Stress and Depressive and Anxiety Symptoms in the General Population and in SARS-CoV-2-Infected Patients—Findings from a Population-Based Three-Wave Study
Abstract
:1. Introduction
1.1. Depressive and Anxiety Symptoms in the COVID-19 Pandemic
1.2. The Role of Stress as a Predictor of Depressive Symptoms in the COVID-19 Pandemic
1.3. Depressive Symptoms among SARS-CoV-2-Infected versus General Population
2. Methods
2.1. Data Analysis
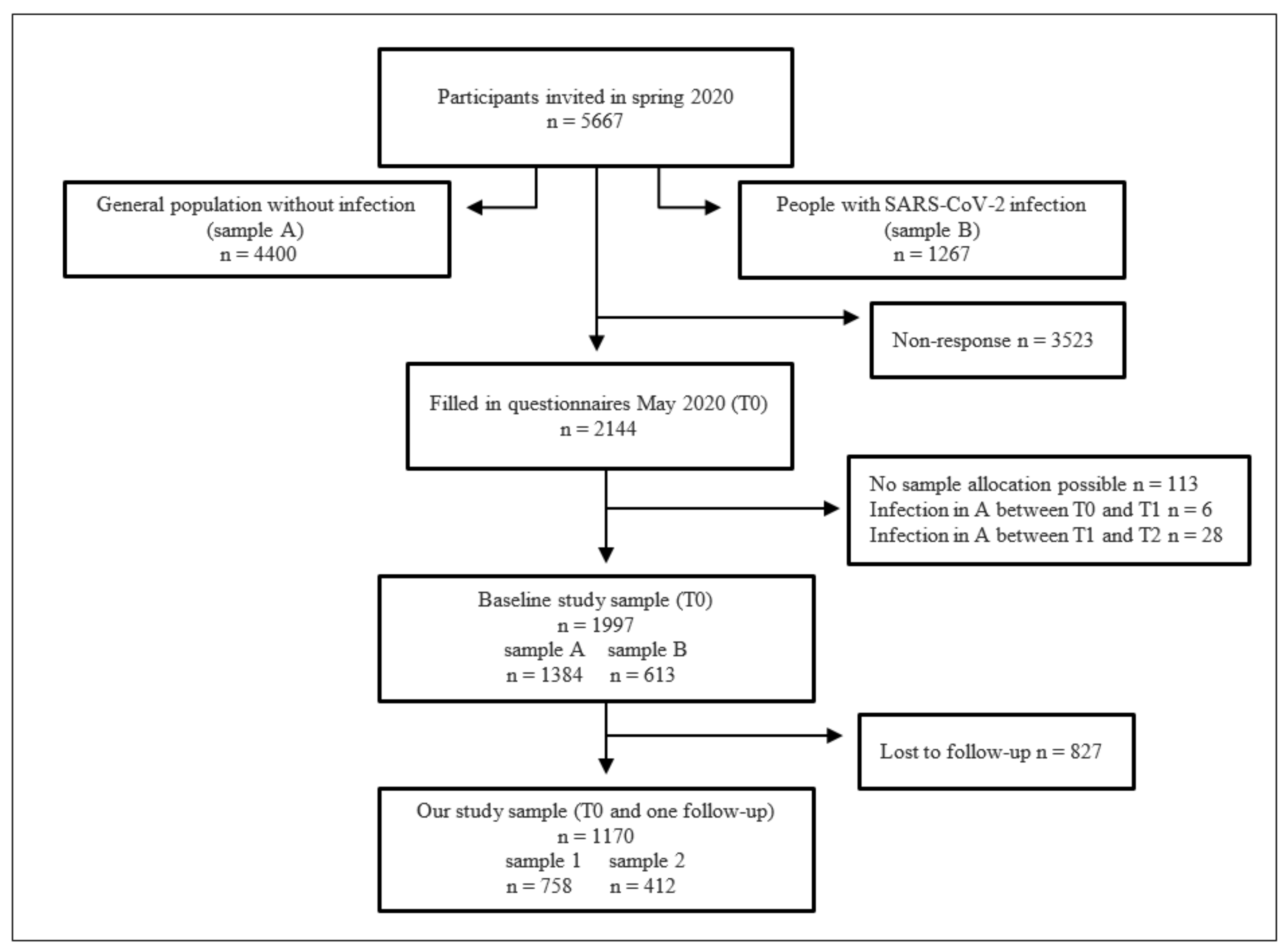
2.2. Sample and Procedure
2.3. Measures
3. Results
3.1. Sample Characteristics at Baseline
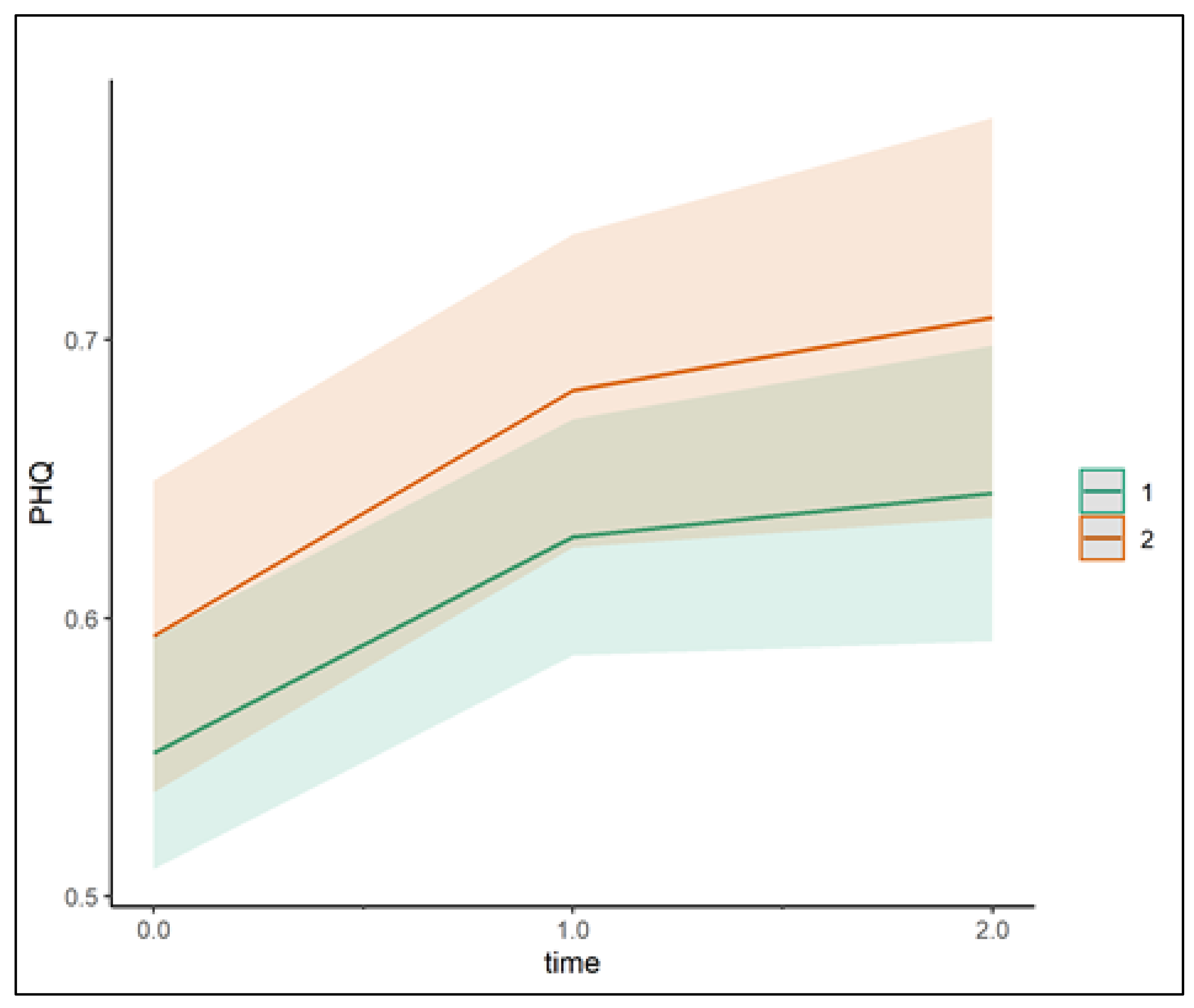
3.2. Prediction of Depressive and Anxiety Symptoms over Time (Model 1)
3.3. Prediction of Depressive and Anxiety Symptoms over Time When Integrating General Stress as a Predictor (Model 2)
3.4. Prediction of Depressive and Anxiety Symptoms over Time, with Detailed Analysis of the Four Subcategories of Stress (Model 3)
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Danese, A.; Smith, P. Debate: Recognising and responding to the mental health needs of young people in the era of COVID-19. Child Adolesc. Ment. Heal. 2020, 25, 169–170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020, 87, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Huang, E.; Zuo, Q.K. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: A meta-analysis. Ann. N. Y. Acad. Sci. 2020, 1486, 90–111. [Google Scholar] [CrossRef] [PubMed]
- Robinson, E.; Sutin, A.R.; Daly, M.; Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 2022, 296, 567–576. [Google Scholar] [CrossRef]
- Santomauro, D.F.; Herrera, A.M.M.; Shadid, J.; Zheng, P.; Ashbaugh, C.; Pigott, D.M.; Abbafati, C.; Adolph, C.; Amlag, J.O.; Aravkin, A.Y.; et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Bendau, A.; Kunas, S.L.; Wyka, S.; Petzold, M.B.; Plag, J.; Asselmann, E.; Ströhle, A. Longitudinal changes of anxiety and depressive symptoms during the COVID-19 pandemic in Germany: The role of pre-existing anxiety, depressive, and other mental disorders. J. Anxiety Disord. 2021, 79, 102377. [Google Scholar] [CrossRef]
- Giel, K.E.; Martus, P.; Paul, G.; Jürgensen, J.S.; Löwe, B.; Higuita, L.M.S.; Dörsam, A.F.; Stuber, F.; Ehehalt, S.; Zipfel, S.; et al. Longitudinal development of depression and anxiety during COVID-19 pandemic in Germany: Findings from a population-based probability sample survey. Front. Psychiatry 2022, 13, 1000722. [Google Scholar] [CrossRef]
