Pelvic Ring Fractures in Older Adult Patients—Assessing Physician Practice Variation among (Orthopedic) Trauma Surgeons
Abstract
:1. Introduction
2. Materials and Methods
3. Results
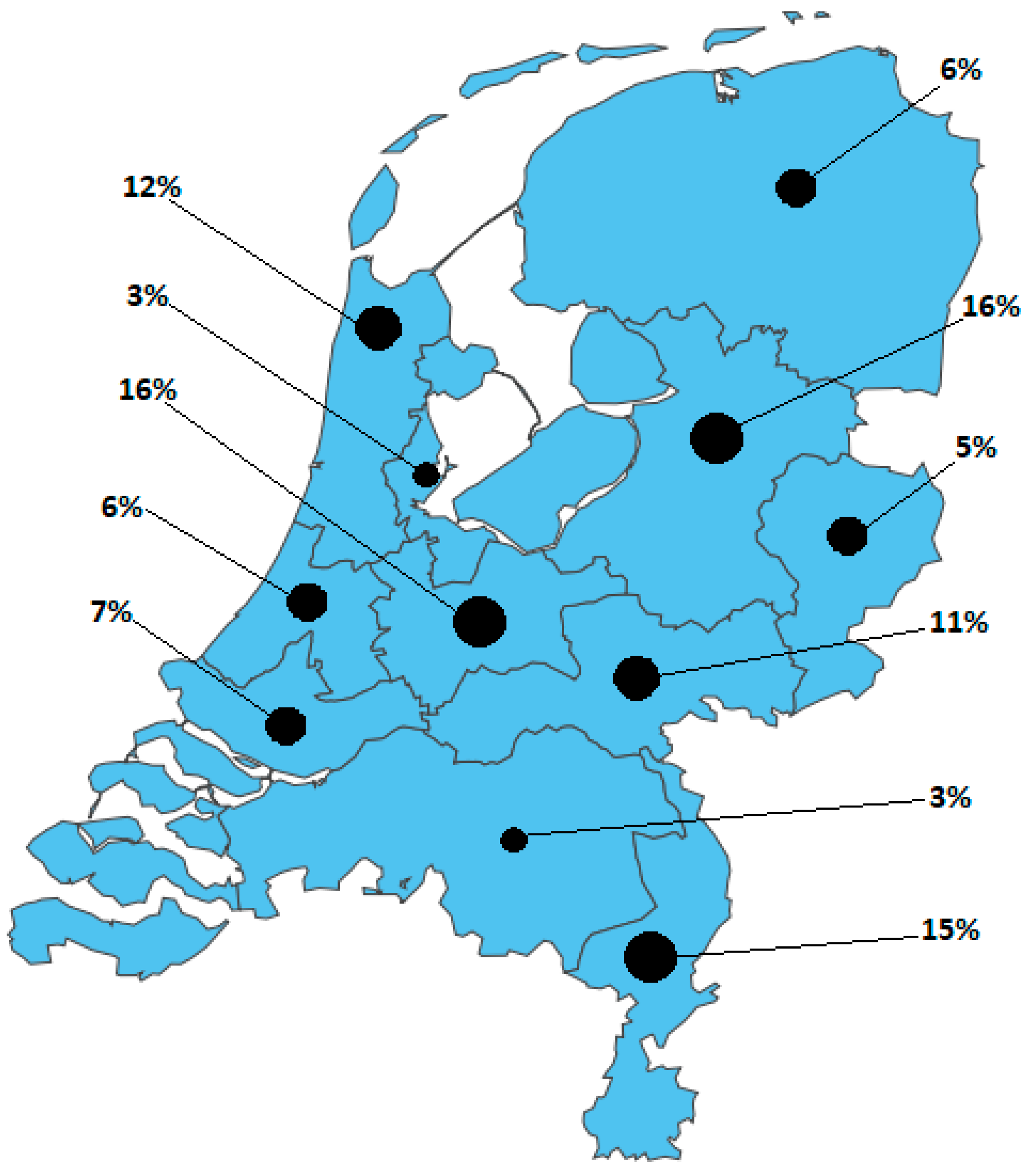
3.1. Respondents
3.2. Imaging
3.3. Treatment and Referral
3.4. Aftercare
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Questions | Answer Options |
|---|---|
| 1. What are you? | A. Trauma surgeon B. Trauma surgery resident C. Orthopedic surgeon D. Orthopedic surgery resident |
| 2. For how long have you worked as a trauma or an orthopedic surgeon? | A. 0–5 years B. 6–10 years C. 11–20 years D. >20 years E. In residency |
| 3. In which trauma care network region do you work? | A. Eastern Regional Emergency Healthcare Network B. Acute Care Network North-West C. Network Emergency Care Brabant D. Network Acute Care West E. Network Emergency Care Euregio F. Trauma Center Southwest Netherlands G. Network Acute Care Limburg H. Network Emergency Care Zwolle I. Trauma Network Middle Netherlands region J. AcuteCareNet AMC K. Acute Care Network North Netherlands |
| 4. Which Trauma Center Level meets your hospital? | A. Level 1 (highest) B. Level 2 C. Level 3 (lowest) |
| 5. Are pelvic and acetabular fracture operations performed in your hospital? | A. Yes, 1–20 operations per year B. Yes, 21–40 operations per year C. Yes, 41–60 operations per year D. Yeas, >60 operations per year E. No |
| 6. Do you perform pelvic and acetabular fracture operations? | A. Yes, 1–10 operations per year B. Yes, 11–20 operations per year C. Yes, 21–40 operations per year D. Yes, >40 operations per year E. No |
| 7. How many elderly patients (≥65 years) with a superior/inferior ramus fracture on plain radiographic imaging do you treat in your hospital (both operatively and conservatively)? | A. 1–25 patients per year B. 26–50 patients per year C. 51–75 patients per year D. 76–100 patients per year E. >100 patients per year |
| 8. How often do you refer elderly patients with pelvic fractures after low-energy trauma to a specialized pelvic center? | A. 1–5 times per year B. 6–10 times per year C. >10 times per year D. Not applicable |
| 9. Who generally assesses an elderly patient with a superior/inferior ramus fracture in your hospital’s Emergency Department (ED)? | A. Surgeon/orthopedic surgeon B. Surgical/orthopedic residents (not in training) C. Surgical/orthopedic residents (in training) D. Emergency physician E. Otherwise, namely: |
| 10. In case an elderly patient with a superior/inferior ramus fracture needs to be admitted to the hospital, where will this patient be admitted? | A. Surgical ward/orthopedic ward B. Geriatric ward C. Nursing home D. ‘Primary care’ nursing home E. Otherwise, namely: |
| 11. Is there a treatment protocol for elderly patients with a superior/inferior ramus fracture in your hospital? | A. Yes, named: B. No C. I am not aware if there is such a treatment protocol |
| 12. Mrs. A. is a 75-year-old, independently living ASA 2 patient. She tripped and fell at home. Plain radiographic imaging showed a superior/inferior ramus fracture on the left side. Would you, based on this information, perform a CT scan in the hospital you work at? | A. No, a CT scan has no treatment consequences B. Yes, always C. Yes, if the patient has pain on palpation of the sacrum D. Yes, if the patient is very painful during mobilization E. Otherwise, namely: |
