Abstract
Our study aimed to analyze the prognosis and reproductive outcomes of patients with advanced-stage serous borderline ovarian tumors (SBOTs) who underwent fertility-sparing surgery (FSS). This study included patients aged ≤ 45 years diagnosed with advanced-stage (International Federation of Gynecology and Obstetrics II and III) SBOTs who were treated with FSS. Conservative surgeries were performed in 65 patients with advanced-stage SBOT with a median age of 28 years (range, 16–44 years). Nine patients had invasive implants. The median follow-up was 81.7 months. Forty-six patients (70.8%) had a relapse (median time to first recurrence, 22.8 months). Thirteen patients subsequently developed recurrence as an invasive disease, and two died due to disease progression. After multivariate analysis, age < 30 years and incomplete cytoreduction were independent risk factors for recurrence. Invasive implants and postoperative residual tumors were significantly associated with shorter disease-free survival. Of 35 patients attempting to conceive, 12 underwent assisted reproductive technology. Additionally, 19 pregnancies, including 15 full-term births, were documented. FSS provides a good chance of reproductive success in women with advanced-stage SBOT who desire fertility preservation, but it has a high recurrence rate and risk of malignancy transformation. Patients with invasive implants should be strictly selected for FSS.
1. Introduction
Borderline ovarian tumors (BOTs) are common gynecological tumors, accounting for 10–15% of ovarian epithelial tumors, and commonly occur in young women in their mid-40s, with the onset ranging from 35–53 years [1,2]. Histopathologically, BOT cells proliferate actively without destructive stromal invasion. The two most prevalent BOT subtypes are serous and mucinous variants, accounting for 96% of cases. These subtypes manifest with different clinical characteristics and biological behaviors, which may contribute to distinct postoperative risk profiles [3,4]. Clinically, the characteristics of BOT are atypical proliferative tumor cells, late relapse patterns, and good prognosis [5]. Most patients with BOT (75%) are diagnosed early, and the lesions are commonly confined to the ovaries [6]. Serous BOT (SBOT), one of the most frequent BOT subtypes, could occur bilaterally, and extraovarian lesions are found in 20–40% of SBOTs [5,6]. A limited number of SBOT cases could develop into low-grade serous ovarian carcinoma (LGSOC). Recurrences frequently occur as SBOT and do not lower the survival rate. Fertility-sparing surgery (FSS) is generally accepted among patients with BOT, especially for patients within the reproductive age. Most studies showed the clinical efficacy of conservative surgery in early-stage patients, whereas only several scattered studies focused on advanced-stage patients, which partially revealed its feasibility and safety with a good prognosis [7,8]. However, data on uncertain prognostic factors and reproductive outcomes of FSS are lacking. Therefore, this retrospective study was conducted to show the oncological and reproductive outcomes of patients with advanced-stage SBOT who were treated conservatively from a single tertiary center in China.
2. Materials and Methods
2.1. Basic Characteristics
The medical records of patients with advanced-stage (II-III) SBOT who were treated with FSS at Peking Union Medical College Hospital (PUMCH) between January 1999 to December 2021 were screened. The Institutional Review Board of PUMCH approved the study. The information included demographic information, CA125 levels, surgical procedures, surgical stage, histology, residual mass, chemotherapy regimens, and relapse details. Two experienced pathologists reviewed and confirmed the original pathologic slides according to the 2014 and 2020 World Health Organization (WHO) criteria (BOT classification) and Bell’s criteria for peritoneal implants [9,10]. The tumor-staging system was based on the International Federation of Gynecology and Obstetrics 2014 criteria (FIGO 2014). The inclusion criteria included (i) age under 45 years, (ii) stage II/III SBOT confirmed by pathology, (iii) treated by FSS, (iv) with valid follow-up outcomes. The exclusion criteria were age > 45 years, non-serous histological component, and history of malignancy. FSS was defined as a procedure that preserves the uterus and at least one adnexa. Complete cytoreduction was defined as no residual tumor post-operatively. The indications and type of adjuvant chemotherapy were on the basis of residual diseases and pathological features including invasive implants and lymph node involvement. Patients were followed up by outpatient visits and telephonic interviews. We collected data, including details of recurrences and reproductive outcomes. Relapse was defined as the detection of SBOT or LGSOC at the surgery for suspected recurrence. Disease-free survival (DFS) was defined as the time from the initial surgery to recurrence or censoring, whereas overall survival (OS) was defined as the time between the date of surgery and death or censoring.
