Surgical Management of Scapulothoracic Bursitis in a Patient with Systemic Lupus Erythematosus: A Case Report
Abstract
:1. Introduction
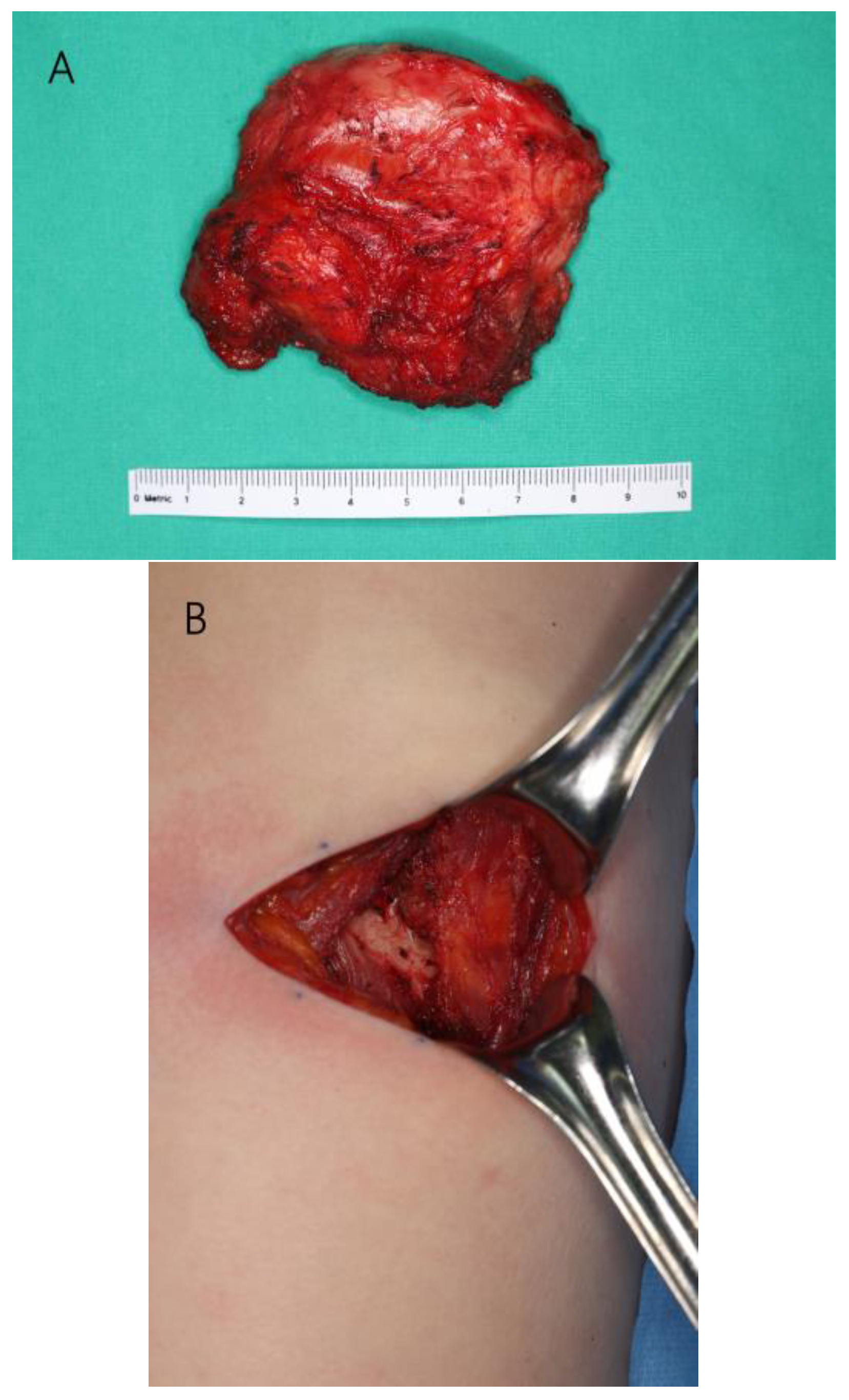
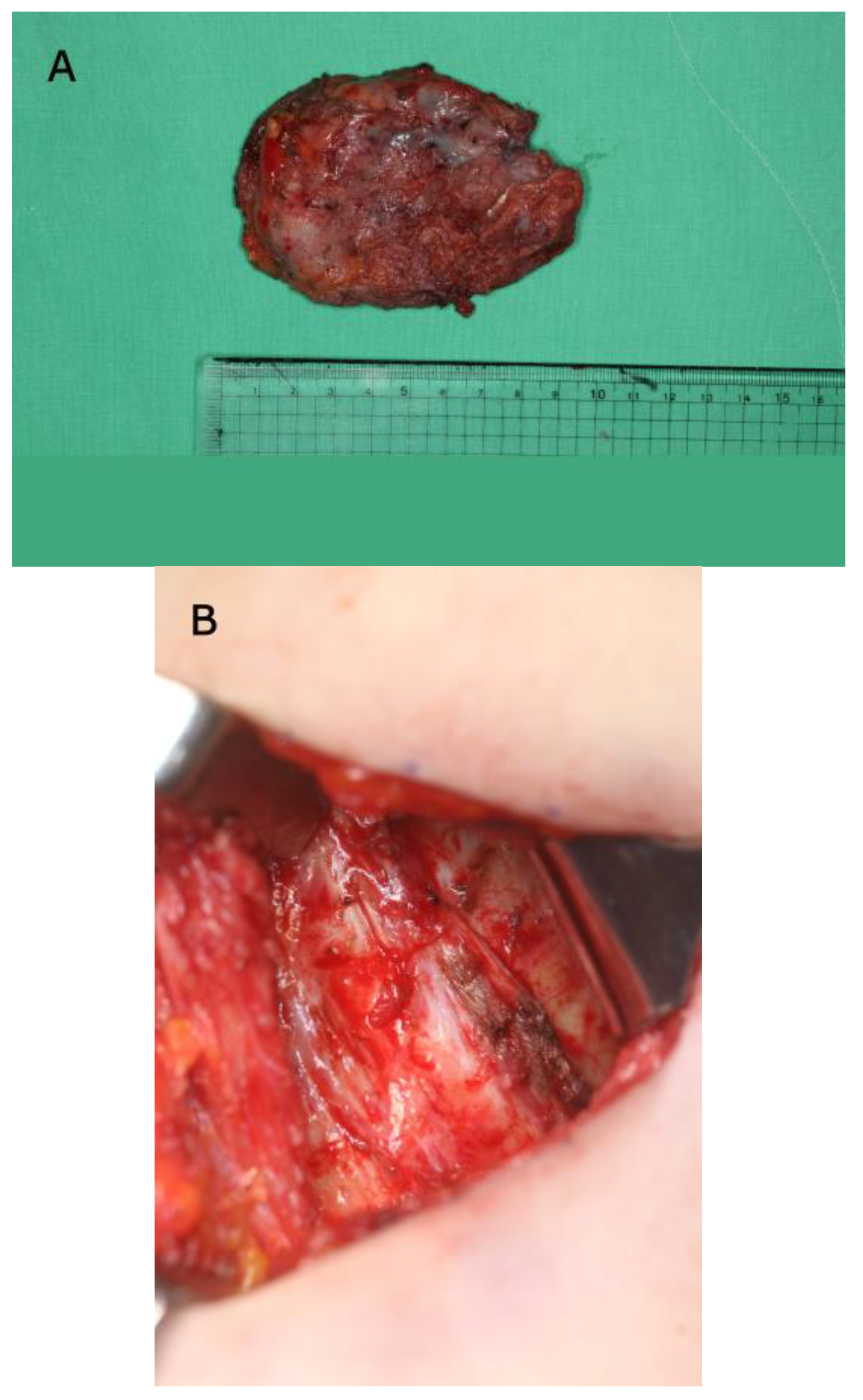
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Kibler, W.B. The role of the scapula in athletic shoulder function. Am. J. Sports Med. 1998, 26, 325–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuhn, J.E.; Plancher, K.D.; Hawkins, R.J. Symptomatic scapulothoracic crepitus and bursitis. J. Am. Acad. Orthop. Surg. 1998, 6, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Warth, R.J.; Spiegl, U.J.; Millett, P.J. Scapulothoracic bursitis and snapping scapula syndrome: A critical review of current evidence. Am. J. Sports Med. 2015, 43, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Schiavon, F.; Ragazzi, R. Bilateral scapulothoracic bursitis. Arthritis Rheumatol. 2008, 58, 585. [Google Scholar] [CrossRef] [PubMed]
- Conduah, A.H.; Baker, C.L., 3rd; Baker, C.L., Jr. Clinical management of scapulothoracic bursitis and the snapping scapula. Sports Health 2010, 2, 147–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, J.Y.; Seo, J.H.; Cha, W.J.; Seo, B.F.; Jung, S.N. A