| 13. Mrs. B. is a 77-year-old ASA 4 patient living in sheltered housing. She tripped and fell at home. Plain radiographic imaging showed a superior/inferior ramus fracture on the left side. Would you, based on this information, perform a CT scan in the hospital you work in? | A. No, a CT scan has no treatment consequences B. Yes, always C. Yes, if the patient has pain on palpation of the sacrum D. Yes, if the patient is very painful during mobilization E. Otherwise, namely: |
| 14. Mrs. C. is a 75-year-old, independently living ASA 2 patient. She fell on the street, and plain radiographic imaging showed a superior/inferior ramus fracture on the right side. She is discharged from the ER with oral painkillers. The patient comes back to your outpatient clinic after 14 days. She mobilizes with difficulty, sits in a wheelchair, walks with a four-wheel walker indoors, and uses Paracetamol and Diclofenac. A CT scan shows an LC1/FFP3c fracture. Do you think, based on this information, the patient is eligible for surgical fixation? | A. No, I do not think this is indicated and would have little impact on this patient’s outcome B. No, I think operative pelvic fixation would be too invasive for this patient C. Yes, if the patient has evident pelvic pain during a physical exam D. Yes, only if the pain did not decrease at 6 weeks follow-up E. Otherwise, namely: |
| 15. Mrs. D. is a 69-year-old, independently living ASA 3 patient with COPD Gold 3. She fell on the street, and plain radiographic imaging showed a superior/inferior ramus fracture on the right side. She is discharged from the ER with oral painkillers. The patient comes back to your outpatient clinic after 14 days. She mobilizes with difficulty, sits in a wheelchair, walks with a four-wheel walker indoors, and uses Paracetamol and Diclofenac. A CT scan shows an LC1/FFP3c fracture. Do you think, based on this information, the patient is eligible for surgical fixation? | A. No, I do not think this is indicated and would have little impact on this patient’s outcome B. No, I think operative pelvic fixation would be too invasive for this patient C. Yes, if the patient has evident pelvic pain during a physical exam D. Yes, only if the pain did not decrease at 6 weeks follow-up E. Otherwise, namely: |
| 16. Mrs. E is an 81-year-old ASA 3 patient. She fell on the street, and plain radiographic imaging showed a superior/inferior ramus fracture on the right side. She is admitted to the nursing ward and has difficulty turning in bed. Transfer from bed to toilet chair is possible. She uses Paracetamol, Diclofenac and Oxynorm. A CT scan shows an LC1/FFP3c fracture. Do you think, based on this information, the patient is eligible for surgical fixation? | A. No, I do not think this is indicated and would have little impact on this patient’s outcome B. No, I think operative pelvic fixation would be too invasive for this patient C. Yes, if the patient has evident pelvic pain during a physical exam D. Yes, only if the pain did not decrease at 6 weeks follow-up E. Otherwise, namely: |
| 17. If plain radiographic imaging shows a superior/inferior ramus fracture and the patient is treated conservatively, when would your first follow-up moment be? | A. No follow-up B. Within 1 week C. Within 2 weeks D. Within 3 to 6 weeks E. After >6 weeks |
