Mapping the Path to Cognitive Balance: Applying the States of Mind Model and Network Analysis to Eating Disorder Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Inclusion Criteria
2.2. Procedures
2.3. Instruments
2.4. Statistical Analyses
2.4.1. Network Estimation
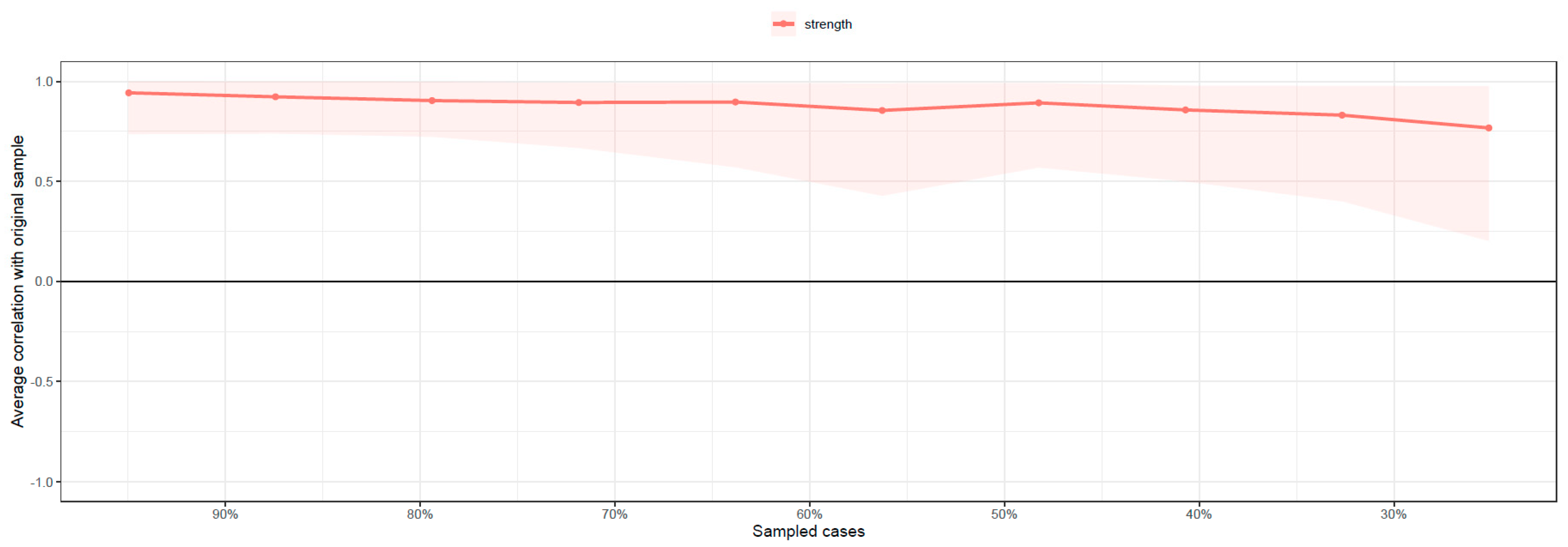
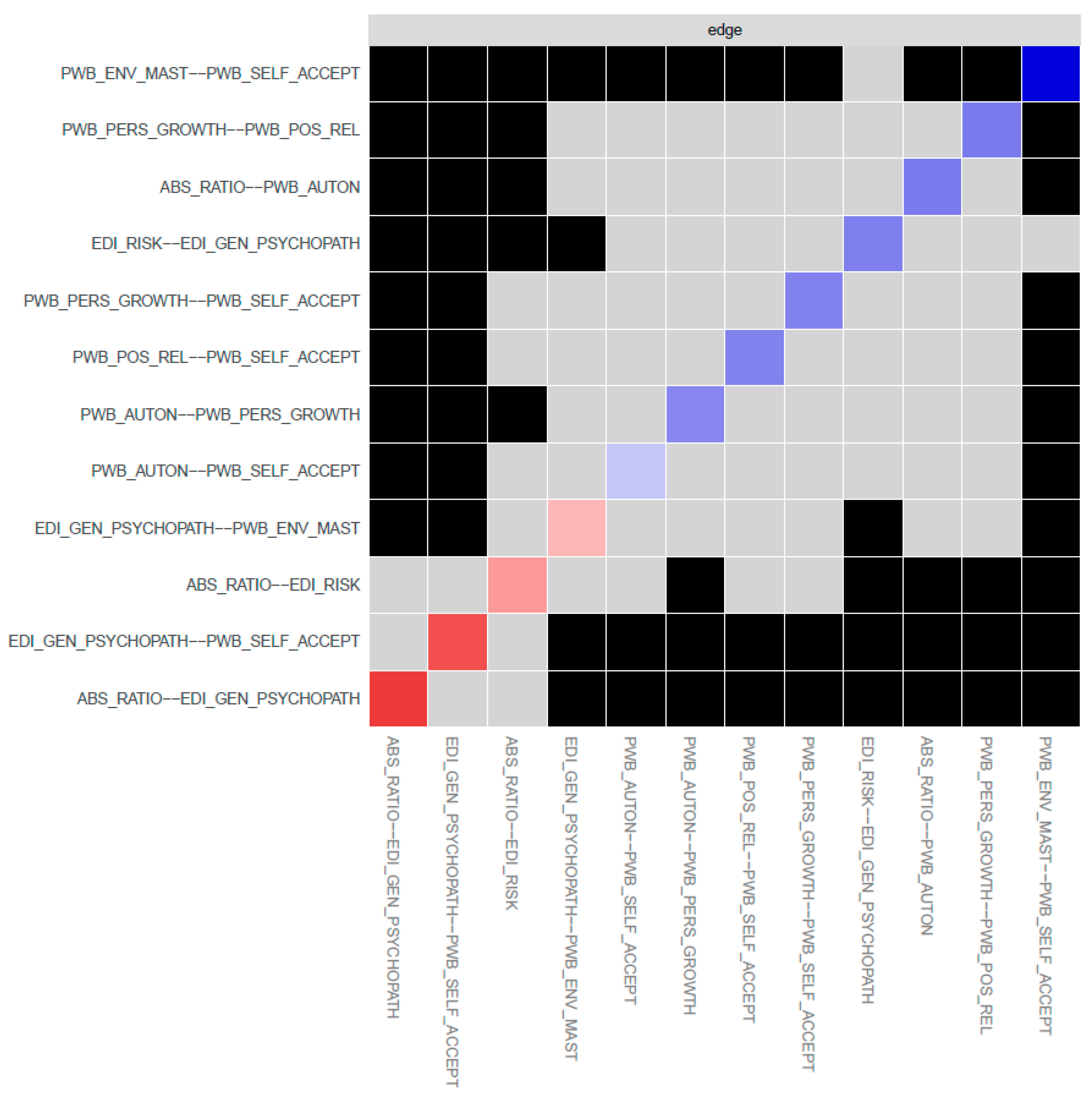
2.4.2. Network Accuracy
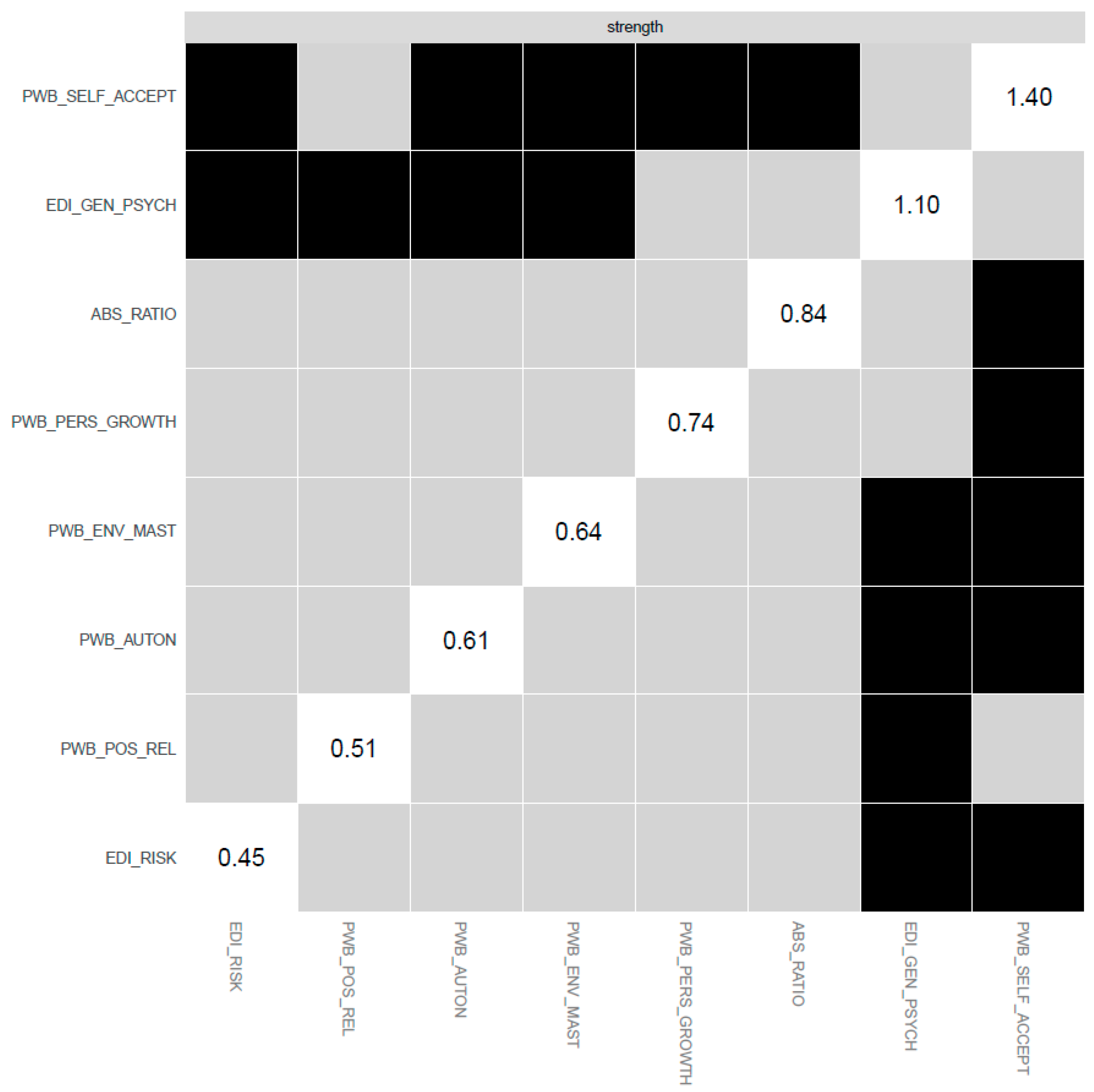
2.4.3. Centrality Indices
3. Results
3.1. Patient Sample Characteristics
3.2. Control Sample Characteristics
3.3. Mean Scores of ED Patients in Psychological Measures and T-Test Comparisons in SOM Ratios and Rational Beliefs between ED Patients and Controls
3.4. Network Analysis with SOM, ED Symptomatology, and Psychological Well-Being
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Treatment of Patients with Eating Disorders, third edition. Am. J. Psychiatry 2006, 163, 4–54. [Google Scholar]
- National Health Service. National Institute for Clinical Excellence (NICE) Clinical Guideline for Eating Disorders; National Institute for Clinical Excellence: London, UK, 2017. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Dahlgren, C.L.; Stedal, K.; Rø, Ø. Eating Disorder Examination Questionnaire (EDE-Q) and Clinical Impairment Assessment (CIA): Clinical norms and functional impairment in male and female adults with eating disorders. Nord. J. Psychiatry 2017, 71, 256–261. [Google Scholar] [CrossRef] [PubMed]
- Güler, K.; Özgörüş, Z. Investigation of the relationship between early maladaptive schemas, temperament and eating attitude in adults. J. Eat. Disord. 2022, 10, 187. [Google Scholar] [CrossRef] [PubMed]
- Shorey, R.C.; Anderson, S.E.; Stuart, G.L. Gender Differences in Early Maladaptive Schemas in a Treatment-Seeking Sample of Alcohol-Dependent Adults. Subst. Use Misuse 2012, 47, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Alimoradi, Z.; Zarabadipour, S.; Arrato, N.A.; Griffiths, M.D.; Andersen, B.L.; Bahrami, N. The relationship between cognitive schemas activated in sexual context and early maladaptive schemas among married women of childbearing age. BMC Psychol. 2022, 10, 131. [Google Scholar] [CrossRef] [PubMed]
