Retromolar Triangle Anesthesia Technique: A Feasible Alternative to Classic?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruitment
- Age: 18–50 years.
- Both males and females.
- Inferior molars with indication of exodontia: teeth with decays unrestorable by odontal therapy, apical pathology, severe periodontal diseases, orthodontic extractions, pre-prosthetic extractions.
- Age: <18 years.
- Pregnancy.
- Patients with acute pulpitis of the inferior molars.
- Patients with odontogenic abscesses.
- Patients with tumors of the intermaxillary commissure.
- Patients with contraindications to the administration of anesthetics with adrenaline or articaine.
- Patients with mucosa lesions on the injection site.
2.2. Armamentarium
- Short needle: 21 mm, 30 gauge diameter (Septoject, Septodont, Saint-Maur-des-Fosses Cedex, France).
- One ampoule: 1.7 mL of articaine with 1:100,000 adrenaline (Septanest, Septodont, Allington Kent, UK).
- Chlorhexidine solution (Eludril, Pierre Fabre, Lavaur, France).
- Electric pulp test (DenjoyDental Co., Ltd., Changsha, China),
- Periodontal probe.
2.3. Patient Position
- The pulp test checks the vitality of the first/second lower molar on the vestibular face and notes the intensity to which it responds.
- The inferior occlusal plane is parallel with the Camper plane.
2.4. Doctor Position
- For the fourth quadrant: 8–9 o’clock position.
- For the third quadrant: 9–10 o’clock position.
- The left hand removes the soft tissues.
- Direct visibility of the puncture site.
2.5. Vitality Tests
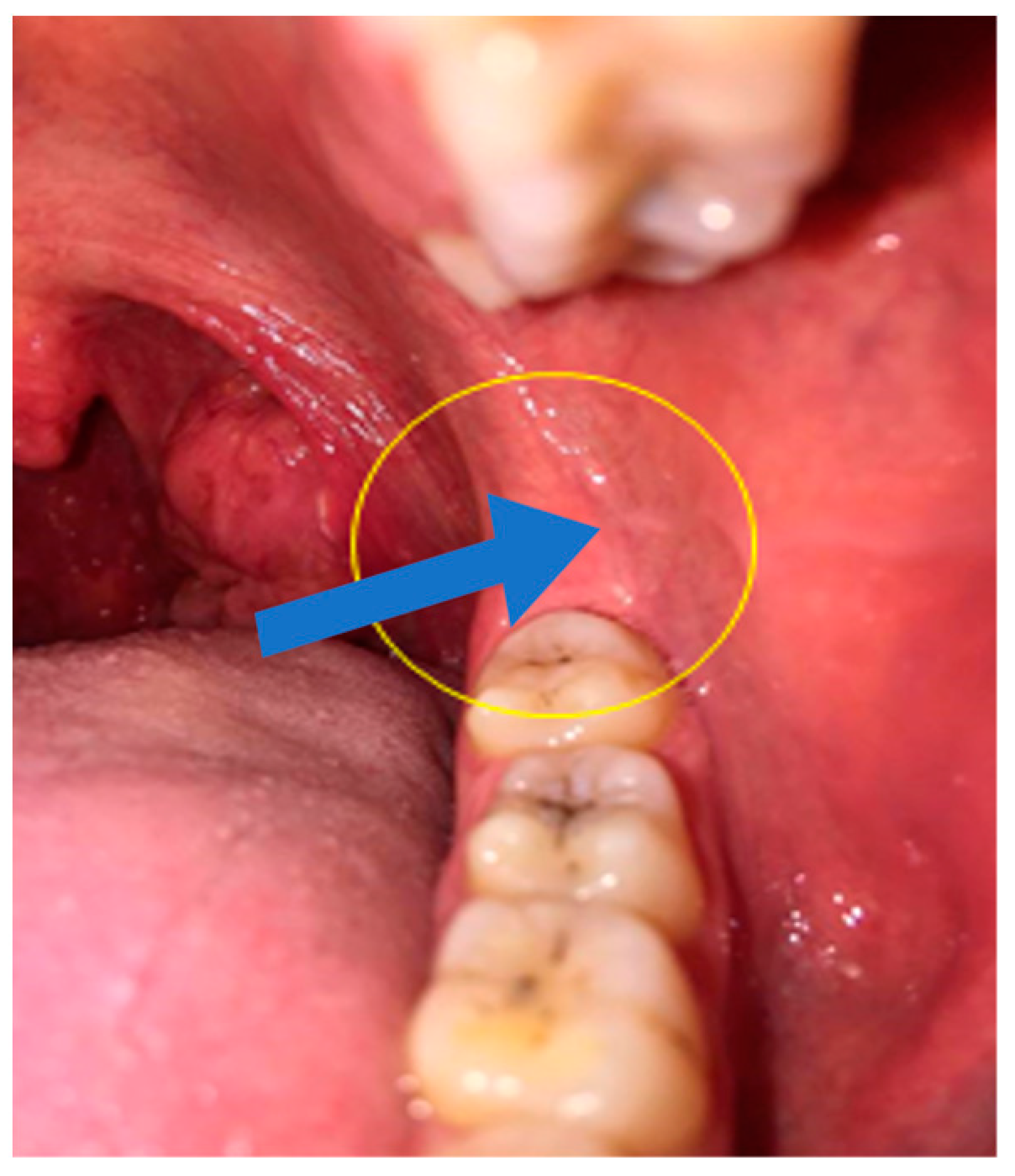
2.6. Insertion Needle Area (Figure 1)
- The oral mucosa of the area of the retromolar triangle.
- At 5 mm distal from the distal face of the last molar.
- In the most central part of the lateral retromolar triangle.
2.7. Needle Level
- Perpendicular to the mandibular bone.
- Rearward, outward, and downward orientation.
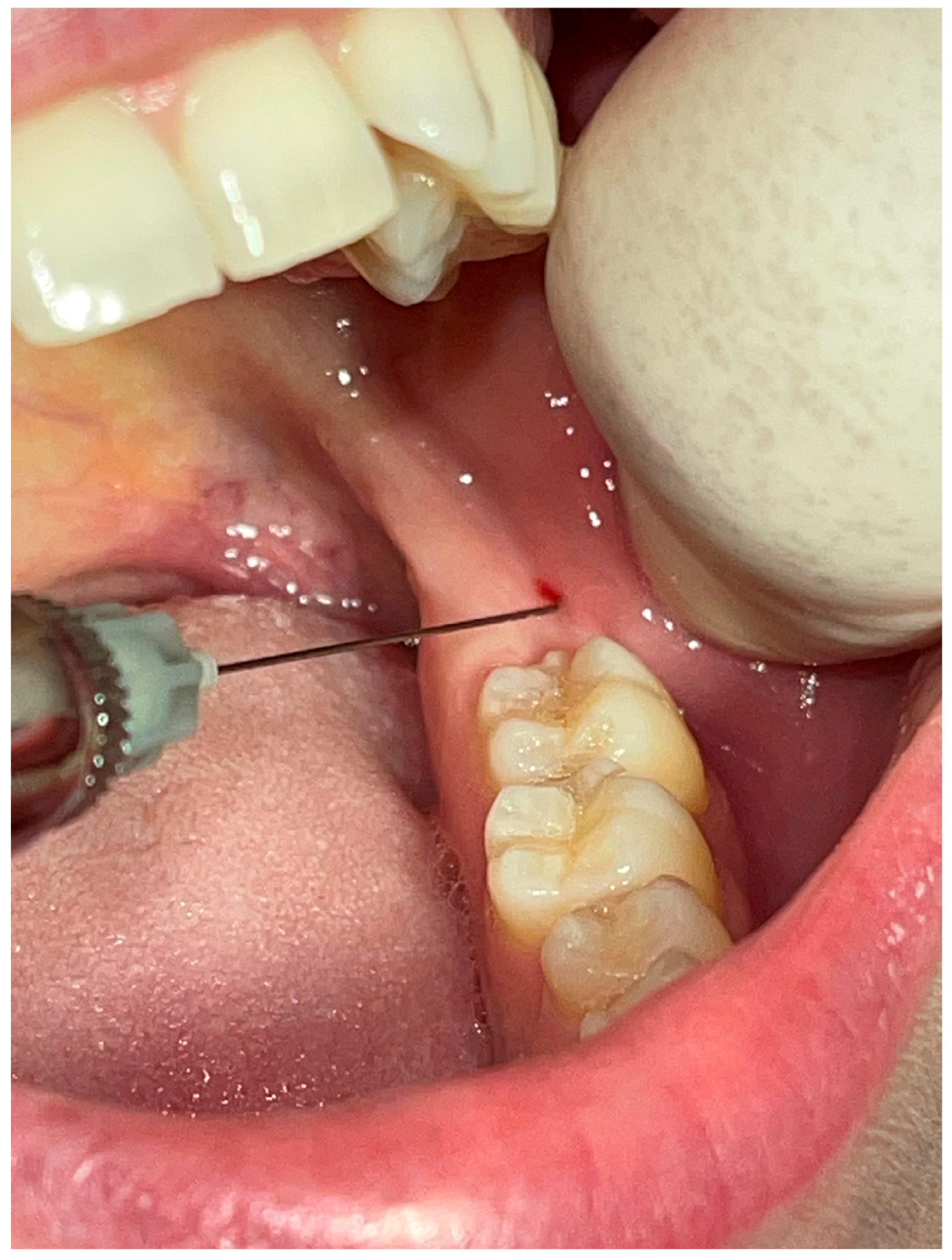
2.8. Anesthesia Technique (Figure 2)
- The puncture site must be dried with a sterile cotton gauze.
- A chlorhexidine-based antiseptic solution is applied.
- Local anesthesia with topical anesthetic (benzocaine 20%) is performed (Opahl, USA).
- The syringe is drawn parallel to the occlusal mandibular plane.