| 18. If plain radiographic imaging shows a superior/inferior ramus fracture and the patient is treated conservatively, when would you advise the patient to use full weight bearing? | A. Immediately, based on the patient’s pain B. After 2 to 4 weeks C. After 4 to 6 weeks D. After 6 to 8 weeks E. Otherwise, namely: |
| 19. If a patient underwent operative fixation related to a right-sided sacrum and superior/inferior ramus fracture, when would you advise the patient to use full weight bearing? | A. Immediately, based on the patient’s pain B. 2 to 4 weeks minimal weight bearing, afterward full weight bearing C. 4–6 weeks minimal weight bearing, then full weight bearing D. 6 to 8 weeks minimal weight bearing, then full weight bearing E. Otherwise, namely: |
Appendix B

Appendix C

References
- Kozar, R.A.; Arbabi, S.; Stein, D.M.; Shackford, S.R.; Barraco, R.D.; Biffl, W.L.; Brasel, K.J.; Cooper, Z.; Fakhry, S.M.; Livingston, D.; et al. Injury in the aged: Geriatric trauma care at the crossroads. J. Trauma Acute Care Surg. 2015, 78, 1197–1209. [Google Scholar] [PubMed]
- Hartholt, K.A.; van der Velde, N.; Looman, C.W.N.; van Lieshout, E.M.M.; Panneman, M.J.M.; van Beeck, E.F.; Patka, P.; van der Cammen, T.J.M. Trends in Fall-Related Hospital Admissions in Older Persons in the Netherlands. Arch. Intern. Med. 2010, 170, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, D.O.; Ponsen, K.J.; Fiocco, M.; Amodio, S.; Leenen, L.P.H.; Goslings, J.C. Pelvic fractures in the Netherlands: Epidemiology, characteristics and risk factors for in-hospital mortality in the older and younger population. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P.; Palvanen, M.; Niemi, S.; Parkkari, J.; Järvinen, M. Epidemiology of Osteoporotic Pelvic Fractures in Elderly People in Finland: Sharp Increase in 1970–1997 and Alarming Projections for the New Millennium. Osteoporos. Int. 2000, 11, 443–448. [Google Scholar] [CrossRef]
- Behanova, M.; Haschka, J.; Reichardt, B.; Dimai, H.-P.; Resch, H.; Zwerina, J.; Kocijan, R. Pelvic Fractures-An Underestimated Problem? Incidence and Mortality Risk after Pelvic Fracture in Austria, 2010–2018. J. Clin. Med. 2022, 11, 2834. [Google Scholar]
- Marrinan, S.; Pearce, M.S.; Jiang, X.Y.; Waters, S.; Shanshal, Y. Admission for osteoporotic pelvic fractures and predictors of length of hospital stay, mortality and loss of independence. Age Ageing 2015, 44, 258–261. [Google Scholar] [CrossRef]
- Reito, A.; Kuoppala, M.; Pajulammi, H.; Hokkinen, L.; Kyrölä, K.; Paloneva, J. Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: A comparison with an age-matched femoral neck fracture cohort and general population. BMC Geriatr. 2019, 19, 315–317. [Google Scholar] [CrossRef]
- Banierink, H.; Duis, K.T.; de Vries, R.; Wendt, K.; Heineman, E.; Reininga, I.; Ijpma, F. Pelvic ring injury in the elderly: Fragile patients with substantial mortality rates and long-term physical impairment. PLoS ONE 2019, 14, e0216809. [Google Scholar] [CrossRef]
- Studer, P.; Suhm, N.; Zappe, B.; Bless, N.; Jakob, M. Pubic rami fractures in the elderly—A neglected injury? Swiss Med. Wkly. 2013, 143, w13859. [Google Scholar]
