The Validation of Two-Dimensional and Three-Dimensional Radiographic Measurements of Host Bone Coverage in Total Hip Arthroplasty for Hip Dysplasia: A Comparison with Intra-Operative Measurements
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort Enrollment
2.2. Surgical Procedure and Prosthesis
2.3. Clinical Outcomes
2.4. Cup Position and Fixation
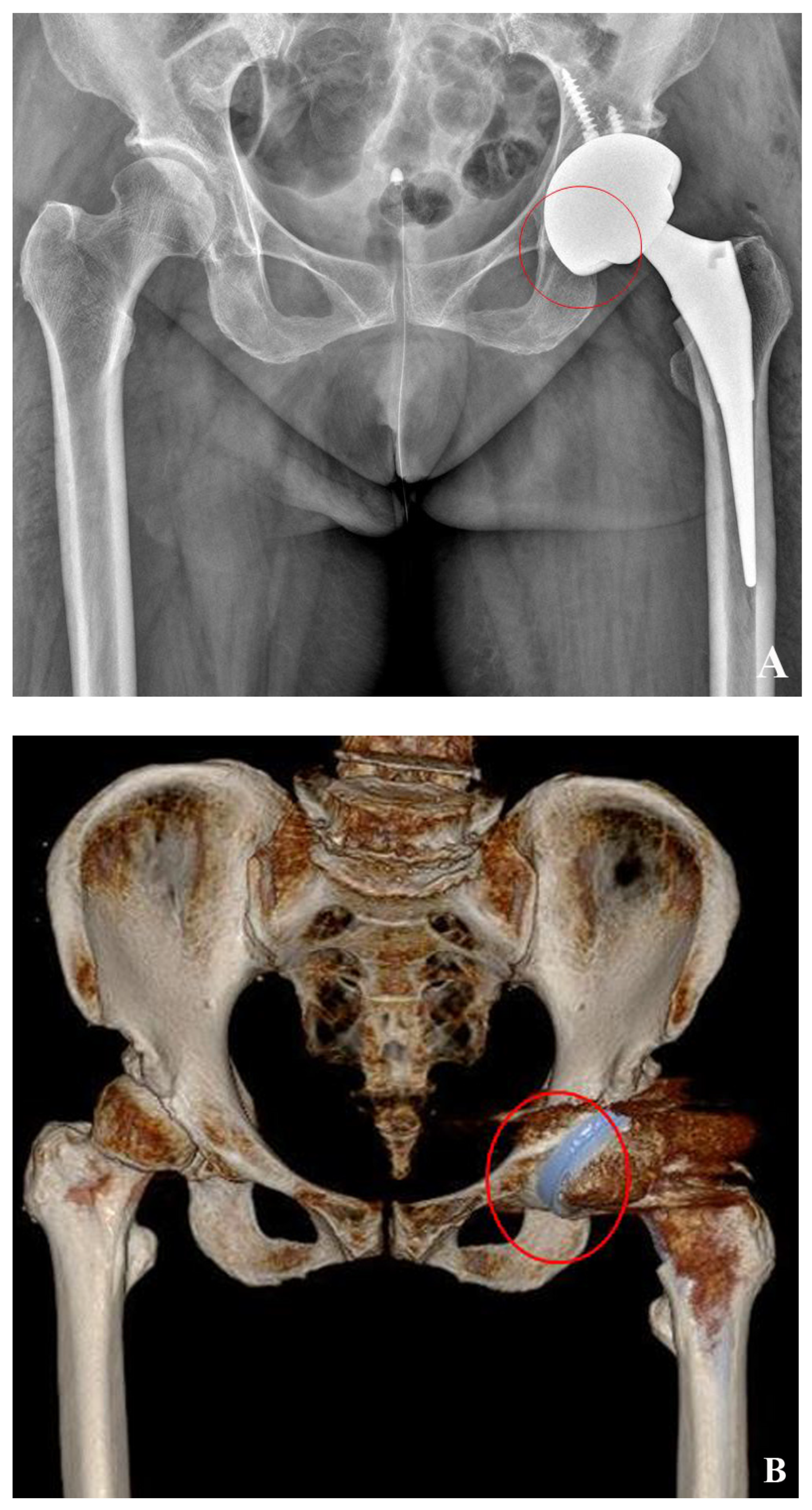
2.5. 2D-Based Measurement of Host Bone Coverage from Plain Radiographs of the Pelvis
2.6. 3D-Based Measurement of Host Bone Coverage from CT Scans
2.7. Measurement of Intra-Operative Host Bone Coverage
2.8. Statistical Analyses
3. Results
3.1. Clinical Outcomes
3.2. Cup Position and Fixation
3.3. Correlation of Three Methods of Host Bone Coverage
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lim, Y.W.; Kim, M.J.; Lee, Y.S.; Kim, Y.S. Total Hip Arthroplasty in Patient with the Sequelae of Legg-Calve-Perthes Disease. Hip Pelvis 2014, 26, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.N.; Liu, J.L.; Jia, X.L.; Zhou, Q.; Yang, L.; Zhang, Y. Midterm Results of Total Hip Arthroplasty in Patients with High Hip Dislocation after Suppurative Hip Arthritis. J. Arthroplast. 2019, 34, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Greber, E.M.; Pelt, C.E.; Gililland, J.M.; Anderson, M.B.; Erickson, J.A.; Peters, C.L. Challenges in Total Hip Arthroplasty in the Setting of Developmental Dysplasia of the Hip. J. Arthroplast. 2017, 32, S38–S44. [Google Scholar] [CrossRef] [PubMed]
- Vanlommel, J.; Vanlommel, L.; Molenaers, B.; Simon, J.P. Hybrid total hip arthroplasty for multiple epiphyseal dysplasia. Orthop. Traumatol. Surg. Res. 2018, 104, 301–305. [Google Scholar] [CrossRef]
- Tateda, K.; Nagoya, S.; Suzuki, D.; Kosukegawa, I.; Yamashita, T. Acetabular Morphology in Patients with Developmental Dysplasia of the Hip with High Dislocation. Hip Pelvis 2021, 33, 25–32. [Google Scholar] [CrossRef]
- Sakellariou, V.I.; Christodoulou, M.; Sasalos, G.; Babis, G.C. Reconstruction of the acetabulum in developmental dysplasia of the hip in total hip replacement. Arch. Bone Jt. Surg. 2014, 2, 130. [Google Scholar]
- Moldovan, F.; Moldovan, L.; Bataga, T. A Comprehensive Research on the Prevalence and Evolution Trend of Orthopedic Surgeries in Romania. Healthcare 2023, 11, 1866. [Google Scholar] [CrossRef]
- Rogers, B.A.; Garbedian, S.; Kuchinad, R.A.; Backstein, D.; Safir, O.; Gross, A.E. Total hip arthroplasty for adult hip dysplasia. J. Bone Jt. Surg. Am. 2012, 94, 1809–1821. [Google Scholar] [CrossRef]
- Hartig-Andreasen, C.; Stilling, M.; Soballe, K.; Thillemann, T.M.; Troelsen, A. Is cup positioning challenged in hips previously treated with periacetabular osteotomy? J. Arthroplast. 2014, 29, 763–768. [Google Scholar] [CrossRef]
- Patil, S.; Bergula, A.; Chen, P.C.; Colwell, C.W.J.; D’Lima, D.D. Polyethylene Wear and Acetabular Component Orientation. J. Bone Jt. Surg. 2003, 85, 56–63. [Google Scholar] [CrossRef]
