Torticollis in Non-Syndromic Unicoronal Craniosynostosis Is Predominantly Ocular Related
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Variables
2.3. Orthoptic Measurements
- (1)
- The presence of torticollis was collected by reviewing the records of the orthoptist and ophthalmologist for the description of observed torticollis. Also, the records of the Department of Plastic and Reconstructive Surgery were scanned for descriptions of torticollis. The type of torticollis was defined as a face turn, chin elevation, chin depression, head tilt or a combination of the aforementioned. Patients were considered to have OT based on their ophthalmic and/or orthoptic diagnosis.
- (2)
- The BSV was determined using the following stereotests: Bagolini Straited Glasses (positive or negative outcome). Or, the Lang, Titmus housefly, and/or TNO tests (outcomes measured in arc seconds). Outcomes were categorized as ‘not present’ if Bagolini was negative, ‘poor’ if Bagolini was positive and Titmus housefly measured 3.552 arc seconds; ‘moderate’ if Titmus circles 200–40 arc seconds were recognized; and ‘good’ if all figures of the Lang Test (200 arc seconds) or TNO plate V (480–240 arc seconds), VI or VII (120–15 arc seconds) were positive [37].
- (3)
- The angle of the strabismus (horizontal, vertical, or combined deviations) was measured using the prism cover test at nearly (30 cm) in prism degrees. Outcomes were categorized as esotropia, exotropia, esotropia and vertical deviation, exotropia and vertical deviation, vertical deviation alone, or not present.
- (4)
- Ocular motility abnormalities were described as elevation or depression in the adduction of one or both eyes, if present. The presence of an alphabetical pattern, defined as a V- or A-strabismus pattern or not present, was also noted during the assessment of ocular motility.
- (5)
- Cyclotorsion was measured using the Maddox Double Rod test or assessed anatomically by the ophthalmologist during fundus examination. Outcomes were defined as incyclotorsion, excyclotorsion, or not present.
- (6)
- Refractive errors were obtained by retinoscopy in cycloplegia. Outcomes were defined as hypermetropia (≥+1.0 D), high hypermetropia (≥+5.0 D), myopia (≥−1.0 D), high myopia (≥−5.0 D), astigmatism (≥−1.0 D) and anisometropia (≥1.0 D).
- (7)
- The presence of amblyopia was defined as a visual acuity (VA) difference of ≥0.2 LogMAR between both eyes and was categorized as present or not present. VA was measured using the Lea Hyvarine, Amsterdam Picture Chart, tumbling E-chart, or Snellen chart depending on the age of the patient.
2.4. Statistical Methods
2.5. Reporting and Ethical Issues
3. Results
3.1. Study Characteristics and Participants
3.2. The Prevalence of Torticollis
3.3. The Ophthalmic-Related Features Associated with OT
3.3.1. Binocular Single Vision
