Efficacy of Insulin Titration Driven by SMS in Improving Glycemic Control in People with Type 2 Diabetes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Subjects and Inclusion Criteria
- −
- Cases (intervention group): subjects with T2D that used an SMS-based insulin titration service. Cases were recruited from Primary Health Care Centers (PHCC) of our engagement area.
- −
- Controls: subjects with T2D under the standard of care. This group was obtained from electronic records belonging to the System for the Development of Research in Primary Care (SIDIAP) database. This comprises the clinical information coded in the corresponding medical records from the PHCC of Institut Català de la Salut (ICS). The control group was matched with each case (1:1) by age (±3 years), sex, diabetes duration (±3 years), body mass index (BMI) (±3), diabetic complications and socioeconomic and geographical area (from the same PHCC as the cases).
2.2. Methods
2.3. Primary and Secondary Endpoints or Objectives
2.4. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [PubMed]
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998, 352, 837–853. [Google Scholar] [CrossRef]
- Buse, J.B.; Wexler, D.J.; Tsapas, A.; Rossing, P.; Mingrone, G.; Mathieu, C.; D’Alessio, D.A.; Davies, M.J. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020, 43, 487–493. [Google Scholar]
- Stumvoll, M.; Goldstein, B.J.; van Haeften, T.W. Type 2 diabetes: Principles of pathogenesis and therapy. Lancet 2005, 365, 1333–1346. [Google Scholar] [CrossRef] [PubMed]
- Lovshin, J.A.; Zinman, B. Diabetes: Clinical inertia—A barrier to effective management of T2DM. Nat. Rev. Endocrinol. 2013, 9, 635–636. [Google Scholar] [CrossRef] [PubMed]
- Van Bruggen, R.; Gorter, K.; Stolk, R.; Klungel, O.; Rutten, G. Clinical inertia in general practice: Widespread and related to the outcome of diabetes care. Fam. Pract. 2009, 26, 428–436. [Google Scholar] [CrossRef]
- Khunti, K.; Wolden, M.L.; Thorsted, B.L.; Andersen, M.; Davies, M.J. Clinical inertia in people with type 2 diabetes: A retrospective cohort study of more than 80,000 people. Diabetes Care 2013, 36, 3411–3417. [Google Scholar] [CrossRef]
- Khunti, K.; Nikolajsen, A.; Thorsted, B.L.; Andersen, M.; Davies, M.J.; Paul, S.K. Clinical inertia with regard to intensifying therapy in people with type 2 diabetes treated with basal insulin. Diabetes Obes. Metab. 2016, 18, 401–409. [Google Scholar] [CrossRef]
- Khunti, K.; Millar-Jones, D. Clinical inertia to insulin initiation and intensification in the UK: A focused literature review. Prim. Care Diabetes 2017, 11, 3–12. [Google Scholar] [CrossRef]
