Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children—A Single-Center Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Procedures and Participants
2.2. Anthropometric Measurements and CRF Measurement
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Group (Anthropometric Measures and Indices)
3.2. Regression Models
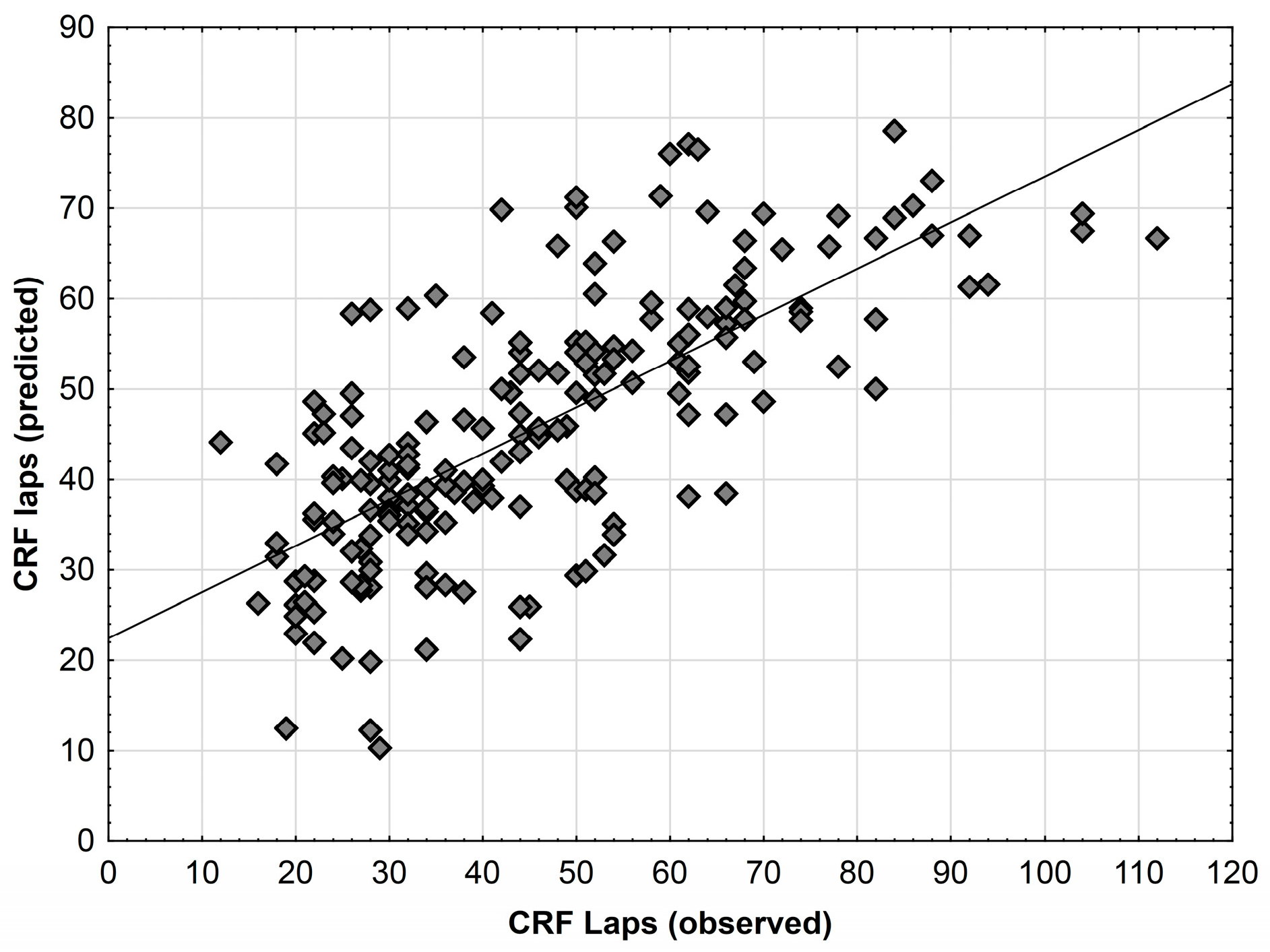
3.3. Multivariable Models
3.3.1. Multivariable Model for the Whole Test Group
3.3.2. Multivariable Models—Separate for Girls and Boys
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, H.J.; Shim, Y.S.; Yoon, J.S.; Jeong, H.R.; Kang, M.J.; Hwang, I.T. Distribution of Waist-to-Height Ratio and Cardiometabolic Risk in Children and Adolescents: A Population-Based Study. Sci. Rep. 2021, 11, 9524. [Google Scholar] [CrossRef]
- Shen, S.; Lu, Y.; Qi, H.; Li, F.; Shen, Z.; Wu, L.; Yang, C.; Wang, L.; Shui, K.; Yao, W.; et al. Waist-to-Height Ratio Is an Effective Indicator for Comprehensive Cardiovascular Health. Sci. Rep. 2017, 7, 43046. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Liu, A.; Zhao, T.; Gong, X.; Pang, T.; Zhou, Y.; Xiao, Y.; Yan, Y.; Fan, C.; Teng, W.; et al. Comparison of Anthropometric Indices for Predicting the Risk of Metabolic Syndrome and Its Components in Chinese Adults: A Prospective, Longitudinal Study. BMJ Open 2017, 7, e016062. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gibson, S. Waist-to-Height Ratio as an Indicator of “Early Health Risk”: Simpler and More Predictive than Using a “matrix” Based on BMI and Waist Circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed]
- Lo, K.; Huang, Y.-Q.; Shen, G.; Huang, J.-Y.; Liu, L.; Yu, Y.-L.; Chen, C.-L.; Feng, Y.Q. Effects of Waist to Height Ratio, Waist Circumference, Body Mass Index on the Risk of Chronic Diseases, All-Cause, Cardiovascular and Cancer Mortality. Postgrad. Med. J. 2021, 97, 306–311. [Google Scholar] [CrossRef] [PubMed]
