The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria
Abstract
:1. Introduction
2. Methods
3. Results
3.1. ECOHIS-G
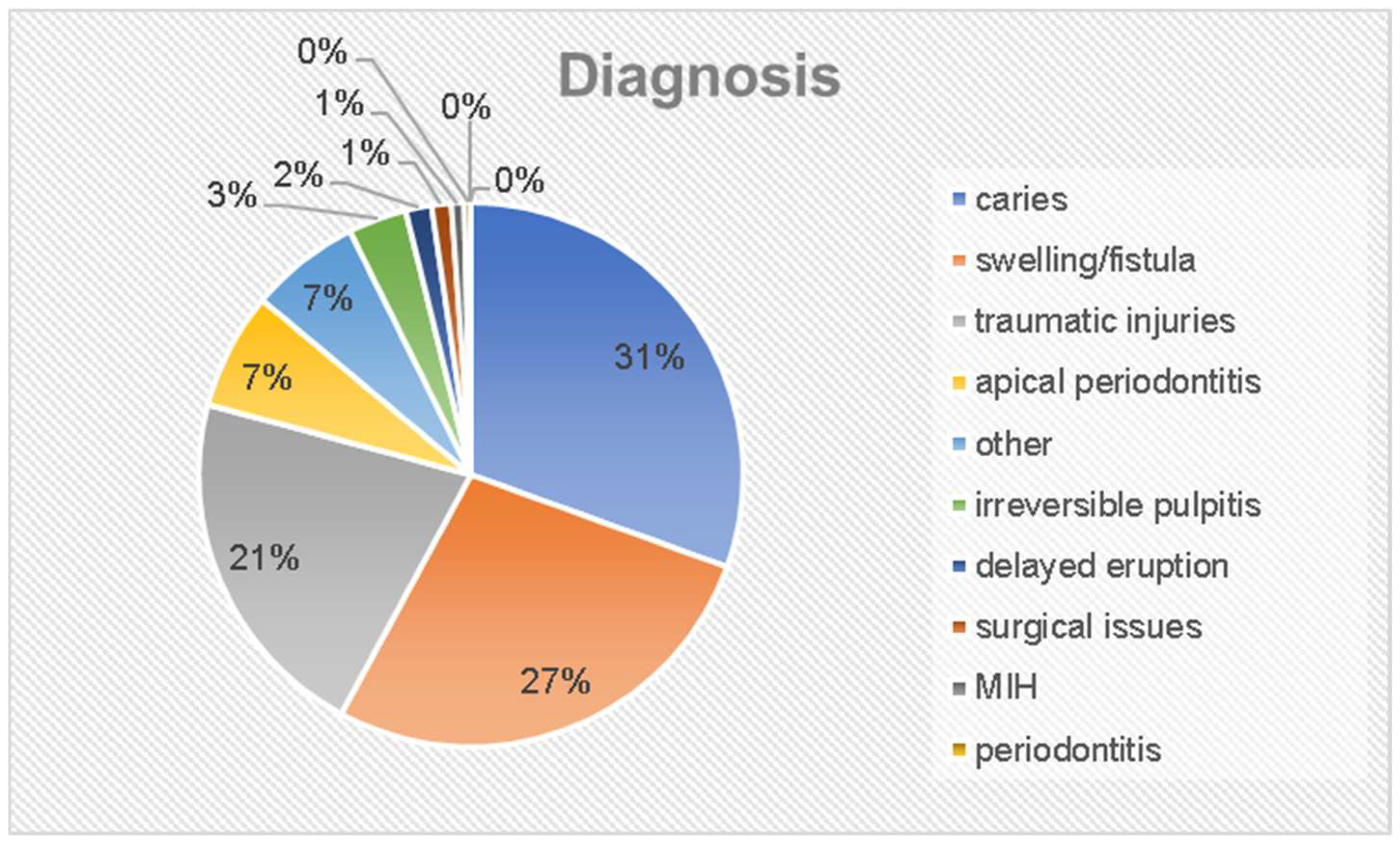
3.2. Clinical Screening
3.3. Correlation Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raja, S.N.; Carr, D.B.; Cohen, M.; Finnerup, N.B.; Flor, H.; Gibson, S.; Keefe, F.J.; Mogil, J.S.; Ringkamp, M.; Sluka, K.A.; et al. The revised International Association for the Study of Pain definition of pain: Concepts, challenges, and compromises. Pain 2020, 161, 1976–1982. [Google Scholar] [CrossRef]
- Ortiz, F.R.; Tomazoni, F.; Oliveira, M.D.; Piovesan, C.; Mendes, F.; Ardenghi, T.M. Toothache, associated factors, and its impact on Oral Health-Related Quality of Life (OHRQoL) in preschool children. Braz. Dent. J. 2014, 25, 546–553. [Google Scholar] [CrossRef]
- Mashoto, K.O.; Astrom, A.N.; David, J.; Masalu, J.R. Dental pain, oral impacts and perceived need for dental treatment in Tanzanian school students: A cross-sectional study. Health Qual. Life Outcomes 2009, 7, 73. [Google Scholar] [CrossRef]
- Pau, A.K.; Croucher, R.; Marcenes, W. Prevalence estimates and associated factors for dental pain: A review. Oral Health Prev. Dent. 2003, 1, 209–220. [Google Scholar] [PubMed]
- Lewis, C.; Stout, J. Toothache in US children. Arch. Pediatr. Adolesc. Med. 2010, 164, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, M.M.; Colares, V. The relationship between dental anxiety and dental pain in children aged 18 to 59 months: A study in Recife, Pernambuco State, Brazil. Cad. Saude Publica 2009, 25, 743–750. [Google Scholar] [CrossRef]
- Barretto, E.P.; Ferreira, E.F.; Pordeus, I.A. Determinant factors of toothache in 8- and 9-year-old schoolchildren, Belo Horizonte, MG, Brazil. Braz. Oral Res. 2009, 23, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Boeira, G.F.; Correa, M.B.; Peres, K.G.; Peres, M.A.; Santos, I.S.; Matijasevich, A.; Barros, A.J.; Demarco, F.F. Caries is the main cause for dental pain in childhood: Findings from a birth cohort. Caries Res. 2012, 46, 488–495. [Google Scholar] [CrossRef]
- Zhang, K.; Li, J.; Lu, Z. The Prevalence of Dental Caries in Primary Dentition in 3- to 5-Year-Old Preschool Children in Northern China. BioMed Res. Int. 2020, 2020, 5315236. [Google Scholar] [CrossRef]
- Al-Meedani, L.A.; Al-Dlaigan, Y.H. Prevalence of dental caries and associated social risk factors among preschool children in Riyadh, Saudi Arabia. Pak. J. Med. Sci. 2016, 32, 452–456. [Google Scholar] [CrossRef]
- Wagner, Y.; Greiner, S.; Heinrich-Weltzien, R. Evaluation of an oral health promotion program at the time of birth on dental caries in 5-year-old children in Vorarlberg, Austria. Community Dent. Oral Epidemiol. 2014, 42, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Aldrigui, J.M.; Abanto, J.; Carvalho, T.S.; Mendes, F.M.; Wanderley, M.T.; Bonecker, M.; Raggio, D.P. Impact of traumatic dental injuries and malocclusions on quality of life of young children. Health Qual. Life Outcomes 2011, 9, 78. [Google Scholar] [CrossRef]
