Acromioclavicular Joint Lesions in Adolescents—A Systematic Review and Treatment Guidelines
Abstract
:1. Introduction
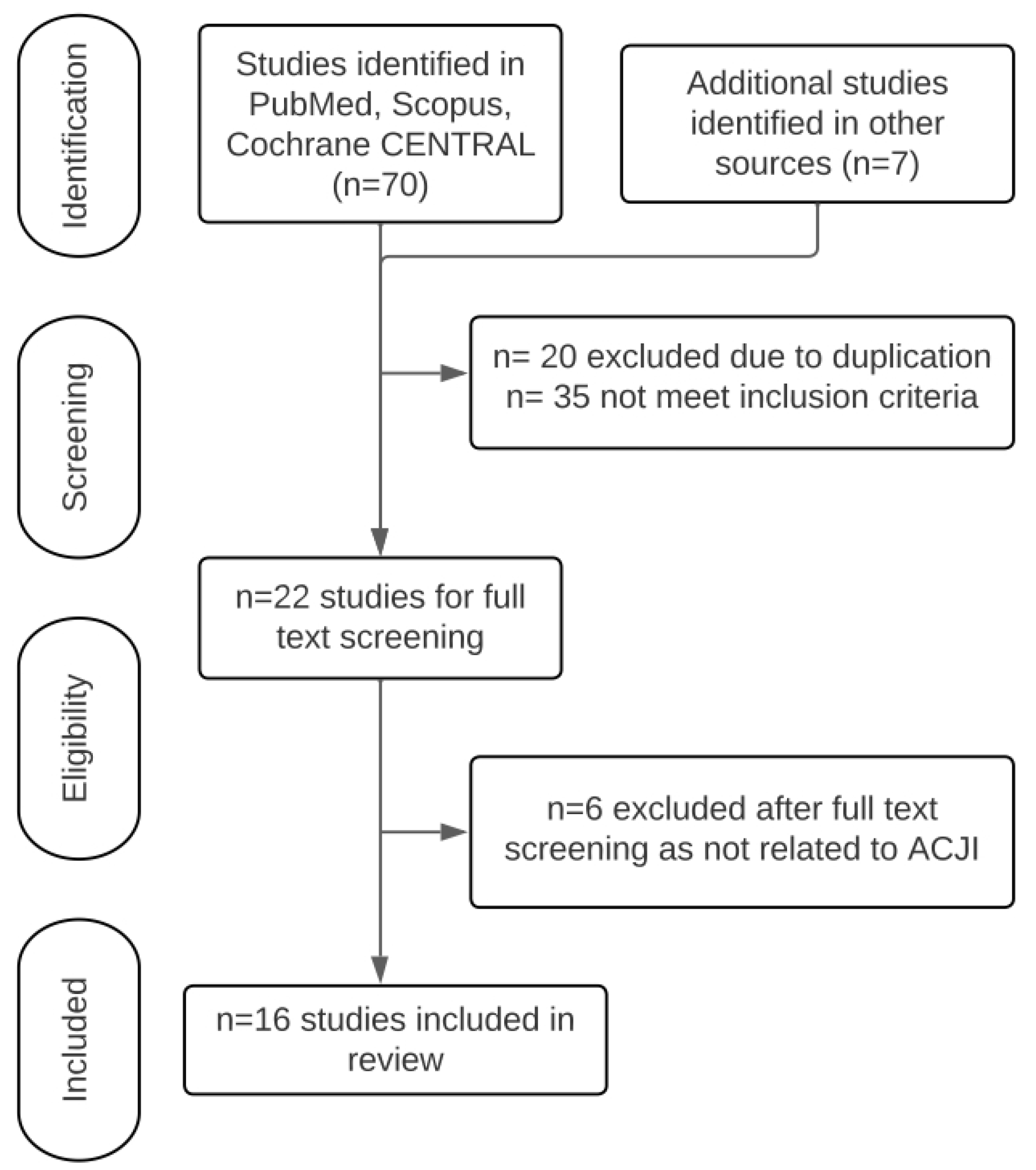
2. Materials and Methods
2.1. Study Question
2.2. Ethical Committee Clearance
2.3. Inclusion and Exclusion Criteria
2.4. Literature Search
2.5. Data Extraction
2.6. Quality Appraisal and Bias Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Appraisal and Bias Assessment
3.4. Patient Demographics (Table 1)
3.5. Imaging (Table 1)
3.6. Diagnosis (Table 1)
3.7. Intervention (Table 1)
3.8. Conservative Management (Table 1)
3.9. Outcome and Complications (Table 1)
3.10. Quantitative Synthesis of Data and Statistical Analysis
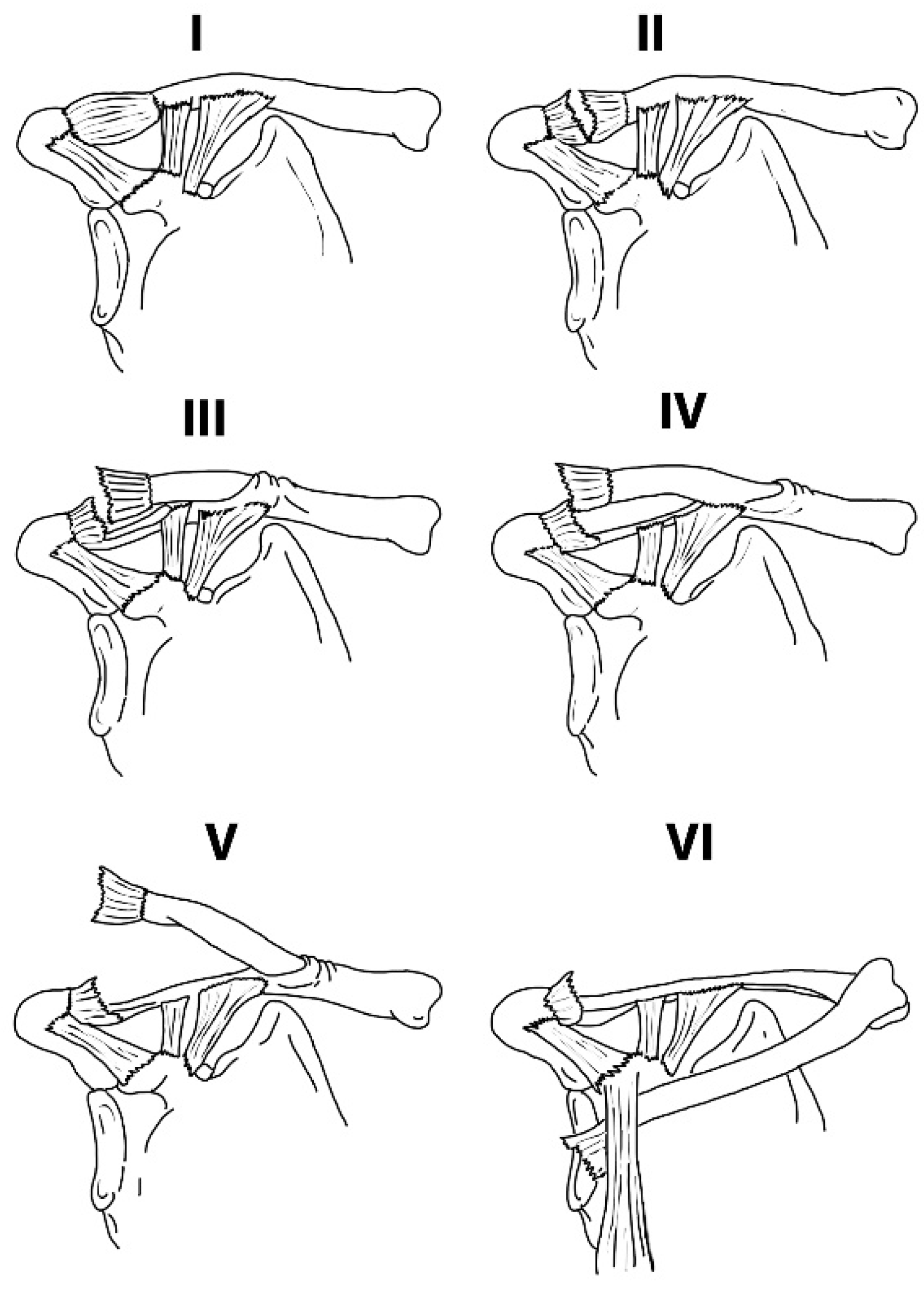
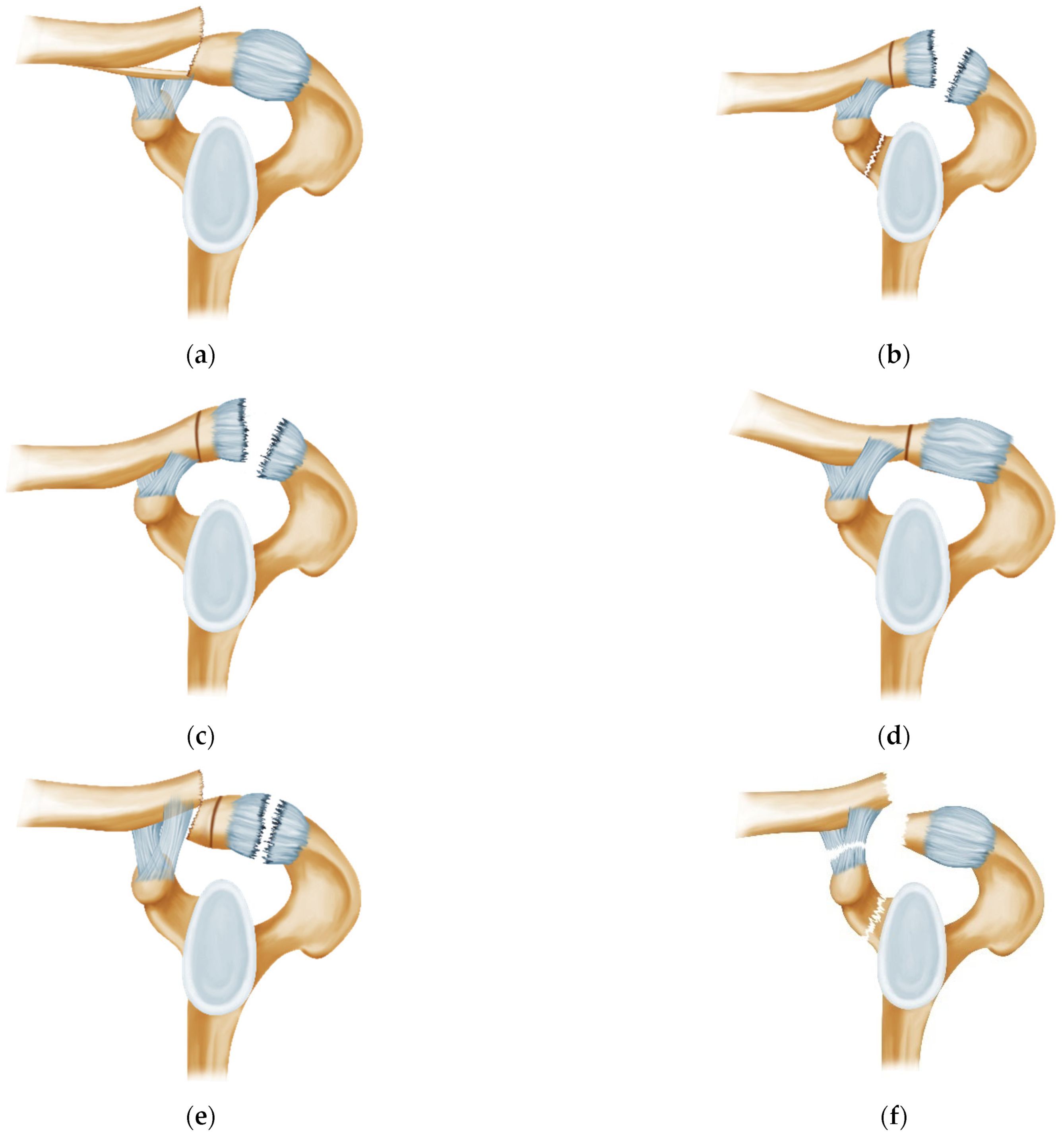
3.11. Categorization of the Injuries
- Type 1: Pseudo-dislocation of the AC joint (Figure 3a)
- Type 2: Coracoid fracture with ACJ dislocation (Figure 3b)
- Type 3: True dislocation of the ACJ (Figure 3c)
- Type 4: Voluntary atraumatic dislocation of the ACJ (Figure 3d)
- Type 5: Distal Clavicle fracture with true ACJ dislocation (Figure 3e)
- Type 6: “Triple Injury”: Coracoid fracture with pseudo-dislocation of ACJ with CC ligament rupture (Figure 3f)
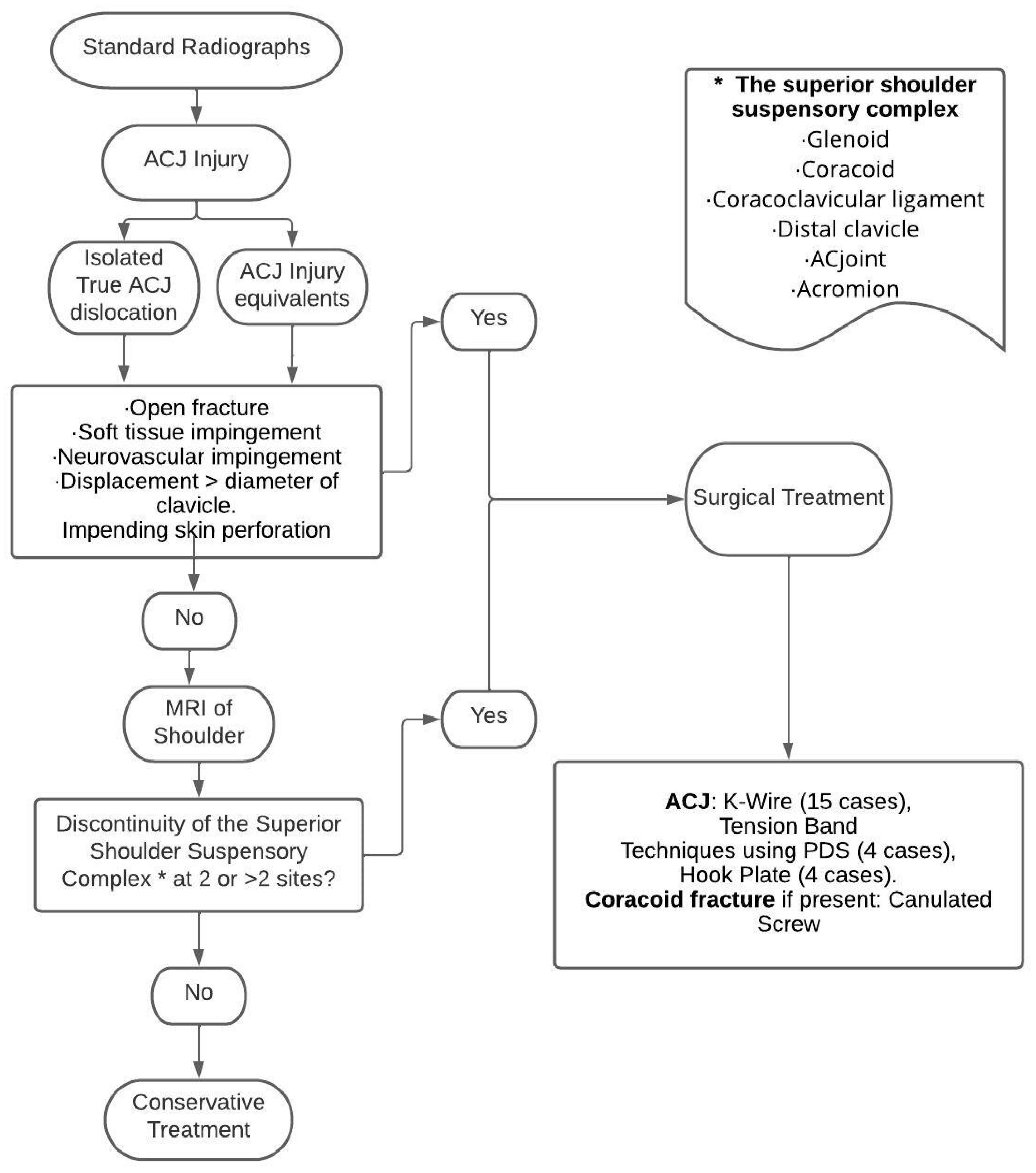
3.12. Development of the Management Algorithm
4. Discussion
4.1. The Existing Classification and Its Shortcomings
4.2. The New Categorization of AC Joint Injuries According to Frequency of Occurence
- Type 1: Pseudo-dislocation of the AC joint (Figure 3a)
- Type 2: Coracoid fracture with ACJ dislocation (Figure 3b)
- Type 4: Voluntary atraumatic dislocation of the ACJ (Figure 3d)
- Type 5: Distal Clavicle fracture with true ACJ dislocation (Figure 3e)
- Type 6: “Triple Injury”: Coracoid fracture with pseudo-dislocation of ACJ with CC ligament rupture (Figure 3f)
4.3. Management Algorithm (Figure 4)
4.4. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hippocrates. “Part XIII,”. In On the Articulations; Good Press: Glasgow, UK, 2021. [Google Scholar]
- Havránek, P. Injuries of Distal clavicular physis in children. J. Pediatr. Orthop. B 1989, 9, 213–215. [Google Scholar] [CrossRef]
