Nutritional Issues Faced by Patients with Intestinal Stoma: A Narrative Review
Abstract
:1. Introduction
2. Methods
3. Nutrition Issues
3.1. The Risk of Developing Malnutrition or Nutrient Deficiencies in Patients with a Stoma and How to Monitor Malnutrition in Surgical Patients
3.1.1. Pre-Operative Period and Tools for Diagnosis of Malnutrition at Different Stages (Patient Preparation and Hospital Care of Surgical Patients, including Those with a Stoma)
3.1.2. Immediate Post-Operative Period
3.1.3. Delayed Post-Operative Period
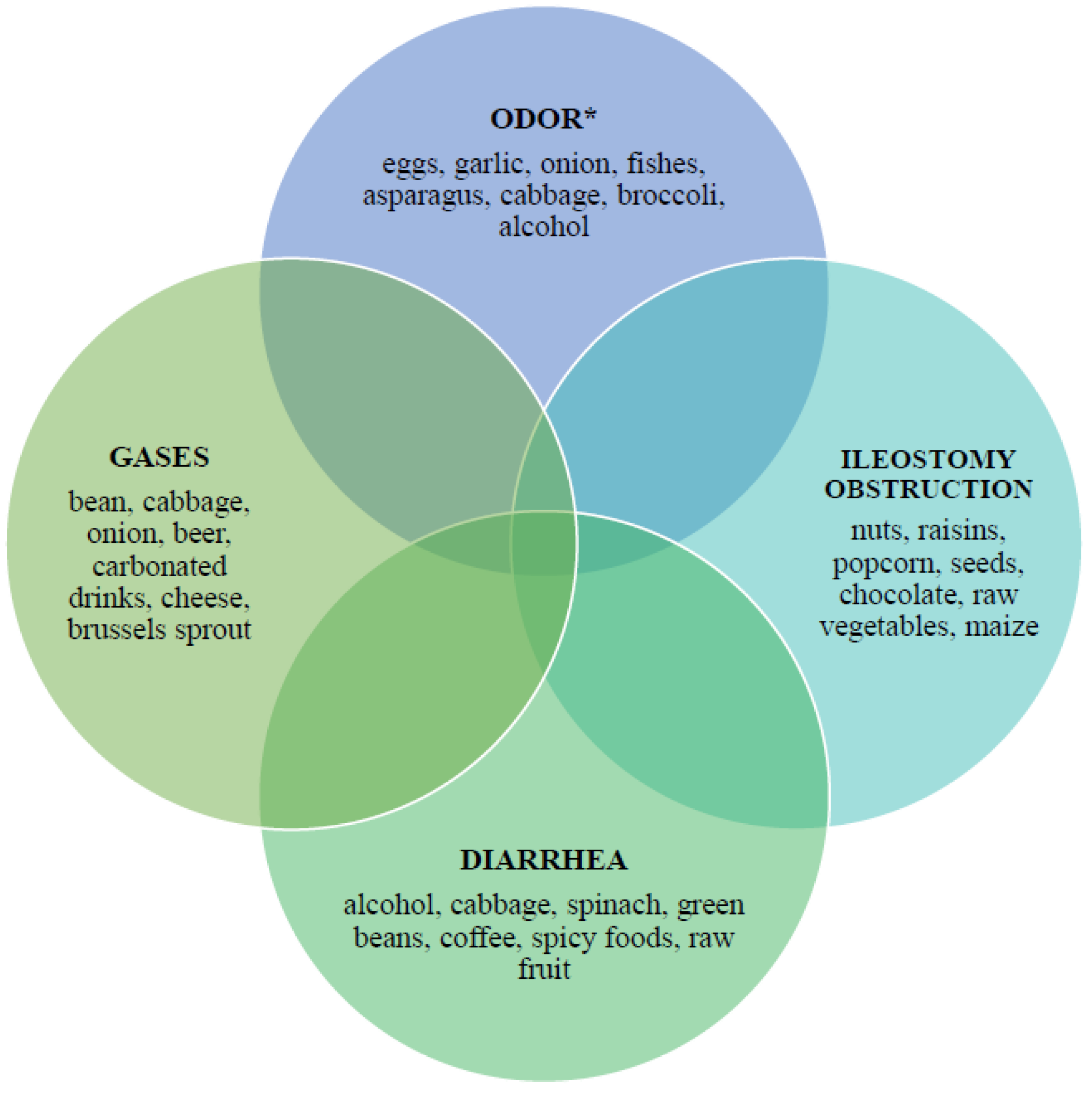
3.2. Ileostomy
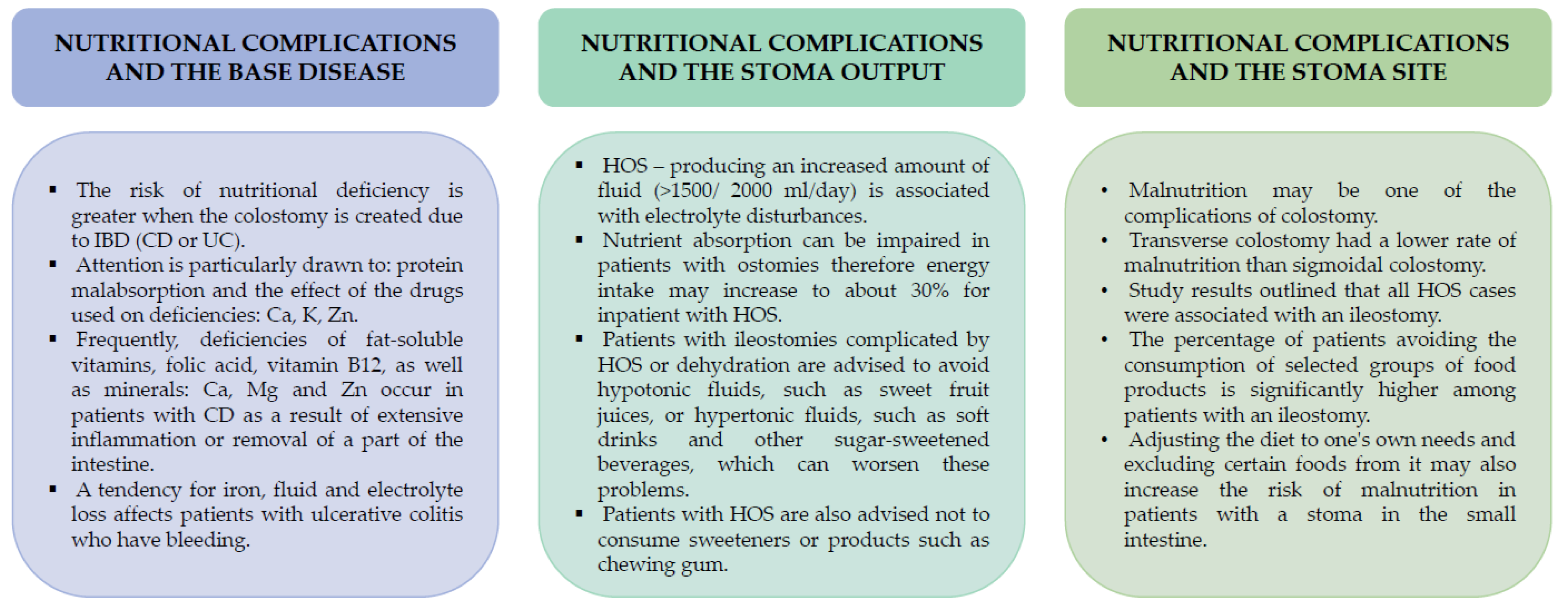
3.3. Colostomy
3.4. Demand for Energy, Macronutrients, Vitamins, and Micronutrients
3.5. Recommendations to Prevent Complications and Deficiencies
3.6. Nutrition Consultation and Education as a Tool for Effective Protection against Complications
3.7. Basic Nutritional Guidelines for an Intestinal Stoma
4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ellis, H.; Calne, S.R.; Watson, C. General Surgery, 13th ed.; Wiley: New York, NY, USA, 2016; pp. 209, 187, 191, 217–219. [Google Scholar]
- Baiu, I.; Spain, D.A. Enteral Nutrition. JAMA 2019, 321, 2040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burch, J. Nutrition for people with stomas. 2: An overview of dietary advice. Nurs. Times 2008, 104, 26–27. [Google Scholar]
- Everhov, H.; Kalman, T.D.; Söderling, J.; Nordenvall, C.; Halfvarson, J.; Ekbom, A.; Ludvigsson, J.F.; Olén, O.; Myrelid, P. Probability of Stoma in Incident Patients With Crohn’s Disease in Sweden 2003-2019: A Population-based Study. Inflamm. Bowel Dis. 2021, 28, 1160–1168. [Google Scholar] [CrossRef] [PubMed]
- Arumugam, P.J.; Bevan, L.; Macdonald, L.; Watkins, A.; Morgan, A.R.; Beynon, J.; Carr, N.D. A prospective audit of stomas-analysis of risk factors and complications and their management. Color. Dis. 2003, 5, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.Y.; Stem, M.; Cerullo, M.; Canner, J.K.; Gearhart, S.L.; Safar, B.; Fang, S.H.; Efron, J.E. Predicting the Risk of Readmission from Dehydration After Ileostomy Formation: The Dehydration Readmission After Ileostomy Prediction Score. Dis. Colon Rectum 2018, 61, 1410–1417. [Google Scholar] [CrossRef] [PubMed]
- Schiergens, T.S.; Hoffmann, V.; Schobel, T.N.; Englert, G.H.; Kreis, M.E.; Thasler, W.E.; Werner, J.; Kasparek, M.S. Long-term Quality of Life of Patients with Permanent End Ileostomy: Results of a Nationwide Cross-Sectional Survey. Dis. Colon Rectum 2017, 60, 51–60. [Google Scholar] [CrossRef]
