Blend Sign and Haemorrhage Location and Volume Predict Late Recurrence and Mortality in Intracerebral Haemorrhage Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Protocol Approvals and Data Availability
2.3. Longitudinal Data
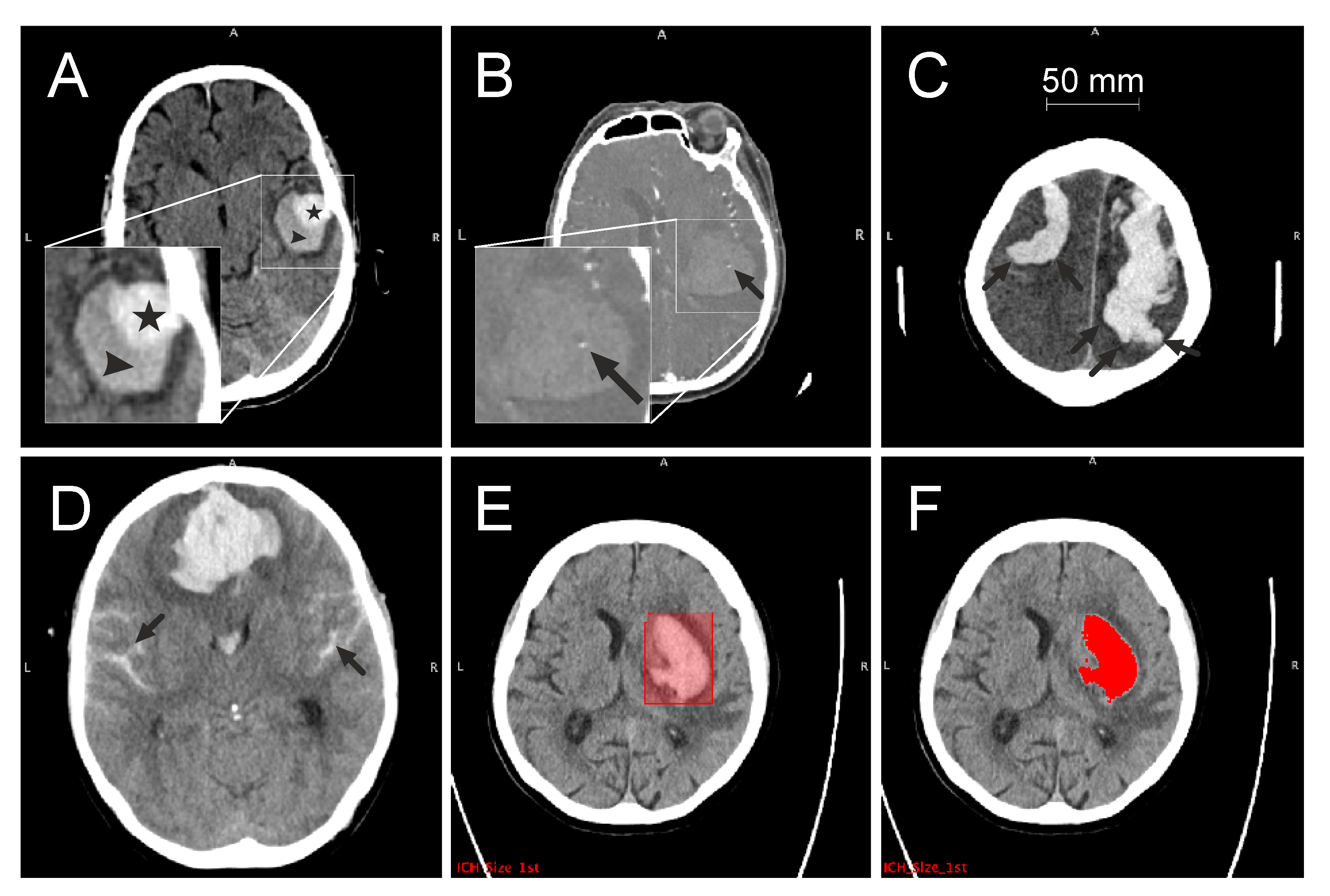
2.4. CT Acquisition and Analysis
2.5. Statistical Analysis
3. Results
3.1. Baseline Data
3.1.1. Comparison of Demographics and CT Markers
3.1.2. CT Sign Carriers
3.2. Longitudinal Data
3.2.1. ICH Volume Expansion
3.2.2. ICH Recurrence
3.2.3. Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qureshi, A.I.; Mendelow, A.D.; Hanley, D.F. Intracerebral haemorrhage. Lancet 2009, 373, 1632–1644. [Google Scholar] [CrossRef] [PubMed]
- Ironside, N.; Chen, C.-J.; Dreyer, V.; Christophe, B.; Buell, T.J.; Connolly, E.S. Location-specific differences in hematoma volume predict outcomes in patients with spontaneous intracerebral hemorrhage. Int. J. Stroke 2020, 15, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Poon, M.T.; Fonville, A.F.; Al Shahi, S.R. Long-term prognosis after intracerebral haemorrhage: Systematic review and meta-analysis. J. Neurol. Neurosurg. Psychiatry 2014, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Zhang, G.; Huang, Y.-J.; Dong, M.-X.; Lv, F.-J.; Wei, X.; Chen, J.-J.; Zhang, L.-J.; Qin, X.-Y.; Xie, P. Blend Sign on Computed Tomography: Novel and Reliable Predictor for Early Hematoma Growth in Patients with Intracerebral Hemorrhage. Stroke 2015, 46, 2119–2123. [Google Scholar] [CrossRef]
- Morotti, A.; Arba, F.; Boulouis, G.; Charidimou, A. Noncontrast CT markers of intracerebral hemorrhage expansion and poor outcome: A meta-analysis. Neurology 2020, 95, 632–643. [Google Scholar] [CrossRef]
- Morotti, A.; Boulouis, G.; Charidimou, A.; Schwab, K.; Kourkoulis, C.; Anderson, C.D.; Gurol, M.E.; Viswanathan, A.; Romero, J.M.; Greenberg, S.M.; et al. Integration of Computed Tomographic Angiography Spot Sign and Noncontrast Computed Tomographic Hypodensities to Predict Hematoma Expansion. Stroke 2018, 49, 2067–2073. [Google Scholar] [CrossRef]