- Korduba, L.A.; Essner, A.; Pivec, R.; Lancin, P.; Mont, M.A.; Wang, A.; Delanois, R.E. Effect of acetabular cup abduction angle on wear of ultrahigh-molecular-weight polyethylene in hip simulator testing. Am. J. Orthop. 2014, 43, 466–471. [Google Scholar] [PubMed]
- Kaku, N.; Tagomori, H.; Tsumura, H. Comparison of Cup Setting Angle Accuracy between Computed Tomography-Based and Computed Tomography-Free Navigation in the Same Patients with Crowe’s Classification I or II Hip Dysplasia. Clin. Orthop. Surg. 2021, 13, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; Stryker, L.S.; Trousdale, R.T.; Berry, D.J.; Cabanela, M.E. Uncemented acetabular components with femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip: A concise follow-up report at a mean of twenty years. J. Bone Jt. Surg. Am. 2014, 96, 1878–1882. [Google Scholar] [CrossRef]
- Ozden, V.E.; Dikmen, G.; Beksac, B.; Tozun, I.R. Long-term retrospective study on the placement of the cementless acetabular cup and clinical outcomes in patients undergoing femoral head autografting for hip dysplasia and total hip arthroplasty. J. Orthop. Sci. 2018, 23, 525–531. [Google Scholar] [CrossRef]
- Dorr, L.D.; Tawakkol, S.; Moorthy, M.; Long, W.; Wan, Z. Medial Protrusio Technique for Placement of a Porous-Coated, Hemispherical Acetabular Component without Cement in a Total Hip Arthroplasty in Patients Who Have Acetabular Dysplasia. J. Bone Jt. Surg. 1999, 81, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Mou, P.; Liao, K.; Chen, H.L.; Yang, J. Controlled fracture of the medial wall versus structural autograft with bulk femoral head to increase cup coverage by host bone for total hip arthroplasty in osteoarthritis secondary to developmental dysplasia of the hip: A retrospective cohort study. J. Orthop. Surg. Res. 2020, 15, 561. [Google Scholar] [CrossRef] [PubMed]
- Stirling, P.; Viamont-Guerra, M.-R.; Strom, L.; Chen, A.F.; Saffarini, M.; Nover, L.; Laude, F. Does cup position at the high hip center or anatomic hip center in THA for developmental dysplasia of the hip result in better Harris hip scores and revision incidence? A systematic review. Clin. Orthop. Relat. Res. 2021, 479, 1119. [Google Scholar] [CrossRef] [PubMed]
- Mozafari, J.K.; Pisoudeh, K.; Gharanizadeh, K.; Ghazavi, M.; Abolghasemian, M. Impaction Grafting Is Sufficient to Address Acetabular Deficiency During Total Hip Arthroplasty of Most Dysplastic Hips with over 30% Bone Defect. J. Arthroplast. 2022, 37, 1302–1307. [Google Scholar] [CrossRef] [PubMed]
- Volpin, A.; Konan, S.; Biz, C.; Tansey, R.; Haddad, F. Reconstruction of failed acetabular component in the presence of severe acetabular bone loss: A systematic review. Musculoskelet. Surg. 2019, 103, 1–13. [Google Scholar] [CrossRef]
- Ueno, T.; Kabata, T.; Kajino, Y.; Ohmori, T.; Yoshitani, J.; Tsuchiya, H. Three-Dimensional Host Bone Coverage Required in Total Hip Arthroplasty for Developmental Dysplasia of the Hip and Its Relationship with 2-Dimensional Coverage. J. Arthroplast. 2019, 34, 93–101. [Google Scholar] [CrossRef]