3.3.2. Strabismus
3.3.3. Ocular Motility
3.3.4. Alphabetical Pattern
3.3.5. Cyclotorsion
3.3.6. Association between the Presence of Strabismus, Ocular Motility Abnormalities and Alphabetical Patterns
3.3.7. Refractive Error
3.3.8. Amblyopia
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Proctor, M.R.; Meara, J.G. A Review of the Management of Single-Suture Craniosynostosis, Past, Present, and Future: JNSPG 75th Anniversary Invited Review Article. J. Neurosurg. Pediatr. 2019, 24, 622–631. [Google Scholar] [CrossRef] [PubMed]
- Boulet, S.L.; Rasmussen, S.A.; Honein, M.A. A Population-Based Study of Craniosynostosis in Metropolitan Atlanta, 1989–2003. Am. J. Med. Genet. A 2008, 146A, 984–991. [Google Scholar] [CrossRef] [PubMed]
- Neusel, C.; Class, D.; Eckert, A.W.; Firsching, R.; Göbel, P.; Götz, D.; Haase, R.; Jorch, G.; Köhn, A.; Kropf, S.; et al. Multicentre Approach to Epidemiological Aspects of Craniosynostosis in Germany. Br. J. Oral Maxillofac. Surg. 2018, 56, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Collett, B.R.; Aylward, E.H.; Berg, J.; Davidoff, C.; Norden, J.; Cunningham, M.L.; Speltz, M.L. Brain Volume and Shape in Infants with Deformational Plagiocephaly. Childs Nerv. Syst. 2012, 28, 1083–1090. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Hormozi, H.; Abbaszadeh-Kasbi, A.; Sharifi, G.; Davai, N.R.; Kalantar-Hormozi, A. Incidence of Familial Craniosynostosis Among Patients With Nonsyndromic Craniosynostosis. J. Craniofac. Surg. 2019, 30, e514–e517. [Google Scholar] [CrossRef] [PubMed]
- Ciurea, A.V.; Toader, C. Genetics of Craniosynostosis: Review of the Literature. J. Med. Life 2009, 2, 5. [Google Scholar]
- Bruneteau, R.; Mulliken, J. Frontal Plagiocephaly: Synostotic, Compensational, or Deformational. Plast. Reconstr. Surg. 1992, 89, 21–31. [Google Scholar] [CrossRef]
- Balaji, S.M. Unicoronal Craniosynostosis and Plagiocephaly Correction with Fronto-Orbital Bone Remodeling and Advancement. Ann. Maxillofac. Surg. 2017, 7, 108–111. [Google Scholar] [CrossRef]
- Van Vlimmeren, L.A.; Helders, P.J.M.; Van Adrichem, L.N.A.; Engelbert, R.H.H. Torticollis and Plagiocephaly in Infancy: Therapeutic Strategies. Pediatr. Rehabil. 2006, 9, 40–46. [Google Scholar] [CrossRef]
- Nucci, P.; Kushner, B.J.; Serafino, M.; Orzalesi, N. A Multi-Disciplinary Study of the Ocular, Orthopedic, and Neurologic Causes of Abnormal Head Postures in Children. Am. J. Ophthalmol. 2005, 140, 65.e1–65.e6. [Google Scholar] [CrossRef]
- Touzé, R.; Paternoster, G.; Arnaud, E.; Khonsari, R.H.; James, S.; Bremond-Gignac, D.; Robert, M.P. Ophthalmological Findings in Children with Unicoronal Craniosynostosis. Eur. J. Ophthalmol. 2022, 32, 3274–3280. [Google Scholar] [CrossRef] [PubMed]