- Rodrigues, M.A.; Samarasekera, N.; Lerpiniere, C.; Humphreys, C.; McCarron, M.O.; White, P.M.; Nicoll, J.A.R.; Sudlow, C.L.M.; Cordonnier, C.; Wardlaw, J.M.; et al. The Edinburgh CT and genetic diagnostic criteria for lobar intracerebral haemorrhage associated with cerebral amyloid angiopathy: Model development and diagnostic test accuracy study. Lancet Neurol. 2018, 17, 232–240. [Google Scholar] [CrossRef]
- Li, J.; Liao, X.; Yu, Z.; Li, H.; Zheng, J. Predictive Ability of Ultraearly Hematoma Growth and Spot Sign for Redefined Hematoma Expansion in Patients with Spontaneous Intracerebral Hemorrhage. J. Stroke Cerebrovasc. Dis. 2021, 30, 105950. [Google Scholar] [CrossRef]
- Morotti, A.; Boulouis, G.; Charidimou, A.; Poli, L.; Costa, P.; de Giuli, V.; Leuci, E.; Mazzacane, F.; Busto, G.; Arba, F.; et al. Imaging markers of intracerebral hemorrhage expansion in patients with unclear symptom onset. Int. J. Stroke 2022, 17, 1013–1020. [Google Scholar] [CrossRef]
- Lei, K.; Wei, S.; Liu, X.; Yuan, X.; Pei, L.; Xu, Y.; Song, B.; Sun, S. Combination of Ultraearly Hematoma Growth and Hypodensities for Outcome Prediction after Intracerebral Hemorrhage. World Neurosurg. 2020, 135, e610–e615. [Google Scholar] [CrossRef]
- Roh, D.; Boehme, A.; Young, C.; Roth, W.; Gutierrez, J.; Flaherty, M.; Rosand, J.; Testai, F.; Woo, D.; Elkind, M.S.V. Hematoma expansion is more frequent in deep than lobar intracerebral hemorrhage. Neurology 2020, 95, e3386–e3393. [Google Scholar] [CrossRef] [PubMed]
- Charidimou, A.; Schmitt, A.; Wilson, D.; Yakushiji, Y.; Gregoire, S.M.; Fox, Z.; Jäger, H.R.; Werring, D.J. The Cerebral Haemorrhage Anatomical RaTing inStrument (CHARTS): Development and assessment of reliability. J. Neurol. Sci. 2017, 372, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Specogna, A.V.; Turin, T.C.; Patten, S.B.; Hill, M.D. Hospital treatment costs and length of stay associated with hypertension and multimorbidity after hemorrhagic stroke. BMC Neurol. 2017, 17, 158. [Google Scholar] [CrossRef]
