Treatment of Fracture-Related Infection after Pelvic Fracture
Abstract
:1. Introduction
2. Methods
- Age over 18;
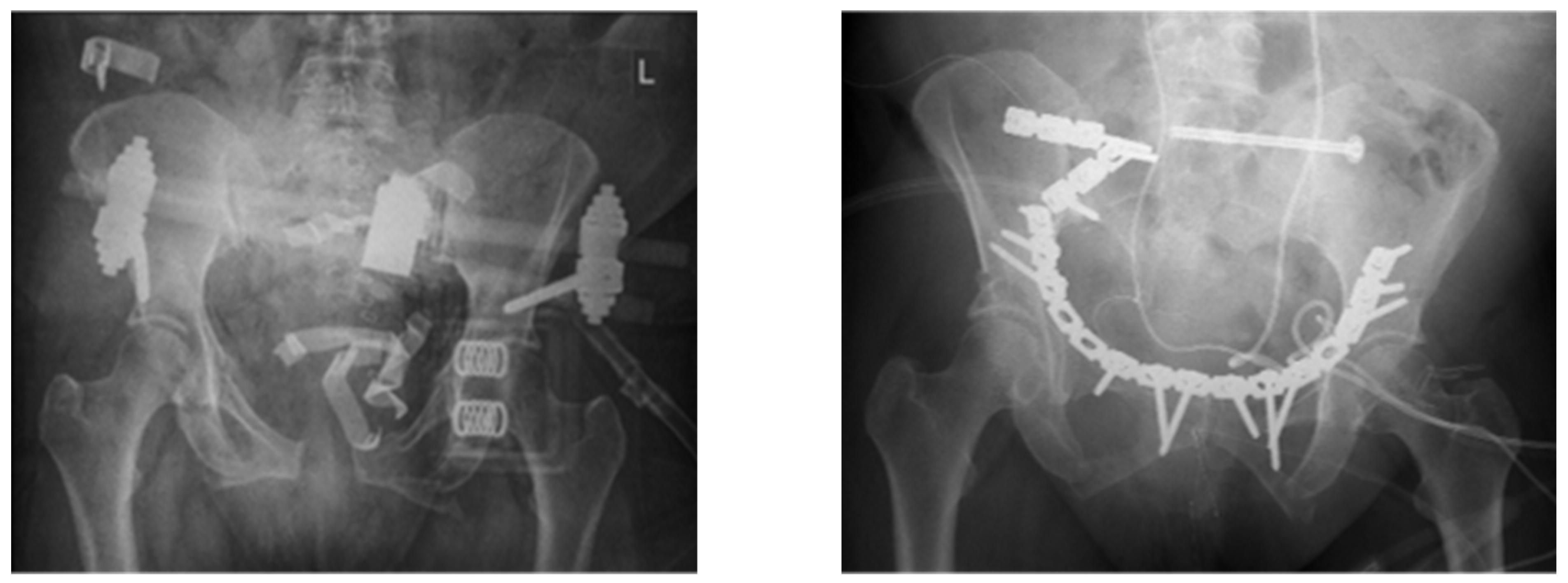
- Pelvic fracture treatment with open reduction and internal fixation;
- FRI diagnosed according to clinical symptoms of infection AND a positive culture of a bacterial infection;
- A complete dataset regarding preoperative and postoperative computed tomography.
- Isolated external fixator treatment (pin track infection);
- Missing data or lack of consent to participate in the study.