2.2. Statistical Analyses
A single-variable Cox proportional hazard model was used to analyze the association between prognostic factors and recurrence. Variables with p < 0.05 were included in the multivariate analysis. Hazard ratios were calculated for potential risk factors for relapse. Survival curves were calculated using the Kaplan–Meier method and compared with the log-rank test. All tests were two-sided, and p = 0.05 indicated statistical significance. SPSS software version 21.0 was used for all statistical analyses.
3. Results
3.1. Patients’ Characteristics
During the study period, 65 patients with FIGO stage II and III SBOT who underwent FSS in our hospital were selected from the overall database. The median age was 28 years, and the median follow-up was 81.7 months (range, 9.8–285.4 months). Table 1 shows the clinicopathological characteristics. Of the patients who underwent FSS, 34 and 31 were diagnosed with FIGO stage II (52.3%) and III SBOTs (47.7%), respectively. Unilateral salpingo-oophorectomy and contralateral cystectomy (USO + CC) were performed in 25 patients with BOTs, and bilateral cystectomy (BC) was performed in 31 patients. Of nine patients with unilateral disease, three and six patients underwent unilateral cystectomy (UC) and USO, respectively. Invasive implants were seen in nine (13.8%) patients. Moreover, 44 (67.7%) patients achieved complete cytoreduction. Chemotherapy was administered in 15 patients after initial surgery, and chemotherapy regimens included single-agent platinum, paclitaxel/platinum, and platinum/cyclophosphamide, with treatment duration ranging from 1–8 cycles. Table A1 shows the surgical procedures.

Table 1.
Clinicopathologic characteristics in patients with advanced-stage SBOT.
3.2. Oncological Outcomes
The total recurrence rate and median DFS were 70.8% (46/65) and 22.8 months (range, 3.0–185.7 months), respectively. Moreover, 33 (71.7%) patients relapsed with non-invasive diseases. Of 46 (78.2%) patients with recurrence, 36 underwent conservative re-operation during the first relapse. Thirteen patients (20.0%) had recurrences as invasive diseases (six with invasive implants and seven with LGSOC). Table 2 shows the characteristics of patients with invasive recurrences.

Table 2.
Characteristics of patients with invasive recurrence.