- Boulouis, G.; Morotti, A.; Brouwers, H.B.; Charidimou, A.; Jessel, M.J.; Auriel, E.; Pontes-Neto, O.; Ayres, A.; Vashkevich, A.; Schwab, K.M.; et al. Association Between Hypodensities Detected by Computed Tomography and Hematoma Expansion in Patients with Intracerebral Hemorrhage. JAMA Neurol. 2016, 73, 961–968. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Feinstein, A.R.; Holford, T.R. Importance of events per independent variable in proportional hazards regression analysis. II. Accuracy and precision of regression estimates. J. Clin. Epidemiol. 1995, 48, 1503–1510. [Google Scholar] [CrossRef] [PubMed]
- Sporns, P.B.; Schwake, M.; Kemmling, A.; Minnerup, J.; Schwindt, W.; Niederstadt, T.; Schmidt, R.; Hanning, U. Comparison of Spot Sign, Blend Sign and Black Hole Sign for Outcome Prediction in Patients with Intracerebral Hemorrhage. J. Stroke 2017, 19, 333–339. [Google Scholar] [CrossRef]
- van Etten, E.S.; Kaushik, K.; van Zwet, E.W.; Voigt, S.; van Walderveen, M.A.A.; van Buchem, M.A.; Terwindt, G.M.; Wermer, M.J.H. Sensitivity of the Edinburgh Criteria for Lobar Intracerebral Hemorrhage in Hereditary Cerebral Amyloid Angiopathy. Stroke 2020, 51, 3608–3612. [Google Scholar] [CrossRef]
- Morotti, A.; Brouwers, H.B.; Romero, J.M.; Jessel, M.J.; Vashkevich, A.; Schwab, K.; Afzal, M.R.; Cassarly, C.; Greenberg, S.M.; Martin, R.H.; et al. Intensive Blood Pressure Reduction and Spot Sign in Intracerebral Hemorrhage: A Secondary Analysis of a Randomized Clinical Trial. JAMA Neurol. 2017, 74, 950–960. [Google Scholar] [CrossRef]
- New, P.F.; Aronow, S. Attenuation measurements of whole blood and blood fractions in computed tomography. Radiology 1976, 121, 635–640. [Google Scholar] [CrossRef]
- Wada, R.; Aviv, R.I.; Fox, A.J.; Sahlas, D.J.; Gladstone, D.J.; Tomlinson, G.; Symons, S.P. CT angiography “spot sign” predicts hematoma expansion in acute intracerebral hemorrhage. Stroke 2007, 38, 1257–1262. [Google Scholar] [CrossRef]