- Ettman, C.K.; Cohen, G.H.; Abdalla, S.M.; Sampson, L.; Trinquart, L.; Castrucci, B.C.; Bork, R.H.; Clark, M.A.; Wilson, I.; Vivier, P.M.; et al. Persistent depressive symptoms during COVID-19: A national, population-representative, longitudinal study of U.S. adults. Lancet Reg. Health Am. 2022, 5, 100091. [Google Scholar] [CrossRef]
- Sachs, J.D.; Karim, S.S.A.; Aknin, L.; Allen, J.; Brosbøl, K.; Colombo, F.; Barron, G.C.; Espinosa, M.F.; Gaspar, V.; Gaviria, A.; et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. Lancet 2022, 400, 1224–1280. [Google Scholar] [CrossRef]
- Mækelæ, M.J.; Reggev, N.; Defelipe, R.P.; Dutra, N.; Tamayo, R.M.; Klevjer, K.; Pfuhl, G. Identifying Resilience Factors of Distress and Paranoia During the COVID-19 Outbreak in Five Countries. Front. Psychol. 2021, 12, 661149. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J. Pers. Soc. Psychol. 1985, 48, 150–170. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Transactional theory and research on emotions and coping. Eur. J. Pers. 1987, 1, 141–169. [Google Scholar] [CrossRef]
- Quittkat, H.L.; Düsing, R.; Holtmann, F.-J.; Buhlmann, U.; Svaldi, J.; Vocks, S. Perceived Impact of Covid-19 Across Different Mental Disorders: A Study on Disorder-Specific Symptoms, Psychosocial Stress and Behavior. Front. Psychol. 2020, 11, 586246. [Google Scholar] [CrossRef]
- Liu, S.; Heinzel, S.; Haucke, M.N.; Heinz, A. Increased Psychological Distress, Loneliness, and Unemployment in the Spread of COVID-19 over 6 Months in Germany. Medicina 2021, 57, 53. [Google Scholar] [CrossRef]
- Wechsler, T.F.; Schmidmeier, M.; Biehl, S.; Gerczuk, J.; Guerrero-Cerda, F.-M.; Mühlberger, A. Individual changes in stress, depression, anxiety, pathological worry, posttraumatic stress, and health anxiety from before to during the COVID-19 pandemic in adults from Southeastern Germany. BMC Psychiatry 2022, 22, 528. [Google Scholar] [CrossRef]