- Carratalá-Munuera, M.C.; Gil-Guillen, V.F.; Orozco-Beltran, D.; Navarro-Pérez, J.; Caballero-Martínez, F.; Álvarez-Guisasola, F.; García-Soidán, J.; Fluixá-Carrascosa, C.; Franch-Nadal, J.; Martín-Rioboó, E.; et al. Barriers associated with poor control in Spanish diabetic patients. A consensus study. Int. J. Clin. Pract. 2013, 67, 888–894. [Google Scholar] [CrossRef]
- Phillips, L.S.; Branch, W.T., Jr.; Cook, C.B.; Doyle, J.P.; El-Kebbi, I.M.; Gallina, D.L.; Miller, C.D.; Ziemer, D.C.; Barnes, C.S. Clinical inertia. Ann. Intern. Med. 2001, 135, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Ziemer, D.C.; Miller, C.D.; Rhee, M.K.; Doyle, J.P.; Watkins, C.; Cook, C.B.; Gallina, D.L.; El-Kebbi, I.M.; Barnes, C.S.; Dunbar, V.G.; et al. Clinical inertia contributes to poor diabetes control in a primary care setting. Diabetes Educ. 2005, 31, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.R.; Hux, J.E.; Laupacis, A.; Zinman, B.; van Walraven, C. Clinical inertia in response to inadequate glycemic control: Do specialists differ from primary care physicians? Diabetes Care 2005, 28, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Ratanawongsa, N.; Crosson, J.C.; Schillinger, D.; Karter, A.J.; Saha, C.K.; Marrero, D.G. Getting under the skin of clinical inertia in insulin initiation: The Translating Research Into Action for Diabetes (TRIAD) Insulin Starts Project. Diabetes Educ. 2012, 38, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Leiter, L.A.; Boras, D.; Woo, V.C. Dosing irregularities and self-treated hypoglycemia in type 2 diabetes: Results from the Canadian cohort of an international survey of patients and healthcare professionals. Can. J. Diabetes 2014, 38, 38–44. [Google Scholar] [CrossRef]
- Donnelly, L.A.; Morris, A.D.; Evans, J.M.M. DARTS/MEMO collaboration. Adherence to insulin and its association with glycaemic control in patients with type 2 diabetes. QJM Mon. J. Assoc. Physicians 2007, 100, 345–350. [Google Scholar] [CrossRef]
- Munshi, M.N.; Slyne, C.; Greenberg, J.M.; Greaves, T.; Lee, A.; Carl, S.; Atakov-Castillo, A.; Toschi, E. Nonadherence to Insulin Therapy Detected by Bluetooth-Enabled Pen Cap Is Associated With Poor Glycemic Control. Diabetes Care 2019, 42, 1129–1131. [Google Scholar] [CrossRef]
- Polonsky, W.H.; Fisher, L.; Earles, J.; Dudl, R.J.; Lees, J.; Mullan, J.; Jackson, R.A. Assessing psychosocial distress in diabetes: Development of the diabetes distress scale. Diabetes Care 2005, 28, 626–631. [Google Scholar] [CrossRef]
- Snaith, R.P. The Hospital Anxiety and Depression Scale. Health Qual. Life Outcomes 2003, 1, 29. [Google Scholar] [CrossRef]