- Najafabadi, Z.P.; Alibeigi, N.; Eskandarnia, E. Comparison of cognitive and emotional schema in women with and without marital satisfaction. World J. Adv. Res. Rev. 2021, 12, 056–065. [Google Scholar] [CrossRef]
- Anderson, D.A.; Maloney, K.C. The efficacy of cognitive–behavioral therapy on the core symptoms of bulimia nervosa. Clin. Psychol. Rev. 2001, 21, 971–988. [Google Scholar] [CrossRef]
- Cooper, M.; Cohen-Tovée, E.; Todd, G.; Wells, A.; Tovée, M. The Eating Disorder Belief Questionnaire: Preliminary development. Behav. Res. Ther. 1997, 35, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.J.; Rose, K.S.; Turner, H. Core beliefs and the presence or absence of eating disorder symptoms and depressive symptoms in adolescent girls. Int. J. Eat. Disord. 2005, 39, 60–64. [Google Scholar] [CrossRef]
- del Pozo, M.A.; Harbeck, S.; Zahn, S.; Kliem, S.; Kröger, C. Cognitive distortions in anorexia nervosa and borderline personality disorder. Psychiatry Res. 2018, 260, 164–172. [Google Scholar] [CrossRef]
- Ford, G.; Waller, G.; Mountford, V. Invalidating Childhood Environments and Core Beliefs in Women with Eating Disorders. Eur. Eat. Disord. Rev. 2011, 19, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.; Leung, N.; Harris, G. Dysfunctional Core Beliefs in Eating Disorders: A Review. J. Cogn. Psychother. 2007, 21, 156–171. [Google Scholar] [CrossRef]
- Legenbauer, T.; Radix, A.K.; Augustat, N.; Schütt-Strömel, S. Power of Cognition: How Dysfunctional Cognitions and Schemas Influence Eating Behavior in Daily Life Among Individuals with Eating Disorders. Front. Psychol. 2018, 9, 2138. [Google Scholar] [CrossRef]
- Tecuta, L.; Gardini, V.; DiGiuseppe, R.; Tomba, E. Do metacognitions mediate the relationship between irrational beliefs, eating disorder symptoms and cognitive reappraisal? J. Clin. Med. 2021, 31, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Waller, G.; Babbs, M.; Milligan, R.; Meyer, C.; Ohanian, V.; Leung, N. Anger and core beliefs in the eating disorders. Int. J. Eat. Disord. 2003, 34, 118–124. [Google Scholar] [CrossRef] [PubMed]