- Jowett, S.D.; Shevlin, M.; Hyland, P.; Karatzias, T. Posttraumatic Stress Disorder and Persistent Somatic Symptoms During the COVID-19 Pandemic: The Role of Sense of Threat. Psychosom. Med. 2020, 83, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Lapin, B.; Katzan, I.L. Health-Related Quality of Life Mildly Affected Following COVID-19: A Retrospective Pre-post Cohort Study with a Propensity Score-Matched Control Group. J. Gen. Intern. Med. 2022, 37, 862–869. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, I.H.; Magnus, P.; Trogstad, L. Excess risk and clusters of symptoms after COVID-19 in a large Norwegian cohort. Eur. J. Epidemiol. 2022, 37, 539–548. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models using lme4. arXiv 2014. [Google Scholar] [CrossRef]
- Little, R.J.A. A Test of Missing Completely at Random for Multivariate Data with Missing Values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Löwe, B. An Ultra-Brief Screening Scale for Anxiety and Depression: The PHQ–4. Psychosomatics 2009, 50, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. Validierung des “Perceived Stress Questionnaire“ (PSQ) an einer deutschen Stichprobe. Diagnostica 2001, 47, 142–152. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. PSQ-Perceived Stress Questionnaire; ZPID (Leibniz Institute for Psychology Information)–Testarchiv: Trier, Germany, 2009. [Google Scholar]
- Cohen, S.; Janicki-Deverts, D.; Miller, G.E. Psychological stress and disease. JAMA 2007, 298, 1685–1687. [Google Scholar] [CrossRef]
- Bardeen, J.R.; Fergus, T.A.; Orcutt, H.K. Experiential avoidance as a moderator of the relationship between anxiety sensitivity and perceived stress. Behav. Ther. 2013, 44, 459–469. [Google Scholar] [CrossRef]
- Li, X.; Lyu, H. Epidemic Risk Perception, Perceived Stress, and Mental Health During COVID-19 Pandemic: A Moderated Mediating Model. Front. Psychol. 2021, 11, 563741. [Google Scholar] [CrossRef]
- Bäuerle, A.; Musche, V.; Schmidt, K.; Schweda, A.; Fink, M.; Weismüller, B.; Kohler, H.; Herrmann, K.; Tewes, M.; Schadendorf, D.; et al. Mental Health Burden of German Cancer Patients before and after the Outbreak of COVID-19: Predictors of Mental Health Impairment. Int. J. Environ. Res. Public Health 2021, 18, 2318. [Google Scholar] [CrossRef]
- Moradian, S.; Teufel, M.; Jahre, L.; Musche, V.; Fink, M.; Dinse, H.; Schweda, A.; Weismüller, B.; Dörrie, N.; Tan, S.; et al. Mental health burden of patients with diabetes before and after the initial outbreak of COVID-19: Predictors of mental health impairment. BMC Public Health 2021, 21, 2068. [Google Scholar] [CrossRef] [PubMed]
