Amniocentesis—When It Is Clear That It Is Not Clear
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. One of Three Criteria Used
3.2. Two of the Three Criteria Used
3.3. All of the Three Criteria Used
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jummaat, F.; Ahmad, S.; Ismail, N.A.M. 5-Year review on amniocentesis and its maternal fetal complications. Horm. Mol. Biol. Clin. Investig. 2019, 40, 20190006. [Google Scholar] [CrossRef] [PubMed]
- Ghi, T.; Sotiriadis, A.; Calda, P.; Costa, F.D.S.; Raine-Fenning, N.; Alfirevic, Z.; McGillivray, G. International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) ISUOG Practice Guidelines: Invasive procedures for prenatal diagnosis. Ultrasound Obstet. Gynecol. 2016, 48, 256–268. [Google Scholar] [CrossRef] [PubMed]
- Anandakumar, C.; Wong, Y.C.; Annapoorna, V.; Arulkumaran, S.; Chia, D.; Bongso, A.; Ratnam, S.S. Amniocentesis and Its Complications. Aust. New Zealand J. Obstet. Gynaecol. 1992, 32, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Carlson, L.M.; Vora, N.L. Prenatal Diagnosis: Screening and Diagnostic Tools. Obstet. Gynecol. Clin. N. Am. 2017, 44, 245–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goto, M.; Nakamura, M.; Takita, H.; Sekizawa, A. Study for risks of amniocentesis in anterior placenta compared to placenta of other locations. Taiwan J. Obstet. Gynecol. 2021, 60, 690–694. [Google Scholar] [CrossRef]