- The needle is inserted in the mucosa, searching for bone contact, after which the anesthetic solution is slowly deposited (1 mL/min).
2.9. Anesthesia Instalation and Check
- For inferior alveolar nerve: With the pulp test, we checked after 15 min the anesthesia on the same first/second inferior molars that were initially tested by measuring the intensity of the stimuli necessary for the tooth pulp to respond. The guide values followed by the manufacturer were 0–40 for the normal reaction of the dental pulp, 40–80 for partial anesthesia, and over 80 for installed anesthesia of the tooth pulp. The value was noted.
- For mental nerve: With the periodontal probe, the mucosa of the lower lip was punctured in front the inferior canine on the anesthetized side.
- For buccal nerve: With the periodontal probe, the vestibular mucosa was punctured in front of the first molar on the lower anesthetized side.
- For lingual nerve: With the periodontal probe, the lingual mucosa was punctured on the lingual gingival sulcus of the first molar on the lower anesthetized side.
- The results for mental, buccal, and lingual nerves were noted using the visual analog scale for pain (VAS).
2.10. Statistical Analysis
3. Results
3.1. Patients’ Sex and Age Distribution
3.2. Extracted Teeth
3.3. Retromolar Triangle Anesthesia Efficiency
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghatak, R.N.; Helwany, M.; Ginglen, J.G. Anatomy, Head and Neck, Mandibular Nerve. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar] [PubMed]
- Adnindya, M.; Indri, S.S.; Tri, S.; Wardiansah, W. Functional anatomy of mandibular nerve. J. Kedokt. Dan Kesehat. Publ. Ilm. Fak. Kedokt. Univ. Sriwij. 2023, 10, 215–220. [Google Scholar] [CrossRef]
- Suazo-Galdames, I.C.; Cantín-López, M.G.; Zavando-Matamala, D.A. Inferior alveolar nerve block anesthesia via the retromolar triangle, an alternative for patients with blood dyscrasias. Med. Oral Patol. Oral Cir. Bucal. 2008, 13, E43–E47. [Google Scholar] [PubMed]
- Ahmed, S.; Tabassum, N.; Alyousef, S.; Al Dayel, O. A single injection straight line approach to anesthetize inferior alveolar nerve, long buccal nerve, and lingual nerve: A new technique. J. Int. Oral Health 2016, 8, 319–323. [Google Scholar]