- Nenopoulos, S.P.; Gigis, I.P.; Chytas, A.A.; Beslikas, T.A.; Nenopoulos, A.S.; Christoforidis, J.E. Outcome of distal clavicular fracture separations and dislocations in immature skeleton. Injury 2011, 42, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Sirin, E.; Aydin, N.; Topkar, O.M. Acromioclavicular joint injuries: Diagnosis, classification and ligamentoplasty procedures. EFORT Open Rev. 2018, 3, 426–433. [Google Scholar] [CrossRef]
- Beitzel, K.; Cote, M.P.; Apostolakos, J.; Solovyova, O.; Judson, C.H.; Ziegler, C.G.; Edgar, C.M.; Imhoff, A.B.; Arciero, R.A.; Mazzocca, A.D. Current Concepts in the Treatment of Acromioclavicular Joint Dislocations. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 387–397. [Google Scholar] [CrossRef] [PubMed]
- Eidman, D.K.; Siff, S.J.; Tullos, H.S. Acromioclavicular lesions in children. Am. J. Sport. Med. 1981, 9, 150–154. [Google Scholar] [CrossRef]
- Kraus, R.; Zwingmann, J.; Jablonski, M.; Bakir, M.S. Dislocations of the acromioclavicular and sternoclavicular joint in children and adolescents: A retrospective clinical study and big data analysis of routine data. PLoS ONE 2020, 15, e0244209. [Google Scholar] [CrossRef]
- Black, G.B.; McPherson, J.A.; Reed, M.H. Traumatic pseudodislocation of the acromioclavicular joint in children: A fifteen year review. Am. J. Sport. Med. 1991, 19, 644–646. [Google Scholar] [CrossRef]
- Sarwark, J.F.; King, E.C.; Luhmann, S.J. Proximal humerus, scapula and clavicle. In Rockwood and Wilkins Frac-Tures in Children, 6th ed.; Beaty, J.A., Kasser, J.R., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 2006. [Google Scholar]
- Pendleton, A.M.; Kocher, M.S. Shoulder Injuries in Pediatric Athletes. In Sports Injuries; Doral, M.N., Karlsson, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 1–15. [Google Scholar] [CrossRef]
- Owens, B.D.; Goss, T.P. The floating shoulder. J. Bone Jt. Surg. 2006, 88, 1419–1424. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Évid. Synth. 2019, 18, 2127–2133. [Google Scholar] [CrossRef]