2.1. Initial Surgical Management and After-Care
2.2. Surgical Management of Fracture-Related Infection
2.3. Statistical Analysis
3. Results
3.1. Demographics and Clinical Characteristics
3.2. Treatment Strategies and Risk Factors for Recurrent Infections
3.3. Microbiology and Anti-Infective Therapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marmor, M.; El Naga, A.N.; Barker, J.; Matz, J.; Stergiadou, S.; Miclau, T. Management of Pelvic Ring Injury Patients with Hemodynamic Instability. Front. Surg. 2020, 7, 588845. [Google Scholar] [CrossRef]
- Ruatti, S.; Guillot, S.; Brun, J.; Thony, F.; Bouzat, P.; Payen, J.F.; Tonetti, J. Which Pelvic Ring Fractures Are Potentially Lethal? Injury 2015, 46, 1059–1063. [Google Scholar] [CrossRef]
- Mann, S.M.; Banaszek, D.; Lajkosz, K.; Brogly, S.B.; Stanojev, S.M.; Evans, C.; Bardana, D.D.; Yach, J.; Hall, S. High-Energy Trauma Patients with Pelvic Fractures: Management Trends in Ontario, Canada. Injury 2018, 49, 1830–1840. [Google Scholar] [CrossRef]
- Chen, H.-T.; Wang, Y.-C.; Hsieh, C.-C.; Su, L.-T.; Wu, S.-C.; Lo, Y.-S.; Chang, C.-C.; Tsai, C.-H. Trends and Predictors of Mortality in Unstable Pelvic Ring Fracture: A 10-Year Experience with a Multidisciplinary Institutional Protocol. World J. Emerg. Surg. 2019, 14, 61. [Google Scholar] [CrossRef]
- Durão, C.; Alves, M.; Barros, A.; Pedrosa, F. The Importance of Pelvic Ring Stabilization as a Life-Saving Measure in Pre-Hospital—A Case Report Commented by Autopsy. J. Clin. Orthop. Trauma 2017, 8, S17–S20. [Google Scholar] [CrossRef]
- The Role of Pelvic Packing for Hemodynamically Unstable Pelvic Ring Injuries—Thomas Lustenberger, Sebastian Wutzler, Philipp Störmann, Ingo Marzi. 2015. Available online: https://journals.sagepub.com/doi/10.4137/CMTIM.S12257 (accessed on 29 November 2022).
- Pelvic Ring Fractures: What the Orthopedic Surgeon Wants to Know|RadioGraphics. Available online: https://pubs.rsna.org/doi/10.1148/rg.345135113 (accessed on 29 November 2022).
- Pavelka, T.; Salášek, M.; Weisová, D. Complications associated with surgical treatment of pelvic ring fractures. Acta Chir. Orthop. Traumatol. Cechoslov. 2013, 80, 208–215. [Google Scholar] [CrossRef]
- Kanakaris, N.K.; Ciriello, V.; Stavrou, P.Z.; West, R.M.; Giannoudis, P.V. Deep Infection following Reconstruction of Pelvic Fractures: Prevalence, Characteristics, and Predisposing Risk Factors. Eur. J. Trauma Emerg. Surg. 2022, 48, 3701–3709. [Google Scholar] [CrossRef]
- Metsemakers, W.-J.; Onsea, J.; Neutjens, E.; Steffens, E.; Schuermans, A.; McNally, M.; Nijs, S. Prevention of Fracture-Related Infection: A Multidisciplinary Care Package. Int. Orthop. 2017, 41, 2457–2469. [Google Scholar] [CrossRef]
- Iliaens, J.; Onsea, J.; Hoekstra, H.; Nijs, S.; Peetermans, W.E.; Metsemakers, W.-J. Fracture-Related Infection in Long Bone Fractures: A Comprehensive Analysis of the Economic Impact and Influence on Quality of Life. Injury 2021, 52, 3344–3349. [Google Scholar] [CrossRef]
- O’Connor, O.; Thahir, A.; Krkovic, M. How Much Does an Infected Fracture Cost? Arch. Bone Jt. Surg. 2022, 10, 135–140. [Google Scholar] [CrossRef]
