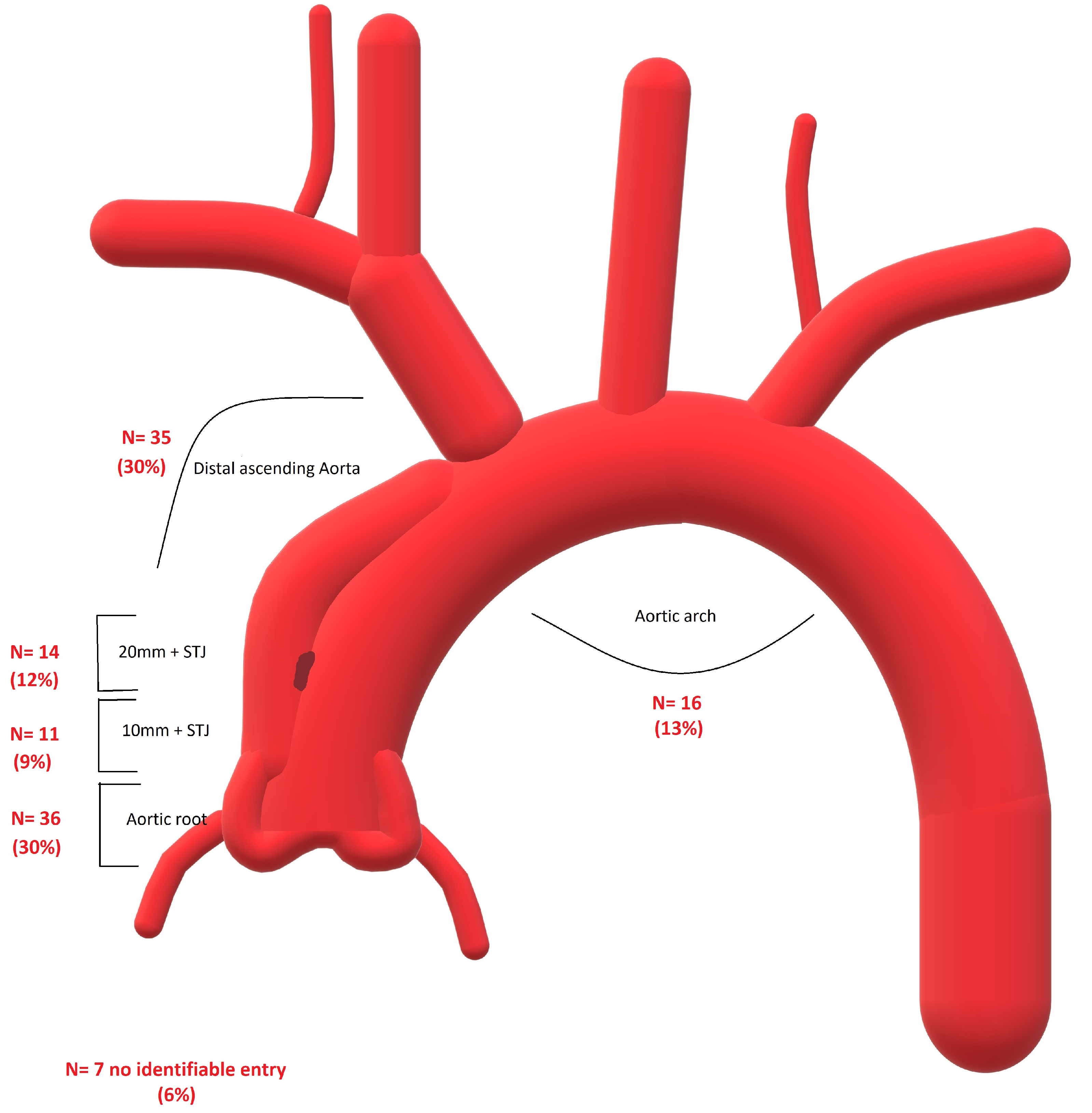
3.2. Entries’ Locations
3.3. Eligibility for Endovascular Treatment
3.4. Comparison between the Eligible and Noneligible Morphologies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wee, I.; Varughese, R.S.; Syn, N.; Choong, A. Non-operative Management of Type A Acute Aortic Syndromes: A Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2019, 58, 41–51. [Google Scholar] [CrossRef]
- Lau, C.; Robinson, N.B.; Farrington, W.J.; Rahouma, M.; Gambardella, I.; Gaudino, M.; Girardi, L.N. A tailored strategy for repair of acute type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2022, 164, 1698–1707. [Google Scholar] [CrossRef]
- Pape, L.A.; Awais, M.; Woznicki, E.M.; Suzuki, T.; Trimarchi, S.; Evangelista, A.; Myrmel, T.; Larsen, M.; Harris, K.M.; Greason, K.; et al. Presentation, Diagnosis, and Outcomes of Acute Aortic Dissection: 17-Year Trends From the International Registry of Acute Aortic Dissection. J. Am. Coll. Cardiol. 2015, 66, 350–358. [Google Scholar] [CrossRef]
- Rylski, B.; Milewski, R.K.; Bavaria, J.E.; Vallabhajosyula, P.; Moser, W.; Szeto, W.Y.; Desai, N.D. Long-term results of aggressive hemiarch replacement in 534 patients with type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2014, 148, 2981–2985. [Google Scholar] [CrossRef]
- Chiu, P.; Goldstone, A.B.; Schaffer, J.M.; Lingala, B.; Miller, D.C.; Mitchell, R.S.; Woo, Y.J.; Fischbein, M.P.; Dake, M.D. Endovascular Versus Open Repair of Intact Descending Thoracic Aortic Aneurysms. J. Am. Coll. Cardiol. 2019, 73, 643–651. [Google Scholar] [CrossRef]
- Howard, C.; Sheridan, J.; Picca, L.; Reza, S.; Smith, T.; Ponnapalli, A.; Calow, R.; Cross, O.; Iddawela, S.; George, M.; et al. TEVAR for complicated and uncomplicated type B aortic dissection—Systematic review and meta-analysis. J. Card. Surg. 2021, 36, 3820–3830. [Google Scholar] [CrossRef] [PubMed]
- Nienaber, C.A.; Kische, S.; Ince, H.; Fattori, R. Thoracic endovascular aneurysm repair for complicated type B aortic dissection. J. Vasc. Surg. 2011, 54, 1529–15333. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, W.; Liakopoulos, O.J.; Mylonas, S.; Wegner, M.; Brunkwall, J.; Dorweiler, B. Long-Term Outcomes after Thoracic Endovascular Aortic Repair Using Chimney Grafts for Aortic Arch Pathologies: 10 Years of Single-Center Experience. Ann. Vasc. Surg. 2021, 72, 400–408. [Google Scholar] [CrossRef] [PubMed]
- Shu, C.; Fan, B.; Luo, M.; Li, Q.; Fang, K.; Li, M.; Li, X.; He, H.; Wang, T.; Yang, C.; et al. Endovascular treatment for aortic arch pathologies: Chimney, on-the-table fenestration, and in-situ fenestration techniques. J. Thorac. Dis. 2020, 12, 1437–1448. [Google Scholar] [CrossRef]