- Seeds, J.W. Diagnostic mid trimester amniocentesis: How safe? Am. J. Obstet. Gynecol. 2004, 191, 607–615. [Google Scholar] [CrossRef]
- Benn, P.; Borrell, A.; Cuckle, H.; Dugoff, L.; Gross, S.; Johnson, J.-A.; Maymon, R.; Odibo, A.; Schielen, P.; Spencer, K.; et al. Prenatal Detection of Down Syndrome using Massively Parallel Sequencing (MPS): A rapid response statement from a committee on behalf of the Board of the International Society for Prenatal Diagnosis, 24 October 2011. Prenat. Diagn. 2012, 32, 1–2. [Google Scholar] [CrossRef]
- Gregg, A.R.; Gross, S.; Best, R.; Monaghan, K.; Bajaj, K.; Skotko, B.; Thompson, B.; Watson, M. ACMG statement on noninvasive prenatal screening for fetal aneuploidy. Anesth. Analg. 2013, 15, 395–398. [Google Scholar] [CrossRef] [Green Version]
- Langlois, S.; Brock, J.-A.; Wilson, R.D.; Audibert, F.; Carroll, J.; Cartier, L.; Gagnon, A.; Johnson, J.-A.; MacDonald, W.; Murphy-Kaulbeck, L.; et al. RETIRED: Current Status in Non-Invasive Prenatal Detection of Down Syndrome, Trisomy 18, and Trisomy 13 Using Cell-Free DNA in Maternal Plasma. J. Obstet. Gynaecol. Can. 2013, 35, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Obstetricians & Gynaecologists. Non-invasive Prenatal Testing for Chromosomal Abnormality using Maternal Plasma DNA. RCOG Sci. Impact Pap. 2014, 15, 1–14. [Google Scholar]