- Morotti, A.; Li, Q.; Mazzoleni, V.; Nawabi, J.; Schlunk, F.; Mazzacane, F.; Busto, G.; Scola, E.; Brancaleoni, L.; Giacomozzi, S.; et al. Non-contrast CT markers of intracerebral hemorrhage expansion: The influence of onset-to-CT time. Int. J. Stroke 2023, 18, 704–711. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Shen, Z.; Wang, L.; Sun, S.; Luo, J.; Mao, Y. Post-operative re-bleeding in patients with hypertensive ICH is closely associated with the CT blend sign. BMC Neurol. 2017, 17, 131. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, H.B.; Biffi, A.; McNamara, K.A.; Ayres, A.M.; Valant, V.; Schwab, K.; Romero, J.M.; Viswanathan, A.; Greenberg, S.M.; Rosand, J.; et al. Apolipoprotein E genotype is associated with CT angiography spot sign in lobar intracerebral hemorrhage. Stroke 2012, 43, 2120–2125. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Cheng, Y.; Song, Q.; Yuan, R.; Zhang, S.; Hao, Z.; Liu, M. Total Burden of Cerebral Small Vessel Disease in Recurrent ICH versus First-ever ICH. Aging Dis. 2019, 10, 570–577. [Google Scholar] [CrossRef]
- Samarasekera, N.; Rodrigues, M.A.; Toh, P.S.; Al-Shahi, S. Imaging features of intracerebral hemorrhage with cerebral amyloid angiopathy: Systematic review and meta-analysis. PLoS ONE 2017, 12, e0180923. [Google Scholar] [CrossRef]
- Seiffge, D.J.; Wilson, D.; Ambler, G.; Banerjee, G.; Hostettler, I.C.; Houlden, H.; Shakeshaft, C.; Cohen, H.; Yousry, T.A.; Al-Shahi Salman, R.; et al. Small vessel disease burden and intracerebral haemorrhage in patients taking oral anticoagulants. J. Neurol. Neurosurg. Psychiatry 2021, 92, 805–814. [Google Scholar] [CrossRef]

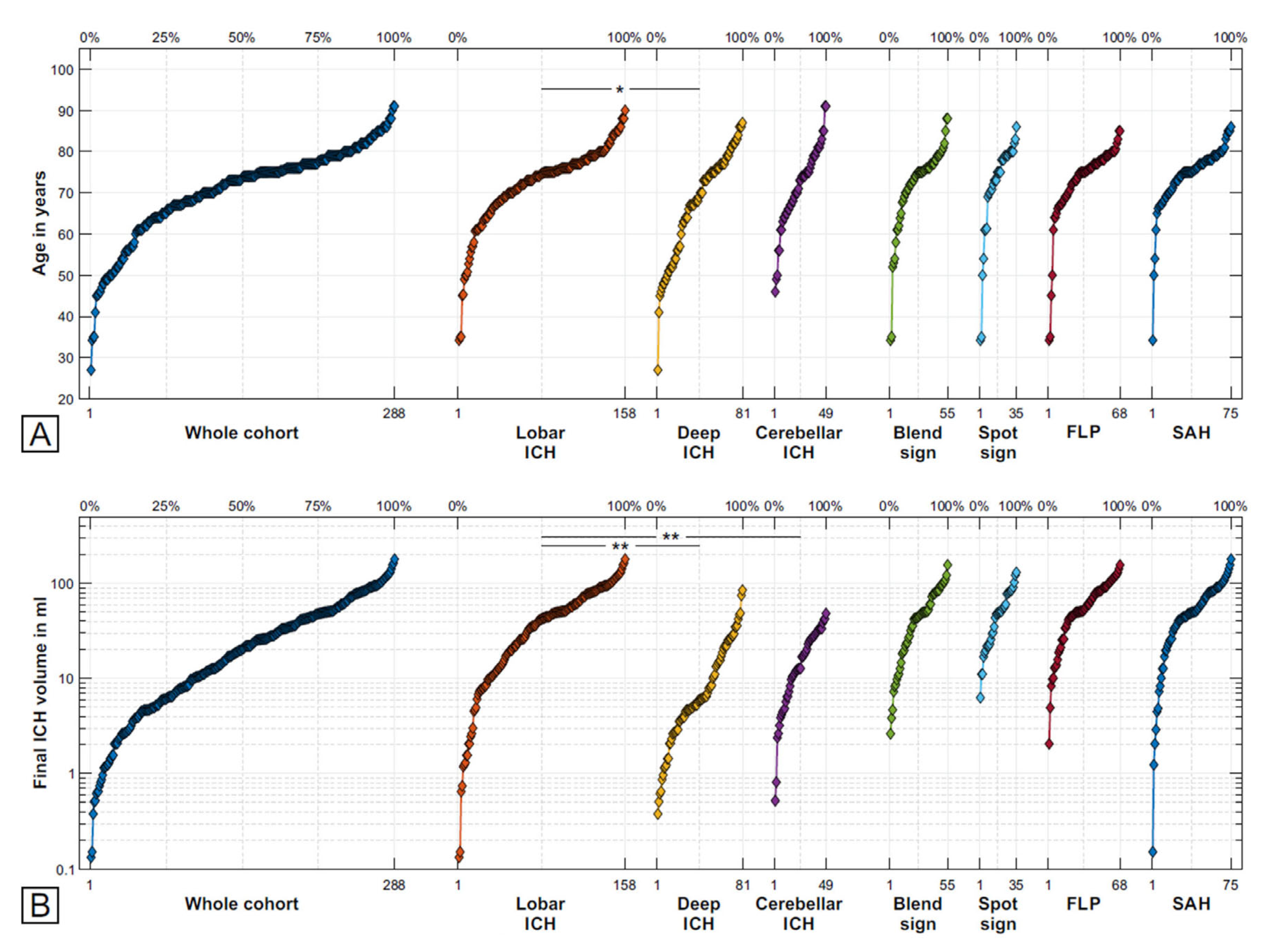

| Variable | Total (n = 288) | Lobar (n = 158) | Deep (n = 81) | Cerebellar (n = 49) | Group Univariate Analysis | Group Multivariate Analysis | Lobar vs. Deep | Lobar vs. Cerebellar | Deep vs. Cerebellar |
|---|---|---|---|---|---|---|---|---|---|
| Age (years) | 70.6 (11.0) | 71.9 (10.0) | 67.4 (12.8) | 71.5 (10.0) | p = 0.009 | p = 0.003 B(1) = −4.5 (−7.4; −1.5) | p = 0.781 B(1) = −0.5 (−3.7; 2.8) | p = 0.062 B(1) = 4.0 (−0.2; 8.2) | |
| Male sex n (%) | 150 (52) | 77 (49) | 49 (62) | 24 (49) | p = 0.100 | p = 0.038 OR = 1.8 (1.0; 3.1) | p = 0.853 OR = 1.1 (0.6; 2.0) | p = 0.156 OR = 0.6 (0.3; 1.2) | |
| VRFS | 0.49 (0.27) | 0.45 (0.30) | 0.56 (0.20) | 0.55 (0.23) | p = 0.012 | p = 0.004 B(1) = 0.1 (0.0; 0.2) | p = 0.250 B(1) = 0.1 (−0.1; 0.3) | p = 0.904 B(1) = 0.0 (−0.1; 0.1) | |