- Ononamadu, C.J.; Ezekwesili, C.N.; Onyeukwu, O.F.; Umeoguaju, U.F.; Ezeigwe, O.C.; Ihegboro, G.O. Comparative Analysis of Anthropometric Indices of Obesity as Correlates and Potential Predictors of Risk for Hypertension and Prehypertension in a Population in Nigeria. Cardiovasc. J. Afr. 2017, 28, 92–99. [Google Scholar] [CrossRef]
- Agirbasli, M.; Agaoglu, N.B.; Ergonul, O.; Yagmur, I.; Aydogar, H.; Oneri, T.; Ozturk, O. Comparison of Anthropometric Indices in Predicting Metabolic Syndrome Components in Children. Metab. Syndr. Relat. Disord. 2011, 9, 453–459. [Google Scholar] [CrossRef]
- López-González, D.; Miranda-Lora, A.; Klünder-Klünder, M.; Queipo-García, G.; Bustos-Esquivel, M.; Paez-Villa, M.; Villanueva-Ortega, E.; Chávez-Requena, I.; Laresgoiti-Servitje, E.; Garibay-Nieto, N. Diagnostic Performance of Waist Circumference Measurements for Predicting Cardiometabolic Risk in Mexican Children. Endocr. Pract. Off. J. Am. Coll. Endocrinol. Am. Assoc. Clin. Endocrinol. 2016, 22, 1170–1176. [Google Scholar] [CrossRef]
- Tee, J.Y.H.; Gan, W.Y.; Lim, P.Y. Comparisons of Body Mass Index, Waist Circumference, Waist-to-Height Ratio and a Body Shape Index (ABSI) in Predicting High Blood Pressure among Malaysian Adolescents: A Cross-Sectional Study. BMJ Open 2020, 10, e032874. [Google Scholar] [CrossRef]
- Kułaga, Z.; Świąder-Leśniak, A.; Kotowska, A.; Litwin, M. Population-Based References for Waist and Hip Circumferences, Waist-to-Hip and Waist-to-Height Ratios for Children and Adolescents, and Evaluation of Their Predictive Ability. Eur. J. Pediatr. 2023, 182, 3217–3229. [Google Scholar] [CrossRef]
- Zeng, Q.; He, Y.; Dong, S.; Zhao, X.; Chen, Z.; Song, Z.; Chang, G.; Yang, F.; Wang, Y. Optimal Cut-off Values of BMI, Waist Circumference and Waist:Height Ratio for Defining Obesity in Chinese Adults. Br. J. Nutr. 2014, 112, 1735–1744. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Guideline: Integrated Management of Adolescents in All Their Diversity with Obesity. Available online: https://www.who.int/news-room/events/detail/2022/12/08/default-calendar/who-guideline-integrated-management-of-adolescent-in-all-their-diversity-with-obesity (accessed on 4 August 2023).