- Burdine, J.N.; Felix, M.R.; Abel, A.L.; Wiltraut, C.J.; Musselman, Y.J. The SF-12 as a population health measure: An exploratory examination of potential for application. Health Serv. Res. 2000, 35, 885–904. [Google Scholar]
- Fisher, L.; Hessler, D.M.; Polonsky, W.H.; Mullan, J. When is diabetes distress clinically meaningful?: Estab-lishing cut points for the Diabetes Distress Scale. Diabetes Care 2012, 35, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.S.; Park, S.Y.; Kang, J.G.; Lee, S.J.; Ihm, S.H.; Choi, M.G.; Yoo, H.J. Insulin dose titration system in diabetes patients using a short messaging service automatically produced by a knowledge matrix. Diabetes Technol. Ther. 2010, 12, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Levy, N.; Moynihan, V.; Nilo, A.; Singer, K.; Bernik, L.S.; Etiebet, M.A.; Fang, Y.; Cho, J.; Natarajan, S. The Mobile Insulin Titration Intervention (MITI) for Insulin Adjustment in an Urban, Low-Income Population: Randomized Controlled Trial. J. Med. Internet Res. 2015, 17, e180. [Google Scholar] [CrossRef] [PubMed]
- Langford, A.T.; Wang, B.; Orzeck-Byrnes, N.A.; Aidasani, S.R.; Hu, L.; Applegate, M.; Moloney, D.N.; Sevick, M.A.; Rogers, E.S.; Levy, N.K. Sociodemographic and clinical correlates of key outcomes from a Mobile Insulin Titration Intervention (MITI) for medically underserved patients. Patient Educ. Couns. 2019, 102, 520–527. [Google Scholar] [CrossRef]
- Ferrara, A.; Hedderson, M.M.; Brown, S.D.; Ehrlich, S.F.; Tsai, A.L.; Feng, J.; Galarce, M.; Marcovina, S.; Catalano, P.; Quesenberry, C.P. A telehealth lifestyle intervention to reduce excess gestational weight gain in pregnant women with overweight or obesity (GLOW): A randomised, parallel-group, controlled trial. Lancet Diabetes Endocrinol. 2020, 8, 490–500. [Google Scholar] [CrossRef]
- Al-Mutairi, A.M.; Alshabeeb, M.A.; Abohelaika, S.; Alomar, F.A.; Bidasee, K.R. Impact of telemedicine on glycemic control in type 2 diabetes mellitus during the COVID-19 lockdown period. Front. Endocrinol. 2023, 14, 1068018. [Google Scholar] [CrossRef]
- Middelbeek, R.J.W.; Bouchonville, M.F.; Agarwal, S.; Romeo, G.R. Editorial: Application of telehealth to diabetes care delivery and medical training: Challenges and opportunities. Front. Endocrinol. 2023, 14, 1229706. [Google Scholar] [CrossRef]
- Rosenstock, J.; Fitchet, M. Vildagliptin: Clinical trials programme in monotherapy and combination therapy for type 2 diabetes. Int. J. Clin. Pract. 2008, 62, 15–23. [Google Scholar] [CrossRef]