- Hatoum, A.H.; Burton, A.L.; Abbott, M.J. Assessing negative core beliefs in eating disorders: Revision of the Eating Disorder Core Beliefs Questionnaire. J. Eat. Disord. 2022, 10, 18. [Google Scholar] [CrossRef]
- Ellis, A. Reason and Emotion in Psychotherapy (Rev. Ed.); Birch Lane: New York, NY, USA, 1994. [Google Scholar]
- Kronemyer, D.; Bystritsky, A. A non-linear dynamical approach to belief revision in cognitive behavioral therapy. Front. Comput. Neurosci. 2014, 8, 55. [Google Scholar] [CrossRef] [PubMed]
- Tomba, E.; Tecuta, L.; Crocetti, E.; Squarcio, F.; Tomei, G. Residual eating disorder symptoms and clinical features in remitted and recovered eating disorder patients: A systematic review with meta-analysis. Int. J. Eat. Disord. 2019, 52, 759–776. [Google Scholar] [CrossRef]
- American Psychiatric Association. Practice Guideline for the Treatment of Patients with Eating Disorders, 3rd ed.; American Psychiatric Association: Washington, DC, USA, 2010. [Google Scholar]
- National Institute for Health and Care Excellence (NICE). Eating Disorders: Recognition and Treatment; National Institute for Health and Care Excellence (NICE): London, UK, 2020. [Google Scholar]
- Tomba, E.; Offidani, E.; Tecuta, L.; Schumann, R.; Ballardini, D. Psychological well-being in out-patients with eating disorders: A controlled study. Int. J. Eat. Disord. 2014, 47, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Tomba, E.; Tecuta, L.; Schumann, R.; Ballardini, D. Does psychological well-being change following treatment? An exploratory study on outpatients with eating disorders. Compr. Psychiatry 2017, 74, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Fava, G.A. Well-Being Therapy. Treatment Manual and Clinical Applications; Karger: Basel, Switzerland, 2016. [Google Scholar]