- Fulham, J. Providing dietary advice for the individual with a stoma. Br. J. Nurs. 2008, 17, S22–S27. [Google Scholar] [CrossRef] [PubMed]
- Arnott, S.M.; Zollinger, B.; Haviland, S.; Ng, M.; Obias, V. A nutritional screening threshold for optimal outcomes after Hartmann’s reversal. Int. J. Color. Dis. 2022, 37, 2041–2048. [Google Scholar] [CrossRef]
- Elia, M. The MUST Report: Nutritional Screening for Adults: A Multidisciplinary Responsibility; BAPEN: Maidenhead, UK, 2003; pp. 1–6, 13–19. [Google Scholar]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. J. Cachexia Sarcopenia Muscle 2019, 10, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Wischmeyer, P.E.; Carli, F.; Evans, D.; Guilbert, S.; Kozar, R.; Pryor, A.; Thiele, R.H.; Everett, S.; Grocott, M.; Gan, T.J.; et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Nutrition Screening and Therapy Within a Surgical Enhanced Recovery Pathway. Obstet. Anesthesia Dig. 2018, 126, 1883–1895. [Google Scholar] [CrossRef]
- Santamaría, M.M.; Villafranca, J.J.A.; Abilés, J.; Ruiz, F.R.; Navarro, P.U.; Goitia, B.T. Impact of a nutrition consultation on the rate of high output stoma-related readmission: An ambispective cohort study. Sci. Rep. 2021, 11, 16620–16627. [Google Scholar] [CrossRef] [PubMed]
- Vasilopoulos, G.; Makrigianni, P.; Polikandrioti, M.; Tsiampouris, I.; Karayiannis, D.; Margari, N.; Avramopoulou, L.; Toulia, G.; Fasoi, G. Pre- and Post-Operative Nutrition Assessment in Patients with Colon Cancer Undergoing Ileostomy. Int. J. Environ. Res. Public Health 2020, 17, 6124. [Google Scholar] [CrossRef] [PubMed]
- Gropper, S.; Smith, J.L.; Groff, J.L. The digestive system: Mechanism for nourishing the body. In Advanced Nutrition and Human Nutrition, 5th ed.; Gropper, S., Smith, J.L., Groff, J.L., Eds.; Cengage Learning: Wadsworth, OH, USA, 2009; pp. 43–45, 51, 53–55. [Google Scholar]
- Mukhopadhyay, A. Can Postoperative Nutrition be Favourably Maintained by Oral Diet in Patients with Emergency Temporary Ileostomy? A Tertiary Hospital Based Study. J. Clin. Diagn. Res. 2015, 9, PC04–PC08. [Google Scholar] [CrossRef] [PubMed]
- Fulham, J. Improving the nutritional status of colorectal surgical and stoma patients. Br. J. Nurs. 2004, 13, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Cerantola, Y.; Grass, F.; Cristaudi, A.; Demartines, N.; Schäfer, M.; Hübner, M. Perioperative Nutrition in Abdominal Surgery: Recommendations and Reality. Gastroenterol. Res. Pract. 2011, 2011, 739347. [Google Scholar] [CrossRef] [Green Version]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- De Olieira, A.L.; Moreira, A.P.B.; Netto, M.P.; Leite, I.C.G. A Cross-sectional Study of Nutritional Status, Diet, and Dietary Restrictions Among Persons with an Ileostomy or Colostomy. J. Wound, Ostomy Cont. Nurs. 2018, 64, 18–29. [Google Scholar] [CrossRef]