- Antonopoulos, A.S.; Oikonomou, E.K.; Antoniades, C.; Tousoulis, D. From the BMI Paradox to the Obesity Paradox: The Obesity-Mortality Association in Coronary Heart Disease. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2016, 17, 989–1000. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, M.C.; Correia, M.I.T.D.; Heymsfield, S.B. A Requiem for BMI in the Clinical Setting. Curr. Opin. Clin. Nutr. Metab. Care 2017, 20, 314–321. [Google Scholar] [CrossRef] [PubMed]
- Elagizi, A.; Kachur, S.; Lavie, C.J.; Carbone, S.; Pandey, A.; Ortega, F.B.; Milani, R.V. An Overview and Update on Obesity and the Obesity Paradox in Cardiovascular Diseases. Prog. Cardiovasc. Dis. 2018, 61, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Carbone, S.; Canada, J.M.; Billingsley, H.E.; Siddiqui, M.S.; Elagizi, A.; Lavie, C.J. Obesity Paradox in Cardiovascular Disease: Where Do We Stand? Vasc. Health Risk Manag. 2019, 15, 89–100. [Google Scholar] [CrossRef]
- Marin-Jimenez, N.; Cruz-Leon, C.; Sanchez-Oliva, D.; Jimenez-Iglesias, J.; Caraballo, I.; Padilla-Moledo, C.; Cadenas-Sanchez, C.; Cuenca-Garcia, M.; Castro-Piñero, J. Criterion-Related Validity of Field-Based Methods and Equations for Body Composition Estimation in Adults: A Systematic Review. Curr. Obes. Rep. 2022, 11, 336–349. [Google Scholar] [CrossRef]
- Bray, G.A. Beyond BMI. Nutrients 2023, 15, 2254. [Google Scholar] [CrossRef]
- Bergman, R.N.; Stefanovski, D.; Buchanan, T.A.; Sumner, A.E.; Reynolds, J.C.; Sebring, N.G.; Xiang, A.H.; Watanabe, R.M. A Better Index of Body Adiposity. Obesity 2011, 19, 1083–1089. [Google Scholar] [CrossRef]
- Peterson, C.M.; Su, H.; Thomas, D.M.; Heo, M.; Golnabi, A.H.; Pietrobelli, A.; Heymsfield, S.B. Tri-Ponderal Mass Index vs Body Mass Index in Estimating Body Fat During Adolescence. JAMA Pediatr. 2017, 171, 629–636. [Google Scholar] [CrossRef]
- Woolcott, O.O.; Bergman, R.N. Relative Fat Mass (RFM) as a New Estimator of Whole-Body Fat Percentage—A Cross-Sectional Study in American Adult Individuals. Sci. Rep. 2018, 8, 10980. [Google Scholar] [CrossRef]
- Woolcott, O.O.; Bergman, R.N. Relative Fat Mass as an Estimator of Whole-Body Fat Percentage among Children and Adolescents: A Cross-Sectional Study Using NHANES. Sci. Rep. 2019, 9, 15279. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Huang, Y.; Lo, K.; Huang, Y.; Chen, J.; Feng, Y. Quotient of Waist Circumference and Body Mass Index: A Valuable Indicator for the High-Risk Phenotype of Obesity. Front. Endocrinol. 2021, 12, 697437. [Google Scholar] [CrossRef] [PubMed]
- Ripka, W.L.; Orsso, C.E.; Haqq, A.M.; Prado, C.M.; Ulbricht, L.; Leite, N. Validity and Accuracy of Body Fat Prediction Equations Using Anthropometrics Measurements in Adolescents. Eat. Weight Disord. EWD 2021, 26, 879–886. [Google Scholar] [CrossRef]
- Sun, J.; Yang, R.; Zhao, M.; Bovet, P.; Xi, B. Tri-Ponderal Mass Index as a Screening Tool for Identifying Body Fat and Cardiovascular Risk Factors in Children and Adolescents: A Systematic Review. Front. Endocrinol. 2021, 12, 694681. [Google Scholar] [CrossRef] [PubMed]