- Malamed, S. Maryland Heights: Mosby. In Handbook of Local Anesthesia, 6th ed.; Elsevier: St. Louis, MO, USA, 2012; pp. 157–253. [Google Scholar]
- Rabinovich, S.A.; Vasil’ev, Y.L.; Kuzin, A.N. Anatomic rationale for clinical efficacy of intraosseous mental nerve anesthesia. Stomatologiya 2018, 97, 41. [Google Scholar] [CrossRef]
- Kuzin, A.V.; Semkin, V.A.; Dydykin, S.S. Scientific anatomical rationalefor lower teeth local anesthesia. Stomatologiya 2015, 94, 35. [Google Scholar] [CrossRef]
- Alhindi, M.; Rashed, B.; Alotaibi, N. Failure rate of inferior alveolar nerve block among dental students and interns. Saudi Med. J. 2016, 37, 84–89. [Google Scholar] [CrossRef]
- Madan, G.; Madan, S.; Madan, A. Failure of inferior alveolar nerve block. J. Am. Dent. Assoc. 2003, 133, 843–846. [Google Scholar] [CrossRef]
- Wong, J. Adjuncts to Local Anesthesia: Separating Fact form fiction. J. Can. Dent. Assoc. 2001, 67, 397. [Google Scholar]
- Desantis, J.; Liebow, C. Four common mandibular nerve anomalies that lead to local anesthesia failures. J. Am. Dent. Assoc. 1996, 127, 1081–1086. [Google Scholar] [CrossRef]
- Haas, D.A. Alternative mandibular nerve block techniques: A review of the Gow-Gates and Akinosi-Vazirani closed-mouth mandibular nerve block techniques. J. Am. Dent. Assoc. 2011, 142, 8S–12S. [Google Scholar] [CrossRef]
- Sferlazza, L.; Zaccheo, F.; Campogrande, M.E.; Petroni, G.; Cicconetti, A. Common Anatomical Variations of Neurovascular Canals and Foramina Relevant to Oral Surgeons: A Review. Anatomia 2022, 1, 91–106. [Google Scholar] [CrossRef]
- Suazo, G.I.; Zavando, M.D.; Cantín, L.M. Retromolar canal and foramen prevalence in dried mandibles and clinical implications. Int. J. Odontostomatol. 2008, 2, 183–187. [Google Scholar]
- Park, M.-K.; Jung, W.; Bae, J.-H.; Kwak, H.-H. Anatomical and radiographic study of the mandibular retromolar canal. J. Dent. Sci. 2016, 11, 370–376. [Google Scholar] [CrossRef]
- Lee, C.R.; Yang, H.J. Alternative techniques for failure of conventional inferior alveolar nerve block. J. Dent. Anesth. Pain Med. 2019, 19, 125–134. [Google Scholar] [CrossRef]
- Takasugi, Y.; Furuya, H.; Moriya, K.; Okamoto, Y. Clinical evaluation of inferior alveolar nerve block by injection into thepterygomandibular space anterior to the mandibular foramen. Anesth. Prog. 2000, 47, 125–129. [Google Scholar] [PubMed]