- Stellwagen, L.; Hubbard, E.; Chambers, C.; Jones, K.L. Torticollis, Facial Asymmetry and Plagiocephaly in Normal Newborns. Arch. Dis. Child. 2008, 93, 827–831. [Google Scholar] [CrossRef] [PubMed]
- Chieffo, D.P.R.; Arcangeli, V.; Bianchi, F.; Salerni, A.; Massimi, L.; Frassanito, P.; Tamburrini, G. Single-Suture Craniosynostosis: Is There a Correlation between Preoperative Ophthalmological, Neuroradiological, and Neurocognitive Findings? Child’s Nerv. Syst. 2020, 36, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Raco, A.; Raimondi, A.J.; De Ponte, F.S.; Brunelli, A.; Bristot, R.; Bottini, D.J.; Ianetti, G. Congenital Torticollis in Association with Craniosynostosis. Child’s Nerv. Syst. 1999, 15, 163–168. [Google Scholar] [CrossRef]
- Hussein, M.A.; Yun, I.S.; Lee, D.W.; Park, H.; Oock, K.Y. Cervical Spine Dysmorphism in Congenital Muscular Torticollis. J. Craniofac. Surg. 2018, 29, 925–929. [Google Scholar] [CrossRef]
- Ben Zvi, I.; Thompson, D.N.P. Torticollis in Childhood—A Practical Guide for Initial Assessment. Eur. J. Pediatr. 2022, 181, 865–873. [Google Scholar] [CrossRef]
- Tomczak, K.K.; Rosman, N.P. Torticollis. J. Child Neurol. 2012, 28, 365–378. [Google Scholar] [CrossRef]
- Turan, K.E.; Şekeroğlu, H.T.; Koç, İ.; Vural, E.; Karakaya, J.; Şener, E.C.; Sanaç, A.Ş. Ocular Causes of Abnormal Head Position: Strabismus Clinic Data. Turk. J. Ophthalmol. 2017, 47, 211–215. [Google Scholar] [CrossRef]
- Nucci, P.; Curiel, B. Abnormal Head Posture Due to Ocular Problems—A Review. Curr. Pediatr. Rev. 2009, 5, 105–111. [Google Scholar] [CrossRef]
- Rubin, S.E.; Wagner, R.S. Ocular Torticollis. Surv. Ophthalmol. 1986, 30, 366–376. [Google Scholar] [CrossRef]
- Stevens, P.; Downey, C.; Boyd, V.; Cole, P.; Stal, S.; Edmond, J.; Hollier, L. Deformational Plagiocephaly Associated with Ocular Torticollis: A Clinical Study and Literature Review. J. Craniofac. Surg. 2007, 18, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.R.P.; O’Flynn, E.; Clarke, N.M.P.; Morris, R.J. Torticollis Secondary to Ocular Pathology. J. Bone Jt. Surg. Br. 1996, 78, 620–624. [Google Scholar] [CrossRef]
- Hofsli, M.; Vinding, T.; Sandfeld, L.; Buch Hesgaard, H. Ocular Torticollis Is a Diagnostic and Surgical Challenge. Ugeskr. Laeger 2013, 181, 23. [Google Scholar]
- Tay, T.; Martin, F.; Rowe, N.; Johnson, K.; Poole, M.; Tan, K.; Kennedy, I.; Gianoutsos, M. Prevalence and Causes of Visual Impairment in Craniosynostotic Syndromes. Clin. Exp. Ophthalmol. 2006, 34, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.H.; Nischal, K.K.; Dean, F.; Hayward, R.D.; Walker, J. Visual Outcomes and Amblyogenic Risk Factors in Craniosynostotic Syndromes: A Review of 141 Cases. Br. J. Ophthalmol. 2003, 87, 999–1003. [Google Scholar] [CrossRef]
- Nischal, K.K. Ocular Aspects of Craniofacial Disorders. Am. Orthopt. J. 2002, 52, 58–68. [Google Scholar] [CrossRef]