- Pan, Y.; Liu, Y.; Guo, H.; Jabir, M.S.; Liu, X.; Cui, W.; Li, D. Associations between Folate and Vitamin B12 Levels and Inflammatory Bowel Disease: A Meta-Analysis. Nutrients 2017, 9, 382. [Google Scholar] [CrossRef]
- Villafranca, J.J.A.; López-Rodríguez, C.; Abilés, J.; Rivera, R.; Adán, N.G.; Navarro, P.U. Protocol for the detection and nutritional management of high-output stomas. Nutr. J. 2015, 14, 45. [Google Scholar] [CrossRef] [Green Version]
- Medlin, S. Nutritional and fluid requirements: High-output stomas. Br. J. Nurs. 2012, 21, S22–S25. [Google Scholar] [CrossRef]
- Fabisiak, N.; Fabisiak, A.; Watala, C.; Fichna, J. Fat-soluble Vitamin Deficiencies and Inflammatory Bowel Disease. J. Clin. Gastroenterol. 2017, 51, 878–889. [Google Scholar] [CrossRef] [PubMed]
- Aksan, A.; Işık, H.; Radeke, H.H.; Dignass, A.; Stein, J. Systematic review with network meta-analysis: Comparative efficacy and tolerability of different intravenous iron formulations for the treatment of iron deficiency anaemia in patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2017, 45, 1303–1318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandramouli, B.; Srinivasan, K.; Jagdish, S.; Ananthakrishnan, N. Morbidity and mortality of colostomy and its closure in children. J. Pediatr. Surg. 2004, 39, 596–599. [Google Scholar] [CrossRef] [PubMed]
- Migdanis, A.; Koukoulis, G.; Mamaloudis, I.; Baloyiannis, I.; Migdanis, I.; Vagena, X.; Malissiova, E.; Tzovaras, G. The effect of a diverting ileostomy formation on nutritional status and energy intake of patients undergoing colorectal surgery. Clin. Nutr. ESPEN 2020, 40, 357–362. [Google Scholar] [CrossRef]
- Ellegård, L.; Andersson, H. Oat bran rapidly increases bile acid excretion and bile acid synthesis: An ileostomy study. Eur. J. Clin. Nutr. 2007, 61, 938–945. [Google Scholar] [CrossRef] [Green Version]
- Ellegård, L.; Bosaeus, I.; Andersson, H. Will recommended changes in fat and fibre intake affect cholesterol absorption and sterol excretion? An ileostomy study. Eur. J. Clin. Nutr. 2000, 54, 306–313. [Google Scholar] [CrossRef] [Green Version]
- Ellegård, L.; Andersson, H.; Bosaeus, I. Rapeseed oil, olive oil, plant sterols, and cholesterol metabolism: An ileostomy study. Eur. J. Clin. Nutr. 2005, 59, 1374–1378. [Google Scholar] [CrossRef] [Green Version]