- Walter, N.; Rupp, M.; Lang, S.; Alt, V. The Epidemiology of Fracture-Related Infections in Germany. Sci. Rep. 2021, 11, 10443. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.A.; Ochsner, P.E.; Kuehl, R.; Raschke, M.; et al. Fracture-Related Infection: A Consensus on Definition from an International Expert Group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Govaert, G.A.M.; Kuehl, R.; Atkins, B.L.; Trampuz, A.; Morgenstern, M.; Obremskey, W.T.; Verhofstad, M.H.J.; McNally, M.A.; Metsemakers, W.-J.; Fracture-Related Infection (FRI) Consensus Group. Diagnosing Fracture-Related Infection: Current Concepts and Recommendations. J. Orthop. Trauma 2020, 34, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Puetzler, J.; Zalavras, C.; Moriarty, T.F.; Verhofstad, M.H.J.; Kates, S.L.; Raschke, M.-J.; Rosslenbroich, S.; Metsemakers, W.-J. Clinical Practice in Prevention of Fracture-Related Infection: An International Survey among 1197 Orthopaedic Trauma Surgeons. Injury 2019, 50, 1208–1215. [Google Scholar] [CrossRef] [PubMed]
- Lu, V.; Zhang, J.; Patel, R.; Zhou, A.K.; Thahir, A.; Krkovic, M. Fracture Related Infections and Their Risk Factors for Treatment Failure—A Major Trauma Centre Perspective. Diagnostics 2022, 12, 1289. [Google Scholar] [CrossRef] [PubMed]
- Makihara, K.; Takegami, Y.; Tokutake, K.; Yamauchi, K.; Hiramatsu, Y.; Matsuura, Y.; Imagama, S. Risk Factors for Fracture-Related Infection after Open Reduction and Internal Fixation of Proximal Humerus Fractures: A Multicenter Retrospective Study of 496 Fractures (TRON Group Study). Injury 2022, 53, 2573–2578. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.R.; Hux, J.E. Quantifying the Risk of Infectious Diseases for People with Diabetes. Diabetes Care 2003, 26, 510–513. [Google Scholar] [CrossRef]
- Carrillo-Larco, R.M.; Anza-Ramírez, C.; Saal-Zapata, G.; Villarreal-Zegarra, D.; Zafra-Tanaka, J.H.; Ugarte-Gil, C.; Bernabé-Ortiz, A. Type 2 Diabetes Mellitus and Antibiotic-Resistant Infections: A Systematic Review and Meta-Analysis. J. Epidemiol. Community Health 2022, 76, 75–84. [Google Scholar] [CrossRef]
- Al, G.; Ll, H.; Gd, S. Immunosenescence of Ageing. J. Pathol. 2007, 211, 144–156. [Google Scholar] [CrossRef]
- Gerstein, A.D.; Phillips, T.J.; Rogers, G.S.; Gilchrest, B.A. Wound Healing and Aging. Dermatol. Clin. 1993, 11, 749–757. [Google Scholar] [CrossRef]
- Tamma, P.D.; Cosgrove, S.E. Antimicrobial Stewardship. Infect. Dis. Clin. N. Am. 2011, 25, 245–260. [Google Scholar] [CrossRef] [PubMed]
- Struijs, P.A.A.; Poolman, R.W.; Bhandari, M. Infected Nonunion of the Long Bones. J. Orthop. Trauma 2007, 21, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Knabl, L.; Kuppelwieser, B.; Mayr, A.; Posch, W.; Lackner, M.; Coraça-Huber, D.; Danita, A.; Blauth, M.; Lass-Flörl, C.; Orth-Höller, D. High Percentage of Microbial Colonization of Osteosynthesis Material in Clinically Unremarkable Patients. Microbiologyopen 2018, 8, e00658. [Google Scholar] [CrossRef] [PubMed]