- Ryff, C.D. Psychological Well-Being Revisited: Advances in the Science and Practice of Eudaimonia. Psychother. Psychosom. 2014, 83, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.M.; Garamoni, G.L. A structural model of positive and negative states of mind: Asymmetry in the internal dialogue In Advances in Cognitive—Behavioral Research and Therapy; Kendall, P.C., Ed.; Academic Press: Cambridge, MA, USA, 1986; Volume 5, pp. 1–62. [Google Scholar]
- Schwartz, R.M.; Caramoni, G.L. Cognitive balance and psychopathology: Evaluation of an information processing model of positive and negative states of mind. Clin. Psychol. Rev. 1989, 9, 271–294. [Google Scholar] [CrossRef]
- Alsaleh, M.; Lebreuilly, R.; Lebreuilly, J.; Tostain, M. Cognitive balance: States-of-mind and mental health among French students. Best Pract. Ment. Health 2015, 11, 42–53. [Google Scholar]
- Bruch, M.A. Positive Thoughts or Cognitive Balance as a Moderator of the Negative Life Events–Dysphoria Relationship: A Reexamination. Cogn. Ther. Res. 1997, 21, 25–38. [Google Scholar] [CrossRef]
- Cherkasova, L. Application of the States-Of-Mind Model with Rational Emotive Behavior Theory. Ph.D. Thesis, Saint John’s University, New York, NY, USA, 2020. Available online: https://scholar.stjohns.edu/theses_dissertations/56 (accessed on 6 February 2022).
- Hogendoorn, S.M.; Prins, P.J.; Vervoort, L.; Wolters, L.H.; Nauta, M.H.; Hartman, C.A.; Moorlag, H.; de Haan, E.; Boer, F. Positive thinking in anxiety disordered children reconsidered. J. Anxiety Disord. 2012, 26, 71–78. [Google Scholar] [CrossRef]
- Kendall, P.C.; Howard, B.L.; Hays, R.C. Self-referent speech and psychopathology: The balance of positive and negative thinking. Cogn. Ther. Res. 1989, 13, 583–598. [Google Scholar] [CrossRef]
- Ronan, K.R.; Kendall, P.C. Self-talk in distressed youth: States-of-mind and content specificity. J. Clin. Child Psychol. 1997, 26, 330–337. [Google Scholar] [CrossRef]
- Bruch, M.A.; Heimberg, R.G.; Hope, D.A. States of mind model and cognitive change in treated social phobics. Cogn. Ther. Res. 1991, 15, 429–441. [Google Scholar] [CrossRef]
- Michelson, L.K.; Schwartz, R.M.; Marchione, K.E. States-of-mind model: Cognitive balance in the treatment of agoraphobia—II. Adv. Behav. Res. Ther. 1991, 13, 193–213. [Google Scholar] [CrossRef]