- Tenorio, E.R.; Oderich, G.S.; Kölbel, T.; Dias, N.V.; Sonesson, B.; Karelis, A.; Farber, M.A.; Parodi, F.E.; Timaran, C.H.; Scott, C.K.; et al. Multicenter global early feasibility study to evaluate total endovascular arch repair using three-vessel inner branch stent-grafts for aneurysms and dissections. J. Vasc. Surg. 2021, 74, 1055–1065. [Google Scholar] [CrossRef] [PubMed]
- Tsilimparis, N.; Detter, C.; Law, Y.; Rohlffs, F.; Heidemann, F.; Brickwedel, J.; von Kodolitsch, Y.; Debus, E.S.; Kölbel, T. Single-center experience with an inner branched arch endograft. J. Vasc. Surg. 2019, 69, 977–985. [Google Scholar] [CrossRef]
- Verscheure, D.; Haulon, S.; Tsilimparis, N.; Resch, T.; Wanhainen, A.; Mani, K.; Dias, N.; Sobocinski, J.; Eagleton, M.; Ferreira, M.; et al. Endovascular Treatment of Post Type A Chronic Aortic Arch Dissection With a Branched Endograft: Early Results From a Retrospective International Multicenter Study. Ann. Surg. 2021, 273, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, W.; Wegner, M.; Dorweiler, B. Meta-analysis and meta-regression of the total endovascular aortic repair in aortic arch. VASA Z. Fur Gefasskrankh. 2023, 52, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Roselli, E.E.; Hasan, S.M.; Idrees, J.J.; Aftab, M.; Eagleton, M.J.; Menon, V.; Svensson, L.G. Inoperable patients with acute type A dissection: Are they candidates for endovascular repair? Interact. Cardiovasc. Thorac. Surg. 2017, 25, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Catalano, M.A.; Mamdouhi, T.; Pupovac, S.; Kennedy, K.F.; Brinster, D.R.; Hartman, A.; Yu, P.-J. Age, sex, and contemporary outcomes in surgical repair of type A aortic dissection: Insights from the National Inpatient Sample. JTCVS Open 2022, 11, 23–36. [Google Scholar] [CrossRef]
- Hauck, S.R.; Kupferthaler, A.; Stelzmüller, M.; Eilenberg, W.; Ehrlich, M.; Neumayer, C.; Wolf, F.; Loewe, C.; Funovics, M.A. Endovascular Stent-Graft Repair of the Ascending Aorta: Assessment of a Specific Novel Stent-Graft Design in Phantom, Cadaveric, and Clinical Application. Cardiovasc. Interv. Radiol. 2021, 44, 1448–1455. [Google Scholar] [CrossRef]
- Kreibich, M.; Soekeland, T.; Beyersdorf, F.; Bavaria, J.E.; Schröfel, H.; Czerny, M.; Rylski, B. Anatomic feasibility of an endovascular valve–carrying conduit for the treatment of type A aortic dissection. J. Thorac. Cardiovasc. Surg. 2019, 157, 26–34. [Google Scholar] [CrossRef]
- Ahmed, Y.; Houben, I.B.; Figueroa, C.A.; Burris, N.S.; Williams, D.M.; Moll, F.L.; Patel, H.J.; Herwaarden, J.A. Endovascular ascending aortic repair in type A dissection: A systematic review. J. Card. Surg. 2021, 36, 268–279. [Google Scholar] [CrossRef]
- e Melo, R.G.; Stana, J.; Prendes, C.F.; Kölbel, T.; Peterss, S.; Stavroulakis, K.; Rantner, B.; Pichlmaier, M.; Tsilimparis, N. Current state and future directions of endovascular ascending and arch repairs: The motion towards an endovascular Bentall procedure. Semin. Vasc. Surg. 2022, 35, 350–363. [Google Scholar] [CrossRef]