- Wang, L.; Thoreson, A.R.; Trousdale, R.T.; Morrey, B.F.; Dai, K.; An, K.N. Two-dimensional and three-dimensional cup coverage in total hip arthroplasty with developmental dysplasia of the hip. J. Biomech. 2013, 46, 1746–1751. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Qu, X.; Li, H.; Mao, Y.; Yu, D.; Zhu, Z. Three-Dimensional Host Bone Coverage in Total Hip Arthroplasty for Crowe Types II and III Developmental Dysplasia of the Hip. J. Arthroplast. 2017, 32, 1374–1380. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kadowaki, T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin. Orthop. Relat. Res. 2010, 468, 1611–1620. [Google Scholar] [CrossRef] [PubMed]
- Fujii, M.; Nakashima, Y.; Nakamura, T.; Ito, Y.; Hara, T. Minimum lateral bone coverage required for securing fixation of cementless acetabular components in hip dysplasia. BioMed Res. Int. 2017, 2017, 4937151. [Google Scholar] [CrossRef]
- Goyal, T.; Paul, S.; Choudhury, A.K.; Gupta, T. Assessment of Acetabular Component Anteversion after Total Hip Arthroplasty: Comparison of Anteroposterior and Cross-Table Lateral Radiographs with Computed Tomography Scans. Clin. Orthop. Surg. 2021, 13, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Nieuwenhuijse, M.J.; Valstar, E.R.; Kaptein, B.L.; Nelissen, R.G. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups: Results from ten years of follow-up with Roentgen stereophotogrammetric analysis (RSA). J. Bone Jt. Surg. 2012, 94, 874–880. [Google Scholar] [CrossRef]
- Windsor, E.N.; Sharma, A.K.; Premkumar, A.; Gkiatas, I.; Sculco, P.K.; Vigdorchik, J.M. The Use of Technology to Achieve the Functional Acetabular Safe Zone in Total Hip Arthroplasty. JBJS Rev. 2022, 10, e21.00070. [Google Scholar] [CrossRef]
- Nie, Y.; Wang, H.; Huang, Z.; Shen, B.; Kraus, V.B.; Zhou, Z. Radiographic Underestimation of In Vivo Cup Coverage Provided by Total Hip Arthroplasty for Dysplasia. Orthopedics 2018, 41, e46–e51. [Google Scholar] [CrossRef] [PubMed]
- Tabata, T.; Kaku, N.; Hara, K.; Tsumura, H. Initial stability of cementless acetabular cups: Press-fit and screw fixation interaction—An in vitro biomechanical study. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 497–502. [Google Scholar] [CrossRef]
- Takao, M.; Nakamura, N.; Ohzono, K.; Sakai, T.; Nishii, T.; Sugano, N. The results of a press-fit-only technique for acetabular fixation in hip dysplasia. J. Arthroplast. 2011, 26, 562–568. [Google Scholar] [CrossRef]
- Miura, T.; Kijima, H.; Kimura, R.; Watanabe, J.; Okazaki, Y.; Miyakoshi, N. Efficacy and Safety of Acetabular Cup without Screw Fixation in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. Medicina 2022, 58, 1058. [Google Scholar] [CrossRef] [PubMed]
- Polus, J.S.; Vasarhelyi, E.M.; Lanting, B.A.; Teeter, M.G. Acetabular cup fixation with and without screws following primary total hip arthroplasty: Migration evaluated by radiostereometric analysis. HIP Int. 2023. [Google Scholar] [CrossRef] [PubMed]
- Pijls, B.G.; Nieuwenhuijse, M.J.; Fiocco, M.; Plevier, J.W.; Middeldorp, S.; Nelissen, R.G.; Valstar, E.R. Early proximal migration of cups is associated with late revision in THA: A systematic review and meta-analysis of 26 RSA studies and 49 survival studies. Acta Orthop. 2012, 83, 583–591. [Google Scholar] [CrossRef] [PubMed]