- van Dijk, W.; Poeze, M.; van Helden, S.; Brink, P.; Verbruggen, J. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury 2010, 41, 411–414. [Google Scholar] [CrossRef]
- Clement, N.D.; Court-Brown, C.M. Elderly pelvic fractures: The incidence is increasing and patient demographics can be used to predict the outcome. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 1431–1437. [Google Scholar] [CrossRef]
- Schicho, A.; Schmidt, S.A.; Seeber, K.; Olivier, A.; Richter, P.H.; Gebhard, F. Pelvic X-ray misses out on detecting sacral fractures in the elderly—Importance of CT imaging in blunt pelvic trauma. Injury 2016, 47, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Scheyerer, M.J.; Osterhoff, G.; Wehrle, S.; Wanner, G.A.; Simmen, H.-P.; Werner, C.M. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury 2012, 43, 1326–1329. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Dietz, S.-O.; Ossendorf, C.; Pairon, P.; Wagner, D.; Hofmann, A. Fragility fractures of the pelvis: Should they be fixed? Acta Chir. Orthop. Traumatol. Cech. 2015, 82, 101–112. [Google Scholar] [CrossRef]
- Soles, G.L.; Ferguson, T.A. Fragility fractures of the pelvis. Curr. Rev. Musculoskelet. Med. 2012, 5, 222–228. [Google Scholar]
- Smith, H.E.; Yuan, P.S.; Sasso, R.; Papadopolous, S.; Vaccaro, A.R. An Evaluation of Image-Guided Technologies in the Placement of Percutaneous Iliosacral Screws. Spine 2006, 31, 234–238. [Google Scholar] [CrossRef] [PubMed]
- Hopf, J.C.; Krieglstein, C.F.; Müller, L.P.; Koslowsky, T.C. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury 2015, 46, 1631–1636. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.G.G.; Kelly, J.; Rickman, M. Operative management of fragility fractures of the pelvis—A systematic review. BMC Musculoskelet. Disord. 2021, 22, 717. [Google Scholar] [CrossRef]
- LeBoff, M.S.; Greenspan, S.L.; Insogna, K.L.; Lewiecki, E.M.; Saag, K.G.; Singer, A.J.; Siris, E.S. The clinician’s guide to prevention and treatment of osteoporosis. Osteoporos. Int. 2022, 33, 2049–2102. [Google Scholar] [CrossRef]
- Nüchtern, J.; Hartel, M.; Henes, F.; Groth, M.; Jauch, S.; Haegele, J.; Briem, D.; Hoffmann, M.; Lehmann, W.; Rueger, J.; et al. Significance of clinical examination, CT and MRI scan in the diagnosis of posterior pelvic ring fractures. Injury 2015, 46, 315–319. [Google Scholar] [CrossRef]
- Wagner, D.; Ossendorf, C.; Gruszka, D.; Hofmann, A.; Rommens, P.M. Fragility fractures of the sacrum: How to identify and when to treat surgically? Eur. J. Trauma Emerg. Surg. 2015, 41, 349–362. [Google Scholar] [PubMed]
- Mennen, A.; Peters, R.; Rutten, M.; van Embden, D. Spinal anesthesia in the percutaneous fixation of fragility fractures of the pelvis. Trauma Case Rep. 2022, 42, 100735. [Google Scholar] [CrossRef]
- Eckardt, H.; Egger, A.; Hasler, R.M.; Zech, C.J.; Vach, W.; Suhm, N.; Morgenstern, M.; Saxer, F. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: Assessment of complications and factors influencing failure. Injury 2017, 48, 2717–2723. [Google Scholar] [CrossRef] [PubMed]
- Arduini, M.; Saturnino, L.; Piperno, A.; Iundusi, R.; Tarantino, U. Fragility fractures of the pelvis: Treatment and preliminary results. Aging Clin. Exp. Res. 2015, 27 (Suppl. S1), S61–S67. [Google Scholar] [CrossRef]
