Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement
Abstract
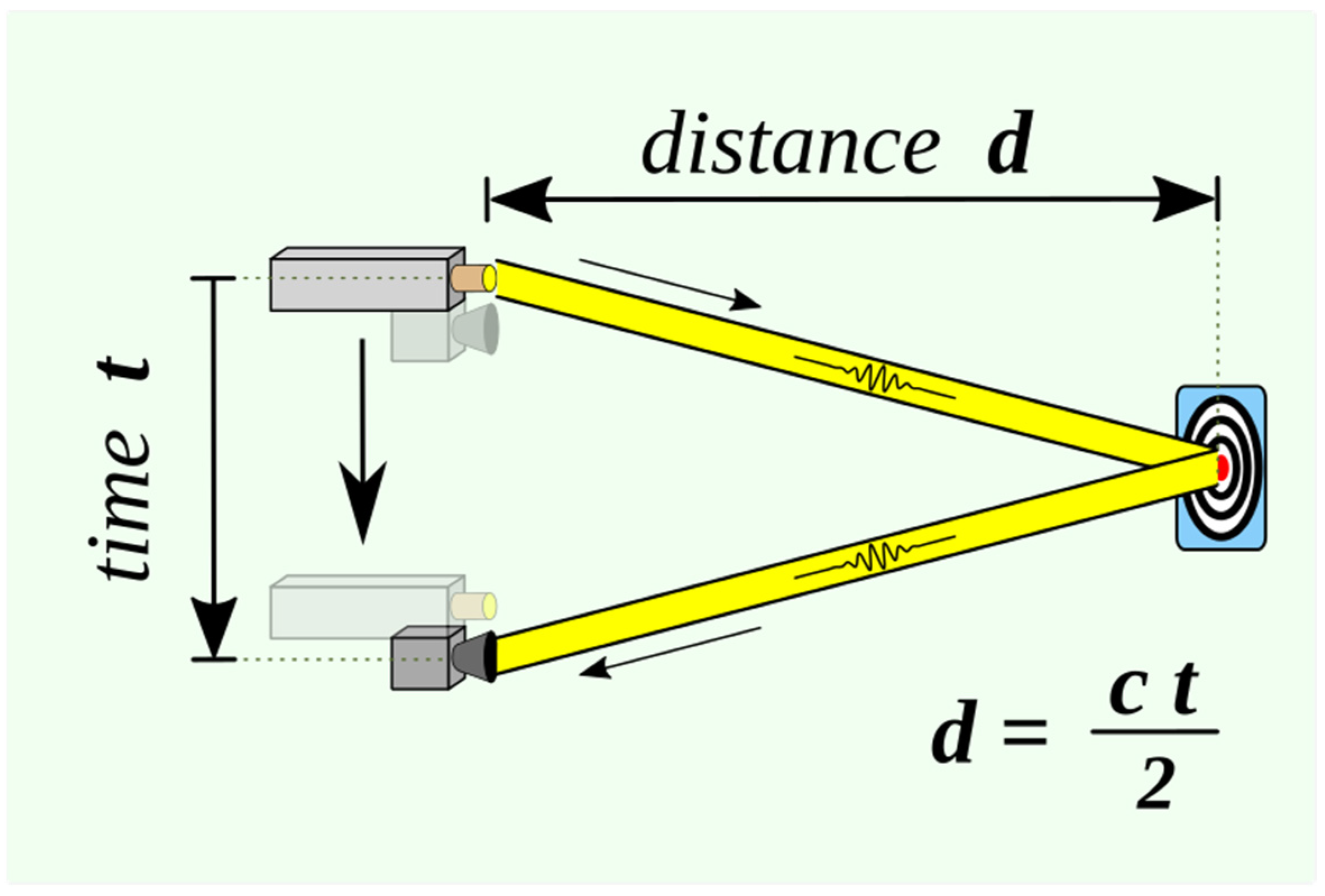
:1. Introduction
2. Materials and Methods
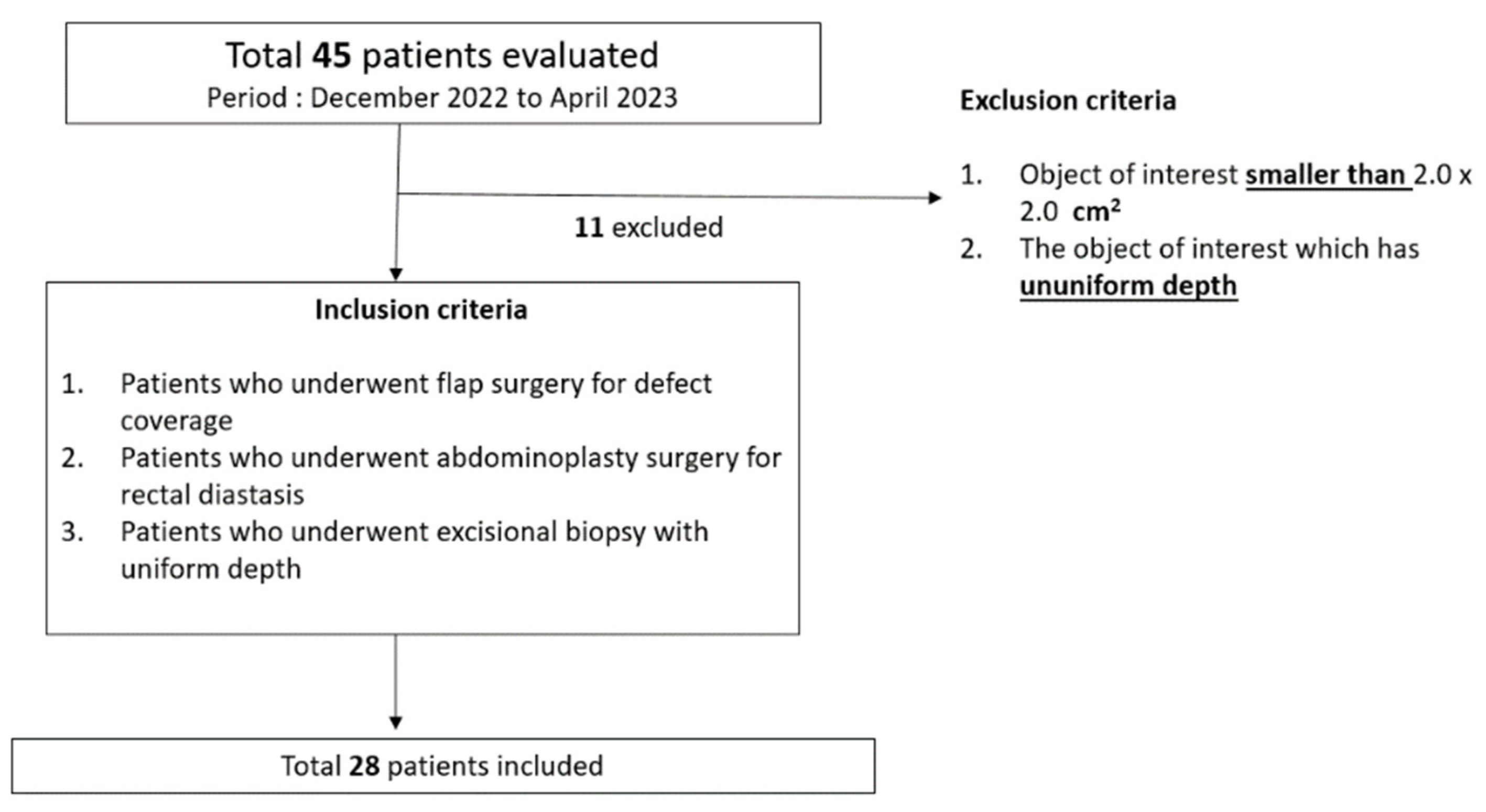
2.1. Study Design and Patient Selection
- Exclusion criteria:
- ○
- Object of interest (mass, wound, or flap) smaller than 2.0 × 2.0 cm2.
- ○
- Object of interest (mass, wound, or flap) with uneven depth that may cause inaccurate recognition by LiDAR-based surface-area scanning.