- Palti, D.G.; Almeida, C.M.; Rodrigues Ade, C.; Andreo, J.C.; Lima, J.E. Anesthetic technique for inferior alveolar nerve block: A newapproach. J. Appl. Oral Sci. 2011, 19, 11–15. [Google Scholar] [CrossRef]
- Thangavelu, K.; Kannan, R.; Senthil Kumar, N. Inferior alveolar nerve block: Alternative technique. Anesth. Essays Res. 2012, 6, 53–57. [Google Scholar] [CrossRef]
- Thangavelu, K.; Sabitha, S.; Kannan, R.; Saravanan, K. Inferior alveolar nerve block using internal oblique ridge as landmark. SRM J. Res. Dent. Sci. 2012, 3, 15–18. [Google Scholar]
- Boonsiriseth, K.; Sirintawat, N.; Arunakul, K.; Wongsirichat, N. Comparative study of the novel and conventional injection approach for inferior alveolar nerve block. Int. J. Oral Maxillofac. Surg. 2013, 42, 852–856. [Google Scholar] [CrossRef]
- Nooh, N.; Abdullah, W. Incidence of complications of inferior alveolar nerve block injection. J. Med. Biomed. Sci. 2010, 1, 52–56. [Google Scholar]
- Khoury, J.N.; Mihailidis, S.; Ghabriel, M.; Townsend, G. Applied anatomy of the pterygomandibular space: Improving the success of inferior alveolar nerve blocks. Aust. Dent. J. 2011, 56, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Khalil, H. A basic review on the inferior alveolar nerve block techniques. Anesth. Essays Res. 2014, 8, 3–8. [Google Scholar] [CrossRef] [PubMed]
- You, T.M.; Kim, K.D.; Huh, J.; Woo, E.J.; Park, W. The influence of mandibular skeletal characteristics on inferior alveolar nerve block anesthesia. J. Dent. Anesthesia Pain Med. 2015, 15, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.K.; Jacobsen, P.L. Reasons for local anesthesia failures. J. Am. Dent. Assoc. 1992, 123, 69–73. [Google Scholar] [CrossRef]
- Aggarwal, V.; Jain, A.; Kabi, D. Anesthetic efficacy of supplemental buccal and lingual infiltrations of articaine and lidocaine after an inferior alveolar nerve block in patients with irreversible pulpitis. J. Endod. 2009, 35, 925–929. [Google Scholar] [CrossRef]
- Meechan, J.G. How to overcome failed local anaesthesia. Br. Dent. J. 1999, 186, 15–20. [Google Scholar] [CrossRef]