- Guzmán-León, A.E.; Velarde, A.G.; Vidal-Salas, M.; Urquijo-Ruiz, L.G.; Caraveo-Gutiérrez, L.A.; Valencia, M.E. External Validation of the Relative Fat Mass (RFM) Index in Adults from North-West Mexico Using Different Reference Methods. PLoS ONE 2019, 14, e0226767. [Google Scholar] [CrossRef]
- Paek, J.K.; Kim, J.; Kim, K.; Lee, S.Y. Usefulness of Relative Fat Mass in Estimating Body Adiposity in Korean Adult Population. Endocr. J. 2019, 66, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Jayawardena, R.; Ranasinghe, P.; Ranathunga, T.; Mathangasinghe, Y.; Wasalathanththri, S.; Hills, A.P. Novel Anthropometric Parameters to Define Obesity and Obesity-Related Disease in Adults: A Systematic Review. Nutr. Rev. 2020, 78, 498–513. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Castro-Piñero, J.; Artero, E.G.; Ortega, F.B.; Sjöström, M.; Suni, J.; Castillo, M.J. Predictive Validity of Health-Related Fitness in Youth: A Systematic Review. Br. J. Sports Med. 2009, 43, 909–923. [Google Scholar] [CrossRef]
- Kaminsky, L.A.; Arena, R.; Ellingsen, Ø.; Harber, M.P.; Myers, J.; Ozemek, C.; Ross, R. Cardiorespiratory Fitness and Cardiovascular Disease—The Past, Present, and Future. Prog. Cardiovasc. Dis. 2019, 62, 86–93. [Google Scholar] [CrossRef]
- Nawarycz, L.O.; Krzyżaniak, A.; Stawińska-Witoszyńska, B.; Krzywińska-Wiewiorowska, M.; Szilagyi-Pągowska, I.; Kowalska, M.; Krzych, L.; Nawarycz, T. Percentile Distributions of Waist Circumference for 7–19-Year-Old Polish Children and Adolescents. Obes. Rev. 2010, 11, 281–288. [Google Scholar] [CrossRef]
- Song, P.; Zhang, Y.; Yu, J.; Zha, M.; Zhu, Y.; Rahimi, K.; Rudan, I. Global Prevalence of Hypertension in Children: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2019, 173, 1154. [Google Scholar] [CrossRef] [PubMed]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M.; et al. Cardiorespiratory Fitness in Youth: An Important Marker of Health: A Scientific Statement from the American Heart Association. Circulation 2020, 142, e101–e118. [Google Scholar] [CrossRef] [PubMed]
- Franklin, B.A.; Eijsvogels, T.M.H.; Pandey, A.; Quindry, J.; Toth, P.P. Physical Activity, Cardiorespiratory Fitness, and Cardiovascular Health: A Clinical Practice Statement of the ASPC Part I: Bioenergetics, Contemporary Physical Activity Recommendations, Benefits, Risks, Extreme Exercise Regimens, Potential Maladaptations. Am. J. Prev. Cardiol. 2022, 12, 100424. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Myers, J. Cardiorespiratory Fitness and Its Place in Medicine. Rev. Cardiovasc. Med. 2023, 24, 14. [Google Scholar] [CrossRef]
- Black, N.E.; Vehrs, P.R.; Fellingham, G.W.; George, J.D.; Hager, R. Prediction of VO2max in Children and Adolescents Using Exercise Testing and Physical Activity Questionnaire Data. Res. Q. Exerc. Sport 2016, 87, 89–100. [Google Scholar] [CrossRef]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.-P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef]
- Nevill, A.M.; De Menezes-Junior, F.J.; De Jesus, Í.C.; De Fatima Aguiar Lopes, M.; Corazza, P.R.P.; Tadiotto, M.C.; Mota, J.; Leite, N. Predicting Cardiorespiratory Fitness Using the 20-m Shuttle Run Test: New Insights Using Nonlinear Allometry. Med. Sci. Sports Exerc. 2021, 53, 1624–1629. [Google Scholar] [CrossRef]