- Inclusion criteria:
- ○
- Patients who underwent flap surgery for defect coverage.
- ○
- Patients who underwent abdominoplasty surgery for rectal diastasis.
- ○
- Patients who underwent excisional biopsy with uniform depth.
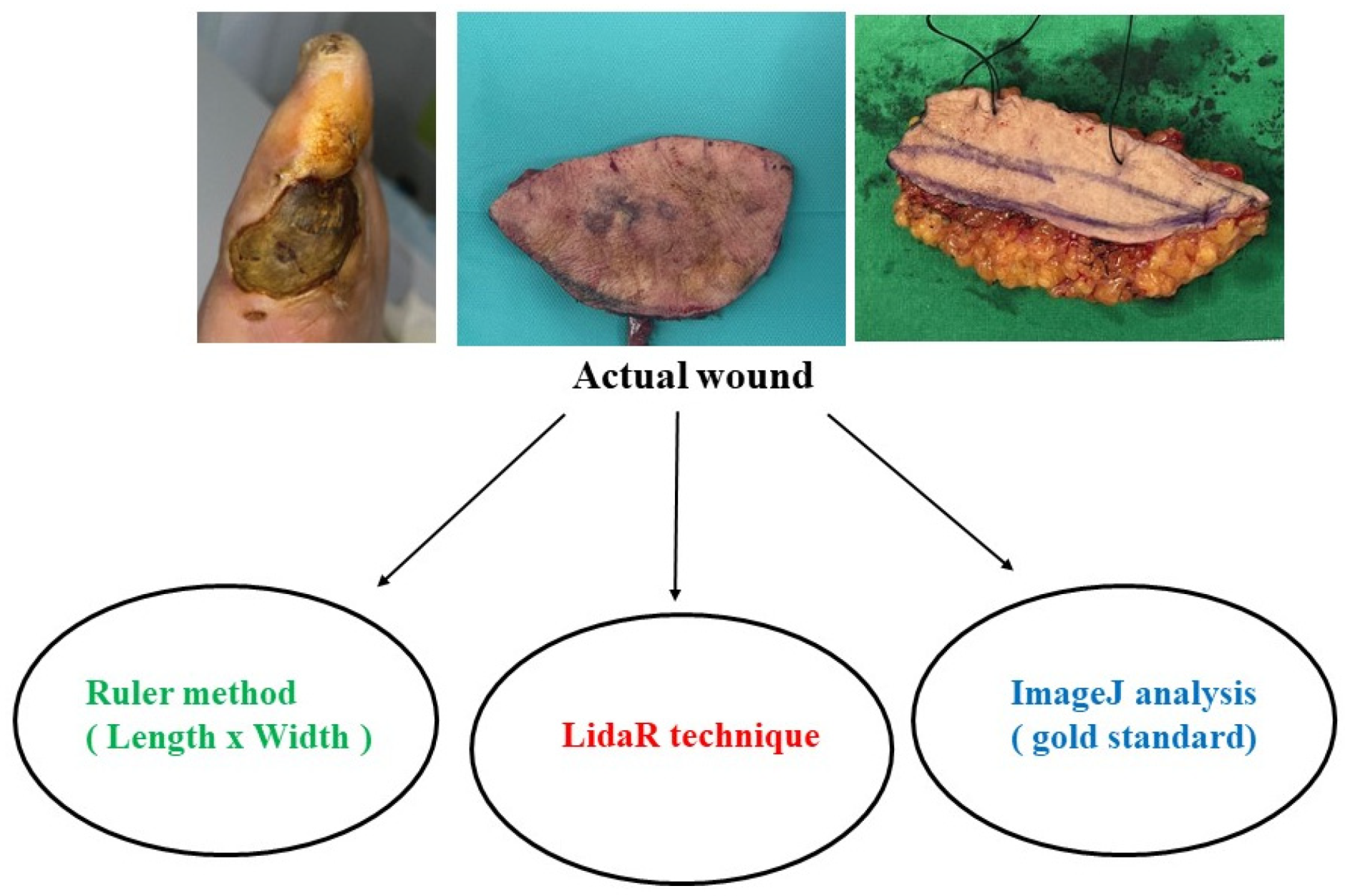
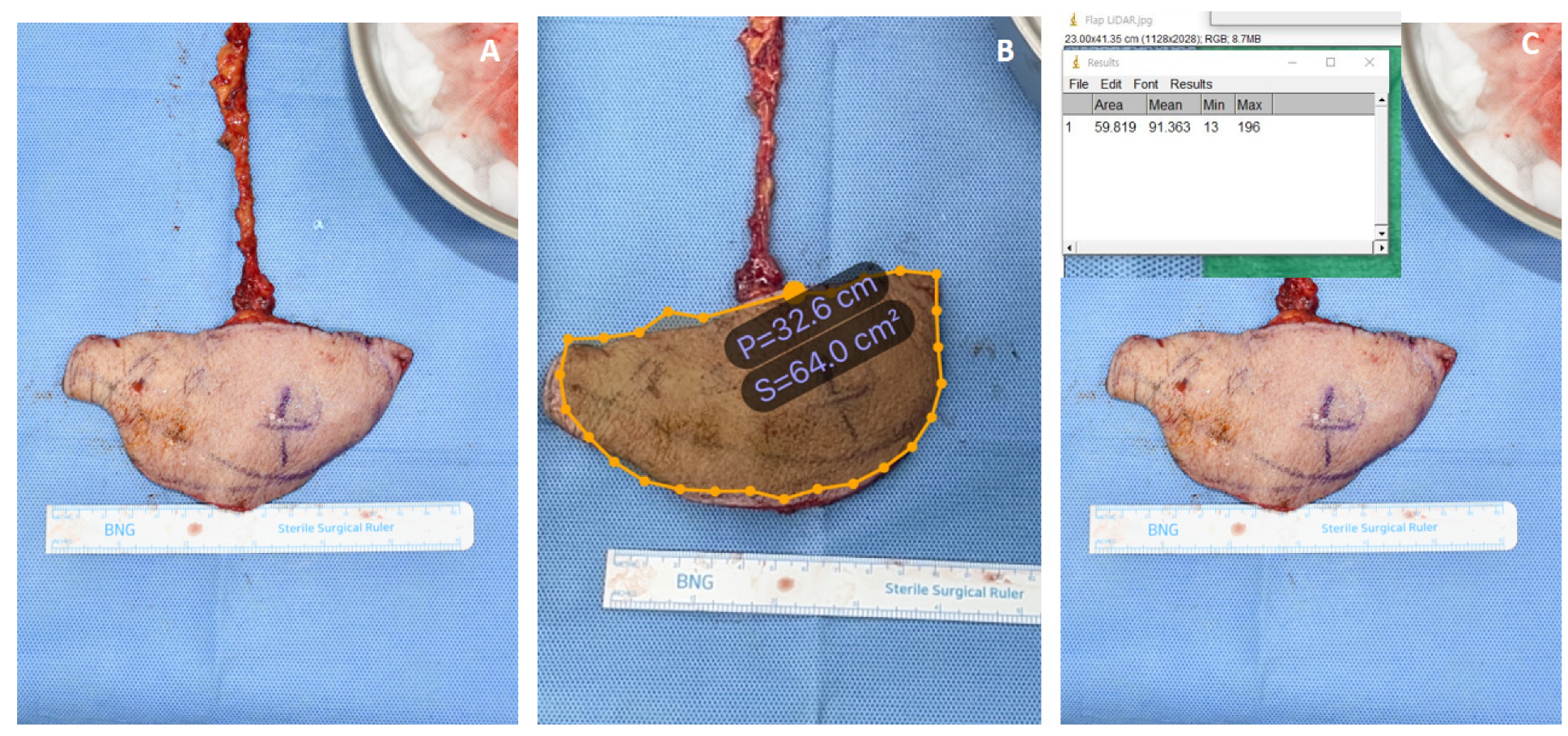
2.2. Measurement Methods
- (1)
- Traditional ruler-based rectangular method
- (2)
