Orthostatic Stress and Baroreflex Sensitivity: A Window into Autonomic Dysfunction in Lone Paroxysmal Atrial Fibrillation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Tilt Test
2.3. Data Analysis
Arterial Baroreflex Function
2.4. Statistical Analysis
3. Results
3.1. Population
3.2. Heart Rate and Blood Pressure Changes
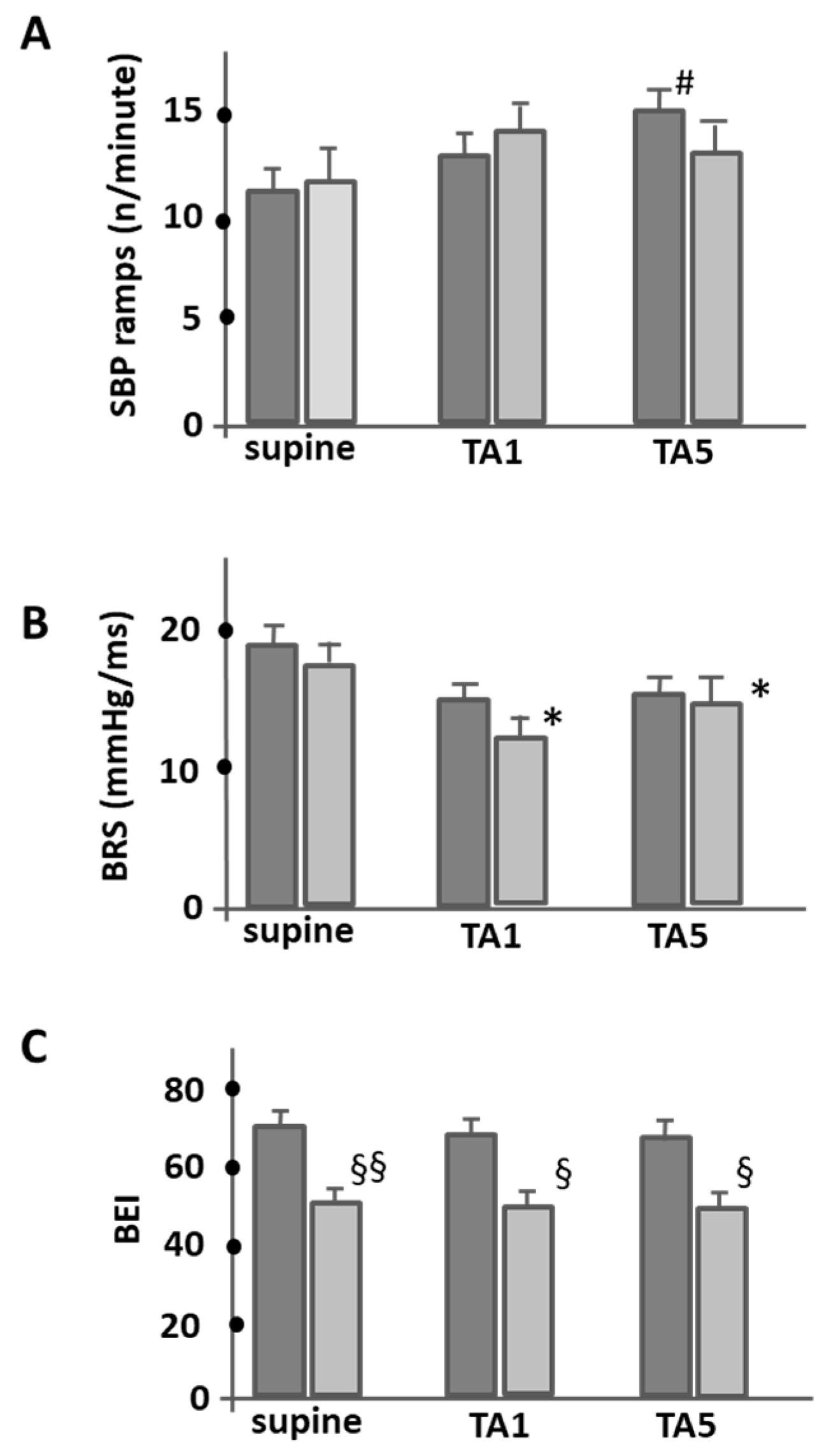
3.3. Baroreflex Sensitivity and Effectiveness
4. Discussion
4.1. Evaluation of Baroreflex Sensitivity in PAF Patients
4.2. Autonomic Nervous System and Its Impact on BRS
4.3. Potential Implications for PAF Patients
4.4. Hemodynamic Influences and Their Effects on the Modulation of the Baroreflex
4.5. Addressing Causality, Association, and Confounders
4.6. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wolf, P.A.; Benjamin, E.J.; Belanger, A.J.; Kannel, W.B.; Levy, D.; D’Agostino, R.B. Secular trends in the prevalence of atrial fibrillation: The Framingham Study. Am. Heart J. 1996, 131, 790–795. [Google Scholar] [CrossRef]
- Chugh, S.S.; Blackshear, J.L.; Shen, W.-K.; Hammill, S.C.; Gersh, B.J. Epidemiology and natural history of atrial fibrillation: Clinical implications. J. Am. Coll. Cardiol. 2001, 37, 371–378. [Google Scholar] [CrossRef]
- Thrall, G.; Lane, D.; Carroll, D.; Lip, G.Y. Quality of Life in Patients with Atrial Fibrillation: A Systematic Review. Am. J. Med. 2006, 119, 448.e1–448.e19. [Google Scholar] [CrossRef]
- Ball, J.; Carrington, M.J.; McMurray, J.J.; Stewart, S. Atrial fibrillation: Profile and burden of an evolving epidemic in the 21st century. Int. J. Cardiol. 2013, 167, 1807–1824. [Google Scholar] [CrossRef]
- Chugh, S.S.; Havmoeller, R.; Narayanan, K.; Singh, D.; Rienstra, M.; Benjamin, E.J.; Gillum, R.F.; Kim, Y.-H.; Zheng, Z.J.; Murray, C.J. Worldwide epidemiology of atrial fibrillation: A Global Burden of Disease 2010 Study. Circulation 2014, 129, 837–847. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J. Am. Coll. Cardiol. 2014, 64, e1–e76. [Google Scholar] [CrossRef]
- Colilla, S.; Crow, A.; Petkun, W.; Singer, D.E.; Simon, T.; Liu, X. Estimates of Current and Future Incidence and Prevalence of Atrial Fibrillation in the U.S. Adult Population. Am. J. Cardiol. 2013, 112, 1142–1147. [Google Scholar] [CrossRef]
- Krijthe, B.P.; Kunst, A.; Benjamin, E.J.; Lip, G.Y.; Franco, O.H.; Hofman, A.; Witteman, J.C.; Stricker, B.H.; Heeringa, J. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 2013, 34, 2746–2751. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS) The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2020, 42, 373–498. [Google Scholar]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in collaboration with the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar]