- Chen, T.Y.; Hsieh, C.J. Real-world effectiveness of sitagliptin as add-on therapy in patients with type 2 diabetes mellitus. Postgrad. Med. 2014, 126, 205–215. [Google Scholar] [CrossRef]
- Dang-Tan, T.; Kamble, P.S.; Meah, Y.; Gamble, C.; Ganguly, R.; Horter, L. Real-world Effectiveness of Liraglutide vs. Sitagliptin Among Older Patients with Type 2 Diabetes Enrolled in a Medicare Advantage Prescription Drug Plan: A Retrospective Observational Study. Diabetes Ther. Res. Treat. Educ. Diabetes Relat. Disord. 2020, 11, 213–228. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, L.; Lin, Y.; Liu, Y.; Yang, X.; Cao, W.; Ji, Y.; Chang, C. Effects of E-health-based interventions on glycemic control for patients with type 2 diabetes: A Bayesian network meta-analysis. Front. Endocrinol. 2023, 14, 1068254. [Google Scholar] [CrossRef] [PubMed]
- Von Storch, K.; Graaf, E.; Wunderlich, M.; Rietz, C.; Polidori, M.C.; Woopen, C. Telemedicine-Assisted Self-Management Program for Type 2 Diabetes Patients. Diabetes Technol. Ther. 2019, 21, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Haider, R.; Sudini, L.; Chow, C.K.; Cheung, N.W. Mobile phone text messaging in improving glycaemic control for patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2019, 150, 27–37. [Google Scholar] [CrossRef] [PubMed]
| Control Group | Intervention Group | p | |
|---|---|---|---|
| n | 59 | 59 | |
| Age (years) | 63.6 ± 11.7 | 64.1 ± 10.1 | 0.788 |
| Sex (women) % | 26 (44.1%) | 26 (44.1%) | 0.265 |
| Smokers (n, %) | 0.071 | ||
| 6 (10.2%) | 4 (6.8%) | |
| 10 (16.9%) | 11 (18.6%) | |
| 43 (72.9%) | 44 (74.6%) | |
| Body mass index (BMI) (kg/m2) | 32.2 ± 4.6 | 31.4 ± 7.6 | 0.531 |
| Hypertension (HTA) (%) | 41 (69.5%) | 40 (67.8%) | 0.315 |
| Dyslipidemia (DLP) (%) | 42 (74.1%) | 43 (74.1%) | 0.258 |
| T2D duration (years) | 10.7 ± 5.4 | 11.5 ± 6.7 | 0.474 |
| Time between T2D diagnosis and insulinization (years) | 3.5 ± 2.5 | 3.5 ± 2.6 | 0.875 |
| HbA1c (%) (mmol/mol) | 8.3 ± 0.4 | 8.3 ± 0.8 | 0.952 |
| 67 ± 3.2 | 67 ± 6.5 | ||
| Severe hypoglycemia (<54 mg/dL) (n) | 0 | 0 | n.s. |
| Mean FCBG at last week (mg/dL) | 168.3 ± 24.9 | 167.9 ± 27.4 | 0.148 |
| Insulin dose (UI/day) | 30.4 ± 7.1 | 30.7 ± 11.5 | 0.354 |
| Insulin dose (UI/Kg/day) | 0.37 ± 0.20 | 0.38 ± 0.13 | 0.167 |
| Fasting venous glucose (mg/dL) | 169.5 ± 65.5 | 170.5 ± 57.5 | 0.101 |
| Diabetes-related complications | |||
| 9 (15.3%) | 8 (13.6%) | 0.194 |
| 13 (22.0%) | 12 (20.3%) | 0.166 |
| 8 (13.6%) | 7 (11.9%) | 0.319 |
| 5 (8.5%) | 4 (6.8%) | 0.752 |
| 1 | 0 | 0.569 |
| 8 (13.6%) | 7 (11.9%) | 0.319 |
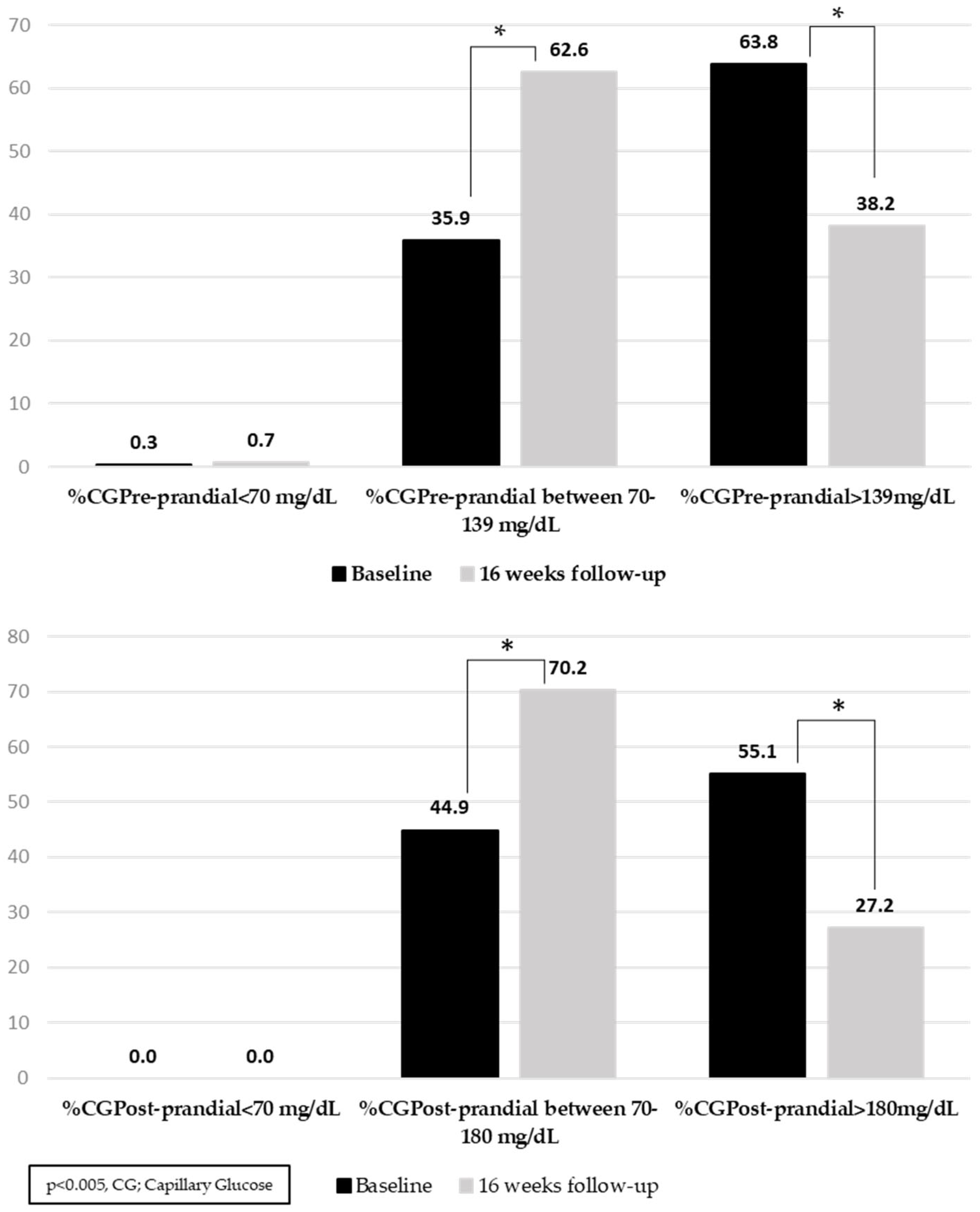