| Antiplatelet therapy | 81 (36) | 60 (45) | 16 (21) | 5 (42) | p < 0.001 | p < 0.001 OR = 0.3 (0.2–0.6) | p = 0.801 OR = 0.9 (0.3–2.8) | p = 0.117 OR = 2.8 (0.8–9.9) | |
| Anticoagulation therapy | 93 (42) | 76 (58) | 14 (18) | 3 (25) | p < 0.001 | p < 0.001 OR = 0.2 (0.1–0.3) | p = 0.042 OR = 0.2 (0.1–0.9) | p = 0.563 OR = 1.5 (0.4–6.4) | |
| Blend sign (final) n (%) | 55 (19) | 48 (30) | 6 (7) | 1 (2) | p < 0.001 | p < 0.001 | p < 0.001 OR = 0.2 (0.1–0.5) | p = 0.003 OR = 0.0 (0.0–0.4) | p = 0.220 OR = 0.3 (0.0–2.2) |
| CTA spot sign (final) n (%) | 35 (14) | 25 (19) | 7 (9) | 3 (7) | p = 0.053 | p = 0.088 | p = 0.066 OR = 0.4 (0.2–1.1) | p = 0.090 OR = 0.3 (0.1–1.2) | p = 0.730 OR = 0.8 (0.2–3.2) |
| FLP (final) n (%) | 68 (24) | 65 (41) | 3 (4) | 0 (0) | p < 0.001 | p < 0.001 | p < 0.001 OR = 0.1 (0.0–0.2) | ||
| SAH (final) n (%) | 75 (26) | 62 (39) | 4 (5) | 9 (18) | p < 0.001 | p < 0.001 | p < 0.001 OR = 0.1 (0.0–0.2) | p = 0.009 OR = 0.3 (0.2–0.8) | p = 0.020 OR = 4.3 (1.3–14.9) |
| Initial baseline ICH volume (mL) | 28.7 (0.1; 180.8) | 41.8 (0.1; 180.8) | 9.2 (0.2; 85) | 16.7 (0.5; 48.4) | p < 0.001 | p < 0.001 | p < 0.001 B(1) = −32.6 (−40.7; −24,6) | p < 0.001 B(1) = −25.0 (−35.2; −14.8) | p = 0.001 B(1) = 7.6 (3.2; 12.0) |
| Final baseline ICH volume (mL) | 32.5 (0.1; 180.8) | 47.1 (0.1; 180.8) | 12.7 (0.4; 85.2) | 17.7 (0.5; 48.4) | p < 0.001 | p < 0.001 | p < 0.001 B(1) = −34.4 (−43.2; 25.7) | p < 0.001 B(1) = −29.4 (−40.4; −18.4) | p = 0.060 B(1) = 5.0 (−0.2; −10.2) |
| ICH volume expansionn (%) | 68 (24) | 40 (25) | 23 (28) | 5 (10) | p = 0.029 | p = 0.464 | p = 0.609 OR = 1.2 (0.6–2.1) | p = 0.031 OR = 0.3 (0.1–0.9) | p = 0.019 OR = 0.3 (0.1–0.8) |
| ICH recurrence n (%) | 54 (22) | 42 (28) | 5 (7) | 7 (33) | p < 0.001 | p = 0.004 | p = 0.001 OR = 0.2 (0.1–0.5) | p = 0.588 OR = 1.3 (0.5–3.5) | p = 0.004 OR = 6.5 (1.8–23.5) |
| Mortality n (%) | 117 (52) | 79 (56) | 29 (43) | 9 (64) | p = 0.136 | p = 0.831 | p = 0.079 OR = 0.6 (0.3–1.1) | p = 0.535 OR = 1.4 (0.5–4.5) | p = 0.147 OR = 2.4 (0.7–8.0) |