- Chen, P.S.; Chen, L.S.; Fishbein, M.C.; Lin, S.F.; Nattel, S. Role of the autonomic nervous system in atrial fibrillation: Pathophysiology and therapy. Circ. Res. 2014, 114, 1500–1515. [Google Scholar] [CrossRef]
- Haïssaguerre, M.; Jaïs, P.; Shah, D.C.; Takahashi, A.; Hocini, M.; Quiniou, G.; Garrigue, S.; Le Mouroux, A.; Le Métayer, P.; Clémenty, J. Spontaneous Initiation of Atrial Fibrillation by Ectopic Beats Originating in the Pulmonary Veins. N. Engl. J. Med. 1998, 339, 659–666. [Google Scholar] [CrossRef]
- Shen, M.J.; Zipes, D.P. Role of the Autonomic Nervous System in Modulating Cardiac Arrhythmias. Circ. Res. 2014, 114, 1004–1021. [Google Scholar] [CrossRef] [PubMed]
- Rebecchi, M.; Fanisio, F.; Rizzi, F.; Politano, A.; De Ruvo, E.; Crescenzi, C.; Panattoni, G.; Squeglia, M.; Martino, A.; Sasso, S.; et al. The Autonomic Coumel Triangle: A New Way to Define the Fascinating Relationship between Atrial Fibrillation and the Autonomic Nervous System. Life 2023, 13, 1139. [Google Scholar] [CrossRef]
- Carlisle, M.A.; Piccini, J.P.; Fudim, M. The interplay between autonomic tone and atrial arrhythmias. Clin. Auton. Res. 2022, 32, 223–225. [Google Scholar] [CrossRef]
- Meyer, C.; Kahle, A.-K. The autonomic nervous system as a piece of the mechanistic puzzle linking sleep and atrial fibrillation. J. Interv. Card. Electrophysiol. 2023, 66, 815–822. [Google Scholar] [CrossRef]
- Scridon, A. Autonomic imbalance and atrial ectopic activity—A pathophysiological and clinical view. Front. Physiol. 2022, 13, 1058427. [Google Scholar] [CrossRef]
- Sharifov, O.F.; Fedorov, V.V.; Beloshapko, G.G.; Glukhov, A.V.; Yushmanova, A.V.; Rosenshtraukh, L.V. Roles of adrenergic and cholinergic stimulation in spontaneous atrial fibrillation in dogs. J. Am. Coll. Cardiol. 2004, 43, 483–490. [Google Scholar] [CrossRef]
- Chen, S.A.; Hsieh, M.H.; Tai, C.T.; Tsai, C.F.; Prakash, V.S.; Yu, W.C.; Hsu, T.L.; Ding, Y.A.; Chang, M.S. Initiation of atrial fibrillation by ectopic beats originating from the pulmonary veins: Electrophysiological characteristics, pharmacological responses, and effects of radiofrequency ablation. Circulation 1999, 100, 1879–1886. [Google Scholar] [CrossRef]
- Zhong, X.; Jiao, H.; Gao, J.; Teng, J. Autonomic tone variations prior to onset of paroxysmal atrial fibrillation. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2022, 28, e934028-1. [Google Scholar] [CrossRef] [PubMed]
- La Rovere, M.T.; Pinna, G.D.; Hohnloser, S.H.; Marcus, F.I.; Mortara, A.; Nohara, R.; Bigger, J.T., Jr.; Camm, A.J.; Schwartz, P.J. Baroreflex sensitivity and heart rate variability in the identification of patients at risk for life-threatening arrhythmias: Implications for clinical trials. Circulation 2001, 103, 2072–2077. [Google Scholar] [CrossRef] [PubMed]