| Baseline | 16 Weeks of Follow-Up | p | |
|---|---|---|---|
| n | 47 | 47 | |
| HbA1c (%) (mmol/mol) | 8.3 ± 0.4 | 7.63 ± 0.1 | <0.001 |
| 67.0 ± 3.2 | 59.0 ± 0.8 | ||
| Fasting venous glucose (mg/dL) | 166.5 ± 9.5 | 131.3 ± 5.9 | <0.001 |
| Last week mean fasting capillary blood glucose (mg/dL) | 163.8 ± 3.5 | 123.4 ± 5.2 | <0.001 |
| Mean capillary blood glucose preprandial (mg/dL) | 152.2 ± 5.1 | 130.3 ± 6.2 | <0.001 |
| Mean capillary blood glucose 2 h postprandial (mg/dL) | 188.1 ± 6.9 | 160.8 ± 6.2 | <0.001 |
| Episodes of mild/moderate hypoglycemia (55–70 mg/dL) (n, %) | 8 (17.0%) | 4 (8.5%) | 0.184 |
| Episodes of severe hypoglycemia (<54 mg/dL) (n) | 0 | 0 | n.s |
| Insulin dose (UI) | 28.3 ± 1.5 | 36.1 ± 3.2 | <0.001 |
| Insulin dose (UI/Kg/day) | 0.35 ± 0.01 | 0.45 ± 0.04 | <0.001 |
| Fasting venous glucose (mg/dL) | 166.5 ± 9.5 | 131.3 ± 5.9 | <0.001 |
| Baseline | 16 Weeks of Follow-Up | p | |
|---|---|---|---|
| n | 59 | 59 | |
| HbA1c (%) (mmol/mol) | 8.3 ± 0.2 | 7.9 ± 0.1 | 0.008 |
| 67.0 ± 1.6 | 63.1 ± 0.8 | ||
| Fasting venous glucose (mg/dL) | 165.1 ± 7.3 | 151.2 ± 3.4 | 0.011 |
| Last week mean fasting capillary blood glucose (mg/dL) | 168.3 ± 24.9 | 149.2 ± 6.0 | 0.021 |
| Episodes of severe hypoglycemia (<54 mg/dL) (n) | 0 | 0 | n.s |
| Insulin dose (UI) | 30.4 ± 7.1 | 31.9 ± 1.6 | 0.519 |
| Insulin dose (UI/Kg/day) | 0.37 ± 0.20 | 0.39 ± 0.2 | 0.519 |
| Questionnaires | Baseline | 16 Weeks of Follow-Up | p |
|---|---|---|---|
| n | 47 | 47 | |
| DDS | |||
| Total Score (absolute) | 2.1 ± 0.2 | 1.9 ± 0.2 | 0.082 |
| Total Score (%) | 48.5 | 34.4 | 0.21 |
| Emotional Burden (absolute) | 2.2 ± 0.2 | 1.9 ± 0.2 | 0.043 |
| Emotional Burden (%) | 47.6 | 30.9 | 0.03 |
| Physician Distress (absolute) | 1.8 ± 0.2 | 1.7 ± 0.2 | 0.529 |
| Physician Distress (%) | 30.6 | 25.0 | 0.57 |
| Regimen Distress (absolute) | 2.4 ± 0.2 | 1.4 ± 0.1 | <0.001 |
| Regimen Distress (%) | 52.2 | 17.2 | <0.001 |
| Interpersonal Distress (absolute) | 1.9 ± 0.2 | 1.4 ± 0.2 | 0.040 |
| Interpersonal Distress (%) | 27.0 | 16.2 | 0.03 |
| HADS | |||
| Anxiety (absolute) | 11.7 ± 0.7 | 12.2 ± 0.5 | 0.347 |
| Anxiety (%) | 61.7 | 57.4 | 0.361 |
| Depression (absolute) | 9.4 ± 0.3 | 8.8 ± 0.3 | 0.179 |
| Depression (%) | 17.7 | 6.6 | 0.049 |
| SF-12 | |||
| Physical (%) | 47.9 | 44.1 | 0.091 |
| Mental (%) | 76.1 | 35.6 | 0.001 |
| General (%) | 65.8 | 50.8 | 0.02 |
| Not At All (%) | A Little Bit (%) | Neither Too Much Nor Too Little (%) | Considerable (%) | A Lot (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Do you think that (SMS) has been useful for your glycemic control? | ||||||||||