propeller superficial transverse cervical artery perforator flap for defect coverage of the submental area: A case report. Arch. Craniofac. Surg. 2021, 22, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.L.; Miller, A.J.; Ballard, B.L.; Botte, M.J. Management of Snapping Scapula Syndrome. Orthopedics 2016, 39, e783–e786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lambie, P.; Kaufman, R.; Beardmore, T. Septic ischial bursitis in systemic lupus erythematosus presenting as a perirectal mass. J. Rheumatol. 1989, 16, 1497–1499. [Google Scholar] [PubMed]
- Thong, B.; Olsen, N.J. Systemic lupus erythematosus diagnosis and management. Rheumatology 2017, 56 (Suppl. 1), i3–i13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ruperto, N.; Hanrahan, L.M.; Alarcón, G.S.; Belmont, H.M.; Brey, R.L.; Brunetta, P.; Buyon, J.P.; Costner, M.I.; Cronin, M.E.; Dooley, M.A.; et al. International consensus for a definition of disease flare in lupus. Lupus 2011, 20, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Ricci, V.; Chang, K.V.; Güvener, O.; Mezian, K.; Kara, M.; Leblebicioğlu, G.; Stecco, C.; Pirri, C.; Ata, A.M.; Dughbaj, M.; et al. EURO-MUSCULUS/USPRM Dynamic Ultrasound Protocols for Shoulder. Am. J. Phys. Med. Rehabil. 