- Mainardi, L.; Corino, V.; Belletti, S.; Terranova, P.; Lombardi, F. Low frequency component in systolic arterial pressure variability in patients with persistent atrial fibrillation. Auton. Neurosci. 2009, 151, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Field, M.E.; Wasmund, S.L.; Page, R.L.; Hamdan, M.H. Restoring Sinus Rhythm Improves Baroreflex Function in Patients with Persistent Atrial Fibrillation. J. Am. Heart Assoc. 2016, 5, e002997. [Google Scholar] [CrossRef] [PubMed]
- Styczkiewicz, K.; Spadacini, G.; Tritto, M.; Perego, G.B.; Facchini, M.; Bilo, G.; Kawecka-Jaszcz, K.; Czarnecka, D.; Malfatto, G.; Parati, G. Cardiac autonomic regulation in patients undergoing pulmonary vein isolation for atrial fibrillation. J. Cardiovasc. Med. 2019, 20, 297–305. [Google Scholar] [CrossRef]
- Miyoshi, M.; Kondo, H.; Ishii, Y.; Shinohara, T.; Yonezu, K.; Harada, T.; Sato, H.; Yano, Y.; Yoshimura, S.; Abe, I.; et al. Baroreflex Sensitivity in Patients With Atrial Fibrillation. J. Am. Heart Assoc. 2020, 9, e018019. [Google Scholar] [CrossRef]
- Kondo, H.; Shinohara, T.; Fukui, A.; Miyoshi, M.; Ishii, Y.; Otsubo, T.; Teshima, Y.; Yufu, K.; Nakagawa, M.; Takahashi, N. Possible Role of Baroreflex Sensitivity in Patients With Paroxysmal Atrial Fibrillation. JACC Clin. Electrophysiol. 2019, 5, 523–525. [Google Scholar] [CrossRef]
- Laranjo, S.; Geraldes, V.; Oliveira, M.; Rocha, I. Insights into the background of autonomic medicine. Rev. Port. De Cardiol. (Engl. Ed. ) 2017, 36, 757–771. [Google Scholar] [CrossRef]
- Di Rienzo, M.; Parati, G.; Castiglione, P.; Tordi, R.; Mancia, G.; Pedotti, A. Baroreflex efectiveness index: An additional measure of baroreflex control of heart rate in daily life. Am. J. Physiol. 2001, 280, R744–R751. [Google Scholar]
- Oliveira, M.; Silva, M.N.; Timoteo, A.; Feliciano, J.; Silva, S.; Xavier, R.; Laranjo, S.; Matos, L.; Silva-Carvalho, L.; Rocha, I.; et al. Wavelet analysis of heart rate and blood pressure variability to assess autonomic activity on tilt test in patients with paroxysmal atrial fibrillation. Eur. J. Neurol. 2008, 15, 237. [Google Scholar]
- Iacoviello, M.; Guida, P.; Forleo, C.; Sorrentino, S.; D’Alonzo, L.; Favale, S. Impaired arterial baroreflex function before nitrate-induced vasovagal syncope during head-up tilt test. Europace 2008, 10, 1170–1175. [Google Scholar] [CrossRef]