- Silva, D.A.S.; Lang, J.J.; Barnes, J.D.; Tomkinson, G.R.; Tremblay, M.S. Cardiorespiratory Fitness in Children: Evidence for Criterion-Referenced Cut-Points. PLoS ONE 2018, 13, e0201048. [Google Scholar] [CrossRef]
- Lang, J.J.; Belanger, K.; Poitras, V.; Janssen, I.; Tomkinson, G.R.; Tremblay, M.S. Systematic Review of the Relationship between 20m Shuttle Run Performance and Health Indicators among Children and Youth. J. Sci. Med. Sport 2018, 21, 383–397. [Google Scholar] [CrossRef]
- Cristi-Montero, C.; Courel-Ibáñez, J.; Ortega, F.B.; Castro-Piñero, J.; Santaliestra-Pasias, A.; Polito, A.; Vanhelst, J.; Marcos, A.; Moreno, L.M.; Ruiz, J.R.; et al. Mediation Role of Cardiorespiratory Fitness on the Association between Fatness and Cardiometabolic Risk in European Adolescents: The HELENA Study. J. Sport Health Sci. 2021, 10, 360–367. [Google Scholar] [CrossRef]
- Peterman, J.E.; Whaley, M.H.; Harber, M.P.; Fleenor, B.S.; Imboden, M.T.; Myers, J.; Arena, R.; Kaminsky, L.A. Comparison of Non-Exercise Cardiorespiratory Fitness Prediction Equations in Apparently Healthy Adults. Eur. J. Prev. Cardiol. 2019, 28, 142–148. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Chen, S.; Lavie, C.J.; Zhang, J.; Sui, X. An Overview of Non-Exercise Estimated Cardiorespiratory Fitness: Estimation Equations, Cross-Validation and Application. J. Sci. Sport Exerc. 2019, 1, 38–53. [Google Scholar] [CrossRef]
- Przednowek, K.; Barabasz, Z.; Zadarko-Domaradzka, M.; Przednowek, K.H.; Nizioł-Babiarz, E.; Huzarski, M.; Sibiga, K.; Dziadek, B.; Zadarko, E. Predictive Modeling of VO2max Based on 20 m Shuttle Run Test for Young Healthy People. Appl. Sci. 2018, 8, 2213. [Google Scholar] [CrossRef]
- Zadarko-Domaradzka, M.; Sobolewski, M.; Nizioł-Babiarz, E.; Barabasz, Z.; Warchoł, K.; Niewczas-Czarna, K.; Zadarko, E. An Investigation of the Utility of Waist Circumference Predicting Cardiorespiratory Fitness in School Children: A Cross-Sectional Study. Int. J. Environ. Res. Public. Health 2023, 20, 851. [Google Scholar] [CrossRef] [PubMed]
- La Grasta Sabolic, L.; Pozgaj Sepec, M.; Valent Moric, B.; Cigrovski Berkovic, M. Association between Cardiorespiratory Fitness Level and Insulin Resistance in Adolescents with Various Obesity Categories. World J. Diabetes 2023, 14, 1126–1136. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Vélez, R.; García-Alonso, Y.; Alonso-Martínez, A.M.; Izquierdo, M. Association of Cardiorespiratory Fitness Levels During Youth with Health Risk Later in Life: A Systematic Review and Meta-Analysis. JAMA Pediatr. 2020, 174, 952–960. [Google Scholar] [CrossRef]
- Mäestu, E.; Harro, J.; Veidebaum, T.; Kurrikoff, T.; Jürimäe, J.; Mäestu, J. Changes in Cardiorespiratory Fitness through Adolescence Predict Metabolic Syndrome in Young Adults. Nutr. Metab. Cardiovasc. Dis. NMCD 2020, 30, 701–708. [Google Scholar] [CrossRef]