| Univariate Analysis | Multivariate Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| Covariate | e/n | HR [exp(bi)] | 95% CI | p-Value | e/n | HR [exp(bi)] | 95% CI | p-Value |
| (A) ICH Expansion | ||||||||
| Age (a) | 60/206 | 1.020 | (0.996–1.045) | 0.096 | 62/206 | 1.017 | (0.992–1.042) | 0.191 |
| Male sex | 60/206 | 1.142 | (0.689–1.891) | 0.607 | 62/206 | 1.113 | (0.662–1.871) | 0.686 |
| VRFS | 53/169 | 1.053 | (0.380–2.920) | 0.920 | ||||
| Antiplatelet | 50/161 | 1.121 | (0.636–1.978) | 0.693 | ||||
| Anticoagulation | 50/161 | 1.276 | (0.733–2.221) | 0.389 | ||||
| Deep ICH | 60/206 | 0.880 | (0.523–1.481) | 0.631 | ||||
| Cerebellar ICH | 60/206 | 0.442 | (0.177–1.103) | 0.080 | 62/206 | 0.531 | (0.210–1.344) | 0.182 |
| Blend sign | 60/206 | 2.641 | (1.475–4.729) | 0.001 | 62/206 | 2.285 | (1.199–4.354) | 0.012 |
| CTA spot sign | 19/57 | 2.397 | (0.971–5.920) | 0.058 | ||||
| FLP | 60/206 | 1.597 | (0.850–2.999) | 0.146 | ||||
| SAH | 60/206 | 1.396 | (0.780–2.496) | 0.261 | 62/206 | 1.234 | (0.662–2.300) | 0.509 |
| ICH volume | 60/206 | 1.147 | (0.754–1.745) | 0.521 | 62/206 | 0.915 | (0.586–1.428) | 0.694 |
| (B) ICH Recurrence | ||||||||
| Age (a) | 54/243 | 1.016 | (0.991–1.041) | 0.205 | ||||
| Male sex | 54/243 | 1.108 | (0.646–1.900) | 0.710 | ||||
| VRFS | 43/214 | 0.438 | (0.146–1.313) | 0.141 | 43/214 | 0.501 | (0.167–1.500) | 0.217 |
| Antiplatelet | 39/204 | 1.193 | (0.620–2.296) | 0.598 | ||||
| Anticoagulation | 39/204 | 1.801 | (0.953–3.405) | 0.070 | ||||
| Deep ICH | 54/243 | 0.221 | (0.088–0.556) | 0.001 | 43/214 | 0.191 | (0.064–0.570) | 0.003 |
| Cerebellar ICH | 54/243 | 1.887 | (0.852–4.179) | 0.118 | ||||
| Blend sign | 54/243 | 1.874 | (1.028–3.417) | 0.040 | 43/214 | 2.305 | (1.171–4.539) | 0.016 |
| CTA spot sign | 17/73 | 0.436 | (0.136–1.403) | 0.164 | ||||
| FLP | 54/243 | 1.006 | (0.530–1.912) | 0.985 | ||||
| SAH | 54/243 | 0.933 | (0.491–1.773) | 0.832 | ||||
| ICH volume | 54/243 | 1.014 | (0.664–1.548) | 0.950 | 43/214 | 0.562 | (0.340–0.929) | 0.025 |
| (C) Overall Survival | ||||||||