- Nuber, S.; Ritter, B.; Fenwick, A.; Förch, S.; Wanzl, M.; Nuber, M.; Mayr, E. Midterm follow-up of elderly patients with fragility fractures of the pelvis: A prospective cohort-study comparing operative and non-operative treatment according to a therapeutic algorithm. Injury 2022, 53, 496–505. [Google Scholar] [CrossRef]
- Pulley, B.R.; Cotman, S.B.; Fowler, T.T. Surgical Fixation of Geriatric Sacral U-Type Insufficiency Fractures: A Retrospective Analysis. J. Orthop. Trauma 2018, 32, 617–622. [Google Scholar] [CrossRef] [PubMed]
- Balling, H. Additional Sacroplasty Does Not Improve Clinical Outcome in Minimally Invasive Navigation-Assisted Screw Fixation Procedures for Nondisplaced Insufficiency Fractures of the Sacrum. Spine 2019, 44, 534–542. [Google Scholar] [CrossRef]
- Vanderschot, P.; Kuppers, M.; Sermon, A.; Lateur, L. Trans-iliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J. Orthop. 2009, 43, 245–252. [Google Scholar] [CrossRef]
- Küper, M.A.; Trulson, A.; Stuby, F.M.; Stöckle, U. Pelvic ring fractures in the elderly. EFORT Open Rev. 2019, 4, 313–320. [Google Scholar] [CrossRef]
- Oberkircher, L.; Lenz, J.; Bücking, B.; Eschbach, D.; Aigner, R.; Bliemel, C.; Schoeneberg, C.; Ruchholtz, S.; Hack, J. Which factors influence treatment decision in fragility fractures of the pelvis?—Results of a prospective study. BMC Musculoskelet. Disord. 2021, 22, 690. [Google Scholar] [CrossRef]
- Timmer, R.A.; Verhage, S.M.; Krijnen, P.; Meylaerts, S.A.G.; Schipper, I.B. Indications for surgical fixation of low-energy pelvic ring fractures in elderly: A systematic review. Arch. Orthop. Trauma Surg. 2022, 143, 2417–2428. [Google Scholar] [CrossRef] [PubMed]
- Hvid, L.; Suetta, C.; Nielsen, J.; Jensen, M.; Frandsen, U.; Ørtenblad, N.; Kjaer, M.; Aagaard, P. Aging impairs the recovery in mechanical muscle function following 4days of disuse. Exp. Gerontol. 2014, 52, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Meyer, V.M.; Benjamens, S.; El Moumni, M.; Lange, J.F.M.; Pol, R.A. Global Overview of Response Rates in Patient and Health Care Professional Surveys in Surgery: A Systematic Review. Ann. Surg. 2022, 275, e75–e81. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mennen, A.H.M.; Oud, S.; Halm, J.A.; Peters, R.W.; Willems, H.C.; Van Embden, D. Pelvic Ring Fractures in Older Adult Patients—Assessing Physician Practice Variation among (Orthopedic) Trauma Surgeons. J. Clin. Med. 2023, 12, 6344. https://doi.org/10.3390/jcm12196344
Mennen AHM, Oud S, Halm JA, Peters RW, Willems HC, Van Embden D. Pelvic Ring Fractures in Older Adult Patients—Assessing Physician Practice Variation among (Orthopedic) Trauma Surgeons. Journal of Clinical Medicine. 2023; 12(19):6344. https://doi.org/10.3390/jcm12196344
Chicago/Turabian StyleMennen, Anna H. M., Sharon Oud, Jens A. Halm, Rolf W. Peters, Hanna C. Willems, and Daphne Van Embden. 2023. "Pelvic Ring Fractures in Older Adult Patients—Assessing Physician Practice Variation among (Orthopedic) Trauma Surgeons" Journal of Clinical Medicine 12, no. 19: 6344. https://doi.org/10.3390/jcm12196344
APA StyleMennen, A. H. M., Oud, S., Halm, J. A., Peters, R. W., Willems, H. C., & Van Embden, D. (2023). Pelvic Ring Fractures in Older Adult Patients—Assessing Physician Practice Variation among (Orthopedic) Trauma Surgeons. Journal of Clinical Medicine, 12(19), 6344. https://doi.org/10.3390/jcm12196344







