Do Concurrent Multiple Infections with High-Risk HPVs Carry a More Malignant Potential than a Single Infection in the Uterine Cervix?
Abstract
:1. Introduction
2. Materials and Methods
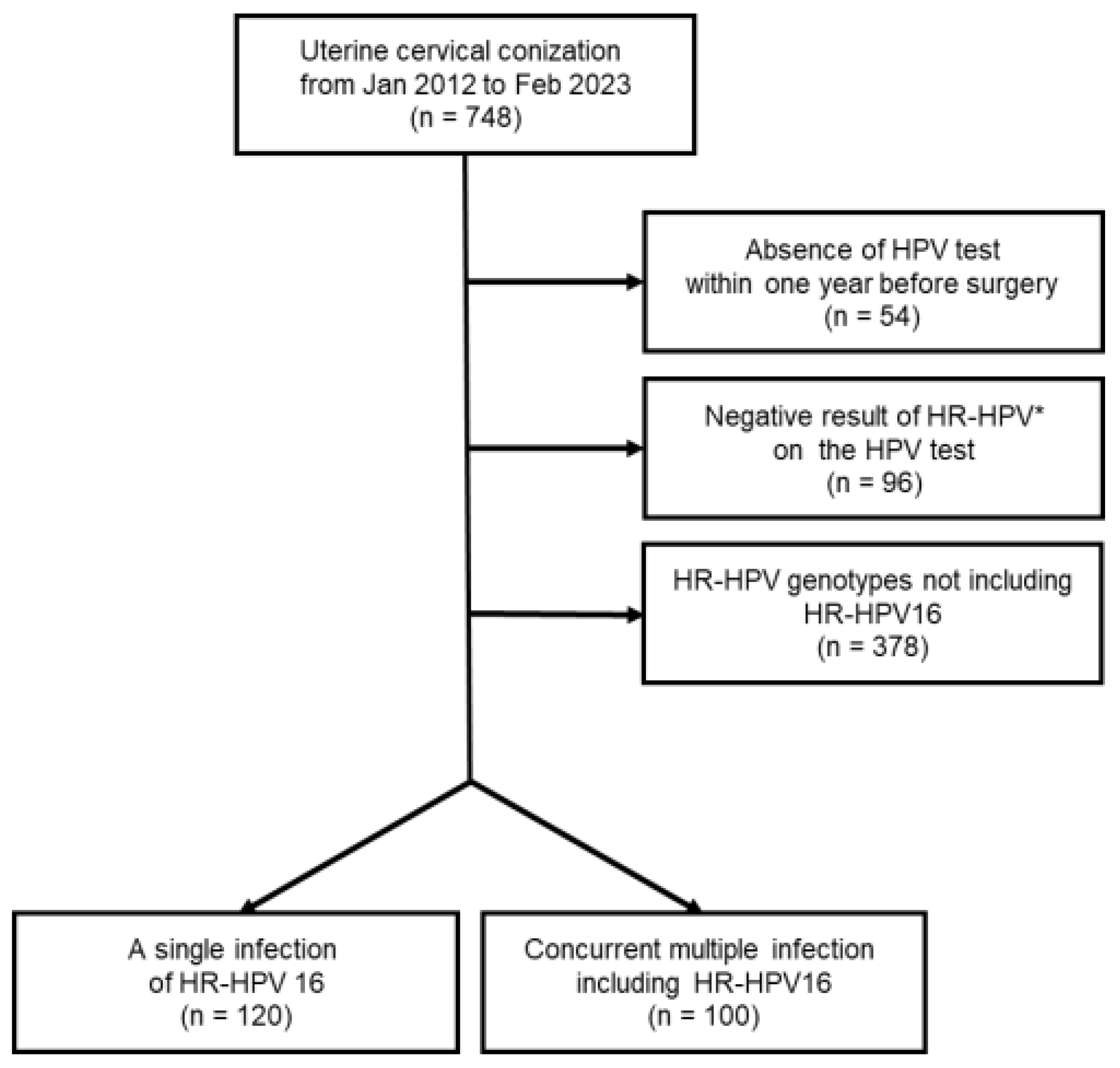
2.1. Patients
2.2. Initial and Final Diagnosis
2.3. Classification of CIS+
2.4. Statistical Analysis
2.5. Uterine Cervical Conization
2.6. HPV Test
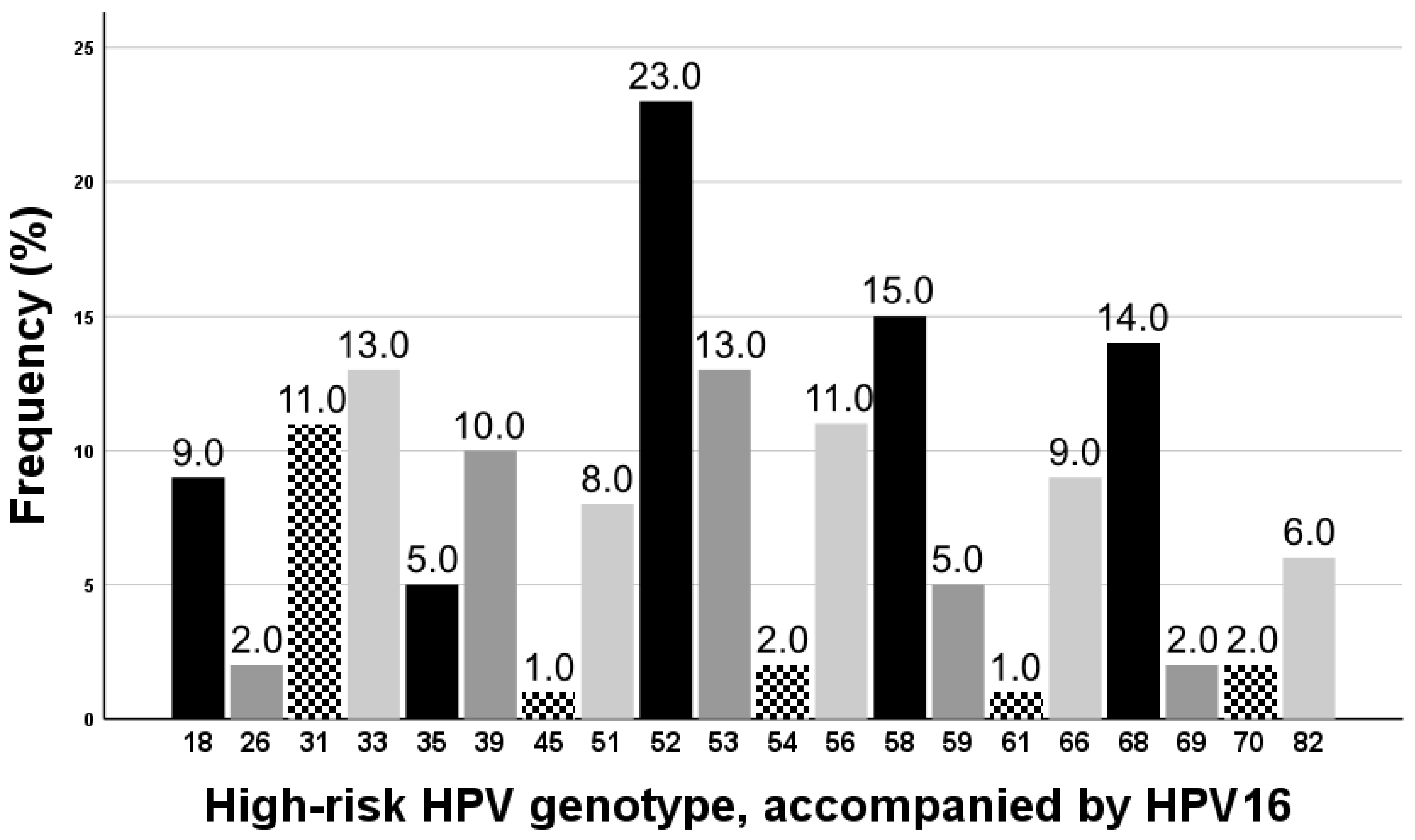
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.M.; Won, Y.J.; Jung, K.W.; Kong, H.J.; Cho, H.; Lee, J.K.; Lee, D.H.; Lee, K.H. Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2013. Cancer Res. Treat. 2016, 48, 436–450. [Google Scholar] [CrossRef] [PubMed]
- Bosch, F.X.; De Sanjosé, S. Chapter 1: Human papillomavirus and cervical cancer—Burden and assessment of causality. J. Natl. Cancer Inst. Monogr. 2003, 2003, 3–13. [Google Scholar] [CrossRef]
- Muñoz, N.; Bosch, F.X.; De Sanjosé, S.; Herrero, R.; Castellsagué, X.; Shah, K.V.; Snijders, P.J.; Meijer, C.J. Epidemiologic classification of human papillomavirus types associated with cervical cancer. N. Engl. J. Med. 2003, 348, 518–527. [Google Scholar] [CrossRef] [PubMed]
- Snijders, P.J.; Steenbergen, R.D.; Heideman, D.A.; Meijer, C.J. HPV-mediated cervical carcinogenesis: Concepts and clinical implications. J. Pathol. 2006, 208, 152–164. [Google Scholar] [CrossRef]