- Porritt, K.; Gomersall, J.; Lockwood, C. JBI’s Systematic Reviews: Study Selection and Critical Appraisal. AJN Am. J. Nurs. 2014, 114, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Rashid, A.; Christofi, T.; Thomas, M. Surgical treatment of physeal injuries of the lateral aspect of the clavicle: A case series. Bone Jt. J. 2013, 95-B, 664–667. [Google Scholar] [CrossRef]
- Richards, D.P.; Howard, A. Distal Clavicle Fracture Mimicking Type IV Acromioclavicular Joint Injury in the Skeletally Immature Athlete. Clin. J. Sport Med. 2001, 11, 57–59. [Google Scholar] [CrossRef] [PubMed]
- Kirkos, J.M.; Papavasiliou, K.A.; Sarris, I.K.; Kapetanos, G.A. A Rare Acromioclavicular Joint Injury in a Twelve-Year-Old Boy: A Case Report. J. Bone Jt. Surg. 2007, 89, 2504–2507. [Google Scholar] [CrossRef]
- Kotb, A.; Yong, T.; Abdelgawad, A. A Posteriorly Displaced Distal Metaphyseal Clavicular Fracture (Type IV AC Joint Dislocation-Like) in Children: A Case Report and Literature Review Study. Case Rep. Orthop. 2016, 2016, 4015212. [Google Scholar] [CrossRef] [PubMed]
- Aebischer, A.S.; Sarai, H.; Wall, C.J. Distal Clavicle Physeal Separation Mimicking an Acromioclavicular Joint Separation: A Case Report. J. Bone Jt. Surg. 2021, 11, e20. [Google Scholar] [CrossRef]
- Gustavo Costa Rios, H.M.G. A Rare Case of a Distal Clavicle Fracture Type IV-Like Acromioclavicular Joint Injury in A Child: Case Report and Literature Review. J. Orthop. Ther. 2017. [Google Scholar]
- Pedersen, V.; Prall, W.C.; Ockert, B.; Haasters, F. Non-operative treatment of a fracture to the coracoid process with acromioclavicular dislocation in an adolescent. Orthop. Rev. 2014, 6, 5499. [Google Scholar] [CrossRef]
- Mondori, T.; Nakagawa, Y.; Kurata, S.; Fujii, S.; Egawa, T.; Inoue, K.; Tanaka, Y. New System for the Classification of Epiphyseal Separation of the Coracoid Process: Evaluation of Nine Cases and Review of the Literature. Adv. Orthop. 2020, 2020, 9749515. [Google Scholar] [CrossRef]
- DiPaola, M.; Marchetto, P. Coracoid process fracture with acromioclavicular joint separation in an American football player: A case report and literature review. Am. J. Orthop. 2009, 38, 37–39. [Google Scholar]