2022, 101, e29–e36. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.H.; Choi, S.Y.; Kim, K.S.; Hwang, J.H.; Lee, S.Y. Surgical Management of Scapulothoracic Bursitis in a Patient with Systemic Lupus Erythematosus: A Case Report. J. Clin. Med. 2023, 12, 561. https://doi.org/10.3390/jcm12020561
Choi JH, Choi SY, Kim KS, Hwang JH, Lee SY. Surgical Management of Scapulothoracic Bursitis in a Patient with Systemic Lupus Erythematosus: A Case Report. Journal of Clinical Medicine. 2023; 12(2):561. https://doi.org/10.3390/jcm12020561
Chicago/Turabian StyleChoi, Jun Ho, Seung Yeon Choi, Kwang Seog Kim, Jae Ha Hwang, and Sam Yong Lee. 2023. "Surgical Management of Scapulothoracic Bursitis in a Patient with Systemic Lupus Erythematosus: A Case Report" Journal of Clinical Medicine 12, no. 2: 561. https://doi.org/10.3390/jcm12020561
APA StyleChoi, J. H., Choi, S. Y., Kim, K. S., Hwang, J. H., & Lee, S. Y. (2023). Surgical Management of Scapulothoracic Bursitis in a Patient with Systemic Lupus Erythematosus: A Case Report. Journal of Clinical Medicine, 12(2), 561. https://doi.org/10.3390/jcm12020561