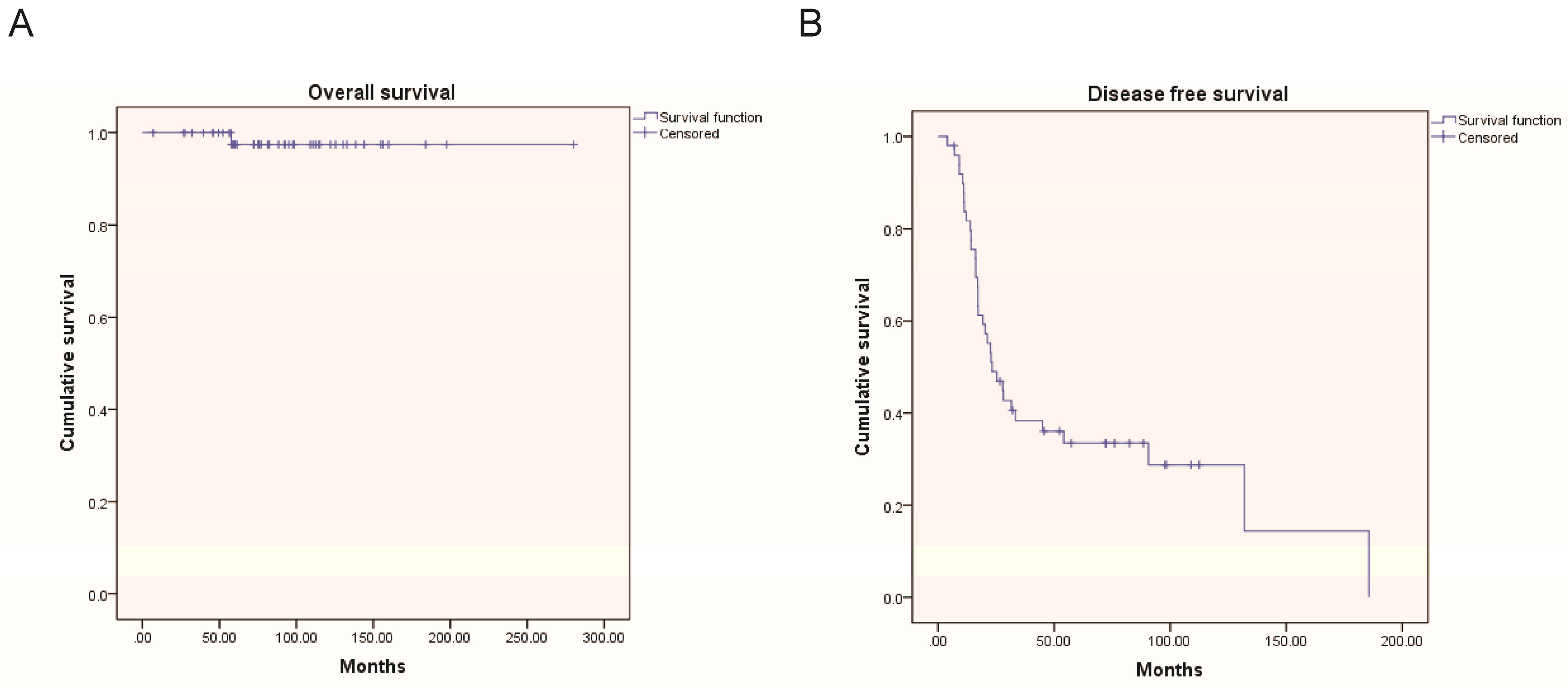
We analyzed potential associations between clinicopathological factors and recurrence (Table 3). In univariate analysis, age < 30 years, FIGO III, and incomplete cytoreduction were significantly associated with higher recurrence rates (p = 0.011, 0.031, and 0.014, respectively). In multivariate analysis, age < 30 years and residual tumor after initial surgery were identified as independent risk factors for relapse (p = 0.013, 0.013, respectively). Shorter disease-free survival was observed in patients with invasive implants and residual tumors using a Cox proportional hazard model (Table 4). Except for two patients who died because of LGSOC, all patients survived. The 5-year OS and DFS rates were 97.0% and 38.5%, respectively. Figure 1 shows the Kaplan–Meier curves for DFS and OS.

Table 3.
Risk factors for recurrence in patients with advanced-stage SBOT.

Table 4.
Prognostic factors on disease-free survival in patients with advanced-stage SBOT.
Figure 1.
Survival curves for overall survival (A) and disease-free survival (B). OS: overall survival, DFS: disease-free survival.
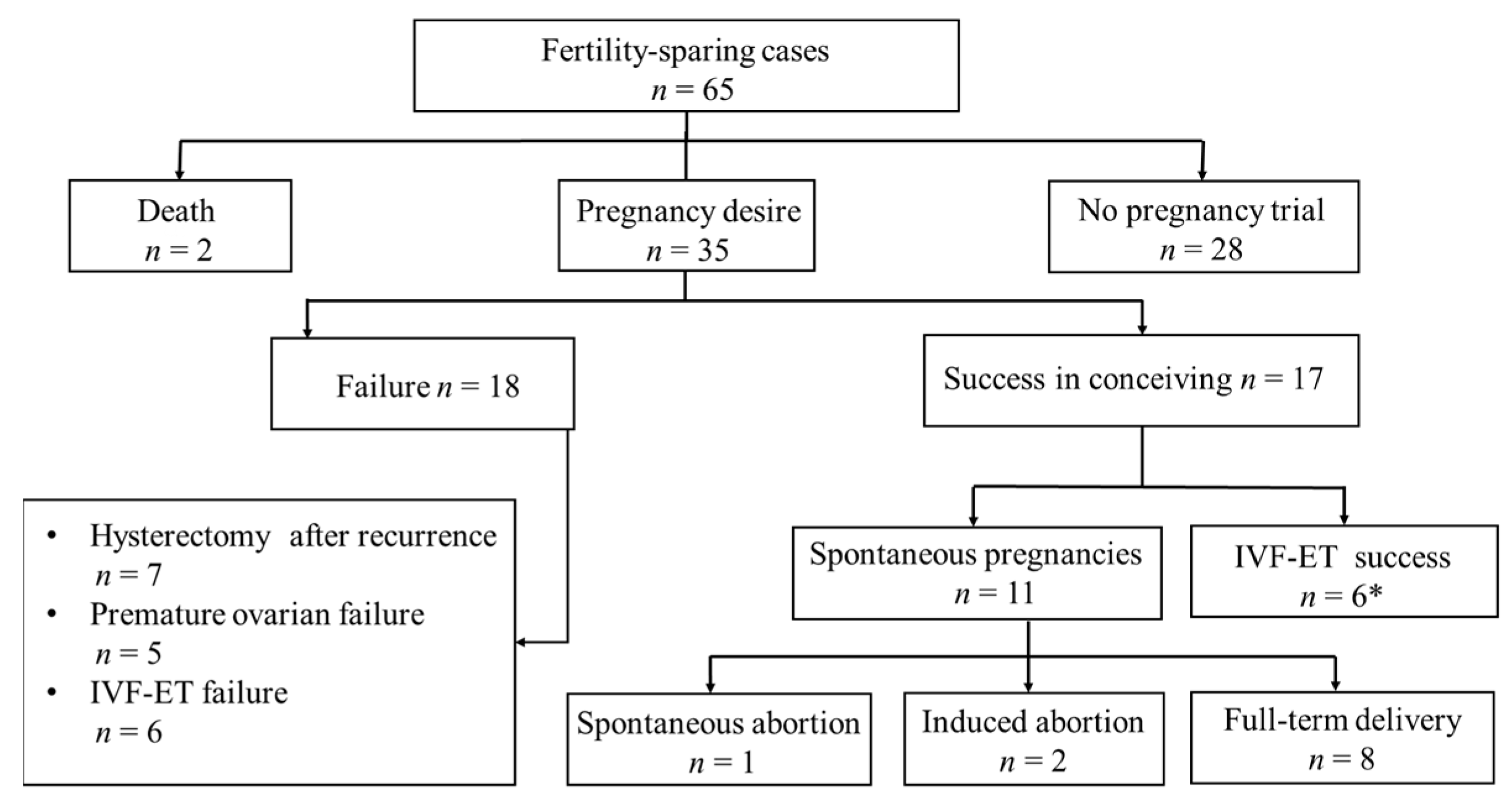
3.3. Reproductive Outcomes
Thirty-five (53.8%) patients desired to conceive. Of these, 17 became pregnant, with 15 healthy live births in 13 women (Figure 2). Two patients had two full-term deliveries. Additionally, one woman was seven months pregnant by the end of the follow-up. One had a spontaneous abortion, and two underwent termination of pregnancy. Twelve women underwent ART, and five had at least one live-born infant. Two women underwent radical surgeries for SBOT recurrence after delivery. The median age of patients with pregnancies was similar to that of infertile patients (26 versus 27 years). The median interval between the initial operation and the first parturition was 23.7 months.
Figure 2.
Flowchart representing reproductive outcomes. * Including five live births and one still in pregnant.
4. Discussion
Existing international guidelines recommended that fertility-sparing surgery is the standard approach in young patients with early-stage BOTs [10]. However, there is still no consensus on the use of FSS in cases of advanced-stage diseases. There are very few studies about conservative management, and most of those did not specifically focus on advanced-stage SBOTs [11,12,13].