- Rostamzad, P.; Arslan, Z.F.; Mathijssen, I.M.J.; Koudstaal, M.J.; Pleumeekers, M.M.; Versnel, S.L.; Loudon, S.E. Prevalence of Ocular Anomalies in Craniosynostosis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1060. [Google Scholar] [CrossRef]
- MacIntosh, C.; Wall, S.; Leach, C. Strabismus in Unicoronal Synostosis: Ipsilateral or Contralateral? J. Craniofac. Surg. 2007, 18, 465–469. [Google Scholar] [CrossRef]
- Ntoula, E.; Nowinski, D.; Holmstrom, G.; Larsson, E. Ophthalmological Findings in Children with Non-Syndromic Craniosynostosis: Preoperatively and Postoperatively up to 12 Months after Surgery. BMJ Open Ophthalmol. 2021, 6, e000677. [Google Scholar] [CrossRef]
- Tan, K.P.; Sargent, M.A.; Poskitt, K.J.; Lyons, C.J. Ocular Overelevation in Adduction in Craniosynostosis: Is It the Result of Excyclorotation of the Extraocular Muscles? J. AAPOS 2005, 9, 550–557. [Google Scholar] [CrossRef]
- Hashemi, H.; Pakzad, R.; Heydarian, S.; Yekta, A.; Aghamirsalim, M.; Shokrollahzadeh, F.; Khoshhal, F.; Pakbin, M.; Ramin, S.; Khabazkhoob, M. Global and Regional Prevalence of Strabismus: A Comprehensive Systematic Review and Meta-Analysis. Strabismus 2019, 27, 54–65. [Google Scholar] [CrossRef] [PubMed]
- Gusek-Schneider, G.C.; Kästle, N.; Reil, F.; Schürhoff, S.; Engelhorn, T. Isolated Unilateral Strabismus Sursoadductorius (Congenital Trochlear Palsy) with and without Hypotrophia of the Superior Oblique Muscle-Orthoptic Differences in Adulthood. Klin. Monbl. Augenheilkd. 2018, 235, 1122–1128. [Google Scholar] [CrossRef] [PubMed]
- Voith-Sturm, V.; Rezar-Dreindl, S.; Neumayer, T.; Schmidt-Erfurth, U.; Stifter, E. Pre- and Postsurgical Measurements in Patients with Strabismus Sursoadductorius a Retrospective Study. Eur. J. Ophthalmol. 2023, 33, 1604–1610. [Google Scholar] [CrossRef] [PubMed]
- Touzé, R.; Bremond-Gignac, D.; Robert, M.P. Ophthalmological Management in Craniosynostosis. Neurochirurgie 2019, 65, 310–317. [Google Scholar] [CrossRef]
- Gosain, A.K.; Steele, M.A.; McCarthy, J.G.; Thorne, C.H. A Prospective Study of the Relationship between Strabismus and Head Posture in Patients with Frontal Plagiocephaly. Plast. Reconstr. Surg. 1996, 97, 881–891. [Google Scholar] [CrossRef]
- Robb, R.M.; Boger, W.P. Vertical Strabismus Associated with Plagiocephaly. J. Pediatr. Ophthalmol. Strabismus 1983, 20, 58–62. [Google Scholar] [CrossRef]
- Simonsz, H.J.; Kolling, G.H.; Unnebrink, K. Final Report of the Early vs. Late Infantile Strabismus Surgery Study (ELISSS), a Controlled, Prospective, Multicenter Study. Strabismus 2005, 13, 169–199. [Google Scholar] [CrossRef]
- Kim, H.-Y. Statistical Notes for Clinical Researchers: Chi-Squared Test and Fisher’s Exact Test. Restor. Dent. Endod. 2017, 42, 152–155. [Google Scholar] [CrossRef]
- Mitchell, P.B. Ocular Torticollis. Trans. Am. Ophthalmol. Soc. 1999, 97, 697. [Google Scholar]