- Zur Hausen, H. Papillomaviruses and cancer: From basic studies to clinical application. Nat. Rev. Cancer 2002, 2, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Walboomers, J.M.; Jacobs, M.V.; Manos, M.M.; Bosch, F.X.; Kummer, J.A.; Shah, K.V.; Snijders, P.J.; Peto, J.; Meijer, C.J.; Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999, 189, 12–19. [Google Scholar] [CrossRef]
- Burd, E.M. Human papillomavirus and cervical cancer. Clin. Microbiol. Rev. 2003, 16, 1–17. [Google Scholar] [CrossRef]
- Maucort-Boulch, D.; Franceschi, S.; Plummer, M. International correlation between human papillomavirus prevalence and cervical cancer incidence. Cancer Epidemiol. Biomark. Prev. 2008, 17, 717–720. [Google Scholar] [CrossRef]
- So, K.A.; Lee, I.H.; Lee, K.H.; Hong, S.R.; Kim, Y.J.; Seo, H.H.; Kim, T.J. Human papillomavirus genotype-specific risk in cervical carcinogenesis. J. Gynecol. Oncol. 2019, 30, e52. [Google Scholar] [CrossRef]
- Park, E.; Kim, J.Y.; Choi, S.; Kim, D.S.; Oh, Y.L. Carcinogenic risk of human papillomavirus (HPV) genotypes and potential effects of HPV vaccines in Korea. Sci. Rep. 2019, 9, 12556. [Google Scholar] [CrossRef]