- Kubiak, R.; Slongo, T. Operative treatment of clavicle fractures in children: A review of 21 years. J. Pediatr. Orthop. 2002, 22, 736–739. [Google Scholar] [CrossRef]
- Jettoo, P.; de Kiewiet, G.; England, S. Base of coracoid process fracture with acromioclavicular dislocation in a child. J. Orthop. Surg. Res. 2010, 5, 77. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, N.; Haen, P.S.; Onstenk, R. Atraumatic Acromioclavicular Dislocation: A Case Report and Review of the Literature. Case Rep. Orthop. 2017, 2017, 8450538. [Google Scholar] [CrossRef] [PubMed]
- Barchick, S.R.; Otte, R.S.; Garrigues, G.E. Voluntary acromioclavicular joint dislocation: A case report and literature review. J. Shoulder Elb. Surg. 2019, 28, e238–e244. [Google Scholar] [CrossRef]
- Acharya, A.; Garg, N.; Bruce, C. Unusual fracture dislocation of the distal end of clavicle in an adolescent. Injury 2003, 34, 467–470. [Google Scholar] [CrossRef]
- Duerr, R.A.; Melvin, P.R.; Phillips, D.J. Acromioclavicular ‘Pseudo-dislocation’ with Concomitant Cora-coid Process Fracture and Coracoclavicular Ligament Rupture in a 12-year-old Male. Orthop. J. Harv. Med. Sch. 2018, 19, 52–57. [Google Scholar]
- Goss, T.P. Double Disruptions of the Superior Shoulder Suspensory Complex. J. Orthop. Trauma 1993, 7, 99–106. [Google Scholar] [CrossRef] [PubMed]
| Study | Study Design | Participant Characteristics | Categories | Imaging | Intervention | Reason for Intervention | Outcome and Follow-Up (FU) |
|---|---|---|---|---|---|---|---|
| Rashid et al. [15] UK | Case series Retrospective analysis | n = 5, mean age = 12.8 years (9–14), 4 males, 1 female ACJ Pseudo-dislocation | Type 1 | X-rays AP | ORIF (n = 4): Tension band technique using PDS Non-operative (n = 1) | High-grade injuries with displacement | Excellent clinical and radiological outcome. FU: 26 months |
| Richards and Howard [16] Canada | Case report | 13-year-old male Distal Clavicle fracture ACJ Pseudo-dislocation | Type 1 | X-ray—AP and Axillary views CT scan | Closed reduction under sedation | Soft tissue impingement | Return to competitive sports. FU: 12 weeks |