- Berkowitz, R. Etiology of nursing caries: A microbiologic perspective. J. Public Health Dent. 1996, 56, 51–54. [Google Scholar] [CrossRef] [PubMed]
- Colak, H.; Dulgergil, C.T.; Dalli, M.; Hamidi, M.M. Early childhood caries update: A review of causes, diagnoses, and treatments. J. Nat. Sci. Biol. Med. 2013, 4, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Espinoza, G.; Muñoz Millán, P.; Vergara-González, C.; Atala-Acevedo, C.; Zaror, C. Prevalence of early childhood caries in non-fluoridated rural areas of Chile. J. Oral Res. 2016, 5, 307–313. [Google Scholar] [CrossRef]
- Phantumvanit, P.; Makino, Y.; Ogawa, H.; Rugg-Gunn, A.; Moynihan, P.; Petersen, P.E.; Evans, W.; Feldens, C.A.; Lo, E.; Khoshnevisan, M.H.; et al. WHO Global Consultation on Public Health Intervention against Early Childhood Caries. Community Dent. Oral Epidemiol. 2018, 46, 280–287. [Google Scholar] [CrossRef]
- Casamassimo, P.S.; Thikkurissy, S.; Edelstein, B.L.; Maiorini, E. Beyond the dmft: The human and economic cost of early childhood caries. J. Am. Dent. Assoc. 2009, 140, 650–657. [Google Scholar] [CrossRef]
- Sischo, L.; Broder, H.L. Oral health-related quality of life: What, why, how, and future implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef]
- McGrath, C.; Broder, H.; Wilson-Genderson, M. Assessing the impact of oral health on the life quality of children: Implications for research and practice. Community Dent. Oral Epidemiol. 2004, 32, 81–85. [Google Scholar] [CrossRef]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef]
- Von Baeyer, C.L.; Spagrud, L.J. Systematic review of observational (behavioral) measures of pain for children and adolescents aged 3 to 18 years. Pain 2007, 127, 140–150. [Google Scholar] [CrossRef]
- Jabarifar, S.E.; Golkari, A.; Ijadi, M.H.; Jafarzadeh, M.; Khadem, P. Validation of a Farsi version of the early childhood oral health impact scale (F-ECOHIS). BMC Oral Health 2010, 10, 4. [Google Scholar] [CrossRef]
- Peker, K.; Uysal, O.; Bermek, G. Cross—cultural adaptation and preliminary validation of the Turkish version of the early childhood oral health impact scale among 5–6-year-old children. Health Qual. Life Outcomes 2011, 9, 118. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Veronneau, J.; Allison, P.J. Validation of a French language version of the Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2008, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Farsi, N.J.; El-Housseiny, A.A.; Farsi, D.J.; Farsi, N.M. Validation of the Arabic Version of the Early Childhood Oral Health Impact Scale (ECOHIS). BMC Oral Health 2017, 17, 60. [Google Scholar] [CrossRef]