Our study, conducted in a tertiary oncological referral center, is the largest single-center series investigating the oncological and reproductive outcomes of patients with advanced-stage SBOT with fertility preservation, with a median follow-up of up to 81.7 months. The 5-year OS rate of patients with advanced-stage SBOT who underwent FSS was 97.0%, which was similar to previous studies. Although most patients with advanced SBOT have a favorable prognosis, the recurrence risk should be noted. Several prognostic factors were associated with recurrence risk, including invasive implants and surgical approaches [14,15].
Invasive implants have been found in only a minority of BOT patients [16,17]. In 2014, invasive implants were considered extra-ovarian LGSOCs after WHO revised the classification of gynecological tumors [18]. In practice, European Society of Gynecological Oncology/European Society for Medical Oncology (ESGO/ESMO) and National Comprehensive Cancer Network (NCCN) do not support the terminology because they consider patients with invasive implants as different from those of classic advanced-stage LGSOCs in terms of survival of clinical management. FSS could be considered in selected SBOT patients with invasive implants according to international guidelines [10,19]. Data on conservative treatment of SBOTs with invasive implants are limited. To date, only 31 SBOT patients with invasive implants have been reported to receive FSS. In our study, nine patients with invasive implants had at least one recurrence. Moreover, six patients had a relapse with invasive diseases (two patients with LGSOCs), and one died. The median disease-free interval in patients with invasive implants is significantly shorter than in those with non-invasive implants (9.3 months versus 28.1 months, HR = 0.525, p < 0.001). Although the variable analysis did not consider implant type as a risk factor for recurrence due to the limited number of cases with invasive implants, data on DFS suggested the prognostic importance of invasive implants in patients undergoing FSS. Indications for FSS in patients with invasive implants should be strictly mastered. However, a large series should be conducted to explore better surgical options for patients with invasive implants.