- Kang, S.H.; Byun, I.Y.; Kim, J.H.; Park, H.K.; Kim, M.K. Three-dimensional anatomic analysis of mandibular foramen with mandibular anatomic landmarks for inferior alveolar nerve block anesthesia. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 17–23. [Google Scholar] [CrossRef]
- Piot, B.; Sigaud-Fiks, M.; Huet, P.; Fressinaud, E.; Trossaërt, M.; Mercier, J. Management of dental extractions in patients with bleeding disorders. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2002, 93, 247–250. [Google Scholar] [CrossRef]
- Karamifar, K.; Shirali, D.; Saghiri, M.A.; Abbott, P.V. Retromolar canal infiltration as a supplement to the inferior alveolar nerve block injection: An uncontrolled clinical trial. Clin. Oral Investig. 2021, 25, 5473–5478. [Google Scholar] [CrossRef]
- Certosimo, A.J.; Archer, R.D. A clinical evaluation of the electric pulp tester as an indicator of local anesthesia. Oper. Dent. 1996, 21, 25–30. [Google Scholar]
- Aggarwal, K.; Lamba, A.K.; Faraz, F.; Tandon, S.; Makker, K. Comparison of anxiety and pain perceived with conventional and computerized local anesthesia delivery systems for different stages of anesthesia delivery in maxillary and mandibular nerve blocks. J. Dent. Anesthesia Pain Med. 2018, 18, 367–373. [Google Scholar] [CrossRef] [PubMed]
- Tortamano, I.P.; Siviero, M.; Lee, S.; Sampaio, R.M.; Simone, J.L.; Rocha, R.G. Onset and duration period of pulpal anesthesia of articaine and lidocaine in inferior alveolar nerve block. Braz. Dent. J. 2013, 24, 371–374. [Google Scholar] [CrossRef] [PubMed]

| Overall (N = 50) | Data |
|---|---|
| Male | 35 (70.0%) |
| Female | 15 (30.0%) |
| Age range | 18–41 years |
| Age mean (SD) | 27.5 (6.5) |
| Overall (N = 50) | Data |
|---|---|
| Left first mandibular molar: 3.6 | 12 (24.0%) |
| Left second mandibular molar: 3.7 | 4 (8.0%) |
| Left third mandibular molar: 3.8 | 9 (18.0%) |
| Right first mandibular molar: 4.6 | 10 (20.0%) |
| Right second mandibular molar: 4.7 | 8 (16.0%) |
| Right third mandibular molar: 4.8 | 7 (14.0%) |
| Anesthesia Efficiency | Overall (N = 50) |
|---|---|
| Anesthesia worked (IAN) | 32 (64.0%) |
| Anesthesia did not work (IAN) | 18 (36.0%) |
| Anesthesia worked (BUCCAL N.) | 11 (22.0%) |
| Anesthesia did not work (BUCCAL N.) | 39 (78.0%) |
| Anesthesia worked (LINGUAL N.) | 23 (46.0%) |
| Anesthesia did not work (LINGUAL N.) | 27 (54.0%) |