- Diexer, S.; Klee, B.; Gottschick, C.; Xu, C.; Broda, A.; Purschke, O.; Binder, M.; Frese, T.; Girndt, M.; Hoell, J.I.; et al. Association between virus variants, vaccination, previous infections, and post-COVID-19 risk. International journal of infectious diseases: IJID: Official publication of the International Society for Infectious Diseases. Adv. Online Publ. 2023, 136, 14–21. [Google Scholar] [CrossRef]
| Sample 1 M (SD) | N | Sample 2 M (SD) | N | |
|---|---|---|---|---|
| Age (T0) | 45.69 (15.97) | 756 | 45.80 (15.66) | 400 |
| Gender (female; T0) | 54.9% | 758 | 51% | 412 |
| Education (T0) | ||||
| No professional qualification | 37 (5.1%) | 758 | 17(4.1%) | 412 |
| Professional qualification | 236 (31.1%) | 758 | 118 (28.6%) | 412 |
| University degree, Bachelor | 91 (12%) | 758 | 44 (10.7%) | 412 |
| University degree, Master/Diploma | 364 (48.5%) | 758 | 217 (54.7%) | 412 |
| Pre-existing disease % (T0) | 38.7% | 293 | 39.1% | 161 |
| PHQ-4 baseline (T0) | 0.56 (0.54) | 758 | 0.59 (0.67) | 411 |
| PHQ-4 follow-up (T1) | 0.62 (0.59) | 758 | 0.69 (0.67) | 412 |
| PHQ-4 follow-up (T2) | 0.63 (0.63) | 465 | 0.65 (0.69) | 233 |
| PSQ baseline (T0) | 32.3 (19.12) | 737 | 32.47 (18.83) | 393 |
| PSQ follow-up (T1) | 36.20 (19.45) | 717 | 38.43 (20.29) | 398 |
| PSQ follow-up (T2) | 36.20 (20.81) | 465 | 37.26 (20.56) | 231 |
| Confidence Intervals Std. Beta | ||||||
|---|---|---|---|---|---|---|
| Model 1 | ||||||
| beta (B) | Std. beta (β) | Std. error | CI lower | CI upper | p | |
| Time | 0.11 | 0.07 | 0.02 | 0.04 | 0.10 | <0.001 |
| Time2 | −0.03 | −0.03 | 0.01 | −0.06 | −0.01 | 0.010 |
| Sample | 0.05 | 0.09 | 0.03 | −0.02 | 0.20 | 0.170 |
| Education | −0.06 | −0.09 | 0.01 | −0.14 | −0.04 | 0.001 |
| Disease | 0.07 | 0.12 | 0.03 | 0.02 | 0.23 | 0.033 |
| Sample × Time | 0.01 | 0.01 | 0.02 | −0.04 | 0.06 | 0.728 |
| Model 2 | ||||||
| beta (B) | Std. beta (β) | Std. error | CI lower | CI upper | p | |
| Time | −0.04 | −0.02 | 0.02 | −0.04 | 0.01 | 0.117 |
| Time2 | 0.01 | 0.01 | 0.01 | −0.01 | 0.04 | 0.207 |
| Sample | 0.02 | 0.03 | 0.02 | −0.03 | 0.10 | 0.319 |
| Education | −0.06 | −0.10 | 0.07 | −0.13 | −0.07 | <0.001 |
| Disease | 0.05 | 0.08 | 0.02 | 0.02 | 0.15 | 0.011 |
| General stress (PSQ) | 0.02 | 0.73 | 0.04 | 0.70 | 0.76 | <0.001 |
| Sample × Time | 0.02 | 0.01 | 0.02 | −0.05 | 0.03 | 0.727 |
| Model 3 | ||||||
| beta (B) | Std. beta (β) | Std. error | CI lower | CI upper | p | |