- Nasby, W.; Russell, M. Posttraumatic Stress Disorder and the States-of-Mind Model: Evidence of Specificity. Cogn. Ther. Res. 1997, 21, 117–133. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network Analysis: An Integrative Approach to the Structure of Psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- First, M.B.; Williams JB, W.; Karg, R.S.; Spitzer, R.L. SCID-5-CV. Intervista Clinica Strutturata per i Disturbi del DSM-5, Versione per il Clinico ed.; Italiana a cura di Andrea Fossati e Serena Borroni; Raffaello Cortina Editore: Milan, Italy, 2017. [Google Scholar]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- DiGiuseppe, R.; Gorman, B.; Raptis, J. The Factor Structure of the Attitudes and Beliefs Scale 2: Implications for Rational Emotive Behavior Therapy. J. Ration. Cogn. Ther. 2020, 38, 111–142. [Google Scholar] [CrossRef]
- DiGiuseppe, R.; Leaf, R.; Gorman, B.; Robin, M.W. The Development of a Measure of Irrational/Rational Beliefs. J. Ration. Cogn. Ther. 2018, 36, 47–79. [Google Scholar] [CrossRef]
- Ellis, A. Rational Psychotherapy. J. Gen. Psychol. 1958, 59, 35–49. [Google Scholar] [CrossRef] [PubMed]
- Macavei, B. A Romanian adaptation of the Attitudes and Belief Scale 2. Rom. J. Cogn. Behav. Psychother. 2002, 2, 105–122. [Google Scholar]
- Terjesen, M.D.; Salhany, J.; Sciutto, M.J. A Psychometric Review of Measures of Irrational Beliefs: Implications for Psychotherapy. J. Ration. Cogn. Ther. 2009, 27, 83–96. [Google Scholar] [CrossRef]
- Tecuta, L.; Tomba, E.; Lupetti, A.; DiGiuseppe, R. Irrational Beliefs, Cognitive Distortions, and Depressive Symptomatology in a College-Age Sample: A Mediational Analysis. J. Cogn. Psychother. 2019, 33, 116–127. [Google Scholar] [CrossRef]
- Garner, D.M. EDI-3. Eating Disorder Inventory-3. Professional Manual; Psychological Assessment Resources: Lutz, FL, USA, 2008. [Google Scholar]
- Giannini, M.; Pannocchia, L.; dalle Grave, R.; Muratori, F.; Viglione, V. Adattamento Italiano dell’EDI-3. Eating Disorder Inventory-3 trans; Giunti Psychometrics: Florence, Italy, 2008. [Google Scholar]