- Scarpelli, A.C.; Oliveira, B.H.; Tesch, F.C.; Leao, A.T.; Pordeus, I.A.; Paiva, S.M. Psychometric properties of the Brazilian version of the Early Childhood Oral Health Impact Scale (B-ECOHIS). BMC Oral Health 2011, 11, 19. [Google Scholar] [CrossRef]
- Bekes, K.; Omara, M.; Safar, S.; Stamm, T. The German version of Early Childhood Oral Health Impact Scale (ECOHIS-G): Translation, reliability, and validity. Clin. Oral Investig. 2019, 23, 4449–4454. [Google Scholar] [CrossRef] [PubMed]
- Martins, M.T.; Sardenberg, F.; Vale, M.P.; Paiva, S.M.; Pordeus, I.A. Dental caries and social factors: Impact on quality of life in Brazilian children. Braz. Oral Res. 2015, 29, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Petersen, P.E.; Ramon, J.I. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization (WHO): Geneva, Switzerland, 2013.
- Schuch, H.S.; Costa Fdos, S.; Torriani, D.D.; Demarco, F.F.; Goettems, M.L. Oral health-related quality of life of schoolchildren: Impact of clinical and psychosocial variables. Int. J. Paediatr. Dent. 2015, 25, 358–365. [Google Scholar] [CrossRef]
- Gomes, M.C.; Clementino, M.A.; Pinto-Sarmento, T.C.; Martins, C.C.; Granville-Garcia, A.F.; Paiva, S.M. Association between parental guilt and oral health problems in preschool children: A hierarchical approach. BMC Public Health 2014, 14, 854. [Google Scholar] [CrossRef]
- Pesaressi, E.; Villena, R.S.; Frencken, J.E. Dental caries and oral health-related quality of life of 3-year-olds living in Lima, Peru. Int. J. Paediatr. Dent. 2020, 30, 57–65. [Google Scholar] [CrossRef]
- Rajab, L.D.; Abdullah, R.B. Impact of Dental Caries on the Quality of Life of Preschool Children and Families in Amman, Jordan. Oral Health Prev. Dent. 2020, 18, 571–582. [Google Scholar] [CrossRef] [PubMed]
- Randrianarivony, J.; Ravelomanantsoa, J.J.; Razanamihaja, N. Evaluation of the reliability and validity of the Early Childhood Oral Health Impact Scale (ECOHIS) questionnaire translated into Malagasy. Health Qual. Life Outcomes 2020, 18, 39. [Google Scholar] [CrossRef] [PubMed]
- Zaror, C.; Atala-Acevedo, C.; Espinoza-Espinoza, G.; Munoz-Millan, P.; Munoz, S.; Martinez-Zapata, M.J.; Ferrer, M. Cross-cultural adaptation and psychometric evaluation of the early childhood oral health impact scale (ECOHIS) in chilean population. Health Qual. Life Outcomes 2018, 16, 232. [Google Scholar] [CrossRef] [PubMed]
- Ismail, N.S.; Ghani, N.M.A.; Supaat, S.; Kharuddin, A.F.; Dewi Ardini, Y. The early childhood oral health impact scale (ECOHIS): Assessment tool in oral health related quality of life. J. Int. Dent. Med. Res. 2018, 11, 162–168. [Google Scholar]
- Antunes, L.A.A.; Ornellas, G.; Fraga, R.S.; Antunes, L.S. Oral health outcomes: The association of clinical and socio-dental indicators to evaluate dental caries in preschool children. Cien Saude Colet. 2018, 23, 491–500. [Google Scholar] [CrossRef]