The residual disease is an important independent prognostic factor in SBOTs with peritoneal implants [20,21]. In addition, Cytoreductive surgery is recommended in advanced-stage SBOT [10]. Complete rection of all the visible lesions is imperative for both staging and management. Our results emphasized the complete surgical excision of any lesions, which was associated with lower recurrence risk and extended DFS (Table 3 and Table 4). In our study, 14 of fifteen patients with adjuvant chemotherapy relapsed after initial surgery. The relative high recurrence rate is largely due to inherent selection bias in patients receiving adjuvant chemotherapy for more serious condition of tumors. Adjuvant chemotherapy failed to lower the relapse rate or improve the survival rate in SBOTs, even in advanced stages. There is no corroborating evidence to support adjuvant chemotherapy to date. Therefore, cytoreduction remains as the keystone for clinical benefit. To achieve complete cytoreduction, adequate preoperative evaluation should be performed to detect the location and extent of metastatic diseases for the complete removal of tumors. Teams offering cytoreductive surgery should be specialized and experienced. A careful exploration for abdominopelvic cavities, especially the diaphragm and pouch of Douglas, during operation is helpful to allow precise excision of small lesions, optimizing the chance of complete removal. At the same time, ovarian blood vessels need to be cautiously preserved for protection of ovarian function.
The present study showed that the recurrence rate significantly increased among childbearing women aged <30 years. Fotopoulou et al. [22] found that increasing age (per 10 years) seemed to have a protective effect against relapses in BOT patients. The research of Uzan et al. proposed that the young age of 30 may serve as a hallmark for predicting prognosis in stage I borderline ovarian tumors [23]. In the previous series, the role of age in advanced-stage SBOT received little attention. Our study showed no significant difference in the proportion of complete cytoreduction between the two age groups, indicating that the higher recurrence rate in young patients was not influenced by age distribution. Thus, the follow-up of young patients needs to be addressed considering their higher risk of recurrence and intention to conceive.
Many studies have assessed the effects of adnexectomy on tumor results and fertility outcomes. Fang et al. [4] concluded that USO was superior to cystectomy in reducing the relapse rate (24%). Moreover, the recurrence interval of patients undergoing USO was longer than those who received cystectomy. Vasconcelos et al. [24] reported that USO was significantly favored over cystectomy in terms of recurrence reduction. A recent phase III trial concerning BOTs demonstrated that bilateral cystectomies increased the fertility rate without increasing the recurrence rate compared with unilateral adnexectomy and a contralateral cystectomy [25]. In our study, different surgical methods for preserving fertility presented a similar relapse tendency. While the ovary volume plays a key role in fertility, the necessity of adnexectomy is debatable.
Concerning the debate of surgical approaches (laparotomy versus laparoscopy), no significant difference was found in the postoperative recurrence rates between laparoscopy and laparotomy from our study, which was consistent with earlier findings [11,15]. This may confirm the feasibility of laparoscopy. Vandenput et al. [26] pointed out that the high incidence of peritoneal recurrence was caused by less complete resection and incomplete laparoscopic visualization. However, risk factors of tumor rupture, intraperitoneal dissemination, and port-site implantation caused by laparoscopy among advanced-stage patients cannot be ignored.
With regard to pregnancy outcomes, 48.6% (17/35) of young women became pregnant after attempting to conceive following conservative treatment. Interestingly, these women who became pregnant spontaneously were either disease-free or completed childbearing before the first recurrence. The mean time between initial surgery and parturition was comparable to the disease-free interval. Therefore, the optimal timing for pregnancy might be one year after first surgery, which allows sufficient recovery post-operatively and avoid the peak time of recurrence. Considering repeated FSSs is necessary if patients have not finished childbearing before the first relapse. Besides, five women had successfully given birth to healthy babies through ART and they survived with no evidence of disease. However, whether ovarian stimulation would increase the risk of disease progression remains unclear [27,28]. Further evidence is needed for ART in advanced-stage SBOTs. Hence, an oncofertility consultation prior to fertility-sparing surgery is essential in order to assess reproductive status and prepare for postoperative pregnancies.