| Kirkos et al. [17] Greece | Case report | 12-year-old male Distal clavicle fracture ACJ Pseudo-dislocation | Type 1 | X-ray—AP view MRI | ORIF: 2 K-wires and nonabsorbable sutures | High-grade injury with suspected ligamentous disruption | Full ROM FU: 2 years |
| Kotb et al. [18] USA | Case report | 11-year-old male Distal clavicle fracture ACJ Pseudo-dislocation | Type 1 | X-ray AP view CT scan | ORIF: 3 K-wires | Clinical deformity High-grade injury | Return to full activity. FU: 8 weeks |
| Aebischer et al. [19] Australia | Case report | 9-year-old male Distal clavicle fracture ACJ Pseudo-dislocation | Type 1 | X-ray AP view | ORIF: 2 K-wires | Clinical and radiographic deformity | Return to sports. FU: 18 months |
| Goncalves et al. [20] Brazil | Case report | 13-year-old girl. ACJ Pseudo-dislocation | Type 1 | X-ray AP view of left shoulder | ORIF using K wire | Deformity, Soft tissue entrapment | Excellent outcome at FU of 3 months |
| Pedersen et al. [21] Germany | Case report | 14-year-old male Coracoid fracture with ACJ dislocation | Type 2 | CT scan MRI | Non-operative | Intact ACJ capsule, ligaments and CC ligaments | Return to sports at 12 weeks. FU: 5 months |
| Mondori et al. [22] Japan | Case series Retrospective analysis | 9 coracoid fractures, n = 7 associated with ACJ dislocation in 6 males and 1 female, mean age = 14.5 years (11 to 17) | Type 2 | X-ray and 3D- CT scan | ORIF (n = 3) Non operative (n = 4) | Unstable injury pattern. Conservative management performed only in patients who refused surgery | Excellent outcome. FU: 1 year |
| DiPaola and Marchetto [23] USA | Case report | 15-year-old male with fracture of coracoid and ACJ dislocation | Type 2 | AP, Lateral and Axillary X-ray of both shoulders | Non operative | Stable injury pattern with minimal displacement of coracoid | Excellent outcome. FU: 8 weeks |
| Kubiak and Slongo [24] Switzerland | Case series Retrospective analysis | 15 clavicle fractures n = 1 patient (11-year-old male) had ACJ dislocation with clavicle fracture. n = 4 ACJ Pseudo-dislocation | Type 5 (n = 1) Type 1 (n = 4) | X-ray AP view | ORIF (n = 5) K-wire = 3 cases Osseous suture = 2 cases | Soft tissue /muscle impingement in 4 cases Shortening of shoulder girdle in 1 case | Individual FU and implant removal time not mentioned. Median FU for 15 patients was 88 days |