- Fernandes, I.B.; Souto-Souza, D.; Primo-Miranda, E.F.; Marques, L.S.; Ramos-Jorge, M.L.; Ramos-Jorge, J. Perceived impact of dental pain on the quality of life of children aged 1–3 years and their families. Eur. Arch. Paediatr. Dent. 2019, 20, 557–563. [Google Scholar] [CrossRef]
- Clementino, M.A.; Pinto-Sarmento, T.C.; Costa, E.M.; Martins, C.C.; Granville-Garcia, A.F.; Paiva, S.M. Association between oral conditions and functional limitations in childhood. J. Oral Rehabil. 2015, 42, 420–429. [Google Scholar] [CrossRef]
- Stasch, N.; Ganahl, K.; Geiger, H. Soziale Ungleichheit in der Zahngesundheit von Kindern. Prävention und Gesundheitsförderung 2022, 18, 87–92. [Google Scholar] [CrossRef]
- Schiffner, U. Caries Decline in Preschool Children from Low Social Classes and with Migration Background in Hamburg, Germany: Outcome from Repeated Cross-Sectional Caries Epidemiological Studies. J. Clin. Med. 2022, 11, 4251. [Google Scholar] [CrossRef]
- Nair, S.; Kakodkar, P.; Shetiya, S.; Rajpurohit, L.; Kale, S. Impact of different levels of caries experience on the quality of life of preschool children and their families in Pimpri, Pune: A cross-sectional study. J. Indian Assoc. Public Health Dent. 2018, 16, 193–197. [Google Scholar] [CrossRef]
- Ismail, A.I.; Sohn, W.; Tellez, M.; Amaya, A.; Sen, A.; Hasson, H.; Pitts, N.B. The International Caries Detection and Assessment System (ICDAS): An integrated system for measuring dental caries. Community Dent. Oral Epidemiol. 2007, 35, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Leal, S.C.; Bronkhorst, E.M.; Fan, M.; Frencken, J.E. Untreated cavitated dentine lesions: Impact on children’s quality of life. Caries Res. 2012, 46, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Nomura, L.H.; Bastos, J.L.; Peres, M.A. Dental pain prevalence and association with dental caries and socioeconomic status in schoolchildren, Southern Brazil, 2002. Braz. Oral Res. 2004, 18, 134–140. [Google Scholar] [CrossRef]

| Clinical Data | Group | n | Mean Value | SD | Min | Max |
|---|---|---|---|---|---|---|
| age | study group | 259 | 4.2 | 1.5 | 0 | 6 |
| control group | 259 | 4.2 | 1.5 | 0 | 6 | |
| dmf-t | study group | 259 | 6.2 | 5.1 | 0 | 20 |
| control group | 259 | 3.9 | 4.8 | 0 | 20 | |
| dmf-s | study group | 219 | 12.5 | 13.5 | 0 | 78 |
| control group | 256 | 8.5 | 13.0 | 0 | 80 | |
| plaque-index | study group | 259 | 64% | 0.5 | 0 | 1 |
| control group | 259 | 50% | 0.5 | 0 | 1 |
| No. | Question | Mean Value S (SD) | Mean Value C (SD) | Difference S-C | p-Value |
|---|---|---|---|---|---|
| 1 | How often has you child had pain in his/her teeth, mouth or jaws? | 2 (6.2) | 1.6 (8.2) | 0.4 | 0.457 |
| How often has you child … due to dental problems or dental care? | |||||
| 2 | had difficulty drinking hot or cold drinks | 0.8 (0.1) | 0.3 (0.7) | 0.5 | <0.001 |
| 3 | had difficulty eating some foods | 1.1 (1.3) | 0.4 (0.8) | 0.7 | <0.001 |
| 4 | had difficulty pronouncing some words? | 0.5 (1.0) | 0.5 (1.0) | 0 | 0.596 |