- Dikici, K.; Kizilkaya, M. Ocular Casuses of Abnormal Head Posture. Cerrahpaşa Med. J. 2002, 33, 42–46. [Google Scholar]
- Kushner, B.J. Ocular Causes of Abnormal Head Postures. Ophthalmology 1979, 86, 2115–2125. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.R.; Khorrami-Nejad, M.; Kangari, H.; Akbarzadeh Baghban, A.A.; Ranjbar Pazouki, M.R. Ocular Abnormal Head Posture: A Literature Review. J. Curr. Ophthalmol. 2021, 33, 379. [Google Scholar] [CrossRef] [PubMed]
- Erkan Turan, K.; Taylan Sekeroglu, H.; Koc, I.; Kilic, M.; Sanac, A.S. The Frequency and Causes of Abnormal Head Position Based on an Ophthalmology Clinic’s Findings: Is It Overlooked? Eur. J. Ophthalmol. 2016, 27, 491–494. [Google Scholar] [CrossRef] [PubMed]
- Denis, D.; Genitori, L.; Bolufer, A.; Lena, G.; Saracco, J.B.; Choux, M. Refractive Error and Ocular Motility in Plagiocephaly. Child’s Nerv. Syst. 1994, 10, 210–216. [Google Scholar] [CrossRef]
- Bagolini, B.; Campos, E.C.; Chiesi, C. Plagiocephaly Causing Superior Oblique Deficiency and Ocular Torticollis. A New Clinical Entity. Arch. Ophthalmol. 1982, 100, 1093–1096. [Google Scholar] [CrossRef]
- Beckett, J.S.; Persing, J.A.; Steinbacher, D.M. Bilateral Orbital Dysmorphology in Unicoronal Synostosis. Plast. Reconstr. Surg. 2013, 131, 125–130. [Google Scholar] [CrossRef]
- Touzé, R.; Heuzé, Y.; Robert, M.P.; Brémond-Gignac, D.; Roux, C.J.; James, S.; Paternoster, G.; Arnaud, E.; Khonsari, R.H. Extraocular Muscle Positions in Anterior Plagiocephaly: V-Pattern Strabismus Explained Using Geometric Mophometrics. Br. J. Ophthalmol. 2020, 104, 1156–1160. [Google Scholar] [CrossRef]
- Morax, S. Oculo-Motor Disorders in Craniofacial Malformations. J. Maxillofac. Surg. 1984, 12, 1–10. [Google Scholar] [CrossRef]
- Deng, H.; Irsch, K.; Gutmark, R.; Phamonvaechavan, P.; Foo, F.Y.; Anwar, D.S.; Guyton, D.L. Fusion Can Mask the Relationships between Fundus Torsion, Oblique Muscle Overaction/Underaction, and A- and V-Pattern Strabismus. J. AAPOS 2013, 17, 177–183. [Google Scholar] [CrossRef]
- Yoon, J.A.; Choi, H.; Shin, Y.B.; Jeon, H. Development of a Questionnaire to Identify Ocular Torticollis. Eur. J. Pediatr. 2020, 180, 561–567. [Google Scholar] [CrossRef]
- Tumturk, A.; Kaya Ozcora, G.; Kacar Bayram, A.; Kabaklioglu, M.; Doganay, S.; Canpolat, M.; Gumus, H.; Kumandas, S.; Unal, E.; Kurtsoy, A.; et al. Torticollis in Children: An Alert Symptom Not to Be Turned Away. Child’s Nerv. Syst. 2015, 31, 1461–1470. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | Total (n = 146) | Torticollis (n = 57) | No Torticollis (n = 89) | p-Value |
|---|---|---|---|---|
| Sex (n, %) | 0.853 | |||
| Female | 96 (65.8) | 38 (66.7) | 58 (65.2) | |
| Male | 50 (44.2) | 19 (33.3) | 31 (34.8) | |
| Synostotic coronal suture (n, %) | 0.428 | |||
| Right | 85 (58.2) | 31 (54.4) | 54 (60.7) | |