- Taglauer, E.; Wilkins-Haug, L.; Bianchi, D. Review: Cell-free fetal DNA in the maternal circulation as an indication of placental health and disease. Placenta 2014, 35, S64–S68. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, D.W.; Platt, L.D.; Goldberg, J.D.; Abuhamad, A.Z.; Sehnert, A.J.; Rava, R.P. Genome-Wide Fetal Aneuploidy Detection by Maternal Plasma DNA Sequencing. Obstet. Gynecol. 2012, 119, 890–901. [Google Scholar] [CrossRef] [PubMed]
- Dondorp, W.; De Wert, G.; Bombard, Y.; Bianchi, D.W.; Bergmann, C.; Borry, P.; Chitty, L.S.; Fellmann, F.; Forzano, F.; Hall, A.; et al. Non-invasive prenatal testing for aneuploidy and beyond: Challenges of responsible innovation in prenatal screening. Summary and recommendations. Eur. J. Hum. Genet. 2015, 23, 1438–1450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Srouji, S.S.; Carr, D.B.; Gardella, C.M.; Benedetti, T.; Tait, J.F. The Effect of Common Clinical Contaminants on Amniotic Fluid Fluorescence Polarization Results. Obstet. Gynecol. 2004, 104, 1237–1243. [Google Scholar] [CrossRef]
- Weida, J.; Patil, A.S.; Schubert, F.P.; Vance, G.; Drendel, H.; Reese, A.; Dlouhy, S.; Bai, S.; Lee, M.J. Prevalence of maternal cell contamination in amniotic fluid samples. J. Matern. Neonatal Med. 2017, 30, 2133–2137. [Google Scholar] [CrossRef] [PubMed]