- Ryff, C.; Singer, B. Psychological well-being: Meaning, measurements and implications of psychotherapy research. Psychother. Psychosom. 1996, 65, 14–23. [Google Scholar] [CrossRef]
- Ryff, C.D. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J. Personal. Soc. Psychol. 1989, 57, 1069–1081. [Google Scholar] [CrossRef]
- Ruini, C.; Ottolini, F.; Rafanelli, C.; Tossani, E.; Ryff, C.D.; Fava, G.A. The Relationship of Psychological Well-Being to Distress and Personality. Psychother. Psychosom. 2003, 72, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Gremigni, P.; Stuart-Brown, S. Una misura del benessere mentale: Validazione italiana della Warwick–Edinburgh mental well-being scale (WEMWBS). G. Ital. Di Psicol. 2011, 2, 543–563. [Google Scholar] [CrossRef]
- DiGiuseppe, R.; David, D.; Venezia, R. Cognitive Theories. In APA Handbook of Clinical Psychology: Theory and Research; Norcross, J.C., VandenBos, G.R., Freedheim, D.K., Olaseni, B.O., Eds.; American Psychological Association: Washington, DC, USA, 2016; Volume 2, pp. 145–182. [Google Scholar]
- Glass, C.R.; Arnkoff, D.B. Think cognitively: Selected issues in cognitive assessment and therapy. Adv. Cogn. Behav. Res. Ther. 1982, 11, 35–71. [Google Scholar]
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef]
- Blanken, T.; Isvoranu, A.-M.; Epskamp, S. Estimating Network Structure using Model Selection. In Network Psychometrics with, R. A Guide for Behavioral and Social Scientists; Isvoranu, A.-M., Epskamp, S., Waldrop, L.J., Borsboom, D., Eds.; Routledge: Oxford, UK, 2022. [Google Scholar]
- Burger, J.; Isvoranu, A.-M.; Lunansky, G.; Haslbeck, J.M.B.; Epskamp, S.; Hoekstra, R.H.A.; Fried, E.I.; Borsboom, D.; Blanken, T.F. Reporting standards for psychological network analyses in cross-sectional data. Psychol. Methods 2022, 28, 806–824. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.J. networktools: Assorted Tools for Identifying Important Nodes in Networks. R Package Version 1.0.0. 2017. Available online: https://CRAN.R-project.org/package=networktools (accessed on 6 February 2022).