| Jettoo et al. [25] United Kingdom | Case report | 12-year-old male Coracoid fracture with ACJ dislocation | Type 2 | X-ray AP view CT scan | ORIF: 2 threaded half pins for ACJ and screw fixation for coracoid | Early mobilization | Full range of motion at 5 months, return to normal activities at 9 months |
| Kraus et al. [7] Germany | Case series Retrospective analysis 7 trauma centers | n = 7, mean age = 14.5 years (13 to 17), all males True ACJ dislocation | Type 3 | Not mentioned | ORIF (n = 6): 4 Hook-plates and 2 K-wires. Arthroscopic procedure (n = 1): Tight rope | All high-grade injuries | No limitation of range of movement. FU: 6 weeks to 6 months |
| Sadeghi et al. [26] Netherlands | Case report | 17-year-old female Voluntary dislocation of the ACJ | Type 4 | X-ray, CT scan MRI arthrogram | Non-operative | Young age and minor complaints | Sub-optimum recovery at 1 year FU |
| Barchick et al. [27] USA | Case report | 15-year-old female Voluntary dislocation of bilateral ACJ | Type 4 | MRI Arthrogram right shoulder. No imaging for left | Arthroscopic augmentation of ACJ in right shoulder (n = 1) Non-operative for left (n = 1) | Pain and decreased function for right. No comment on left | Right: Poor outcome at 6 months Left: not mentioned |
| Acharya et al. [28] United Kingdom | Case report | 12-year-old male Distal clavicle fracture with ACJ dislocation | Type 5 | X-ray AP view CT scan | ORIF using k-wire | Unusual fracture pattern with unstable ACJ | Full functional recovery. Hypertrophic Scar FU: 1 year |
| Duerr et al. [29] USA | Case report | 12-year-old male with ‘Triple Injury’. Coracoid fracture, CC ligaments avulsion and ACJ Pseudo-dislocation | Type 6 | X-ray AP views of both shoulders | ORIF using Screw for coracoid, transosseous FiberWire sutures for ACJ and Suture Tak anchors (Arthrex) for CC ligaments | Triple injury with disruption of the SSSC | Excellent with return to sports at 1 year |