- Tsilimparis, N.; Debus, E.S.; Oderich, G.S.; Haulon, S.; Terp, K.A.; Roeder, B.; Detter, C.; Kölbel, T. International experience with endovascular therapy of the ascending aorta with a dedicated endograft. J. Vasc. Surg. 2016, 63, 1476–1482. [Google Scholar] [CrossRef]
- Kreibich, M.; Rylski, B.; Beyersdorf, F.; Siepe, M.; Czerny, M. Endo-Bentall for proximal aortic dissection: From conception to application. Asian Cardiovasc. Thorac. Ann. 2021, 29, 697–700. [Google Scholar] [CrossRef] [PubMed]
- Jakob, H.; Dohle, D.; Benedik, J.; Jánosi, R.A.; Schlosser, T.; Wendt, D.; Thielmann, M.; Erbel, R.; Tsagakis, K. Long-term experience with the E-vita Open hybrid graft in complex thoracic aortic diseasedagger. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2017, 51, 329–338. [Google Scholar]
- Liakopoulos, O.J.; Kroener, A.; Sabashnikov, A.; Zeriouh, M.; Ahmad, W.; Choi, Y.-H.; Wahlers, T. Single-center experience with the frozen elephant trunk procedure in 111 patients with complex aortic disease. J. Thorac. Dis. 2020, 12, 5387–5397. [Google Scholar] [CrossRef]
- Shrestha, M.; Martens, A.; Kaufeld, T.; Beckmann, E.; Bertele, S.; Krueger, H.; Neuser, J.; Fleissner, F.; Ius, F.; Abd Alhadi, F.; et al. Single-centre experience with the frozen elephant trunk technique in 251 patients over 15 years. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2017, 52, 858–866. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhou, Y.; Lin, S.; Xiao, J.; Ai, W.; Zhang, W.W. Systematic review and meta-analysis of association of prophylactic cerebrospinal fl uid drainage in preventing spinal cord ischemia following TEVAR. J Vasc Surg. 2021, 75, 1478–1489. [Google Scholar] [CrossRef] [PubMed]
- Tsilimparis, N.; Stana, J.; Konstantinou, N.; Chen, M.; Zhou, Q.; Kölbel, T. Identifying risk factors for early neurological outcomes following thoracic endovascular aortic repair using the SUMMIT database. Eur. J. Cardio-Thoracic Surg. 2021, 62, ezab476. [Google Scholar] [CrossRef]
- Ahmad, W.; Brunkwall, J.; Bunck, A.C.; Dorweiler, B.; Mylonas, S. Favorable Remodeling After TEVAR in Uncomplicated Acute and Subacute Type B Aortic Dissection in Comparison to Conservative Treatment: A Midterm Analysis. J. Endovasc. Ther. 2023, 15266028231158971. [Google Scholar] [CrossRef]
- Khoynezhad, A.; Donayre, C.E.; Walot, I.; Koopmann, M.C.; Kopchok, G.E.; White, R.A. Feasibility of endovascular repair of ascending aortic pathologies as part of an FDA-approved physician-sponsored investigational device exemption. J. Vasc. Surg. 2016, 63, 1483–1495. [Google Scholar] [CrossRef]
- Kern, M.; Hauck, S.R.; Dachs, T.M.; Haider, L.; Stelzmüller, M.E.; Ehrlich, M.; Loewe, C.; Funovics, M.A. Endovascular repair in type A aortic dissection: Anatomical candidacy for currently manufactured stent grafts and conceptual valve-carrying devices for an Endo-Bentall procedure. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2023, 63, ezad085. [Google Scholar] [CrossRef] [PubMed]