- Andreasson, A.; Carlsson, A.C.; Önnerhag, K.; Hagström, H. Predictive Capacity for Mortality and Severe Liver Disease of the Relative Fat Mass Algorithm. Clin. Gastroenterol. Hepatol. 2019, 17, 2619–2620. [Google Scholar] [CrossRef]
- Kobo, O.; Leiba, R.; Avizohar, O.; Karban, A. Relative Fat Mass Is a Better Predictor of Dyslipidemia and Metabolic Syndrome than Body Mass Index. Cardiovasc. Endocrinol. Metab. 2019, 8, 77–81. [Google Scholar] [CrossRef]
- Suthahar, N.; Meems, L.M.G.; Withaar, C.; Gorter, T.M.; Kieneker, L.M.; Gansevoort, R.T.; Bakker, S.J.L.; van Veldhuisen, D.J.; de Boer, R.A. Relative Fat Mass, a New Index of Adiposity, Is Strongly Associated with Incident Heart Failure: Data from PREVEND. Sci. Rep. 2022, 12, 147. [Google Scholar] [CrossRef]
- Kobo, O.; Leiba, R.; Avizohar, O.; Karban, A. Relative Fat Mass (RFM) as Abdominal Obesity Criterion for Metabolic Syndrome. Eur. J. Intern. Med. 2019, 63, e9–e11. [Google Scholar] [CrossRef] [PubMed]
- Machado, M.V.; Policarpo, S.; Coutinho, J.; Carvalhana, S.; Leitão, J.; Carvalho, A.; Silva, A.P.; Velasco, F.; Medeiros, I.; Alves, A.C.; et al. What Is the Role of the New Index Relative Fat Mass (RFM) in the Assessment of Nonalcoholic Fatty Liver Disease (NAFLD)? Obes. Surg. 2020, 30, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, C.R.; Formolo, N.P.S.; Dezanetti, T.; Speretta, G.F.F.; Nunes, E.A. Relative Fat Mass Is a Better Tool to Diagnose High Adiposity When Compared to Body Mass Index in Young Male Adults: A Cross-Section Study. Clin. Nutr. ESPEN 2021, 41, 225–233. [Google Scholar] [CrossRef] [PubMed]
- Lokpo, S.Y.; Ametefe, C.Y.; Osei-Yeboah, J.; Owiredu, W.K.B.A.; Ahenkorah-Fondjo, L.; Agordoh, P.D.; Acheampong, E.; Duedu, K.O.; Adejumo, E.N.; Appiah, M.; et al. Performance of Body Adiposity Index and Relative Fat Mass in Predicting Bioelectric Impedance Analysis-Derived Body Fat Percentage: A Cross-Sectional Study among Patients with Type 2 Diabetes in the Ho Municipality, Ghana. BioMed Res. Int. 2023, 2023, 1500905. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Zhong, Y.; Ge, W.; Lv, H.; Ding, Z.; Han, D.; Hai, B.; Shen, H.; Yin, J.; Gu, A.; et al. Comparisons of Tri-Ponderal Mass Index and Body Mass Index in Discriminating Hypertension at Three Separate Visits in Adolescents: A Retrospective Cohort Study. Front. Nutr. 2022, 9, 1028861. [Google Scholar] [CrossRef] [PubMed]
- Caiano, L.M.; Costanzo, S.; Panzera, T.; Di Castelnuovo, A.; de Gaetano, G.; Donati, M.B.; Ageno, W.; Iacoviello, L.; Moli-Sani Study Investigators. Association between Body Mass Index, Waist Circumference, and Relative Fat Mass with the Risk of First Unprovoked Venous Thromboembolism. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 3122–3130. [Google Scholar] [CrossRef]
- Ministerstwo Zdrowia. Rozporządzenie Ministra Zdrowia z Dnia 24 Września 2013 r. w Sprawie Świadczeń Gwarantowanych z Zakresu Podstawowej Opieki Zdrowotnej (Dz. U. z 2021 r. poz. 540); Ministerstwo Zdrowia: Województwo Mazowieckie, Poland, 2021. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20210000540/O/D20210540.pdf (accessed on 24 August 2023).
- WHO. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 24 August 2023).