| Left | 58 (39.7) | 25 (43.9) | 33 (37.1) | |
| Unknown | 3 (2.1) | 1 (1.8) | 2 (2.2) | |
| Age at initial visit (y, mean (SD)) | 2.72 (SD 3.6) | 2.3 (SD 2.5) | 3.0 (SD 4.1) | 0.256 [95% CI −0.51; 1.91] |
| Craniofacial surgery (n, %) | 0.201 | |||
| Fronto-orbital advancement rim | 135 (92.5) | 52 (91.3) | 83 (93.3) | |
| Reconstruction of one orbit | 5 (3.7) | 2 (3.8) | 3 (3.6) | |
| Reconstruction of both orbits | 127 (94.1) | 49 (94.2) | 78 (93.9) | |
| Unknown | 3 (2.3) | 1 (1.9) | 2 (2.5) | |
| Strip craniotomy | 1 (0.7) | 0 | 1 (1.1) | |
| No surgery | 5 (3.4) | 4 (7) | 1 (1.1) | |
| Unknown | 5 (3.4) | 1 (1.7) | 4 (4.5) | |
| Mean age at surgery (m, mean (SD)) | 11.58 (SD 7.3) | 10.49 (SD 3.0) | 12.26 (SD 8.8) | 0.087 [95% CI −0.78; 4.32] |
| Diagnosis of Torticollis | n = 57 [n, %] |
|---|---|
| Incomitant strabismus | 47 (88.7) |
| Pseudo-superior oblique palsy | 34 (59.6) |
| Pseudo-inferior oblique palsy | 7 (12.3) |
| Infantile esotropia and pseudo-superior oblique palsy | 3 (5.3) |
| Fourth nerve palsy | 1 (1.8) |
| Intermittent exotropia and pseudo-inferior oblique palsy | 1 (1.8) |
| Infantile exotropia and pseudo-superior oblique palsy | 1 (1.8) |
| Concomitant strabismus | 6 (10.5) |
| Accommodative esotropia | 3 (5.3) |
| Intermittent exotropia | 2 (3.5) |
| Micro esotropia | 1 (1.8) |
| Other | 1 (1.7) |
| Congenital nystagmus | 1 (1.8) |
| Non-ocular | 3 (5.3) |
| Type Torticollis | n = 57 [n, %] |
|---|---|
| Face turn | 16 (28.1) |
| Right Left | 4 (7.1%) 12 (21.4%) |
| Head tilt | 27 (47.4) |
| Right Left | 16 (28.6%) 11 (19.6%) |
| Combination | 13 (22.8) |
| Turn, chin, tilt Turn, chin Chin, tilt Tilt, turn | 4 (7.1%) 3 (5.4%) 2 (3.6%) 4 (7.1%) |
| Unspecified | 1 (1.7) |
| Ophthalmic Features | Total [n, %] | Ocular Torticollis [n, %] | No (Ocular) Torticollis [n, %] |
|---|---|---|---|
| Binocular single vision | n = 62 | n = 19 | n = 43 |
| Good Moderate Poor Not present | 29 (46.8) 10 (16.1) 11 (17.7) 12 (19.4) | 3 (15.8) 3 (15.8) 8 (42.1) 5 (26.3) | 26 (60.5) 7 (16.3) 3 (7) 7 (16.3) |
| Strabismus | n = 145 | n = 53 | n = 92 |
| Esotropia Exotropia ET + vertical XT + vertical Vertical alone Not present | 11 (7.6) 8 (5.5) 19 (13.1) 14 (9.7) 17 (11.7) 76 (53.8) | 4 (7.5) 2 (3.8) 10 (18.9) 11 (20.8) 13 (24.5) 13 (24.5) | 7 (7.6) 6 (6.5) 9 (9.8) 3 (3.3) 4 (4.3) 63 (68.5) |
| Ocular motility | n = 143 | n = 53 | n = 90 |
| Elevation in adduction RE Elevation in adduction LE Elevation in adduction RLE Depression in adduction RE Depression in adduction LE Depression in adduction RLE Not present | 26 (18.2) 20 (14) 23 (16.1) 6 (4.2) 5 (3.5) 2 (1.4) 61 (42.7) | 15 (28.3) 12 (22.6) 14 (26.4) 5 (9.4) 2 (3.8) 2 (3.8) 3 (5.7) | 11 (12.2) 8 (8.9) 9 (10) 1 (11.1) 3 (3.3) 0 58 (64.4) |
| Alphabetical pattern | n = 143 | n = 53 | n = 90 |