Our study has several limitations. First, this is a retrospective study conducted in a tertiary center. Some patients were initially diagnosed elsewhere with SBOT and then transferred to our hospital for further management. Our study’s relatively higher recurrence rate might be partly due to referral bias. Second, the limited sample size of our study may affect the generalizability of the results because of the rarity of the disease. Finally, relative shorter follow-up among several patients could result in an underestimation of recurrent risk. The follow-up time should be longer to better understand long-term outcomes, as the present evidence shows that relapse risk could still settle at a high level even after 10-year follow-up [29]. Nevertheless, the present study was the largest series of advanced-stage SBOTs undergoing fertility-preserved surgeries in Asian populations.
5. Conclusions
In a summary, despite the high recurrence rate, FSS could be selected in childbearing SBOT patients diagnosed at advanced stage with favorable reproductive outcomes and no impact on overall survival. Age distribution has been validated to be associated with risk of recurrences. Moreover, patients could benefit from complete cytoreductive surgery. Fertility-sparing treatment should be cautiously considered in those with invasive implants. Prospective studies with larger sample sizes are needed in the future to clarify unresolved issues with FSS for advanced-stage SBOTs.
Author Contributions
Conceptualization, W.C., J.Y. (Junjun Yang) and Y.X.; methodology, W.C. and C.L.; software, W.C.; formal analysis, W.C., C.L. and J.Y. (Junjun Yang); investigation, C.L.,D.W., X.X., D.C., J.Y. (Jiaxin Yang), L.P., M.W., J.Y. (Junjun Yang) and Y.X.; data curation, D.W., X.X., D.C., J.Y. (Jiaxin Yang), L.P., M.W., J.Y. (Junjun Yang) and Y.X.; writing—original draft preparation, W.C.; writing—review and editing, J.Y. (Junjun Yang) and Y.X.; supervision, J.Y. (Junjun Yang) and Y.X.; project administration, J.Y. (Junjun Yang); funding acquisition, J.Y. (Junjun Yang) and Y.X. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81971475 & No. 81972451).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the ethics committee of Peking Union Medical College Hospital (S-K2059).
Informed Consent Statement
Patient consent was waived for its retrospective nature.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to acknowledge the staff in the medical record room for their assistance in retrieving data.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Surgical procedures of patients at the primary fertility-sparing surgeries.
Table A1.
Surgical procedures of patients at the primary fertility-sparing surgeries.
| Characteristics | |
|---|---|
| Surgical treatment | |
| Unilateral cystectomy | 3 |
| Bilateral cystectomy | 25 |
| Unilateral salpingo-oophorectomy | 6 |
| Unilateral salpingo-oophorectomy and contralateral cystectomy | 31 |
| Peritoneal cytology | 19 |
| Positive | 15 |
| Negative | 4 |
| Appendectomy | 14 |
| Lymphadenectomy | 11 |
| Omentectomy | 31 |
| Residual tumor | |
| No residual tumor | 44 |
| Residual disease | 21 |
References
- Ureyen, I.; Karalok, A.; Tasci, T.; Turkmen, O.; Boran, N.; Tulunay, G.; Turan, T. The Factors Predicting Recurrence in Patients with Serous Borderline Ovarian Tumor. Int. J. Gynecol. Cancer 2016, 26, 66–72. [Google Scholar] [CrossRef]
- Gershenson, D.M. Management of borderline ovarian tumours. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 41, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Seong, S.J.; Kim, D.H.; Kim, M.K.; Song, T. Controversies in borderline ovarian tumors. J. Gynecol. Oncol. 2015, 26, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.; Zhao, L.; Chen, X.; Yu, A.; Xia, L.; Zhang, P. The impact of clinicopathologic and surgical factors on relapse and preg-nancy in young patients (≤40 years old) with borderline ovarian tumors. BMC Cancer 2018, 18, 1147. [Google Scholar] [CrossRef]