- Halvachizadeh, S.; Pape, H.-C. Perren’s Strain Theory and Fracture Healing. In Essential Biomechanics for Orthopedic Trauma: A Case-Based Guide; Crist, B.D., Borrelli, J., Jr., Harvey, E.J., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 17–25. ISBN 978-3-030-36990-3. [Google Scholar]
- Foster, A.L.; Moriarty, T.F.; Zalavras, C.; Morgenstern, M.; Jaiprakash, A.; Crawford, R.; Burch, M.-A.; Boot, W.; Tetsworth, K.; Miclau, T.; et al. The Influence of Biomechanical Stability on Bone Healing and Fracture-Related Infection: The Legacy of Stephan Perren. Injury 2021, 52, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Greene, L.R. Guide to the Elimination of Orthopedic Surgery Surgical Site Infections: An Executive Summary of the Association for Professionals in Infection Control and Epidemiology Elimination Guide. Am. J. Infect. Control 2012, 40, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Metsemakers, W.J.; Kuehl, R.; Moriarty, T.F.; Richards, R.G.; Verhofstad, M.H.J.; Borens, O.; Kates, S.; Morgenstern, M. Infection after Fracture Fixation: Current Surgical and Microbiological Concepts. Injury 2018, 49, 511–522. [Google Scholar] [CrossRef]
- Depypere, M.; Morgenstern, M.; Kuehl, R.; Senneville, E.; Moriarty, T.F.; Obremskey, W.T.; Zimmerli, W.; Trampuz, A.; Lagrou, K.; Metsemakers, W.-J. Pathogenesis and Management of Fracture-Related Infection. Clin. Microbiol. Infect. 2020, 26, 572–578. [Google Scholar] [CrossRef]
- Depypere, M.; Kuehl, R.; Metsemakers, W.-J.; Senneville, E.; McNally, M.A.; Obremskey, W.T.; Zimmerli, W.; Atkins, B.L.; Trampuz, A. Recommendations for Systemic Antimicrobial Therapy in Fracture-Related Infection: A Consensus From an International Expert Group. J. Orthop. Trauma 2020, 34, 30–41. [Google Scholar] [CrossRef]
- Influence of Fracture Stability on Staphylococcus epidermidis and Staphylococcus aureus Infection in a Murine Femoral Fracture Model—Zurich Open Repository and Archive. Available online: https://www.zora.uzh.ch/id/eprint/148995/ (accessed on 14 November 2022).
- Merritt, K.; Dowd, J.D. Role of Internal Fixation in Infection of Open Fractures: Studies with Staphylococcus aureus and Proteus mirabilis. J. Orthop. Res. 1987, 5, 23–28. [Google Scholar] [CrossRef]
- Tschudin-Sutter, S.; Frei, R.; Dangel, M.; Jakob, M.; Balmelli, C.; Schaefer, D.J.; Weisser, M.; Elzi, L.; Battegay, M.; Widmer, A.F. Validation of a Treatment Algorithm for Orthopaedic Implant-Related Infections with Device-Retention—Results from a Prospective Observational Cohort Study. Clin. Microbiol. Infect. 2016, 22, 457.e1–457.e9. [Google Scholar] [CrossRef]
- Barberán, J.; Aguilar, L.; Giménez, M.-J.; Carroquino, G.; Granizo, J.-J.; Prieto, J. Levofloxacin plus Rifampicin Conservative Treatment of 25 Early Staphylococcal Infections of Osteosynthetic Devices for Rigid Internal Fixation. Int. J. Antimicrob. Agents 2008, 32, 154–157. [Google Scholar] [CrossRef] [PubMed]
- Acute Infections After Fracture Repair|SpringerLink. Available online: https://link.springer.com/article/10.1007/s11999-007-0053-y (accessed on 14 November 2022).