| Checklist Questions | Richards Howards [16] | Acharya et al. [28] | Sadeghi et al. [26] | Barchick et al. [27] | Pedersen et al. [21] | Jettoo et al. [25] | Kirkos et al. [17] | Kotb et al. [18] | Aebischer et al. [19] | DiPaola and Marchetto [23] | Duerr et al. [29] | Goncalves et al. [29] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Were the patient’s demographic characteristics clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 2.Was the patient’s history clearly described and presented as a timeline? | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 3.Was the current clinical condition of the patient on presentation clearly described? | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 4.Were diagnostic tests or assessment methods and the results clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 5.Was the intervention(s) or treatment procedure(s) clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6. Was the post-intervention clinical condition clearly described? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7.Were adverse events (harms) or unanticipated events identified and described? | No | Yes | Yes | Yes | No | No | No | No | No | No | No | No |
| 8. Does the case report provide takeaway lessons? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Checklist Questions | Kraus et al. [7] | Kubiak and Slongo [24] | Mondori et al. [22] | Rashid et al. [15] |
|---|---|---|---|---|
| 1. Were there clear criteria for inclusion in the case series? | Unclear | Yes | Yes | Yes |
| 2. Was the condition measured in a standard, reliable way for all participants included in the series? | Yes | Yes | Yes | Yes |
| 3. Were valid methods used for the identification of the condition for all participants included? | Yes | Yes | Yes | Yes |
| 4. Did the case series have consecutive inclusion of participants? | Yes | Yes | Yes | Yes |
| 5. Did the case series have complete inclusion of participants? | Yes | Yes | Yes | Yes |
| 6. Was there clear reporting of the demographics of the participants in the study? | Yes | Yes | Yes | Yes |