| Patient | Extension of Dissection * | Suggested Endovascular Procedure | Commentary | Entry Tear Location | DLZ |
|---|---|---|---|---|---|
| 1. | A11 | Endobental + B/FTEVAR + LSA Bp. | FL reaches aortic valve | Aortic Root | 4 |
| 2. | A11 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | Aortic Root | 4 |
| 3. | A11 | Endobental+ ChTEVAR BCT/LCCA + LSA Bp. | FL reaches aortic valve | 0–10 mm above STJ | 4 |
| 4. | A11 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | 0–10 mm above STJ | 4 |
| 5. | A11 | Endobental or: TEVAR + TAVI | FL reaches aortic valve | 10–20 mm above STJ | 5 |
| 6. | A11 | Endobental+ ChTEVAR BCT/LCCA + LSA Bp. | FL reaches aortic valve | 10–20 mm above STJ | 4 |
| 7. | A8 | Endobental + ChTEVAR + LSA-Bp. | FL reaches coronaries | 10–20 mm above STJ | 4 |
| 8. | A0 | Endobental till BCT | FL reaches aortic valve | 10–20 mm above STJ | 0 |
| 9. | A11 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | BCT | 4 |
| 10. | A10 | Endobental + ChTEVAR + LSA-Bp. | FL reaches coronaries | BCT | 4 |
| 11. | A9 | Endobental + ChTEVAR + LSA-Bp. | FL reaches coronaries | BCT | 3 |
| 12. | A11 | B/FTEVAR, ChTEVAR + LSA Bp. | LCCA | 4 | |
| 13. | A9 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | LCCA | 4 |
| 14. | B0 | BTEVAR + LSA Bp. | LSA | 5 | |
| 15. | A11 | B/FTEVAR or ChTEVAR (BCT + LCCA) + LSA Bp. | LSA | 5 | |
| 16. | A1 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | LSA | 2 |
| 17. | A11 | ChTEVAR + LSA-Bp. | LSA | 4 | |
| 18. | A2 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | LSA | 5 |
| 19. | A10 | Endobental + B/F TEVAR | FL reaches aortic valve | LSA | 5 |
| 20. | A0 | Endobental + TEVAR to BCT | FL reaches coronaries | 20 above STJ −20 before BCT | 0 |
| 21. | A9 | Endobental + ChTEVAR +LSA-Bp. | FL reaches aortic valve | 20 above STJ −20 before BCT | 4 |
| 22. | A0 | TEVAR 100 mm | 20 above STJ −20 before BCT | 0 | |
| 23. | A2 | TEVAR + BCT Periscope + RCCA-LCCA, LCCA-LSA Bps. | 20 above STJ −20 before BCT | 4 | |
| 24. | A2 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | 20 above STJ −20 before BCT | 3 |
| 25. | A10 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | 20 above STJ −20 before BCT | 4 |
| 26. | A2 | TEVAR 90 mm | 20 above STJ −20 before BCT | 0 | |
| 27. | A11 | BTEVAR + LSA Bp. | 20 above STJ −20 before BCT | 4 | |
| 28. | A0 | TEVAR 100 mm | 20 above STJ −20 before BCT | 0 | |
| 29. | A11 | B/FTEVAR, Debranching: LCCA-RCCA, Plug in BCT, TEVAR | 20 above STJ −20 before BCT | 1 | |
| 30. | A10 | Endobental + B/FTEVAR + LSA Bp. | FL reaches coronaries | 20 above STJ −20 before BCT | 5 |
| 31. | A3 | ChTEVAR in BCT + RCCA-LCCA Bp. No ness. LSA Bp. | 20 above STJ −20 before BCT | 4 | |