- LiDAR technique-based method (AR Ruler App: Tape Measure Cam, GRYMALA Company, Minsk, Belarus)
- (3)
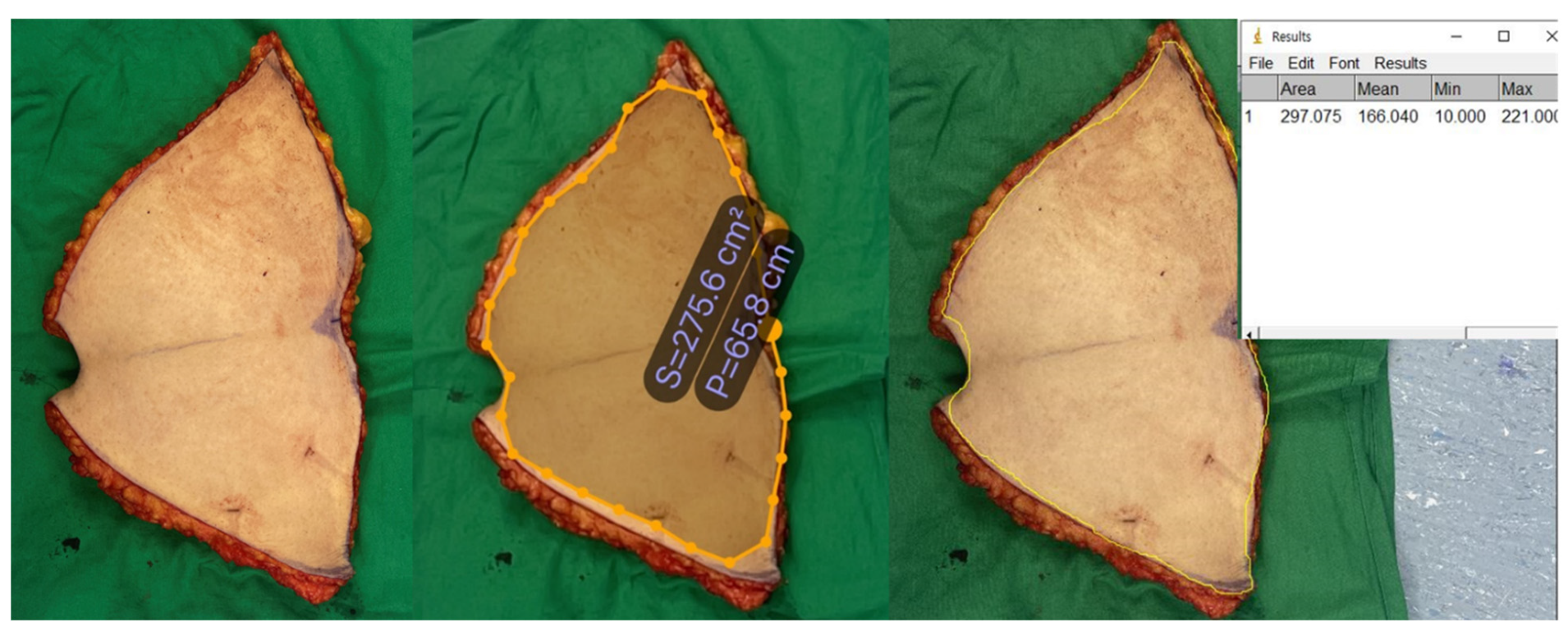
- ImageJ analysis
- ImageJ software(version 1.53t) was opened.
- File > Open (Alternatively, the picture can be dragged and dropped into the software).
- A segment was drawn along the ruler using the “straight line” tool. The examiners drew a 1 cm line along the ruler. The software then calculated the distance in the pixels of the segment.
- Analyze menu > set scale > known distance (we used 1) > unit of length (cm). The software automatically recalculated the number of pixels in cm.
- The wound outline was created using the “Freehand selections” tool by tracing the wound shape with the computer mouse (desktop computers) or trackpad (laptops).
- Analyze menu > measure. The area was calculated in cm2.
- A screenshot was taken of the screen along with the measurement window to save in the database.