| 5 | missed preschool, day care or school | 0.9 (6.2) | 1.5 (10.6) | −0.6 | 0 495 |
| 6 | had trouble sleeping | 1.1 (6.2) | 0.4 (0.7) | 0.7 | 0.061 |
| 7 | been irritable or frustrated | 1.1 (6.2) | 0.8 (6.2) | 0.3 | 0.604 |
| 8 | avoided smiling or laughing | 0.2 (0.7) | 0.1 (0.4) | 0.1 | 0.010 |
| 9 | avoided talking | 0.2 (0.5) | 0.1 (0.4) | 0.1 | 0.056 |
| How often have you or another family member … because of your child’s dental problems or dental care? | |||||
| 10 | been upset | 0.7 (1.1) | 0.3 (0.8) | 0.4 | <0.001 |
| 11 | felt guilty | 0.9 (1.2) | 0.5 (1.0) | 0.4 | 0.001 |
| 12 | taken time off of work | 0.7 (1.0) | 0.5 (0.9) | 02 | 0.127 |
| 13 | been financially impacted | 0.8 (6.2) | 0.2 (0.7) | 0.6 | 0.166 |
| ECOHIS Subsection | Mean Value S (SD) | Mean Value C (SD) | Difference S-C | p-Value |
|---|---|---|---|---|
| Child Impact Section (CIS) | 6.4 (5.6) | 3.3 (4.1) | 3.1 | <0.001 |
| Family Impact Section (FIS) | 2.6 (2.8) | 1.6 (2.5) | 1 | <0.001 |
| ECOHIS-G sum | 9.0 (7.4) | 4.9 (5.6) | 4.1 | <0.001 |
| Clinical Parameter | Mean Value (S) (SD) | Mean Value (C) (SD) | Difference S-C | p-Value |
|---|---|---|---|---|
| dmf-t | 6.2 (5.1) | 3.9 (4.8) | 2.3 | <0.001 |
| dmf-s | 12.5 (13.5) | 8.5 (13.0) | 4 | <0.001 |
| plaque | 0.6 (0.5) | 0.5 (0.5) | 0.1 | 0.002 |
| Correlations | Child Impact Section (CIS) | Family Impact Section (FIS) | ECOHIS Sum | |
|---|---|---|---|---|
| overall well-being | Spearman correlation | 0.236 | 0.173 | 0.382 |
| p-value | 0.000 | 0.005 | 0.000 | |
| global oral health | Spearman correlation | 0.478 | 0.387 | 0.631 |
| p-value | 0.000 | 0.000 | 0.000 | |
| dmf-t | Pearson correlation | 0.174 | −0.034 | 0.183 |
| p-value | 0.005 | 0.584 | 0.003 | |
| plaque | Pearson correlation | 0.173 | −0.005 | 0.182 |
| p-value | 0.005 | 0.940 | 0.003 | |
| Correlation | Overall Well-Being | Global Oral Health | |
|---|---|---|---|
| dmf-t | Spearman correlation | 0.172 | 0.573 |
| p-value | 0.006 | <0.001 | |
| plaque | Chi2 correlation | ||
| p-value | 0.028 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lembacher, S.; Hofer, V.; Bekes, K. The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria. J. Clin. Med. 2023, 12, 5906. https://doi.org/10.3390/jcm12185906
Lembacher S, Hofer V, Bekes K. The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria. Journal of Clinical Medicine. 2023; 12(18):5906. https://doi.org/10.3390/jcm12185906
Chicago/Turabian StyleLembacher, Sophie, Viktoria Hofer, and Katrin Bekes. 2023. "The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria" Journal of Clinical Medicine 12, no. 18: 5906. https://doi.org/10.3390/jcm12185906
APA StyleLembacher, S., Hofer, V., & Bekes, K. (2023). The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria. Journal of Clinical Medicine, 12(18), 5906. https://doi.org/10.3390/jcm12185906