- Möller, A.T.; Bothma, M.E. Body Dissatisfaction and Irrational Beliefs. Psychol. Rep. 2001, 88, 423–430. [Google Scholar] [CrossRef]
- Cooper, M.J.; Proudfoot, J. Positive Core Beliefs and Their Relationship to Eating Disorder Symptoms in Women. Eur. Eat. Disord. Rev. 2013, 21, 155–159. [Google Scholar] [CrossRef]
- Vervaet, M.; Puttevils, L.; Hoekstra RH, A.; Fried, E.; Vanderhasselt, M.A. Transdiagnostic vulnerability factors in eating disorders: A network analysis. Eur. Eat. Disord. Rev. J. Eat. Disord. Assoc. 2021, 29, 86–100. [Google Scholar] [CrossRef]
- Pugh, M. A narrative review of schemas and schema therapy outcomes in the eating disorders. Clin. Psychol. Rev. 2015, 39, 30–41. [Google Scholar] [CrossRef]
- Gerges, S.; Hallit, S.; Malaeb, D.; Obeid, S. Maladaptive Cognitive Schemas as Predictors of Disordered Eating: Examining the Indirect Pathway through Emotion Regulation Difficulties. Int. J. Environ. Res. Public Health 2022, 19, 11620. [Google Scholar] [CrossRef]
- Beck, A.T.; Haigh, E.A. Advances in Cognitive Theory and Therapy: The Generic Cognitive Model. Annu. Rev. Clin. 2014, 10, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Leahy, R.L.; Rego, S.A. Cognitive restructuring In Cognitive Behavior Therapy: Core Principles for Practice; O’Donohue, W.T., Fisher, J.E., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012; pp. 133–158. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Cooper, Z.; Shafran, R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behav. Res. Ther. 2003, 41, 509–528. [Google Scholar] [CrossRef]
- De Vos, J.A.; LaMarre, A.; Radstaak, M.; Bijkerk, C.A.; Bohlmeijer, E.T.; Westerhof, G.J. Identifying fundamental criteria for eating disorder recovery: A systematic review and qualitative meta-analysis. J. Eat. Disord. 2017, 5, 34. [Google Scholar] [CrossRef] [PubMed]
- Rania, M.; Aloi, M.; Caroleo, M.; Carbone, E.A.; Fazia, G.; Calabrò, G.; de Filippis, R.; Staltari, F.; Segura-Garcia, C. ‘Impaired Autonomy and Performance’ predicts binge eating disorder among obese patients. Eat. Weight. Disord. 2020, 25, 1183–1189. [Google Scholar] [CrossRef]
- Sassaroli, S.; Veronese, G.; Nevonen, L.; Fiore, F.; Centorame, F.; Favaretto, E.; Ruggiero, G.M. Autonomy and Submissiveness as Cognitive and Cultural Factors Influencing Eating Disorders in Italy and Sweden: An Exploratory Study. Eur. J. Psychol. 2015, 11, 233–243. [Google Scholar] [CrossRef]
- Nordbø, R.H.S.; Espeset, E.M.S.; Gulliksen, K.S.; Skårderud, F.; Holte, A. The meaning of self-starvation: Qualitative study of patients’ perception of anorexia nervosa. Int. J. Eat. Disord. 2006, 39, 556–564. [Google Scholar] [CrossRef]
- Nordbø, R.H.; Gulliksen, K.S.; Espeset, E.M.; Skårderud, F.; Geller, J.; Holte, A. Expanding the concept of motivation to change: The content of patients’ wish to recover from anorexia nervosa. Int. J. Eat. Disord. 2008, 41, 635–642. [Google Scholar] [CrossRef]
- Noordenbos, G.; Seubring, A. Criteria for Recovery from Eating Disorders According to Patients and Therapists. Eat. Disord. 2006, 14, 41–54. [Google Scholar] [CrossRef]
- Fava, G.A.; Guidi, J. The pursuit of euthymia. World Psychiatry 2020, 19, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L.M.; Lopez, S.J. Toward a Science of Mental Health: Positive Directions in Diagnosis Interventions. In Handbook of Positive Psychology; Lopez, S.J., Snyder, C.R., Eds.; Oxford University Press: New York, NY, USA, 2002; pp. 45–59. [Google Scholar]