- Parsons, B.; Strauss, E. Surgical Management of Chronic Osteomyelitis. Am. J. Surg. 2004, 188, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Rupp, M.; Hierl, K.; Pfeifer, C.; Kerschbaum, M.; Hinterberger, T.; Alt, V. Long-Term Patient-Related Quality of Life after Fracture-Related Infections of the Long Bones. Bone Jt. Res. 2021, 10, 321–327. [Google Scholar] [CrossRef] [PubMed]
| n = 24 | High-Energy Trauma (n = 17) | Low-Energy Trauma (n = 7) | Total | |
|---|---|---|---|---|
| Age | 51.8 (±20.7) | 74.8 (±7.3) | 58.1 (±20.9) | |
| Gender | 5 female/12 male | 5 female/2 male | 9 female/15 male | |
| ASA Score | 8× ASA 2 7× ASA 3 2× ASA 4 | 2× ASA 2 5× ASA 3 | 10× ASA 2 12× ASA 3 2× ASA 4 | |
| Fracture Classification | AO/OTA 5× B-type, 12× C-type | Rommens 4× IIIa, 2× IIIb, 1× IVa | ||
| Stabilization Method | anterior | 15× plate | 1× plate | 16× plate |
| 1× Fix ex | 4× Fix ex | 5× Fix ex | ||
| posterior | 7× screws | 3× screws | 10× screws | |
| 2× plate | 2× plate | 4× plate | ||
| 3× TIFI | 2× TIFI | 5× TIFI | ||
| 2× lumbo-pelvic | 1× lumbo-pelvic | 3× lumbo-pelvic | ||
| Microbiology Results | n = |
|---|---|
| Staphylococcus epidermidis | 9 |
| Staphylococcus aureus | 7 |
| Staphylococcus haemolyticus | 2 |
| Staphylococcus lugdunensis | 2 |
| Staphylococcus caprae | 1 |
| Staphylococcus warneri | 1 |
| E. coli | 5 |
| E. faecium | 5 |
| Proteus mirabilis | 3 |
| Enterobacter cloacae | 2 |
| Klebsiella | 2 |
| Stenotrophomonas maltophilia | 1 |
| Pseudomonas aeroginosa | 1 |
| Propionibacterium species | 1 |
| Cutibacterium acnes | 1 |
| Bacillus megaterium | 1 |
| Corynebacterium amylonatum | 1 |
| Fusarium | 1 |
| Bacillus cereus | 1 |
| Picha norvegensis | 1 |
| Citerobacter freundii | 1 |
| Candida albicans | 2 |
| Aspergillus flavus | 1 |
| Cultural combinations in 17 poly-microbial infection cases | |
| - Citerobacter freundii + Picha norvegiensis + Bacteroides sp. + Aspergillus flavus | |
| - Staph haemolyticus + E. faecium + Candida albicans | |
| - Staph. epi + E. coli | |
| - Staph. epi + Proteus mirabilis | |
| - Staph. epi + Pseudomonas aerogenosa + Proteus mirabilis | |
| - Staph. epi + Staph haemolyticus + E.faecium | |
| - Stenotrophomonas maltophilia + Corynebacterium amylonatum + Bacillus cereus + Fusarium spp. + Candida albicans | |
| - Staph. aureus + Staph. epi | |
| - Staph. aureus + E. coli | |
| - Staph epi + Staph aureus + Klebsiella | |
| - Staph aureus + Enterobacter cloacae | |
| - Staph. epi + Staph caprae + Klebsiella + E. faecium | |
| - Staph. epi + E. cloacae | |
| - E. coli + E. faecium | |
| - Staph. aureus + Bacillus megaterium | |
| - Staph. epi + E. faecium + Proteus mirabilis | |
| - Staph aureus + Staph. warneri | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freigang, V.; Walter, N.; Rupp, M.; Riedl, M.; Alt, V.; Baumann, F. Treatment of Fracture-Related Infection after Pelvic Fracture. J. Clin. Med. 2023, 12, 6221. https://doi.org/10.3390/jcm12196221
Freigang V, Walter N, Rupp M, Riedl M, Alt V, Baumann F. Treatment of Fracture-Related Infection after Pelvic Fracture. Journal of Clinical Medicine. 2023; 12(19):6221. https://doi.org/10.3390/jcm12196221
Chicago/Turabian StyleFreigang, Viola, Nike Walter, Markus Rupp, Moritz Riedl, Volker Alt, and Florian Baumann. 2023. "Treatment of Fracture-Related Infection after Pelvic Fracture" Journal of Clinical Medicine 12, no. 19: 6221. https://doi.org/10.3390/jcm12196221