- Nufl, S.; Brebaum, D.; Grond-Ginsbach, C. Maternal cell contamination in amniotic fluid samples as a consequence of the sampling technique. Hum. Genet. 1994, 93, 121–124. [Google Scholar]
- Benn, P.A.; Hsu, L.Y.F.; Karp, L.E. Maternal cell contamination of amniotic fluid cell cultures: Results of a U.S. nationwide survey. Am. J. Med. Genet. 1983, 15, 297–305. [Google Scholar] [CrossRef]
- Alfirevic, Z.; Navaratnam, K.; Mujezinovic, F. Amniocentesis and chorionic villus sampling for prenatal diagnosis. Cochrane Database Syst. Rev. 2017, 2017, CD003252. [Google Scholar] [CrossRef]
- Buchovecky, C.M.; Nahum, O.; Levy, B. Assessment of Maternal Cell Contamination in Prenatal Samples by Quantitative Fluorescent PCR (QF-PCR). Methods Mol. Biol. 2019, 1885, 117–127. [Google Scholar] [CrossRef]
- Athanasiadis, A.P.; Pantazis, K.; Goulis, D.G.; Chatzigeorgiou, K.; Vaitsi, V.; Assimakopoulos, E.; Tzevelekis, F.; Tsalikis, T.; Bontis, J.N. Comparison between 20G and 22G needle for second trimester amniocentesis in terms of technical aspects and short-term complications. Prenat. Diagn. 2009, 29, 761–765. [Google Scholar] [CrossRef]
- Daum, H.; Ben David, A.; Nadjari, M.; Zenvirt, S.; Helman, S.; Yanai, N.; Meiner, V.; Yagel, S.; Frumkin, A.; Rafid, S.S.; et al. Role of late amniocentesis in the era of modern genomic technologies. Ultrasound Obstet. Gynecol. 2019, 53, 676–685. [Google Scholar] [CrossRef]