| Appropriate use | 4.7 | 9.3 | 7.0 | 27.9 | 51.2 | |||||
| Poor adherence subject | 75 | 25 | 0 | 0 | 0 | |||||
| Are you satisfied with the (SMS) received? | ||||||||||
| Appropriate use | 4.7 | 7.0 | 4.7 | 34.9 | 48.8 | |||||
| Poor adherence subject | 25 | 75 | 0 | 0 | 0 | |||||
| Would you like to continue receiving the SMS service? | ||||||||||
| Appropriate use | 9.5 | 11.9 | 4.8 | 42.9 | 31.0 | |||||
| Poor adherence subject | 50 | 50 | 0 | 0 | 0 | |||||
| Was the Use of the SMS insulin titration service easy for you? | ||||||||||
| Appropriate use | 2.3 | 9.3 | 7.0 | 39.5 | 41.9 | |||||
| Poor adherence subject | ||||||||||
| 0 event (%) | 1 event (%) | 2–3 events (%) | 3–5 events (%) | >5 events (%) | ||||||
| Did you have mild/moderate hypoglycemia during the time you used the SMS insulin titration service? | ||||||||||
| Appropriate use | 97.1 | 2.9 | 0 | 0 | 0 | |||||
| Poor adherence subject | 50 | 50 | 0 | 0 | 0 | |||||
| Did you have severe hypoglycemia during the time you used the SMS insulin titration service? | ||||||||||
| Appropriate use | 100 | 0 | 0 | 0 | 0 | |||||
| Poor adherence subject | 100 | 0 | 0 | 0 | 0 | |||||
| Nothing (%) | Sometimes (%) | Often (%) | A lot (%) | |||||||
| Did the SMS insulin titration service bother you because it interrupted your daily routine? | ||||||||||
| Appropriate use | 81.4 | 11.6 | 4.7 | 2.3 | ||||||
| Poor adherence subject | 0 | 50 | 25 | 25 | ||||||
| 1 (%) | 2 (%) | 3 (%) | 4 (%) | 5 (%) | 6 (%) | 7 (%) | 8 (%) | 9 (%) | 10 (%) | |
| How would you rate the usefulness of the SMS insulin titration service? (1—not at all useful and 10—very useful) | ||||||||||
| Appropriate use | 0 | 2.1 | 0 | 0 | 2.1 | 2.1 | 2.1 | 14.9 | 27.7 | 48.9 |
| Poor adherence subject | 25 | 0 | 25 | 25 | 25 | 0 | 0 | 0 | 0 | 0 |
| Appropriate Use | Poor Adherence Subject | p | |
|---|---|---|---|
| n | 47 | 12 | |
| Age (years) | 63.5 ± 8.9 | 61.3 ± 14.1 | 0.503 |
| Sex (women) % | 19 (40.4%) | 7 (58.3%) | 0.265 |
| Smoking | 0.361 | ||
| 4 (8.5%) | 0 | |
| 8 (17.0%) | 3 (25.0%) | |
| 35 (74.5%) | 9 (75.0%) | |
| Body mass index (BMI) (kg/m2) | 30.2 ± 5.4 | 36.3 ± 12.5 | 0.013 |
| Hypertension (HTA) (%) | 35 (74.5%) | 9 (75.0%) | 0.336 |
| Dyslipidemia (DLP) (%) | 39 (82.9%) | 9 (75.0%) | 0.078 |
| Education (years) | 10.2 ± 3.4 | 5.1 ± 1.2 | 0.001 |
| T2D duration (years) | 11.7 ± 7.3 | 10.8 ± 3.4 | 0.653 |
| Time between T2D diagnosis and insulinization (years) | 3.5 ± 2.5 | 3.7 ± 2.7 | 0.875 |
| HbA1c (%) (mmol/mol) | 8.3 ± 0.8 | 8.3 ± 0.8 | 0.976 |
| 67.1 ± 6.5 | 67.2 ± 6.5 | ||