- Ushijima, K.; Kawano, K.; Tsuda, N.; Nishio, S.; Terada, A.; Kato, H.; Tasaki, K.; Matsukuma, K. Epithelial borderline ovarian tumor: Diagnosis and treatment strategy. Obstet. Gynecol. Sci. 2015, 58, 183–187. [Google Scholar] [CrossRef]
- Hauptmann, S.; Friedrich, K.; Redline, R.; Avril, S. Ovarian borderline tumors in the 2014 WHO classification: Evolving concepts and diagnostic criteria. Virchows Arch. 2016, 470, 125–142. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhang, W.; Wang, Y. The feasibility of fertility-sparing surgery in treating advanced-stage border-line ovarian tumors: A meta-analysis. Taiwan J. Obstet. Gynecol. 2016, 55, 319–325. [Google Scholar] [CrossRef]
- Falcone, F.; Breda, E.; Ferrandina, G.; Malzoni, M.; Perrone, A.M.; Cormio, G.; Di Donato, V.; Frigerio, L.; Mangili, G.; Raspagliesi, F.; et al. Fertility-sparing treatment in advanced-stage serous borderline ovarian tumors. An analysis from the MITO14 study database. Gynecol. Oncol. 2021, 161, 825–831. [Google Scholar] [CrossRef]
- Bell, D.A.; Weinstock, M.A.; Scully, R.E. Peritoneal implants of ovarian serous borderline tumors: Histologic features and prognosis. Cancer 1988, 62, 2212–2222. [Google Scholar] [CrossRef]
- Colombo, N.; Sessa, C.; du Bois, A.; Ledermann, J.; McCluggage, W.G.; McNeish, I.; Morice, P.; Pignata, S.; Ray-Coquard, I.; Vergote, I.; et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: Pathology and molecular biology, early and advanced stages, borderline tumours and recurrent diseasedagger. Ann. Oncol. 2019, 30, 672–705. [Google Scholar] [CrossRef]
- De Iaco, P.; Ferrero, A.; Rosati, F.; Melpignano, M.; Biglia, N.; Rolla, M.; De Aloysio, D.; Sismondi, P. Behaviour of ovarian tumors of low malignant potential treated with conservative surgery. Eur. J. Surg. Oncol. 2009, 35, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Zanetta, G.; Rota, S.; Chiari, S.; Bonazzi, C.; Bratina, G.; Mangioni, C. Behavior of Borderline Tumors with Particular Interest to Persistence, Recurrence, and Progression to Invasive Carcinoma: A Prospective Study. J. Clin. Oncol. 2001, 19, 2658–2664. [Google Scholar] [CrossRef] [PubMed]
- Song, T.; Choi, C.H.; Kim, H.-J.; Lee, W.; Lee, Y.-Y.; Kim, T.-J.; Lee, J.-W.; Bae, D.-S.; Kim, B.-G. Oncologic and reproductive outcomes in patients with advanced-stage borderline ovarian tumors. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011, 156, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Morice, P.; Uzan, C.; Fauvet, R.; Gouy, S.; Duvillard, P.; Darai, E. Borderline ovarian tumour: Pathological diagnostic dilemma and risk factors for invasive or lethal recurrence. Lancet Oncol. 2012, 13, e103–e115. [Google Scholar] [CrossRef]
- Jung, H.-J.; Park, J.-Y.; Kim, D.-Y.; Suh, D.-S.; Kim, J.-H.; Kim, Y.-M.; Kim, Y.-T.; Nam, J.-H. Comparison of Laparoscopic and Open Surgery for Patients with Borderline Ovarian Tumors. Int. J. Gynecol. Cancer 2018, 28, 1657–1663. [Google Scholar] [CrossRef]
- Hart, W.R. Borderline epithelial tumors of the ovary. Mod Pathol. 2005, 18 (Suppl. 2), S33–S50. [Google Scholar] [CrossRef]
- Du Bois, A.; Ewald-Riegler, N.; De Gregorio, N.; Reuss, A.; Mahner, S.; Fotopoulou, C.; Kommoss, F.; Schmalfeldt, B.; Hilpert, F.; Fehm, T.; et al. Borderline tumours of the ovary: A cohort study of the Arbeitsgmeinschaft Gynakologische Onkologie (AGO) Study Group. Eur. J. Cancer 2013, 49, 1905–1914. [Google Scholar] [CrossRef]
- Kurman, R.J.; Carcangiu, M.L.; Herrington, C.S.; Young, R.H. WHO Classification of Tumours of Female Re-Productive Organs, 4th ed.; IARC: Lyon, France, 2014. [Google Scholar]
- Network, National Comprehensive Cancer. NCCN Clinical Practice Guidelines in Oncology. Ovarian Can-cer Including Fallopian Tube Cancer and Primary Peritoneal Cancer, Version 3. 2021. Available online: https://www.nccn.org/professionals/physiciangls/pdf/ovarian.pdf (accessed on 26 February 2021).