| Demographics | |
|---|---|
| Age at surgery (years) | 63.0 ± 12.4 (range: 30–81) |
| Follow up period (months) | 54.9 ± 1.4 (range: 17–72) |
| Height (cm) | 152.5 ± 8.1 |
| Weight (kg) | 59.3 ± 12.9 |
| Pre-op radiologic parameters | |
| Lateral CEA | 1.96 ± 16.7 (range: −48.4–24.0) |
| Tonnis angle | 29.43 ± 6.4 (range: 14.5–40.5) |
| Crowe type | |
| Dysplastic | 16 (51.6%) |
| Low dislocation | 14 (45.2%) |
| High dislocation | 1 (3.2%) |
| Prosthesis data | |
| Acetabular cup size | (52/54/56/58/60/62/68) 1/2/7/13/4/3/1 |
| Supplementary screw (#2/#3) | 16/15 |
| Liner (neutral/elevated) | 18/13 |
| Head (32 mm/36 mm) | 8/23 |
| Fixation Grade | Definition | |
|---|---|---|
| Stable bone ingrowth | IA | No radiolucent line |
| IB | Radiolucent line in 1 zone | |
| IC | Radiolucent line in 2 zones | |
| Stable fibrous fixation | II | Complete radiolucent line, width < 2 mm |
| Unstable fibrous fixation | III | Complete radiolucent line, width ≥ 2 mm, or Cup migration |
| Parameters | Outcomes |
|---|---|
| Clinical outcomes | |
| Pre-op HHS | 60.84 ± 14.2 (range 25–80) |
| Post-op HHS | 93.13 ± 4.6 (range 82–99) |
| Recurrent dislocation | 0 |
| Periprosthetic joint infection | 0 |
| Radiologic outcomes | |
| Cup inclination (°) | 35.3° ± 7.3 (range 25.2–47.6) |
| Cup anteversion (°) | 23.8° ± 12.8 (range −14.1–46.1) |
| Modified DeLee and Chanley classification of fixation | |
| I (A/B/C) | 27/3/1 |
| II | 0 |
| III | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yon, C.-J.; Lee, K.-J.; Choi, B.-C.; Suh, H.-S.; Min, B.-W. The Validation of Two-Dimensional and Three-Dimensional Radiographic Measurements of Host Bone Coverage in Total Hip Arthroplasty for Hip Dysplasia: A Comparison with Intra-Operative Measurements. J. Clin. Med. 2023, 12, 6227. https://doi.org/10.3390/jcm12196227
Yon C-J, Lee K-J, Choi B-C, Suh H-S, Min B-W. The Validation of Two-Dimensional and Three-Dimensional Radiographic Measurements of Host Bone Coverage in Total Hip Arthroplasty for Hip Dysplasia: A Comparison with Intra-Operative Measurements. Journal of Clinical Medicine. 2023; 12(19):6227. https://doi.org/10.3390/jcm12196227
Chicago/Turabian StyleYon, Chang-Jin, Kyung-Jae Lee, Byung-Chan Choi, Ho-Sung Suh, and Byung-Woo Min. 2023. "The Validation of Two-Dimensional and Three-Dimensional Radiographic Measurements of Host Bone Coverage in Total Hip Arthroplasty for Hip Dysplasia: A Comparison with Intra-Operative Measurements" Journal of Clinical Medicine 12, no. 19: 6227. https://doi.org/10.3390/jcm12196227
APA StyleYon, C.-J., Lee, K.-J., Choi, B.-C., Suh, H.-S., & Min, B.-W. (2023). The Validation of Two-Dimensional and Three-Dimensional Radiographic Measurements of Host Bone Coverage in Total Hip Arthroplasty for Hip Dysplasia: A Comparison with Intra-Operative Measurements. Journal of Clinical Medicine, 12(19), 6227. https://doi.org/10.3390/jcm12196227