| Dependent: Anesthesia Efficiency | Anesthesia Did Not Work | Anesthesia Worked | Total | p | |
|---|---|---|---|---|---|
| Anesthesia duration | Mean (SD) | - | 113.1 (18.0) | 72.4 (56.7) | <0.001 |
| VAS mental | Mean (SD) | 7.1 (1.6) | 0.6 (0.8) | 2.9 (3.4) | <0.001 |
| Post-anesthesia value | Mean (SD) | 52.1 (9.4) | 78.2 (1.9) | 68.8 (13.9) | <0.001 |
| Pre-anesthesia value | Mean (SD) | 22.9 (9.4) | 26.6 (7.9) | 25.3 (8.6) | 0.153 |
| Tooth | 3.6 | 3 (16.7) | 9 (28.1) | 12 (24.0) | 0.511 |
| 3.7 | 3 (16.7) | 1 (3.1) | 4 (8.0) | ||
| 3.8 | 4 (22.2) | 5 (15.6) | 9 (18.0) | ||
| 4.6 | 3 (16.7) | 7 (21.9) | 10 (20.0) | ||
| 4.7 | 2 (11.1) | 6 (18.8) | 8 (16.0) | ||
| 4.8 | 3 (16.7) | 4 (12.5) | 7 (14.0) | ||
| VAS buccal | Mean (SD) | 4.8 (2.5) | 5.2 (2.7) | 5.1 (2.6) | 0.624 |
| VAS lingual | Mean (SD) | 3.6 (2.5) | 3.3 (3.0) | 3.4 (2.8) | 0.721 |
| Age | Mean (SD) | 27.6 (6.8) | 27.5 (6.4) | 27.5 (6.5) | 0.964 |
| Sex | M | 14 (77.8) | 21 (65.6) | 35 (70.0) | 0.563 |
| F | 4 (22.2) | 11 (34.4) | 15 (30.0) |
| Predictor | Estimate | SE | t | p |
|---|---|---|---|---|
| Intercept | 80.11821 | 1.8248 | 43.9051 | <0.001 |
| VAS mental | −3.91945 | 0.2007 | −19.5316 | <0.001 |
| VAS buccal | −0.03863 | 0.2560 | −0.1509 | 0.881 |
| VAS lingual | 0.11731 | 0.2400 | 0.4888 | 0.627 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roi, C.I.; Roi, A.; Nicoară, A.; Motofelea, A.C.; Riviș, M. Retromolar Triangle Anesthesia Technique: A Feasible Alternative to Classic? J. Clin. Med. 2023, 12, 5829. https://doi.org/10.3390/jcm12185829
Roi CI, Roi A, Nicoară A, Motofelea AC, Riviș M. Retromolar Triangle Anesthesia Technique: A Feasible Alternative to Classic? Journal of Clinical Medicine. 2023; 12(18):5829. https://doi.org/10.3390/jcm12185829
Chicago/Turabian StyleRoi, Ciprian Ioan, Alexandra Roi, Adrian Nicoară, Alexandru Cătălin Motofelea, and Mircea Riviș. 2023. "Retromolar Triangle Anesthesia Technique: A Feasible Alternative to Classic?" Journal of Clinical Medicine 12, no. 18: 5829. https://doi.org/10.3390/jcm12185829
APA StyleRoi, C. I., Roi, A., Nicoară, A., Motofelea, A. C., & Riviș, M. (2023). Retromolar Triangle Anesthesia Technique: A Feasible Alternative to Classic? Journal of Clinical Medicine, 12(18), 5829. https://doi.org/10.3390/jcm12185829