- Devlieger, R.; Gratacos, E.; Ardon, H.; Vanstraelen, S.; Deprest, J. Factors influencing the flow rate through a surgical defect in human fetal membranes. Prenat. Diagn. 2002, 22, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Hockstein, S.; Chen, P.X.; Thangavelu, M.; Pergament, E. Factors Associated With Maternal Cell Contamination in Amniocentesis Samples as Evaluated by Fluorescent In Situ Hybridization. Obstet. Gynecol. 1998, 92, 551–556. [Google Scholar] [CrossRef] [PubMed]
- Giorlandino, C.; Gambuzza, G.; D’Alessio, P.; Santoro, M.L.; Gentili, P.; Vizzone, A. Blood contamination of amniotic fluid after amniocentesis in relation to placental location. Prenat. Diagn. 1996, 16, 180–182. [Google Scholar] [CrossRef]
- Welch, R.A.; Salem-Elgharib, S.; Wiktor, A.E.; Van Dyke, D.L.; Blessed, W.B. Operator experience and sample quality in genetic amniocentesis. Am. J. Obstet. Gynecol. 2006, 194, 189–191. [Google Scholar] [CrossRef]
- Uludag, S.; Aydin, Y.; Ibrahimova, F.; Madazli, R.; Sen, C. Comparison of complications in second trimester amniocentesis performed with 20G, 21G and 22G needles. J. Périnat. Med. 2010, 38, 597–600. [Google Scholar] [CrossRef]