- Tomei, G.; Pieroni, M.F.; Tomba, E. Network analysis studies in patients with eating disorders: A systematic review and methodological quality assessment. Int. J. Eat. Disord. 2022, 55, 1641–1669. [Google Scholar] [CrossRef]
- Gorrell, S.; Murray, S.B. Eating Disorders in Males. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 641–651. [Google Scholar] [CrossRef] [PubMed]
- Atwood, M.E.; Friedman, A. A systematic review of enhanced cognitive behavioral therapy (CBT-E) for eating disorders. Int. J. Eat. Disord. 2020, 53, 311–330. [Google Scholar] [CrossRef]
- Jansen, A. Eating disorders need more experimental psychopathology. Behav. Res. Ther. 2016, 86, 2–10. [Google Scholar] [CrossRef]
- Stice, E.; Bohon, C.; Gau, J.M.; Rohde, P. Factors that predict persistence versus non-persistence of eating disorder Symptoms: A prospective study of high-risk young women. Behav. Res. Ther. 2021, 144, 103932. [Google Scholar] [CrossRef] [PubMed]
- Amsel, R.; Fichten, C.S. Recommendations for Self-Statement Inventories: Use of Valence, End Points, Frequency, and Relative Frequency. Cogn. Ther. Res. 1998, 22, 255–277. [Google Scholar] [CrossRef]


| Measure | ED PATIENTS (n = 199) (M ± SD) |
|---|---|
| EDI-3 ED Risk (range 0–100) | 52.69 ± 21.30 |
| EDI-3 ED General Psychological Maladjustment (range 0–256) | 98.50 ± 39.08 |
| PWB Autonomy (range 14–84) | 49.72 ±13.41 |
| PWB Environmental Mastery (range 14–84) | 46.30 ±13.04 |
| PWB Personal Growth (range 14–84) | 59.82 ± 11.56 |
| PWB-Positive relations with others (range 14–84) | 56.60 ± 13.33 |
| PWB Life Purpose (range 14–84) | 51.96 ± 13.67 |
| PWB Self-Acceptance (range 14–84) | 41.95 ± 14.50 |
| ED PATIENTS (n = 199) | CONTROLS (n = 95) | ||||
|---|---|---|---|---|---|
| Measure | M ± SD | M ± SD | t (df) | p | d |
| ABS-2 RATIONAL BELIEFS | 79.84 ± 25.13 | 99.81 ± 24.11 | t(289) = 6.44 | <0.0001 | −0.80 |
| SOM RATIO | 0.54 ± 0.18 | 0.67 ± 0.17 | t(241) = −6.36 | <0.0001 | −0.73 |
| ABS_RATIO | EDI_RISK | EDI_GEN_PSYCHOPATH | PWB_AUTON | PWB_ENV_MAST | PWB_PERS_GROWTH | PWB_POS_REL | PWB_SELF_ACCEPT | |
|---|---|---|---|---|---|---|---|---|
| ABS_RATIO | 0.00 | −0.20 | * −0.37 | 0.25 | 0.00 | 0.00 | 0.00 | 0.00 |
| EDI_RISK | −0.20 | 0.00 | 0.25 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| EDI_GEN_PSYCHOPATH | * −0.37 | 0.25 | 0.00 | 0.00 | −0.14 | 0.00 | 0.00 | −0.34 |
| PWB_AUTON | 0.25 | 0.00 | 0.00 | 0.00 | 0.00 | 0.23 | 0.00 | 0.11 |
| PWB_ENV_MAST | 0.00 | 0.00 | −0.14 | 0.00 | 0.00 | 0.00 | 0.00 | * 0.49 |
| PWB_PERS_GROWTH | 0.00 | 0.00 | 0.00 | 0.23 | 0.00 | 0.00 | 0.26 | 0.24 |
| PWB_POS_REL | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.26 | 0.00 | 0.24 |
| PWB_SELF_ACCEPT | 0.00 | 0.00 | −0.34 | 0.11 | *0.49 | 0.24 | 0.24 | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tecuta, L.; Tomei, G.; DiGiuseppe, R.; Schumann, R.; Ballardini, D.; Tomba, E. Mapping the Path to Cognitive Balance: Applying the States of Mind Model and Network Analysis to Eating Disorder Patients. J. Clin. Med. 2023, 12, 5790. https://doi.org/10.3390/jcm12185790
Tecuta L, Tomei G, DiGiuseppe R, Schumann R, Ballardini D, Tomba E. Mapping the Path to Cognitive Balance: Applying the States of Mind Model and Network Analysis to Eating Disorder Patients. Journal of Clinical Medicine. 2023; 12(18):5790. https://doi.org/10.3390/jcm12185790
Chicago/Turabian StyleTecuta, Lucia, Giuliano Tomei, Raymond DiGiuseppe, Romana Schumann, Donatella Ballardini, and Elena Tomba. 2023. "Mapping the Path to Cognitive Balance: Applying the States of Mind Model and Network Analysis to Eating Disorder Patients" Journal of Clinical Medicine 12, no. 18: 5790. https://doi.org/10.3390/jcm12185790