- Trillsch, F.; Mahner, S.; Woelber, L.; Vettorazzi, E.; Reuss, A.; Ewald-Riegler, N.; de Gregorio, N.; Fotopoulou, C.; Schmalfeldt, B.; Burges, A.; et al. Age-dependent differences in borderline ovarian tumours (BOT) regarding clinical characteristics and outcome: Results from a sub-analysis of the Arbeitsgemeinschaft Gynaekologische Onkologie (AGO) ROBOT study. Ann. Oncol. 2014, 25, 1320–1327. [Google Scholar] [CrossRef]
- Kane, A.; Uzan, C.; Rey, A.; Gouy, S.; Camatte, S.; Pautier, P.; Lhommé, C.; Haie-Meder, C.; Duvillard, P.; Morice, P. Prognostic Factors in Patients with Ovarian Serous Low Malignant Potential (Borderline) Tumors with Peritoneal Implants. Oncol. 2009, 14, 591–600. [Google Scholar] [CrossRef]
- Fotopoulou, C.; Sehouli, J.; Ewald-Riegler, N.; De Gregorio, N.; Reuss, A.; Richter, R.; Mahner, S.; Kommoss, F.; Schmalfeldt, B.; Fehm, T.; et al. The Value of Serum CA125 in the Diagnosis of Borderline Tumors of the Ovary: A Subanalysis of the Prospective Multicenter ROBOT Study. Int. J. Gynecol. Cancer 2015, 25, 1248–1252. [Google Scholar] [CrossRef]
- Uzan, C.; Muller, E.; Kane, A.; Rey, A.; Gouy, S.; Bendiffallah, S.; Duvillard, P.; Fauvet, R.; Darai, E.; Morice, P. Prognostic factors for recurrence after conservative treatment in a series of 119 patients with stage I serous borderline tumors of the ovary. Ann. Oncol. 2014, 25, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, I.; de Sousa Mendes, M. Conservative surgery in ovarian borderline tumours: A meta-analysis with emphasis on recurrence risk. Eur. J. Cancer 2015, 51, 620–631. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; Falbo, A.; Del Negro, S.; Rocca, M.; Russo, T.; Cariati, F.; Annunziata, G.; Tolino, A.; Tagliaferri, P.; Zullo, F. Ultra-conservative fertility-sparing strategy for bilateral borderline ovarian tumours: An 11-year follow-up. Hum. Reprod. 2010, 25, 1966–1972. [Google Scholar] [CrossRef] [PubMed]
- Vandenput, I.; Amant, F.; Vergote, I. Peritoneal recurrences might be less common in advanced stage serous borderline ovarian tumors that were treated by laparotomy. Gynecol. Oncol. 2005, 98, 523–524. [Google Scholar] [CrossRef]
- Denschlag, D.; Von Wolff, M.; Amant, F.; Kesic, V.; Reed, N.; Schneider, A.; Rodolakis, A. Clinical recommendation on fertility preservation in border-line ovarian neoplasm: Ovarian stimulation and oocyte retrieval after conservative surgery. Gynecol. Obstet. Invest. 2010, 70, 160–165. [Google Scholar] [CrossRef]
- Attar, E.; Berkman, S.; Topuz, S.; Baysal, B.; Akhan, S.; Chambers, J.T. Evolutive peritoneal disease after conservative management and the use of infertility drugs in a patient with stage IIIC borderline micro-papillary serous carcinoma (MPSC) of the ovary: Case report. Hum. Reprod. 2004, 19, 1472–1475. [Google Scholar] [CrossRef]
- Marchette, M.D.; Ceppi, L.; Andreano, A.; Bonazzi, C.M.; Buda, A.; Grassi, T.; Giuliani, D.; Sina, F.; Lamanna, M.; Bianchi, T.; et al. Oncologic and fertility impact of surgical approach for borderline ovarian tumours treated with fertility sparing surgery. Eur. J. Cancer 2019, 111, 61–68. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).