| Studied Criteria | Contaminated Probes | Uncontaminated Probes | p Value | RE | RN | RR | |
|---|---|---|---|---|---|---|---|
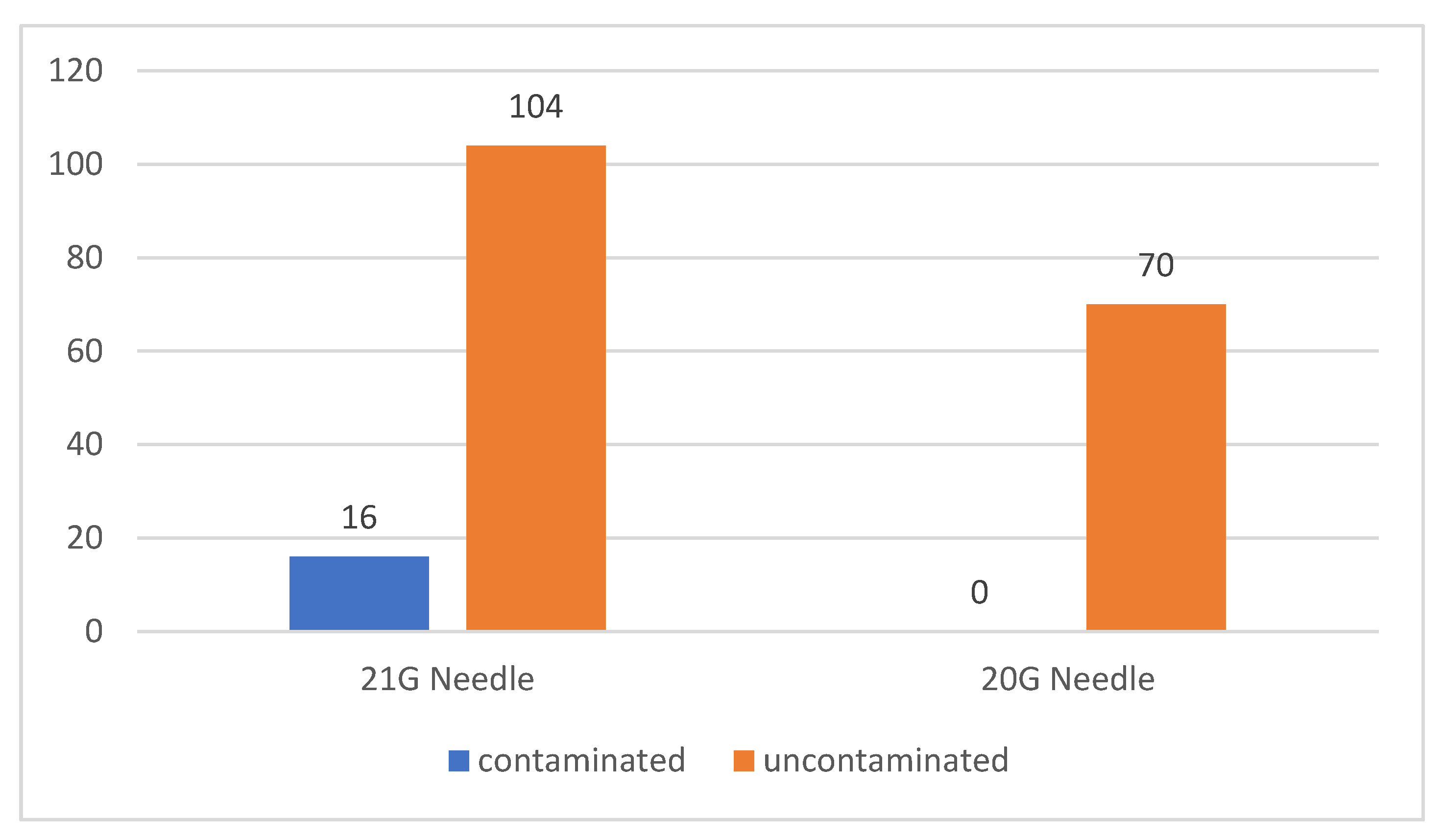
| 21 G Needle | 16 | 104 | 0.0035 | 13.33 | 0 | - | |
| 20 G Needle | 0 | 70 | |||||
| Multiparous | 14 | 102 | 0.0456 | 12.07 | 2.703 | 4.466 | |
| Primiparous | 2 | 72 | |||||
| 21 G needle + anterior placenta | 13 | 67 | 0.0226 | 16.25 | 0 | - | |
| 20 G needle + anterior placenta | 0 | 25 | |||||
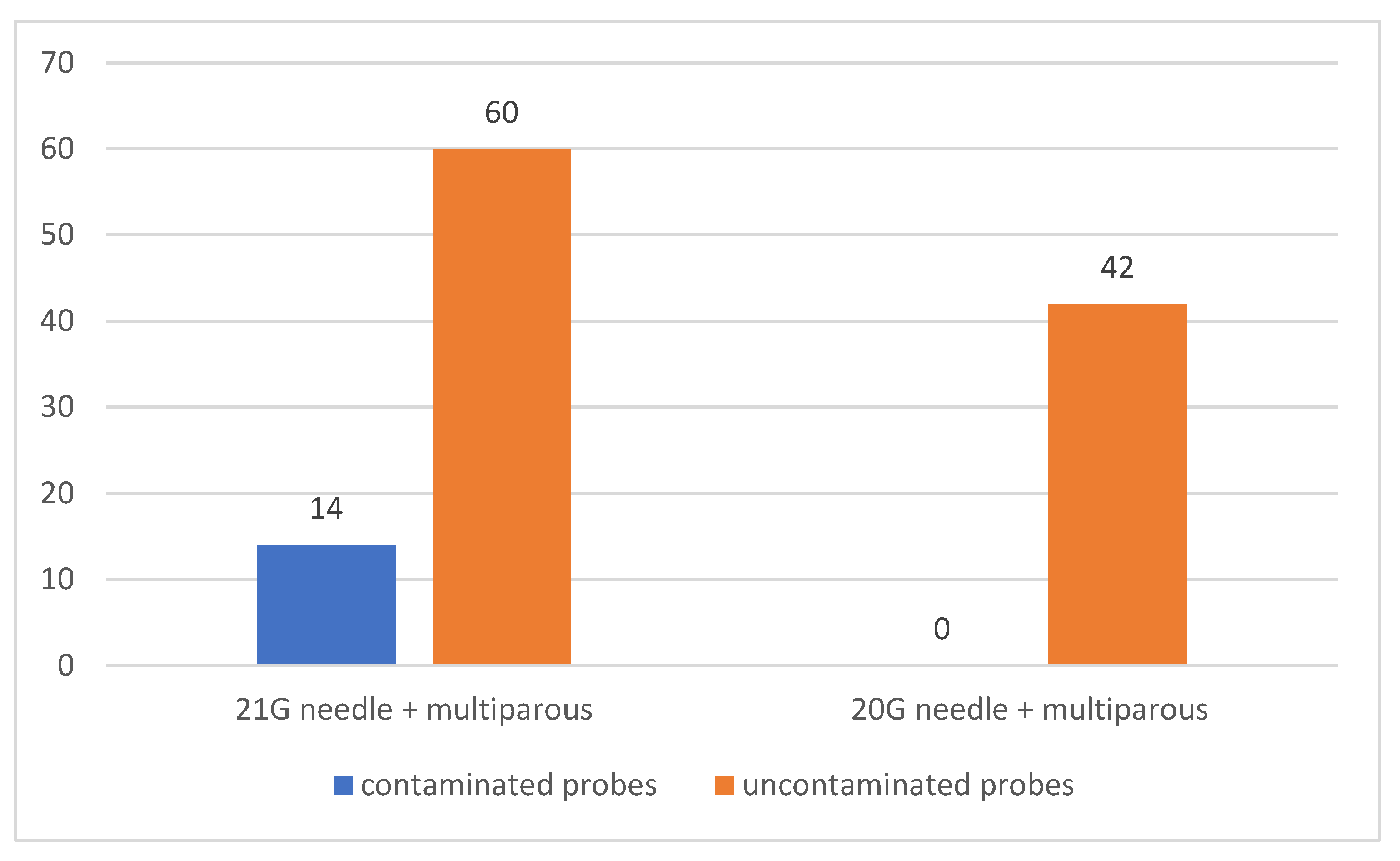
| 21 G needle + multiparous | 14 | 60 | 0.007 | 18.92 | 0 | - | |
| 20 G needle + multiparous | 0 | 42 | |||||
| 21 G needle + multiparous | 14 | 60 | 0.0448 | 18.92 | 4.348 | 4.351 | |
| 21 G needle + primiparous | 2 | 44 | |||||
| 21 G needle + anterior placenta + multiparous | 11 | 38 | 0.0454 | 22.45 | 0 | - | |
| 20 G needle + posterior placenta + primiparous | 0 | 18 | |||||
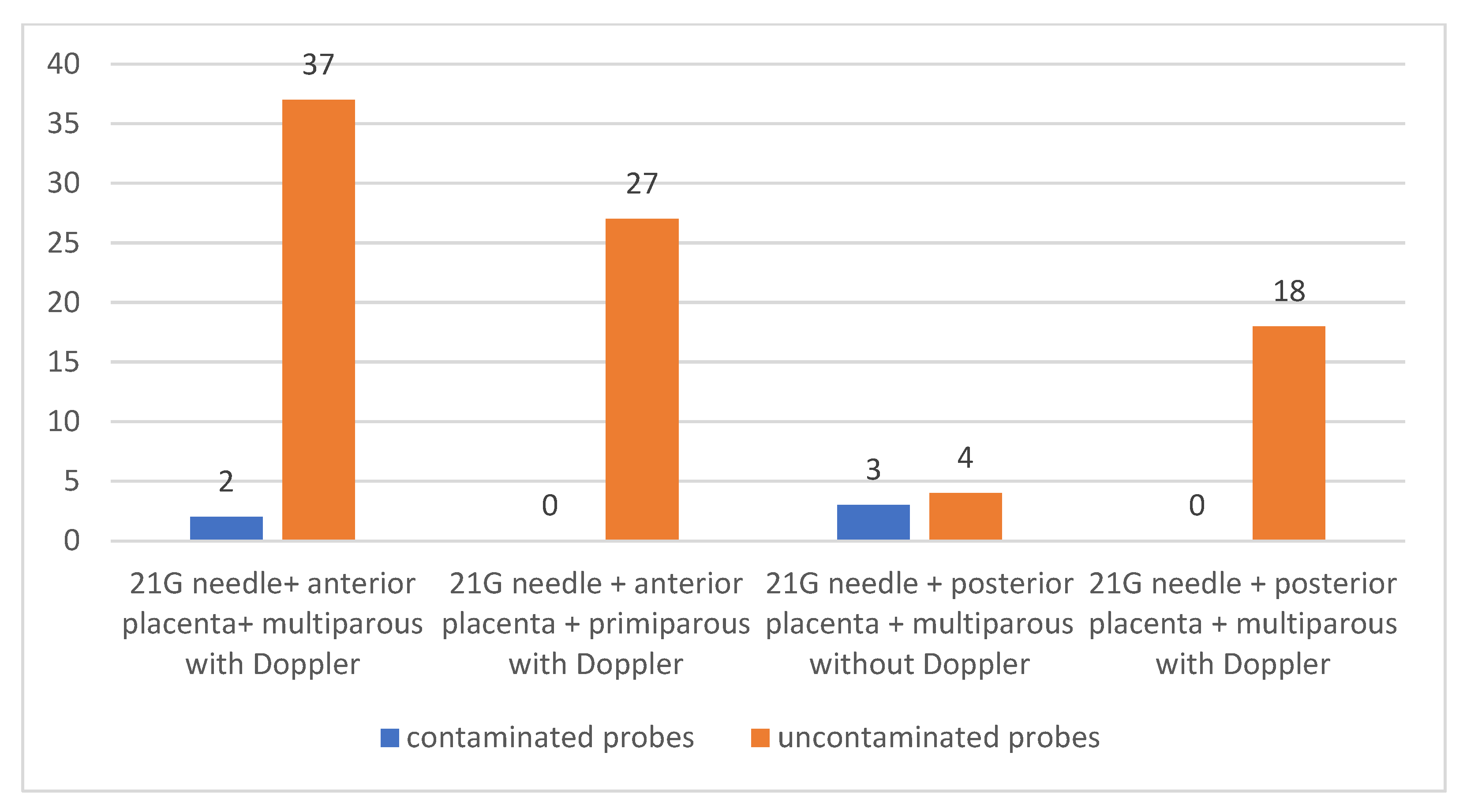
| 21 G needle + anterior placenta + multiparous with Doppler | 37 | 2 | <0.0001 | 94.87 | 10 | 9.487 | |
| 21 G needle + anterior placenta + multiparous without Doppler | 1 | 9 | |||||
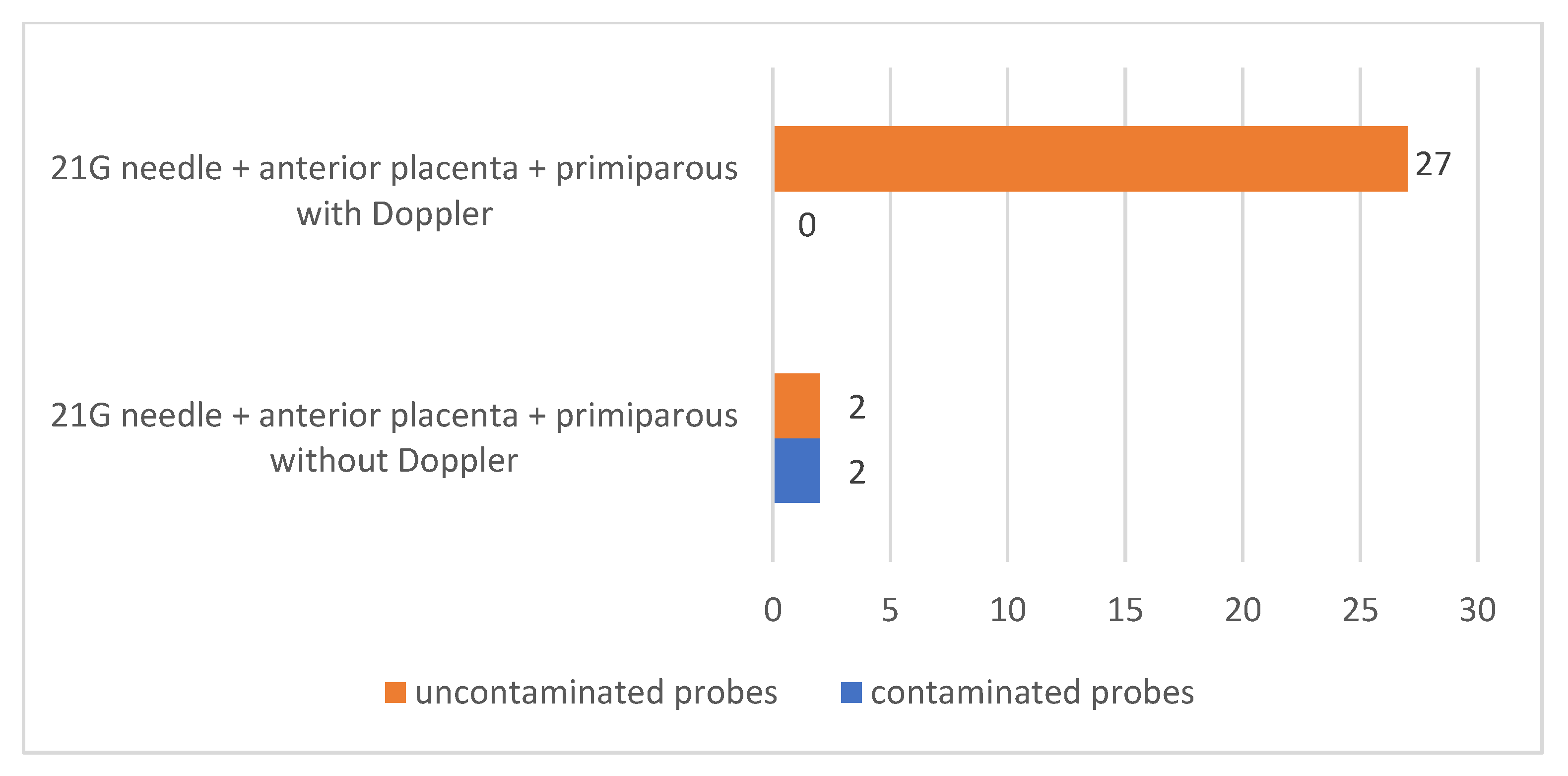
| 21 G needle + anterior placenta + primiparous with Doppler | 27 | 0 | 0.0146 | 100 | 50 | 2 | |
| 21 G needle + anterior placenta + primiparous without Doppler | 2 | 2 | |||||