- Mountford, C.G.; Manas, D.M.; Thompson, N.P. A practical approach to the management of high-output stoma. Front. Gastroenterol. 2013, 5, 203–207. [Google Scholar] [CrossRef] [Green Version]
- Barrett, J.S.; Gearry, R.; Muir, J.G.; Irving, P.M.; Rose, R.; Rosella, O.; Haines, M.L.; Shepherd, S.J.; Gibson, P.R. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment. Pharmacol. Ther. 2010, 31, 874–882. [Google Scholar] [CrossRef]
- Burch, J. Nutrition and the ostomate: Input, output and absorption. Br. J. Community Nurs. 2006, 11, 349–351. [Google Scholar] [CrossRef]
- Gupta, S.; Shen, B. Bone loss in patients with the ileostomy and ileal pouch for inflammatory bowel disease. Gastroenterol. Rep. 2013, 1, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Wu, X.; Moore, T.; Shen, B. Frequency, Risk Factors, and Adverse Sequelae of Bone Loss in Patients with Ostomy for Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2014, 20, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Mantle, D. Nutritional supplementation for vitamin B12 and vitamin K2 deficiency following ileostomy or colostomy formation. Gastrointest. Nurs. 2020, 18, S12–S16. [Google Scholar] [CrossRef]
- Burch, J. Providing information and advice on diet to stoma patients. Br. J. Community Nurs. 2011, 16, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Chiavaroli, L.; Viguiliouk, E.; Nishi, S.K.; Mejia, S.B.; Rahelić, D.; Kahleova, H.; Salas-Salvadó, J.; Kendall, C.W.C.; Sievenpiper, J.L. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients 2019, 11, 338. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, A.K.N.; Rud, C.; Wilkens, T.L.; Borre, M.; Andersen, J.R.; Dahlerup, J.F.; Hvas, C.L. A Single Urine Sodium Measurement May Validly Estimate 24-hour Urine Sodium Excretion in Patients with an Ileostomy. J. Parenter. Enter. Nutr. 2019, 44, 246–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, D.G.; Nadeau, J. Oral rehydration solution: A “low-tech” oft neglected therapy. Pract. Gastro 2004, 28, 51–62. [Google Scholar]
- University of Pittsburgh Medical Center Web site. Available online: https://www.upmc.com/health-library/article?hwid=ug2186 (accessed on 31 October 2022).
- Fernández-Gálvez, A.; Rivera, S.; Ventura, M.D.C.D.; de la Osa, R.M.R. Nutritional and Educational Intervention to Recover a Healthy Eating Pattern Reducing Clinical Ileostomy-Related Complications. Nutrients 2022, 14, 3431. [Google Scholar] [CrossRef]
- Messaris, E.; Sehgal, R.; Deiling, S.; Koltun, W.A.; Stewart, D.; McKenna, K.; Poritz, L.S. Dehydration Is the Most Common Indication for Readmission After Diverting Ileostomy Creation. Dis. Colon Rectum 2012, 55, 175–180. [Google Scholar] [CrossRef]