- Aubert, S.; Barnes, J.D.; Aguilar-Farias, N.; Cardon, G.; Chang, C.-K.; Delisle Nyström, C.; Demetriou, Y.; Edwards, L.; Emeljanovas, A.; Gába, A.; et al. Report Card Grades on the Physical Activity of Children and Youth Comparing 30 Very High Human Development Index Countries. J. Phys. Act. Health 2018, 15, S298–S314. [Google Scholar] [CrossRef]
| Measures and Indices | Sex | N = 190 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 10–11 Years Old | 12–13 Years Old | 14–15 Years Old | |||||||||||
| N = 68 | N = 62 | N = 60 | |||||||||||
| Mean | Sd | Min | Max | Mean | Sd | Min | Max | Mean | Sd | Min | Max | ||
| BH (cm) | f | 152.5 | 8.0 | 134.0 | 165.0 | 160.5 | 6.4 | 149.0 | 173.5 | 162.3 | 5.6 | 149.0 | 172.5 |
| m | 148.2 | 7.6 | 131.0 | 168.0 | 163.2 | 10.1 | 148.3 | 180.0 | 172.9 | 7.6 | 160.4 | 190.4 | |
| BW (kg) | f | 47.9 | 11.1 | 31.4 | 72.9 | 54.2 | 8.3 | 39.4 | 70.5 | 53.9 | 11.2 | 39.6 | 93.6 |
| m | 46.2 | 12.1 | 24.2 | 67.9 | 53.1 | 14.0 | 34.2 | 84.9 | 60.3 | 11.7 | 41.2 | 88.2 | |
| HC (cm) | f | 86.0 | 8.6 | 72.5 | 100.5 | 91.6 | 6.2 | 80.0 | 103.5 | 92.2 | 9.8 | 79.5 | 124.5 |
| m | 83.2 | 10.9 | 65.0 | 102.5 | 86.0 | 9.6 | 71.5 | 108.0 | 90.4 | 7.6 | 79.0 | 104.0 | |
| WC (cm) | f | 67.3 | 8.8 | 54.5 | 87.5 | 68.1 | 6.9 | 54.5 | 80.0 | 66.1 | 6.9 | 56.0 | 86.0 |
| m | 70.1 | 11.0 | 55.0 | 90.0 | 69.5 | 7.6 | 58.0 | 89.0 | 71.2 | 7.3 | 61.0 | 90.0 | |
| BF (%) | f | 23.6 | 7.5 | 8.0 | 37.3 | 26.2 | 6.1 | 9.0 | 40.2 | 21.8 | 7.5 | 7.1 | 37.1 |
| m | 19.0 | 9.8 | 5.1 | 35.4 | 12.0 | 6.6 | 3.6 | 29.1 | 11.0 | 7.2 | 1.4 | 29.1 | |
| BMI | f | 20.5 | 3.9 | 15.0 | 30.3 | 21.0 | 3.0 | 16.0 | 27.2 | 20.5 | 4.1 | 15.5 | 32.0 |
| m | 20.9 | 4.7 | 14.1 | 29.6 | 19.7 | 3.7 | 15.2 | 29.0 | 20.1 | 3.5 | 14.6 | 27.6 | |
| WHR | f | 0.78 | 0.06 | 0.68 | 0.96 | 0.74 | 0.05 | 0.63 | 0.84 | 0.72 | 0.03 | 0.66 | 0.78 |
| m | 0.84 | 0.05 | 0.72 | 0.94 | 0.81 | 0.05 | 0.74 | 0.93 | 0.79 | 0.05 | 0.72 | 0.90 | |
| WHtR | f | 0.44 | 0.06 | 0.37 | 0.59 | 0.42 | 0.04 | 0.35 | 0.51 | 0.41 | 0.05 | 0.34 | 0.50 |
| m | 0.47 | 0.07 | 0.38 | 0.60 | 0.43 | 0.04 | 0.37 | 0.58 | 0.41 | 0.04 | 0.36 | 0.55 | |
| TMI | f | 13.4 | 2.5 | 9.9 | 19.6 | 13.1 | 2.0 | 10.1 | 17.5 | 12.6 | 2.6 | 9.3 | 18.7 |
| m | 14.1 | 3.0 | 10.3 | 20.4 | 12.1 | 2.1 | 9.8 | 18.8 | 11.7 | 2.1 | 8.7 | 16.7 | |
| Waist–BMI ratio | f | 3.33 | 0.27 | 2.88 | 3.79 | 3.26 | 0.25 | 2.85 | 3.78 | 3.29 | 0.32 | 2.69 | 3.99 |
| m | 3.41 | 0.28 | 2.89 | 3.94 | 3.58 | 0.33 | 3.05 | 4.35 | 3.58 | 0.31 | 3.04 | 4.18 | |
| RFMp | f | 28.4 | 6.0 | 19.0 | 41.9 | 26.7 | 5.2 | 16.8 | 36.2 | 24.5 | 5.8 | 14.4 | 35.2 |
| m | 26.5 | 6.6 | 16.3 | 37.5 | 21.9 | 4.8 | 14.1 | 35.9 | 20.1 | 5.1 | 12.4 | 33.8 | |
| HRpeak values (bpm) | f | 197.4 | 6.9 | 180.0 | 213.0 | 195.7 | 9.5 | 176.0 | 213.0 | 194.5 | 9.2 | 177.0 | 216.0 |
| m | 200.6 | 5.6 | 190.0 | 210.0 | 200.4 | 8.3 | 185.0 | 219.0 | 198.0 | 7.0 | 183.0 | 212.0 | |