2.3. Statistical Analyses
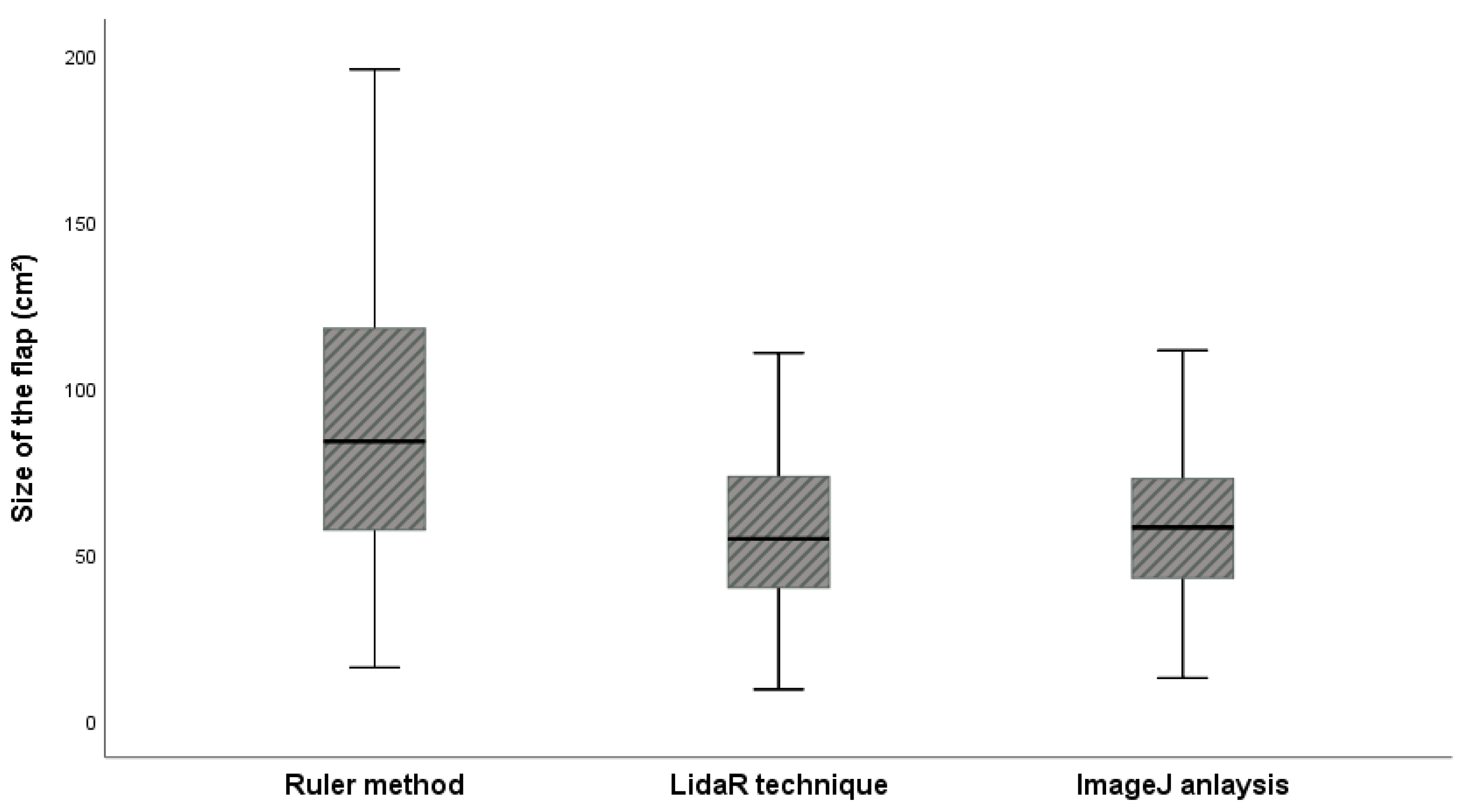
3. Results
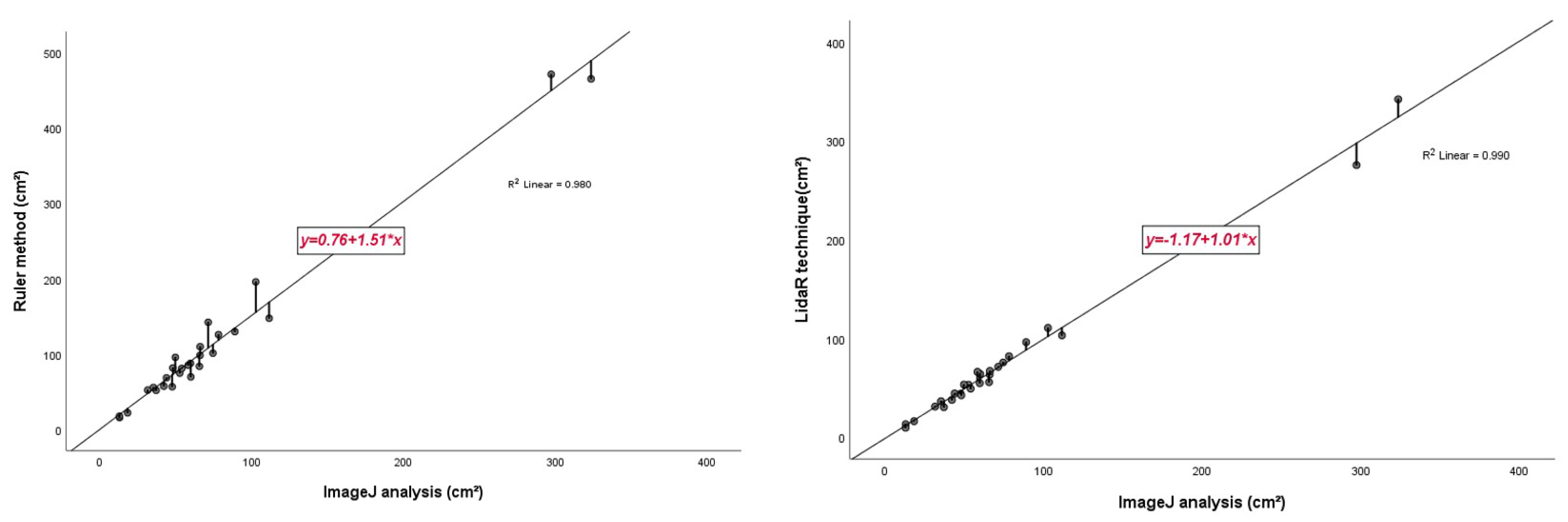
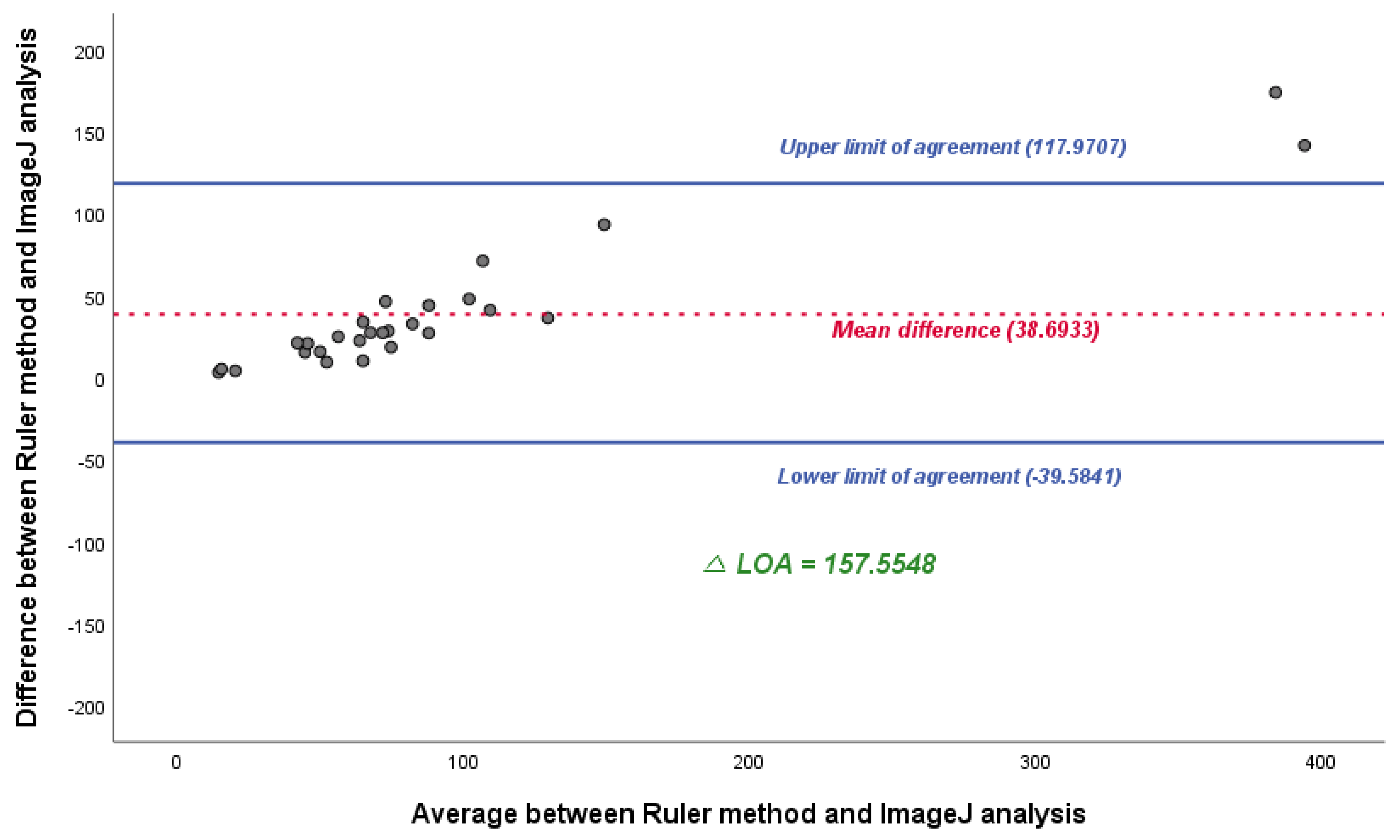
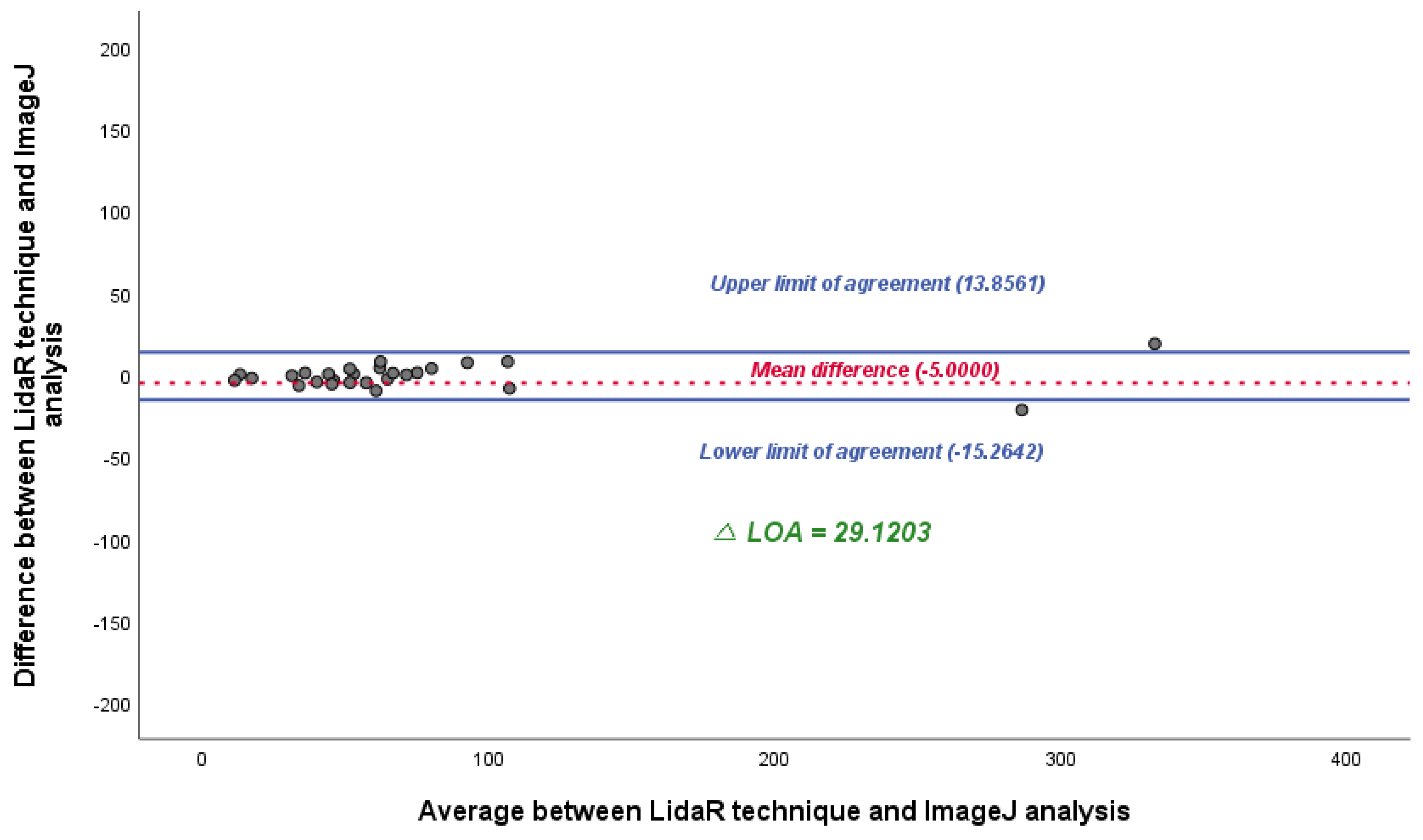
3.1. Statistical Interpretation
3.2. Representative Patients
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bowling, F.L.; King, L.; Fadavi, H.; Paterson, J.A.; Preece, K.; Daniel, R.W.; Matthews, D.J.; Boulton, A.J. An Assessment of the Accuracy and Usability of a Novel Optical Wound Measurement System. Diabet. Med. 2009, 26, 93–96. [Google Scholar] [CrossRef] [PubMed]
- van Rijswijk, L. Computer-Assisted Wound Assessment and Care Education Program in Registered Nurses: Use of an Interactive Online Program by 418 Registered Nurses. J. Wound Ostomy. Continence. Nurs. 2019, 46, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Yee, A.; Harmon, J.; Yi, S. Quantitative Monitoring Wound Healing Status Through Three-Dimensional Imaging on Mobile Platforms. J. Am. Coll. Clin. Wound Spec. 2016, 8, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Papazoglou, E.S.; Zubkov, L.; Mao, X.; Neidrauer, M.; Rannou, N.; Weingarten, M.S. Image Analysis of Chronic Wounds for Determining the Surface Area. Wound Repair Regen. 2010, 18, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Chazette, P.; Totems, J.; Hespel, L.; Bailly, J.-S. Principle and Physics of the LiDAR Measurement. In Optical Remote Sensing of Land Surface; Elsevier: Amsterdam, The Netherlands, 2016; pp. 201–247. [Google Scholar]