- Del Colle, S.; Milan, A.; Caserta, M.; Dematteis, A.; Naso, D.; Mulatero, P.; Rabbia, F.; Veglio, F. Baroreflex sensitivity is impaired in essential hypertensives with central obesity. J. Hum. Hypertens. 2007, 21, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Pinna, G.D.; Maestri, R.; La Rovere, M.T. Assessment of baroreflex sensitivity from spontaneous oscillations of blood pressure and heart rate: Proven clinical value? Physiol. Meas. 2015, 36, 741. [Google Scholar] [CrossRef] [PubMed]
- Waki, H.; Shimizu, T.; Yamasaki, M.; Katahira, K.; Katsuda, S.; Polson, J.W.; Maeda, M. Ramp rate of blood pressure changes does not affect aortic afferent sensitivity in anesthetized rats. Neurosci. Lett. 2008, 448, 37–40. [Google Scholar] [CrossRef]
- Waki, H.; Yamasaki, M.; Katahira, K.; Katsuda, S.; Maeda, M.; Shimizu, T. Developmental changes in functional characteristics of aortic baroreceptor afferents in rats. Exp. Physiol. 2008, 93, 319–324. [Google Scholar] [CrossRef]
- Berg, M.P.v.D.; Hassink, R.J.; Baljé-Volkers, C.; Crijns, H.J.G.M. Role of the autonomic nervous system in vagal atrial fibrillation. Heart 2003, 89, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Lok, N.; Lau, C.P. Abnormal vasogal reaction. Autonomic function, and heart rate variability in patients with paroxysmal atrial fibrillation. PACE 1998, 21, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Styczkiewicz, K.; Spadacini, G.; Tritto, M.; Facchini, M.; Perego, G.B.; Bilo, G.; Castiglioni, P.; Di Rienzo, M.; Kawecka-Jaszcz, K.; Salerno-Uriarte, J.A.; et al. Spontaneous Baroreflex Sensitivity is Reduced in Patients with Recurrent Symptomatic Atrial Fibrillation. High Blood Press. Cardiovasc. Prev. 2007, 14, 145–196. [Google Scholar] [CrossRef]
- Westerhof, B.E.; Gisolf, J.; Karemaker, J.M.; Wesseling, K.H.; Secher, N.H.; van Lieshout, J.J. Time course analysis of baroreflex sensitivity during postural stress. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2864–H2874. [Google Scholar] [CrossRef]
- Taneyama, C.; Goto, H. Fractal Cardiovascular Dynamics and Baroreflex Sensitivity After Stellate Ganglion Block. Head-up tilt protocol and data analysis. Anesth. Analg. 2009, 109, 1335–1340. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, F.C.; Padilha, M.C.S.V.; Rocha, T.M.d.M.S.; Lima, L.S.; Carandina, A.; Bellocchi, C.; Tobaldini, E.; Montano, N.; Soares, P.P.d.S.; Rodrigues, G.D. Cardiovascular autonomic modulation during passive heating protocols: A systematic review. Physiol. Meas. 2023, 44, 01TR01. [Google Scholar] [CrossRef]
- Cooper, V.; Hainsworth, R. Effects of head-up tilting on baroreceptor control in subjects with different tolerances to orthostatic stress. Clin. Sci. 2002, 103, 221–226. [Google Scholar] [CrossRef]