| 21 G needle + anterior placenta + multiparous with Doppler | 2 | 37 | 0.6909 | 5.128 | 0 | - | |
| 21 G needle + anterior placenta + primiparous with Doppler | 0 | 27 | |||||
| 21 G needle + posterior placenta + multiparous without Doppler | 3 | 4 | 0.0152 | 42.86 | 0 | - | |
| 21 G needle + postrerior placenta + multiparous with Doppler | 0 | 18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciortea, R.; Malutan, A.M.; Bucuri, C.E.; Berceanu, C.; Rada, M.P.; Ormindean, C.M.; Mihu, D. Amniocentesis—When It Is Clear That It Is Not Clear. J. Clin. Med. 2023, 12, 454. https://doi.org/10.3390/jcm12020454
Ciortea R, Malutan AM, Bucuri CE, Berceanu C, Rada MP, Ormindean CM, Mihu D. Amniocentesis—When It Is Clear That It Is Not Clear. Journal of Clinical Medicine. 2023; 12(2):454. https://doi.org/10.3390/jcm12020454
Chicago/Turabian StyleCiortea, Razvan, Andrei Mihai Malutan, Carmen Elena Bucuri, Costin Berceanu, Maria Patricia Rada, Cristina Mihaela Ormindean, and Dan Mihu. 2023. "Amniocentesis—When It Is Clear That It Is Not Clear" Journal of Clinical Medicine 12, no. 2: 454. https://doi.org/10.3390/jcm12020454
APA StyleCiortea, R., Malutan, A. M., Bucuri, C. E., Berceanu, C., Rada, M. P., Ormindean, C. M., & Mihu, D. (2023). Amniocentesis—When It Is Clear That It Is Not Clear. Journal of Clinical Medicine, 12(2), 454. https://doi.org/10.3390/jcm12020454