- Lohani, B.; Ghosh, S. Airborne LiDAR Technology: A Review of Data Collection and Processing Systems. Proc. Natl. Acad. Sci. India Sect. A Phys. Sci. 2017, 87, 567–579. [Google Scholar] [CrossRef]
- Luetzenburg, G.; Kroon, A.; Bjørk, A.A. Evaluation of the Apple IPhone 12 Pro LiDAR for an Application in Geosciences. Sci. Rep. 2021, 11, 22221. [Google Scholar] [CrossRef] [PubMed]
- Rosell Polo, J.R.R.; Sanz, R.; Llorens, J.; Arnó, J.; Escolà, A.; Ribes-Dasi, M.; Masip, J.; Camp, F.; Gràcia, F.; Solanelles, F.; et al. A Tractor-Mounted Scanning LIDAR for the Non-destructive Measurement of Vegetative Volume and Surface Area of Tree-Row Plantations: A Comparison with Conventional Destructive Measurements. Biosyst. Eng. 2009, 102, 128–134. [Google Scholar] [CrossRef]
- Schickler, W.; Thorpe, A. Surface Estimation Based on LIDAR. In Proceedings of the ASPRS Annual Conference, St. Louis, MO, USA, 23–27 April 2001; pp. 23–27. [Google Scholar]
- Stockton, K.A.; McMillan, C.M.; Storey, K.J.; David, M.C.; Kimble, R.M. 3D Photography Is as Accurate as Digital Planimetry Tracing in Determining Burn Wound Area. Burns 2015, 41, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Aragón-Sánchez, J.; Quintana-Marrero, Y.; Aragón-Hernández, C.; Hernández-Herero, M.J. ImageJ: A Free, Easy, and Reliable Method to Measure Leg Ulcers Using Digital Pictures. Int. J. Low. Extrem. Wounds 2017, 16, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, M. Wound Measurement: Can It Help Us to Monitor Progression to Healing? J. Wound Care 2003, 12, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Majeske, C. Reliability of Wound Surface Area