- Bahjaoui-Bouhaddi, M.; Henriet, M.T.; Cappelle, S.; Dumoulin, G.; Regnard, J. Active standing and passive tilting similarly reduce the slope of spontaneous baroreflex in healthy subjects. Heart Circ. Physiol. 1998, 47, 227–236. [Google Scholar]
- Samniah, N.; Sakaguchi, S.; Ermis, C.; Lurie, K.G.; Benditt, D.G. Transient modification of baroreceptor response during tilt-induced vasovagal syncope. Europace 2004, 6, 48–54. [Google Scholar] [CrossRef]
- Pitzalis, M.; Parati, G.; Massari, F.; Guida, P.; Rienzo, M.; Rizzon, B.; Castiglioni, P.; Iacoviello, M.; Mastropasqua, F.; Rizzon, P. Enhanced reflex response to baroreceptor deactivation in subjects with tilt-Induced syncope. J. Am. Coll. Cardiol. 2003, 41, 1167–1173. [Google Scholar] [CrossRef]
- Wieling, W.; Karemaker, J.M. Measurement of Heart Rate and Blood Pressure to Evaluate Disturbances in Neurocardiovascular Control; Oxford University Press: Oxford, UK, 1999; pp. 196–210. [Google Scholar]
- Mukkamala, R.; Cohen, R.J.; Aletti, F.; Ferrario, M.; Xu, D.; Greaves, D.K.; Shoemaker, J.K.; Arbeille, P.; Baselli, G.; Hughson, R.L.; et al. A forward model-based validation of cardiovascular system identification. Am. J. Physiol. Heart Circ. Physiol. 2001, 281, H2714–H2730. [Google Scholar] [CrossRef]
- Aletti, F.; Hammond, R.L.; A Sala-Mercado, J.; Chen, X.; O’Leary, D.S.; Baselli, G.; Mukkamala, R. Cardiac output is not a significant source of low frequency mean arterial pressure variability. Physiol. Meas. 2013, 34, 1207–1216. [Google Scholar] [CrossRef]


| Variable | PAF Group | HI Group |
|---|---|---|
| (n = 68) | (n = 34) | |
| Age, years | 53 ± 14 | 49 ± 12 |
| Male gender, % | 47.0 | 36.3 |
| BMI | 26.9 ± 3.6 | 25.0 ± 2.7 |
| Heart rate, bpm | 70 ± 10 | 72 ± 5.8 |
| Systolic blood pressure, mmHg | 121 ± 4.3 | 115 ± 8.3 |
| Diastolic blood pressure, mmHg | 81 ± 5.5 | 76 ± 5.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, M.; Laranjo, S.; Cunha, P.; Geraldes, V.; Oliveira, M.; Rocha, I. Orthostatic Stress and Baroreflex Sensitivity: A Window into Autonomic Dysfunction in Lone Paroxysmal Atrial Fibrillation. J. Clin. Med. 2023, 12, 5857. https://doi.org/10.3390/jcm12185857
Ferreira M, Laranjo S, Cunha P, Geraldes V, Oliveira M, Rocha I. Orthostatic Stress and Baroreflex Sensitivity: A Window into Autonomic Dysfunction in Lone Paroxysmal Atrial Fibrillation. Journal of Clinical Medicine. 2023; 12(18):5857. https://doi.org/10.3390/jcm12185857
Chicago/Turabian StyleFerreira, Mónica, Sérgio Laranjo, Pedro Cunha, Vera Geraldes, Mário Oliveira, and Isabel Rocha. 2023. "Orthostatic Stress and Baroreflex Sensitivity: A Window into Autonomic Dysfunction in Lone Paroxysmal Atrial Fibrillation" Journal of Clinical Medicine 12, no. 18: 5857. https://doi.org/10.3390/jcm12185857