| Mild/moderate hypoglycemia (55–70 mg/dL) | 7 (14.9%) | 1 (8.3%) | 0.011 |
| Severe hypoglycemia (<54 mg/dL) (n) | 0 | 0 | n.s |
| Last week mean fasting capillary blood glucose (mg/dL) | 165.3 ± 24.9 | 178.1 ± 34.8 | 0.148 |
| Basal insulin dose (UI/day) | 28.5 ± 10.9 | 39.2 ± 10.3 | 0.004 |
| Basal insulin dose (UI/Kg/day) | 0.35 ± 0.12 | 0.36 ± 0.24 | 0.785 |
| Fasting venous glucose (mg/dL) | 164.4 ± 53.3 | 199.1 ± 70.3 | 0.101 |
| Retinopathy (%) | 5 (10.6%) | 3 (25.0%) | 0.004 |
| Nephropathy (%) | 9 (19.2%) | 3 (25.0%) | 0.036 |
| Polyneuropathy (%) | 3 (6.4%) | 4 (33.3%) | 0.010 |
| Ischemic heart disease (%) | 4 (8.5%) | 0 | 0.295 |
| Stroke (%) | 0 | 0 | n.s |
| Peripheral arteriopathy (%) | 4 (8.5%) | 3 (25.0%) | 0.002 |
| Confident | Standard Error | z | p | 95% Conf. Interval | ||
|---|---|---|---|---|---|---|
| Education (years) | −1.80165 | 0.63262 | −2.85 | 0.004 | −3.04156 | −0.561746 |
| Age (years) | 0.00199 | 0.08591 | 0.02 | 0.982 | −0.16638 | 0.17037 |
| Body mass index (kg/m2) | 0.94142 | 0.20615 | 0.46 | 0.648 | −0.30991 | 0.49819 |
| Diabetes-related complications (no/yes) | 0.49433 | 2.98491 | 0.17 | 0.868 | −5.35598 | 6.34464 |
| _constant | 9.35905 | 8.95606 | 1.04 | 0.296 | −8.19452 | 26.9126 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortiz-Zúñiga, Á.; Simó-Servat, O.; Amigó, J.; Sánchez, M.; Morer, C.; Franch-Nadal, J.; Mayor, R.; Snel, T.; Simó, R.; Hernández, C. Efficacy of Insulin Titration Driven by SMS in Improving Glycemic Control in People with Type 2 Diabetes. J. Clin. Med. 2023, 12, 6364. https://doi.org/10.3390/jcm12196364
Ortiz-Zúñiga Á, Simó-Servat O, Amigó J, Sánchez M, Morer C, Franch-Nadal J, Mayor R, Snel T, Simó R, Hernández C. Efficacy of Insulin Titration Driven by SMS in Improving Glycemic Control in People with Type 2 Diabetes. Journal of Clinical Medicine. 2023; 12(19):6364. https://doi.org/10.3390/jcm12196364
Chicago/Turabian StyleOrtiz-Zúñiga, Ángel, Olga Simó-Servat, Judit Amigó, Mónica Sánchez, Carla Morer, Josep Franch-Nadal, Regina Mayor, Tim Snel, Rafael Simó, and Cristina Hernández. 2023. "Efficacy of Insulin Titration Driven by SMS in Improving Glycemic Control in People with Type 2 Diabetes" Journal of Clinical Medicine 12, no. 19: 6364. https://doi.org/10.3390/jcm12196364
APA StyleOrtiz-Zúñiga, Á., Simó-Servat, O., Amigó, J., Sánchez, M., Morer, C., Franch-Nadal, J., Mayor, R., Snel, T., Simó, R., & Hernández, C. (2023). Efficacy of Insulin Titration Driven by SMS in Improving Glycemic Control in People with Type 2 Diabetes. Journal of Clinical Medicine, 12(19), 6364. https://doi.org/10.3390/jcm12196364






