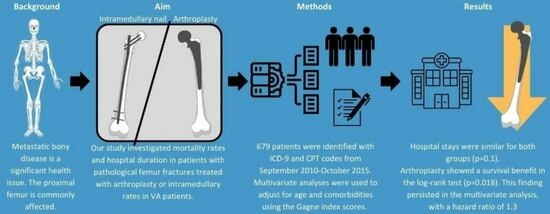
Arthroplasty for Treating Proximal Femur Metastatic Lesions May Be Associated with Lower Mortality Rates Compared to Intramedullary Nailing within the VA Healthcare System
Abstract
Share and Cite
Lam, P.W.; Putnam, D.; Mayeda, M.M.S.; Gundle, K.R. Arthroplasty for Treating Proximal Femur Metastatic Lesions May Be Associated with Lower Mortality Rates Compared to Intramedullary Nailing within the VA Healthcare System. J. Clin. Med. 2023, 12, 5717. https://doi.org/10.3390/jcm12175717
Lam PW, Putnam D, Mayeda MMS, Gundle KR. Arthroplasty for Treating Proximal Femur Metastatic Lesions May Be Associated with Lower Mortality Rates Compared to Intramedullary Nailing within the VA Healthcare System. Journal of Clinical Medicine. 2023; 12(17):5717. https://doi.org/10.3390/jcm12175717
Chicago/Turabian StyleLam, Phillip W., David Putnam, Marissa M. Song Mayeda, and Kenneth R. Gundle. 2023. "Arthroplasty for Treating Proximal Femur Metastatic Lesions May Be Associated with Lower Mortality Rates Compared to Intramedullary Nailing within the VA Healthcare System" Journal of Clinical Medicine 12, no. 17: 5717. https://doi.org/10.3390/jcm12175717
APA StyleLam, P. W., Putnam, D., Mayeda, M. M. S., & Gundle, K. R. (2023). Arthroplasty for Treating Proximal Femur Metastatic Lesions May Be Associated with Lower Mortality Rates Compared to Intramedullary Nailing within the VA Healthcare System. Journal of Clinical Medicine, 12(17), 5717. https://doi.org/10.3390/jcm12175717