| 7. Was there clear reporting of the clinical information of the participants? | Yes | Yes | Yes | Yes |
| 8. Were the outcomes or follow-up results of cases clearly reported? | Yes | Yes | Yes | Yes |
| 9. Was there clear reporting of the presenting site(s)/clinic(s) demographic information? | Yes | Yes | Yes | Yes |
| 10. Was the statistical analysis appropriate? | Yes | Yes | Yes | Yes |
| Types | Description | Disruption of the SSSC at | Total Cases | Operated |
|---|---|---|---|---|
| Type 1 | Pseudo-dislocation of the AC joint | 1 site (AC joint) | 14 | 12 |
| Type 2 | Coracoid fracture with AC joint dislocation | 2 sites (coracoid and AC joint) | 10 | 4 |
| Type 3 | Isolated true dislocation of the AC joint | 1 site (AC joint) | 7 | 7 |
| Type 4 | Voluntary atraumatic dislocation | 1 site (AC joint) | 3 | 1 |
| Type 5 | Distal clavicle fracture with AC joint dislocation | 2 sites (Clavicle and AC joint) | 2 | 2 |
| Type 6 | Triple Injury (coracoid fracture, CC ligament rupture, AC joint dislocation) | 3 sites (Coracoid, CC ligaments and AC joint) | 1 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wahal, N.; Kendirci, A.S.; Abondano, C.; Tauber, M.; Martetschläger, F. Acromioclavicular Joint Lesions in Adolescents—A Systematic Review and Treatment Guidelines. J. Clin. Med. 2023, 12, 5650. https://doi.org/10.3390/jcm12175650
Wahal N, Kendirci AS, Abondano C, Tauber M, Martetschläger F. Acromioclavicular Joint Lesions in Adolescents—A Systematic Review and Treatment Guidelines. Journal of Clinical Medicine. 2023; 12(17):5650. https://doi.org/10.3390/jcm12175650
Chicago/Turabian StyleWahal, Naman, Alper Sukru Kendirci, Carlos Abondano, Mark Tauber, and Frank Martetschläger. 2023. "Acromioclavicular Joint Lesions in Adolescents—A Systematic Review and Treatment Guidelines" Journal of Clinical Medicine 12, no. 17: 5650. https://doi.org/10.3390/jcm12175650
APA StyleWahal, N., Kendirci, A. S., Abondano, C., Tauber, M., & Martetschläger, F. (2023). Acromioclavicular Joint Lesions in Adolescents—A Systematic Review and Treatment Guidelines. Journal of Clinical Medicine, 12(17), 5650. https://doi.org/10.3390/jcm12175650