- Clifford, G.M.; Gallus, S.; Herrero, R.; Munoz, N.; Snijders, P.J.; Vaccarella, S.; Anh, P.T.; Ferreccio, C.; Hieu, N.T.; Matos, E. Worldwide distribution of human papillomavirus types in cytologically normal women in the International Agency for Research on Cancer HPV prevalence surveys: A pooled analysis. Lancet 2005, 366, 991–998. [Google Scholar] [CrossRef] [PubMed]
- De Sanjosé, S.; Diaz, M.; Castellsagué, X.; Clifford, G.; Bruni, L.; Muñoz, N.; Bosch, F.X. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: A meta-analysis. Lancet Infect. Dis. 2007, 7, 453–459. [Google Scholar] [CrossRef]
- Cuschieri, K.S.; Cubie, H.A.; Whitley, M.W.; Gilkison, G.; Arends, M.J.; Graham, C.; McGoogan, E. Persistent high risk HPV infection associated with development of cervical neoplasia in a prospective population study. J. Clin. Pathol. 2005, 58, 946–950. [Google Scholar] [CrossRef]
- De Sanjose, S.; Quint, W.G.; Alemany, L.; Geraets, D.T.; Klaustermeier, J.E.; Lloveras, B.; Tous, S.; Felix, A.; Bravo, L.E.; Shin, H.R.; et al. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010, 11, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Lehtinen, M.; Dillner, J. Clinical trials of human papillomaviarus vaccines and beyond. J. Nat. Rev. Clin. Oncol. 2013, 10, 400–410. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control and Prevention. Available online: https://nip.kdca.go.kr/irhp/infm/goVcntInfo.do?menuLv=1&menuCd=132 (accessed on 23 August 2023).