Measurements. Phys. Ther. 1992, 72, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Lim, S.Y.; Pyon, J.K.; Bang, S.I.; Oh, K.S.; Mun, G.H. Reliable Harvesting of a Large Thoracodorsal Artery Perforator Flap with Emphasis on Perforator Number and Spacing. Plast. Reconstr. Surg. 2011, 128, 140e–150e. [Google Scholar] [CrossRef] [PubMed]

| Methods | Advantages | Disadvantages | Examples |
|---|---|---|---|
| Traditional rectangular method | Simplest measurement method No additional device is required | Inaccuracies of up to 44% [1,2,3] | Ruler |
| LiDAR-based assessment | Easy to use No probe required for calibration | Unknown: no prior studies have investigated this technique | AR Ruler App: tape Measure Cam (not for wound analysis) |
| ImageJ surface analysis | Most common method used to assess size measurement Easy to use Can measure complex objects | Image files must be transferred to a computer Probe necessary for calibration | Wound size measurement Determination of the photosynthetic portion of a variegated leaf Particle counting in molecular biology |
| Hardware Information |
|---|
| iPhone 12 PRO MAX Key Specifications: Screen: 6.7 inches. Processor: Apple A14 Bionic. Storage: 128, 256, and 512 GB. Camera: Three 12-megapixel rear cameras; 12-megapixel front-facing camera. Weight: 226 g. List of cell phones (and devices) that Apple produces that use LiDAR technology iPhone 14 Pro Max iPhone 14 Pro iPhone 13 Pro Max iPhone 13 Pro iPhone 12 Pro iPhone 12 Pro Max iPad Pro (2020 Version and Later) |
| Ruler | LiDAR | ImageJ | |
|---|---|---|---|
| N | 28 | 28 | 28 |