- Iqbal, A.; Sakharuk, I.; Goldstein, L.; Tan, S.A.; Qiu, P.; Li, Z.; Hughes, S.J. Readmission After Elective Ileostomy in Colorectal Surgery Is Predictable. JSLS J. Soc. Laparosc. Robot. Surg. 2018, 22, e2018.00008. [Google Scholar] [CrossRef] [Green Version]
- Fish, D.R.; Mancuso, C.A.; Garcia-Aguilar, J.E.; Lee, S.W.; Nash, G.M.; Sonoda, T.; Charlson, M.E.; Temple, L.K. Readmission After Ileostomy Creation. Ann. Surg. 2017, 265, 379–387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qu, L.; Zhou, M.; Yu, Y.; Li, K. Effects of Nutritious Meal Combined with Online Publicity and Education on Postoperative Nutrition and Psychological State in Patients with Low Rectal Cancer After Colostomy. Comput. Math. Methods Med. 2022, 2022, 1541385. [Google Scholar] [CrossRef] [PubMed]
- Akbulut, G. Nutrition in Stoma Patients: A Practical View of Dietary Therapy. Int. J. Hematol. Oncol. 2011, 21, 61–66. [Google Scholar] [CrossRef]
- Toledano, S.; Sackey, J.; Willcutts, K.; Parrott, J.S.; Tomesko, J.; Al-Mazrou, A.M.; Kiran, R.P.; Brody, R.A. Exploring the Differences Between Early and Traditional Diet Advancement in Postoperative Feeding Outcomes in Patients with an Ileostomy or Colostomy. Nutr. Clin. Pract. 2019, 34, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Fujii, T.; Morita, H.; Sutoh, T.; Yajima, R.; Yamaguchi, S.; Tsutsumi, S.; Asao, T.; Kuwano, H. Benefit of Oral Feeding as Early as One Day After Elective Surgery for Colorectal Cancer: Oral Feeding on First Versus Second Postoperative Day. Int. Surg. 2014, 99, 211–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrelli, N.J.; Cheng, C.; Driscoll, D.; Rodriguez-Bigas, M.A. Early Postoperative Oral Feeding After Colectomy: An Analysis of Factors That May Predict Failure. Ann. Surg. Oncol. 2001, 8, 796–800. [Google Scholar] [CrossRef] [PubMed]

| Part of the Gastrointestinal Tract | Absorbed Nutrients |
|---|---|
| Stomach | water, ethyl alcohol, copper, iodine, fluoride, molybdenum |
| Duodenum | calcium, phosphorus, magnesium, iron, copper, selenium, thiamin, riboflavin, niacin, biotin, folate, vitamins A, D, E, and K |
| Jejunum | lipids, monosaccharides, amino acids, small peptides, thiamin, riboflavin, niacin, pantothenate, biotin, folate, vitamin B6, vitamin C, vitamins A, D, E, and K, calcium, phosphorus, magnesium, iron, zinc, chromium, manganese, molybdenum, |
| Ileum | vitamin C, folate, vitamin B12, vitamin D, vitamin K, magnesium, others *, bile salts and acids |
| Large intestine | water, vitamin K, biotin, sodium, chloride, potassium, short-chain fatty acids |