| 20 mSRT (laps) | f | 32.8 | 11.4 | 16.0 | 66.0 | 37.8 | 14.0 | 12.0 | 78.0 | 46.7 | 14.8 | 24.0 | 82.0 |
| m | 42.3 | 19.7 | 18.0 | 92.0 | 60.2 | 19.4 | 22.0 | 94.0 | 67.7 | 21.7 | 23.0 | 112.0 | |
| Models | Factors (Independent) | Regression Models—Statistics | ||
|---|---|---|---|---|
| R2 | F | p | ||
| 1 | Age, sex, WHR | 39.2% | 41.6 | <0.0001 |
| 2 | Age, sex, BMI | 45.8% | 54.2 | <0.0001 |
| 3 | Age, sex, WHtR | 50.0% | 64.1 | <0.0001 |
| 4 | Age, sex, TMI | 49.1% | 59.7 | <0.0001 |
| 5 | Age, sex, waist–BMI ratio | 40.5% | 42.1 | <0.0001 |
| 6 | Age, sex, RFMp | 51.1% | 65.2 | <0.0001 |
| 7 | Age, sex, WC | 47.1% | 57.2 | <0.0001 |
| 8 | Age, sex, %BF | 50.3% | 64.9 | <0.0001 |
| Independent Variables | Laps R2 = 51.1% F = 64.8 p < 0.0001 | ||
|---|---|---|---|
| B (95% CI) | p | β | |
| Intercept | 45.875 (26.024; 65.726) | <0.0001 | × |
| Sex (m vs. f) | 12.286 (7.941; 16.630) | <0.0001 | 0.30 |
| Age (years) | 2.945 (1.776; 4.114) | <0.0001 | 0.27 |
| RFMp | −1.423 (−1.787; −1.059) | <0.0001 | −0.44 |
| Independent Variables | Laps—Girls R2 = 32.9% F = 13.0 p < 0.0001 | ||
|---|---|---|---|
| B (95% CI) | p | β | |
| Intercept | 27.54 (−26.4; 81.47) | 0.3137 | × |
| WHR (change of 0.01) | 1.11 (0.08; 2.15) | 0.0349 | 0.42 |
| Waist–BMI ratio (change of 0.1) | −1.61 (−3.21; −0.01) | 0.0489 | −0.31 |
| RFMp (change of 1) | −2.04 (−3.09; −0.99) | 0.0002 | −0.83 |
| Age (years) | 2.81 (1.34; 4.27) | 0.0003 | 0.35 |
| Independent Variables | Laps—Boys R2 = 52.9% F = 42.8 p < 0.0001 | ||
|---|---|---|---|
| B (95% CI) | p | β | |
| Intercept | 59.62 (24.27; 94.98) | 0.0012 | × |
| RFMp (change of 1) | −1.99 (−2.64; −1.35) | <0.0001 | −0.55 |
| Age (years) | 3.39 (1.33; 5.46) | 0.0016 | 0.29 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zadarko-Domaradzka, M.; Sobolewski, M.; Zadarko, E. Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children—A Single-Center Cross-Sectional Study. J. Clin. Med. 2023, 12, 6226. https://doi.org/10.3390/jcm12196226
Zadarko-Domaradzka M, Sobolewski M, Zadarko E. Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children—A Single-Center Cross-Sectional Study. Journal of Clinical Medicine. 2023; 12(19):6226. https://doi.org/10.3390/jcm12196226
Chicago/Turabian StyleZadarko-Domaradzka, Maria, Marek Sobolewski, and Emilian Zadarko. 2023. "Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children—A Single-Center Cross-Sectional Study" Journal of Clinical Medicine 12, no. 19: 6226. https://doi.org/10.3390/jcm12196226
APA StyleZadarko-Domaradzka, M., Sobolewski, M., & Zadarko, E. (2023). Comparison of Several Anthropometric Indices Related to Body Fat in Predicting Cardiorespiratory Fitness in School-Aged Children—A Single-Center Cross-Sectional Study. Journal of Clinical Medicine, 12(19), 6226. https://doi.org/10.3390/jcm12196226