| Average | 112.99 | 73.59 | 74.29 |
| Standard Deviation (SD) | 110.07 | 72.97 | 72.15 |
| Range | 455.05 | 332.90 | 310.56 |
| Minimum | 15.99 | 9.40 | 12.80 |
| Maximum | 471.04 | 342.30 | 323.36 |
| Ruler | LiDAR | ImageJ | ||
|---|---|---|---|---|
| Ruler | Pearson Correlation | 1 | 0.984 ** | 0.990 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 28 | 28 | 28 | |
| LiDAR | Pearson Correlation | 0.984 ** | 1 | 0.995 ** |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 28 | 28 | 28 | |
| ImageJ | Pearson Correlation | 0.990 ** | 0.995 ** | 1 |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 28 | 28 | 28 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, B.; Kim, J.; Kwon, H.; Kim, S.; Oh, S.-H.; Ha, Y.; Song, S.-H. Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement. J. Clin. Med. 2023, 12, 6042. https://doi.org/10.3390/jcm12186042
Song B, Kim J, Kwon H, Kim S, Oh S-H, Ha Y, Song S-H. Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement. Journal of Clinical Medicine. 2023; 12(18):6042. https://doi.org/10.3390/jcm12186042
Chicago/Turabian StyleSong, Bokeun, Jeonghee Kim, Hyeokjae Kwon, Sunje Kim, Sang-Ha Oh, Yooseok Ha, and Seung-Han Song. 2023. "Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement" Journal of Clinical Medicine 12, no. 18: 6042. https://doi.org/10.3390/jcm12186042
APA StyleSong, B., Kim, J., Kwon, H., Kim, S., Oh, S.-H., Ha, Y., & Song, S.-H. (2023). Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement. Journal of Clinical Medicine, 12(18), 6042. https://doi.org/10.3390/jcm12186042