| Types of Ostomies | Summary of Nutrition Recommendations |
|---|---|
| Ileostomy | Avoiding products like popcorn, nuts, seeds, raisins, etc., as they can block stoma. Proper hydration is crucial to prevent excessive secretion and fluid disorders. Parenteral nutrition may be necessary due to the higher risk of nutritional deficiencies. Extending the diet after surgery should be done carefully and individually. This will allow easy detection and exclusion of harmful products for patients. |
| Colostomy | The diet does not deviate from the principles of a healthy and balanced diet recommended for healthy people. For possible constipation problems, plenty of exercise and a greater supply of food rich in insoluble fibre fractions, such as whole-grain bread, dark pasta and brown rice are recommended. |
| Both | The diet should be individually selected to meet the needs of the patient and be varied and rich in vitamins and minerals. The basis of the diet should be fresh products and foods and possibly without preservatives and artificial food dyes. The recommended form of food processing is cooking (traditional or steaming), possibly baking in foil and it is recommended to avoid fried, baked and stewed foods after frying. Products that should be avoided or consumed in limited quantities are alcohol (especially beer), sweets (especially chocolate and its products), carbohydrate drinks, egg yolk, salt and hot spices. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michońska, I.; Polak-Szczybyło, E.; Sokal, A.; Jarmakiewicz-Czaja, S.; Stępień, A.E.; Dereń, K. Nutritional Issues Faced by Patients with Intestinal Stoma: A Narrative Review. J. Clin. Med. 2023, 12, 510. https://doi.org/10.3390/jcm12020510
Michońska I, Polak-Szczybyło E, Sokal A, Jarmakiewicz-Czaja S, Stępień AE, Dereń K. Nutritional Issues Faced by Patients with Intestinal Stoma: A Narrative Review. Journal of Clinical Medicine. 2023; 12(2):510. https://doi.org/10.3390/jcm12020510
Chicago/Turabian StyleMichońska, Izabela, Ewelina Polak-Szczybyło, Aneta Sokal, Sara Jarmakiewicz-Czaja, Agnieszka Ewa Stępień, and Katarzyna Dereń. 2023. "Nutritional Issues Faced by Patients with Intestinal Stoma: A Narrative Review" Journal of Clinical Medicine 12, no. 2: 510. https://doi.org/10.3390/jcm12020510
APA StyleMichońska, I., Polak-Szczybyło, E., Sokal, A., Jarmakiewicz-Czaja, S., Stępień, A. E., & Dereń, K. (2023). Nutritional Issues Faced by Patients with Intestinal Stoma: A Narrative Review. Journal of Clinical Medicine, 12(2), 510. https://doi.org/10.3390/jcm12020510