| Time | −0.03 | −0.00 | 0.02 | −0.03 | 0.02 | 0.239 |
| Time2 | 0.02 | 0.01 | 0.01 | −0.01 | 0.04 | 0.202 |
| Sample | 0.01 | 0.03 | 0.02 | −0.03 | 0.08 | 0.559 |
| Education | −0.03 | −0.05 | 0.06 | −0.08 | −0.02 | <0.001 |
| Disease | −0.02 | 0.04 | 0.01 | −0.02 | 0.09 | 0.508 |
| Worry | 0.01 | 0.46 | 0.05 | 0.44 | 0.50 | <0.001 |
| Tension | 0.01 | 0.29 | 0.06 | 0.24 | 0.33 | <0.001 |
| Joy | −0.00 | −0.15 | 0.05 | −0.19 | −0.12 | <0.001 |
| Demands | −0.00 | −0.09 | 0.04 | −0.12 | −0.06 | <0.001 |
| Sample × Time | 0.00 | 0.00 | 0.04 | −0.04 | 0.04 | 0.815 |
| Disease × Worry | 0.01 | 0.05 | 0.02 | 0.00 | 0.10 | 0.030 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wallis, H.; Elgner, M.; Schurr, M.; Giel, K.E.; Martus, P.; Paul, G.; Jürgensen, J.S.; Allwang, C.; Mikolajczyk, R.; Galante-Gottschalk, A.; et al. Stress and Depressive and Anxiety Symptoms in the General Population and in SARS-CoV-2-Infected Patients—Findings from a Population-Based Three-Wave Study. J. Clin. Med. 2023, 12, 6240. https://doi.org/10.3390/jcm12196240
Wallis H, Elgner M, Schurr M, Giel KE, Martus P, Paul G, Jürgensen JS, Allwang C, Mikolajczyk R, Galante-Gottschalk A, et al. Stress and Depressive and Anxiety Symptoms in the General Population and in SARS-CoV-2-Infected Patients—Findings from a Population-Based Three-Wave Study. Journal of Clinical Medicine. 2023; 12(19):6240. https://doi.org/10.3390/jcm12196240
Chicago/Turabian StyleWallis, Hannah, Melanie Elgner, Marisa Schurr, Katrin Elisabeth Giel, Peter Martus, Gregor Paul, Jan Steffen Jürgensen, Christine Allwang, Rafael Mikolajczyk, Annette Galante-Gottschalk, and et al. 2023. "Stress and Depressive and Anxiety Symptoms in the General Population and in SARS-CoV-2-Infected Patients—Findings from a Population-Based Three-Wave Study" Journal of Clinical Medicine 12, no. 19: 6240. https://doi.org/10.3390/jcm12196240
APA StyleWallis, H., Elgner, M., Schurr, M., Giel, K. E., Martus, P., Paul, G., Jürgensen, J. S., Allwang, C., Mikolajczyk, R., Galante-Gottschalk, A., Ehehalt, S., Junne, F., & Binneböse, M. (2023). Stress and Depressive and Anxiety Symptoms in the General Population and in SARS-CoV-2-Infected Patients—Findings from a Population-Based Three-Wave Study. Journal of Clinical Medicine, 12(19), 6240. https://doi.org/10.3390/jcm12196240