- Gupta, S.; Kumar, P.; Das, B.C. HPV: Molecular pathways and targets. Curr. Probl. Cancer 2018, 42, 161–174. [Google Scholar] [CrossRef]
- Sedman, S.; Barbosa, M.; Vass, W.; Hubbert, N.; Haas, J.; Lowy, D.; Schiller, J.T. The full-length E6 protein of human papillomavirus type 16 has transforming and trans-activating activities and cooperates with E7 to immortalize keratinocytes in culture. J. Virol. 1991, 65, 4860–4866. [Google Scholar] [CrossRef] [PubMed]
- Mirabello, L.; Clarke, M.A.; Nelson, C.W.; Dean, M.; Wentzensen, N.; Yeager, M.; Cullen, M.; Boland, J.F.; NCI HPV Workshop; Schiffman, M.; et al. The intersection of HPV epidemiology, genomics and mechanistic studies of HPV-mediated carcinogenesis. Viruses 2018, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, F.; Banks, L. The human papillomavirus E6 protein and its contribution to malignant progression. Oncogene 2001, 20, 7874–7887. [Google Scholar] [CrossRef]
- Gonzalez, S.L.; Stremlau, M.; He, X.; Basile, J.R.; Münger, K. Degradation of the retinoblastoma tumor suppressor by the human papillomavirus type 16 E7 oncoprotein is important for functional inactivation and is separable from proteasomal degradation of E7. J. Virol. 2001, 75, 7583–7591. [Google Scholar] [CrossRef]
- Wheeler, C.M.; Hunt, W.C.; Cuzick, J.; Langsfeld, E.; Pearse, A.; Montoya, G.D.; Robertson, M.; Shearman, C.A.; Castle, P.E. A population-based study of human papillomavirus genotype prevalence in the United States: Baseline measures prior to mass human papillomavirus vaccination. Int. J. Cancer 2013, 132, 198–207. [Google Scholar] [CrossRef]
- Carozzi, F.; Ronco, G.; Gillio-Tos, A.; De Marco, L.; Del Mistro, A.; Girlando, S.; Franceschi, S.; Plummer, M.; Vaccarella, S. Concurrent infections with multiple human papillomavirus (HPV) types in the New Technologies for Cervical Cancer (NTCC) screening study. Eur. J. Cancer 2012, 48, 1633–1637. [Google Scholar] [CrossRef] [PubMed]
- Vaccarella, S.; Franceschi, S.; Snijders, P.J.; Herrero, R.; Meijer, C.J.; Plummer, M. Concurrent infection with multiple human papillomavirus types: Pooled analysis of the IARC HPV Prevalence Surveys. Cancer Epidemiol. Biomark. Prev. 2010, 19, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Tjalma, W.A.; Fiander, A.; Reich, O.; Powell, N.; Nowakowski, A.M.; Kirschner, B.; Koiss, R.; O’Leary, J.; Joura, E.A.; Rosenlund, M.; et al. Differences in human papillomavirus type distribution in high-grade cervical intraepithelial neoplasia and invasive cervical cancer in Europe. Int. J. Cancer 2013, 132, 854–867. [Google Scholar] [CrossRef] [PubMed]
- Solomon, D.; Davey, D.; Kurman, R.; Moriarty, A.; O’Connor, D.; Prey, M.; Raab, S.; Sherman, M.; Wilbur, D.; Wright, T., Jr.; et al. The 2001 Bethesda System: Terminology for reporting results of cervical cytology. JAMA 2002, 287, 2114–2119. [Google Scholar] [CrossRef]
- Ko, K.; Kwon, M.J.; Lee, E.H.; Woo, H.Y.; Park, H. Comparison of GeneFinder human papillomavirus (HPV) liquid beads microarray PCR kit and hybrid capture 2 assay for detection of HPV infection. J. Clin. Lab. Anal. 2017, 31, e22025. [Google Scholar] [CrossRef]
- An, H.; Song, K.S.; Nimse, S.B.; Kim, J.; Nguyen, V.T.; Ta, V.T.; Sayyed, D.R.; Kim, T. HPV 9G DNA chip: 100% clinical sensitivity and specificity. J. Clin. Microbiol. 2012, 50, 562–568. [Google Scholar] [CrossRef]