| V-pattern A-pattern Not present | 46 (32.2) 12 (8.4) 85 (59.4) | 29 (54.7) 7 (13.2) 17 (32.1) | 17 (18.9) 5 (5.6) 67 (75.6) |
| Cyclotorsion | n = 53 | n = 30 | n = 23 |
| Excyclotorsion Incyclotorsion Not present | 33 (62.3) 4 (7.5) 16 (30.2) | 22 (73.3)1 (3.3) 7 (23.3) | 11 (47.8) 3 (13) 9 (39.1) |
| Refractive error * | n = 125 | n = 45 | n = 80 |
| Hypermetropia High hypermetropia Myopia Astigmatism Anisometropia | 112 (89.6) 6 (4.8) 2 (1.6) 55 (44) 33 (22.6) | 41 (89.1) 2 (4.4) 1 (2.2) 20 (43.5) 12 (26.7) | 71 (89.9) 4 (5) 1 (1.3) 35 (44.3) 21 (26.3) |
| Amblyopia | n = 146 | n = 54 | n = 92 |
| Present Absent | 64 (43.8) 82 (56.2) | 33 (61.1) 21 (38.9) | 31 (33.7) 61 (66.3) |
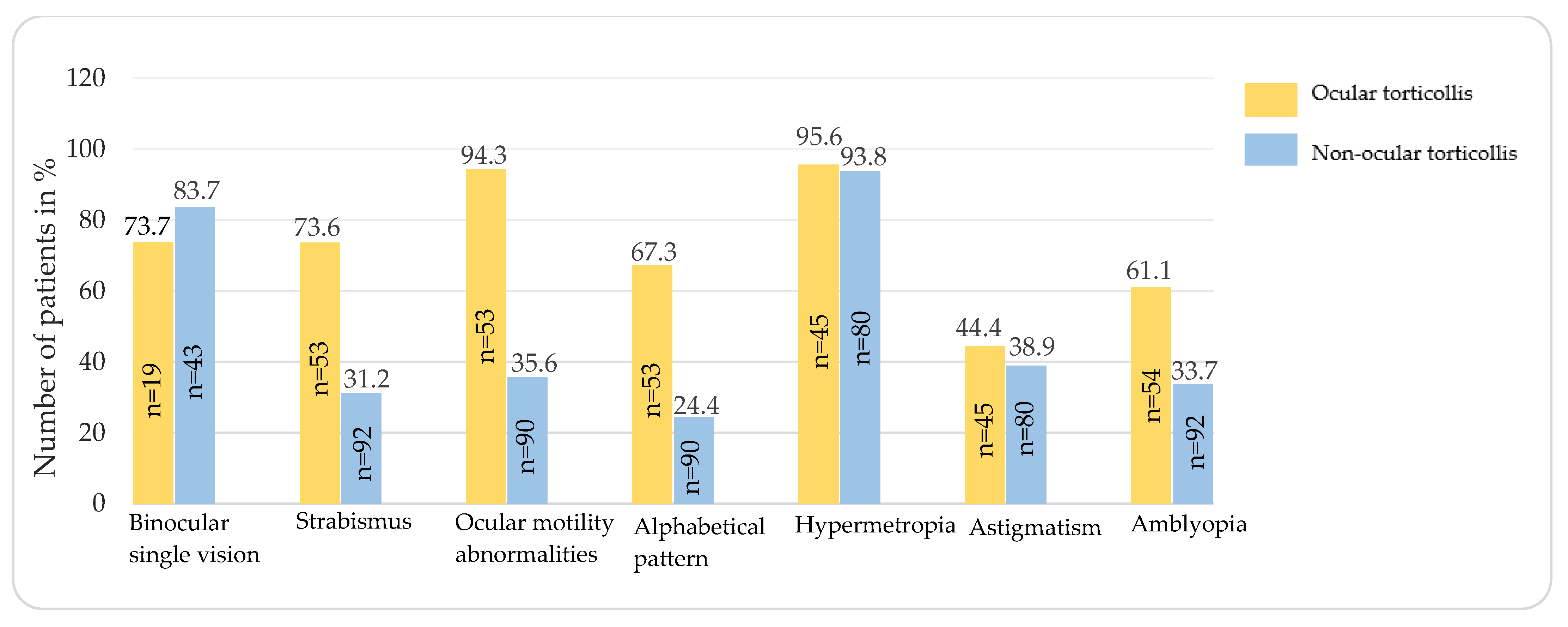
| Ophthalmic Features | Ocular Torticollis [n, %] | No (Ocular) Torticollis [n, %] | p-Value | Cramers’ V |
|---|---|---|---|---|
| Binocular single vision | n = 19 | n = 43 | ||
| Present Absent | 14 (73.7) 5 (26.3) | 36 (83.7) 7 (16.3) | 0.277 | 0.117 |
| Strabismus | n = 53 | n = 92 | ||
| Present Absent | 39 (73.6) 14 (26.4) | 29 (31.2) 63 (68.8) | <0.001 | 0.406 |
| Ocular motility abnormalities | n = 53 | n = 90 | ||
| Present Absent | 50 (94.3) 3 (5.7) | 32 (35.6) 58 (64.4) | <0.001 | 0.574 |
| Alphabetical pattern | n = 53 | n = 90 | ||
| Present Absent | 36 (67.3) 17 (32.7) | 22 (24.4) 68 (75.6) | <0.001 | 0.428 |
| Refractive error * | n = 45 | n = 80 | ||
| Hypermetropia Myopia Astigmatism Anisometropia | 43 (95.6) 1 (2.2) 20 (44.4) 12 (26.7) | 75 (93.8) 1 (1.2) 35 (38.9) 21 (26.2) | 1.0 1.0 1.0 1.0 | - - - - |
| Amblyopia | n = 54 | n = 92 | ||
| Present Absent | 33 (61.1) 21 (38.9) | 31 (33.7) 61 (66.3) | 0.002 | 0.267 |
| Presence of Strabismus [p-Value, Cramers’ V] | Ocular Motility Abnormalities [p-Value, Cramers’ V] | Alphabetical Patterns [p-Value, Cramers’ V] | |
|---|---|---|---|
| Presence of strabismus | - | <0.01 0.483 | <0.01 0.416 |
| Ocular motility abnormalities | <0.01 0.483 | - | <0.01 0.626 |
| Alphabetical patterns | <0.01 0.416 | <0.01 0.626 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tan, E.T.C.; Rostamzad, P.; Esser, Y.S.; Pleumeekers, M.M.; Loudon, S.E. Torticollis in Non-Syndromic Unicoronal Craniosynostosis Is Predominantly Ocular Related. J. Clin. Med. 2023, 12, 6059. https://doi.org/10.3390/jcm12186059
Tan ETC, Rostamzad P, Esser YS, Pleumeekers MM, Loudon SE. Torticollis in Non-Syndromic Unicoronal Craniosynostosis Is Predominantly Ocular Related. Journal of Clinical Medicine. 2023; 12(18):6059. https://doi.org/10.3390/jcm12186059
Chicago/Turabian StyleTan, Emily T. C., Parinaz Rostamzad, Yasmin S. Esser, Mieke M. Pleumeekers, and Sjoukje E. Loudon. 2023. "Torticollis in Non-Syndromic Unicoronal Craniosynostosis Is Predominantly Ocular Related" Journal of Clinical Medicine 12, no. 18: 6059. https://doi.org/10.3390/jcm12186059