| Age (a) | 117/224 | 1.057 | (1.035–1.080) | <0.001 | 97/194 | 1.062 | (1.036–1.089) | <0.001 |
| Male sex | 117/224 | 0.804 | (0.559–1.157) | 0.240 | ||||
| VRFS | 104/205 | 0.710 | (0.355–1.420) | 0.333 | 97/194 | 0.565 | (0.240–1.329) | 0.191 |
| Antiplatelet | 98/197 | 2.088 | (1.404–3.106) | <0.001 | 97/194 | 2.122 | (1.358–3.314) | 0.001 |
| Anticoagulation | 98/197 | 1.018 | (0.678–1.528) | 0.930 | 97/194 | 0.916 | (0.586–1.431) | 0.698 |
| Deep ICH | 117/224 | 0.728 | (0.478–1.110) | 0.140 | 97/194 | 2.117 | (1.168–3.836) | 0.013 |
| Cerebellar ICH | 117/224 | 1.428 | (0.722–2.826) | 0.306 | 97/194 | 1.432 | (0.477–4.302) | 0.522 |
| Blend sign | 117/224 | 1.684 | (1.103–2.570) | 0.016 | 97/194 | 1.617 | (1.030–2.539) | 0.037 |
| CTA spot sign | 37/66 | 1.356 | (0.781–2.353) | 0.280 | ||||
| FLP | 117/224 | 1.580 | (1.062–2.349) | 0.024 | 97/194 | 1.351 | (0.813–2.247) | 0.246 |
| SAH | 117/224 | 1.164 | (0.778–1.743) | 0.460 | ||||
| ICH volume | 117/224 | 1.959 | (1.377–2.788) | <0.001 | 97/194 | 1.947 | (1.182–3.206) | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schreiber, F.; Kuschel, J.-N.; Klai, M.; Chahem, C.; Arndt, P.; Perosa, V.; Assmann, A.; Dörner, M.; Luchtmann, M.; Meuth, S.G.; et al. Blend Sign and Haemorrhage Location and Volume Predict Late Recurrence and Mortality in Intracerebral Haemorrhage Patients. J. Clin. Med. 2023, 12, 6131. https://doi.org/10.3390/jcm12196131
Schreiber F, Kuschel J-N, Klai M, Chahem C, Arndt P, Perosa V, Assmann A, Dörner M, Luchtmann M, Meuth SG, et al. Blend Sign and Haemorrhage Location and Volume Predict Late Recurrence and Mortality in Intracerebral Haemorrhage Patients. Journal of Clinical Medicine. 2023; 12(19):6131. https://doi.org/10.3390/jcm12196131
Chicago/Turabian StyleSchreiber, Frank, Jan-Niklas Kuschel, Marwa Klai, Christian Chahem, Philipp Arndt, Valentina Perosa, Anne Assmann, Marc Dörner, Michael Luchtmann, Sven Günther Meuth, and et al. 2023. "Blend Sign and Haemorrhage Location and Volume Predict Late Recurrence and Mortality in Intracerebral Haemorrhage Patients" Journal of Clinical Medicine 12, no. 19: 6131. https://doi.org/10.3390/jcm12196131