| 32. | A10 | Endobental | FL reaches coronaries | 20 above STJ −20 before BCT | |
| 33. | A9 | Endobental + ChTEVAR + LSA-Bp. | FL reaches aortic valve | 20 above STJ −20 before BCT | 4 |
| 34. | A0 | Endobental till BCT | FL reaches aortic valve | 20 above STJ −20 before BCT | 0 |
| 35. | A10 | Endobental + ChTEVAR (BCT/LCCA) + LSA Bp. | FL reaches aortic valve | 20 above STJ −20 before BCT | 4 |
| 36. | A9 | Endobental + ChTEVAR + LSA-Bp. | FL reaches coronaries | 20 above STJ −20 before BCT | 4 |
| Eligible n = 36 | Not Eligible n = 83 | p | |
|---|---|---|---|
| Diameter of the aortic annulus | 15 (4) | 15(4) | 0.619 |
| Distance highest coronary artery-STJ | 8 (3) | 7 (6) | 0.398 |
| Aortic diameter at STJ | 29 (6) | 32 (9) | 0.001 |
| Distance STJ–Entry | 36 (37) | 1 (22) | 0.001 |
| Distance STJ–BCT on the outer curve | 98 (13) | 102 (14) | 0.003 |
| Length of the entry tear | 12 (12) | 18 (16) | 0.023 |
| Diameter of TL at STJ | 28 (9) | 32 (20) | 0.034 |
| Diameter of TL at 10 above STJ | 28 (11) | 28 (30) | 0.286 |
| Diameter of TL at 20 above STJ | 26 (14) | 24 (34) | 0.928 |
| Diameter of FL at STJ | 18 (11) | 25 (18) | 0.001 |
| Diameter of FL at 10 above STJ | 24 (11) | 34 (18) | 0.001 |
| Diameter of FL at 20 above STJ | 27 (8) | 38 (15) | 0.001 |
| Length of the BCT | 30 (5) | 30 (5) | 0.232 |
| Diameter of the BCT | 18 (4) | 17 (4) | 0.110 |
| Diameter of the LCCA | 10 (8) | 10 (2) | 0.232 |
| Diameter of the LSA | 13 (2) | 13 (3) | 0.372 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ahmad, W.; Liebezeit-Sievert, M.; Wegner, M.; Alokhina, A.; Wahlers, T.; Dorweiler, B.; Luehr, M. Feasibility of Total Endovascular Repair of the Aorta in Patients with Acute Type A Aortic Dissection: Morphological Analysis of 119 Patients. J. Clin. Med. 2023, 12, 5615. https://doi.org/10.3390/jcm12175615
Ahmad W, Liebezeit-Sievert M, Wegner M, Alokhina A, Wahlers T, Dorweiler B, Luehr M. Feasibility of Total Endovascular Repair of the Aorta in Patients with Acute Type A Aortic Dissection: Morphological Analysis of 119 Patients. Journal of Clinical Medicine. 2023; 12(17):5615. https://doi.org/10.3390/jcm12175615
Chicago/Turabian StyleAhmad, Wael, Mark Liebezeit-Sievert, Moritz Wegner, Anastasiia Alokhina, Thorsten Wahlers, Bernhard Dorweiler, and Maximilian Luehr. 2023. "Feasibility of Total Endovascular Repair of the Aorta in Patients with Acute Type A Aortic Dissection: Morphological Analysis of 119 Patients" Journal of Clinical Medicine 12, no. 17: 5615. https://doi.org/10.3390/jcm12175615
APA StyleAhmad, W., Liebezeit-Sievert, M., Wegner, M., Alokhina, A., Wahlers, T., Dorweiler, B., & Luehr, M. (2023). Feasibility of Total Endovascular Repair of the Aorta in Patients with Acute Type A Aortic Dissection: Morphological Analysis of 119 Patients. Journal of Clinical Medicine, 12(17), 5615. https://doi.org/10.3390/jcm12175615