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef]
| Single Infection Group (n = 120) | Concurrent Multiple Infection Group (n = 100) | p-Value | |
|---|---|---|---|
| Age (yrs) | 45.37 ± 12.81 | 42.90 ± 15.84 | 0.212 * |
| Gravida (n) | 2.58 ± 1.74 | 2.28 ± 2.39 | 0.292 * |
| Parity (n) | 1.63 ± 1.11 | 1.19 ± 1.32 | 0.008 * |
| Abortion (n) | 0.96 ± 0.99 | 1.09 ± 1.42 | 0.436 * |
| Number of infection with high-risk HPVs (range) | 1 | 2.63 ± 0.98 | <0.001 * |
| 6 genotypes | 2 (2.0%) | ||
| 5 genotypes | 5 (5.0%) | ||
| 4 genotypes | 9 (9.0%) | ||
| 3 genotypes | 22 (22.0%) | ||
| 2 genotypes | 62 (62.0%) | ||
| Initial diagnosis ‡ (n) | |||
| Normal | 1 (0.8%) | 1 (1.0%) | >0.999 † |
| Atypical cells | 9 (7.5%) | 4 (4.0%) | 0.391 † |
| LSIL | 10 (8.3%) | 5 (5.0%) | 0.424 † |
| HSIL § | 52 (43.3%) | 61 (61.0%) | 0.010 † |
| Carcinoma in situ ¶ | 43 (35.8%) | 25 (25.0%) | 0.107 † |
| Invasive carcinoma | 5 (4.2%) | 4 (4.0%) | >0.999 † |
| Whole Group | Subgroup (≤40 Years) | Subgroup (>40 Years) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Single Infection (n = 120) | Multiple Infection (n = 100) | p-Value | Single Infection (n = 45) | Multiple Infection (n = 50) | p-Value | Single Infection (n = 75) | Multiple Infection (n = 50) | p-Value | |
| Normal | 19 (15.8%) | 5 (5.0%) | 0.015 | 5 (11.1%) | 1 (2.0%) | 0.098 | 14 (18.7%) | 4 (8.0%) | 0.122 |
| Atypical cells | 3 (2.5%) | 1 (1.0%) | 0.628 | 0 (0%) | 1 (2.0%) | >0.999 | 3 (4.0%) | 0 (0%) | 0.274 |
| LSIL | 11 (9.2%) | 13 (13.0%) | 0.392 | 2 (4.4%) | 3 (6.0%) | >0.999 | 9 (12.0%) | 10 (20.0%) | 0.309 |
| HSIL † | 19 (15.8%) | 33 (33.0%) | 0.004 * | 11 (24.4%) | 20 (40.0%) | 0.128 | 8 (10.7%) | 13 (26.0%) | 0.030 * |
| Carcinoma in situ ‡ | 60 (50.0%) | 45 (45.0%) | 0.499 | 25 (55.6%) | 24 (48.0%) | 0.539 | 35 (46.7%) | 21 (42.0%) | 0.714 |
| Invasive carcinoma | 8 (6.7%) | 3 (3.0%) | 0.352 | 2 (4.4%) | 1 (2.0%) | 0.602 | 6 (8.0%) | 2 (4.0%) | 0.474 |
| HSIL+ | 87 (72.5%) | 81 (81.0%) | 0.154 | 38 (84.4%) | 45 (90.0%) | 0.540 | 49 (65.3%) | 36 (72.0%) | 0.557 |
| CIS+ | 68 (56.7%) | 48 (48.0%) | 0.223 | 27 (60.0%) | 25 (25.0%) | 0.410 | 41 (54.7%) | 23 (46.0%) | 0.366 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Lee, H.J. Do Concurrent Multiple Infections with High-Risk HPVs Carry a More Malignant Potential than a Single Infection in the Uterine Cervix? J. Clin. Med. 2023, 12, 6155. https://doi.org/10.3390/jcm12196155
Lee J, Lee HJ. Do Concurrent Multiple Infections with High-Risk HPVs Carry a More Malignant Potential than a Single Infection in the Uterine Cervix? Journal of Clinical Medicine. 2023; 12(19):6155. https://doi.org/10.3390/jcm12196155
Chicago/Turabian StyleLee, Juhun, and Hyun Jung Lee. 2023. "Do Concurrent Multiple Infections with High-Risk HPVs Carry a More Malignant Potential than a Single Infection in the Uterine Cervix?" Journal of Clinical Medicine 12, no. 19: 6155. https://doi.org/10.3390/jcm12196155
APA StyleLee, J., & Lee, H. J. (2023). Do Concurrent Multiple Infections with High-Risk HPVs Carry a More Malignant Potential than a Single Infection in the Uterine Cervix? Journal of Clinical Medicine, 12(19), 6155. https://doi.org/10.3390/jcm12196155





