Factors Associating with Non-Dipping Pattern of Nocturnal Blood Pressure in Patients with Essential Hypertension
Abstract
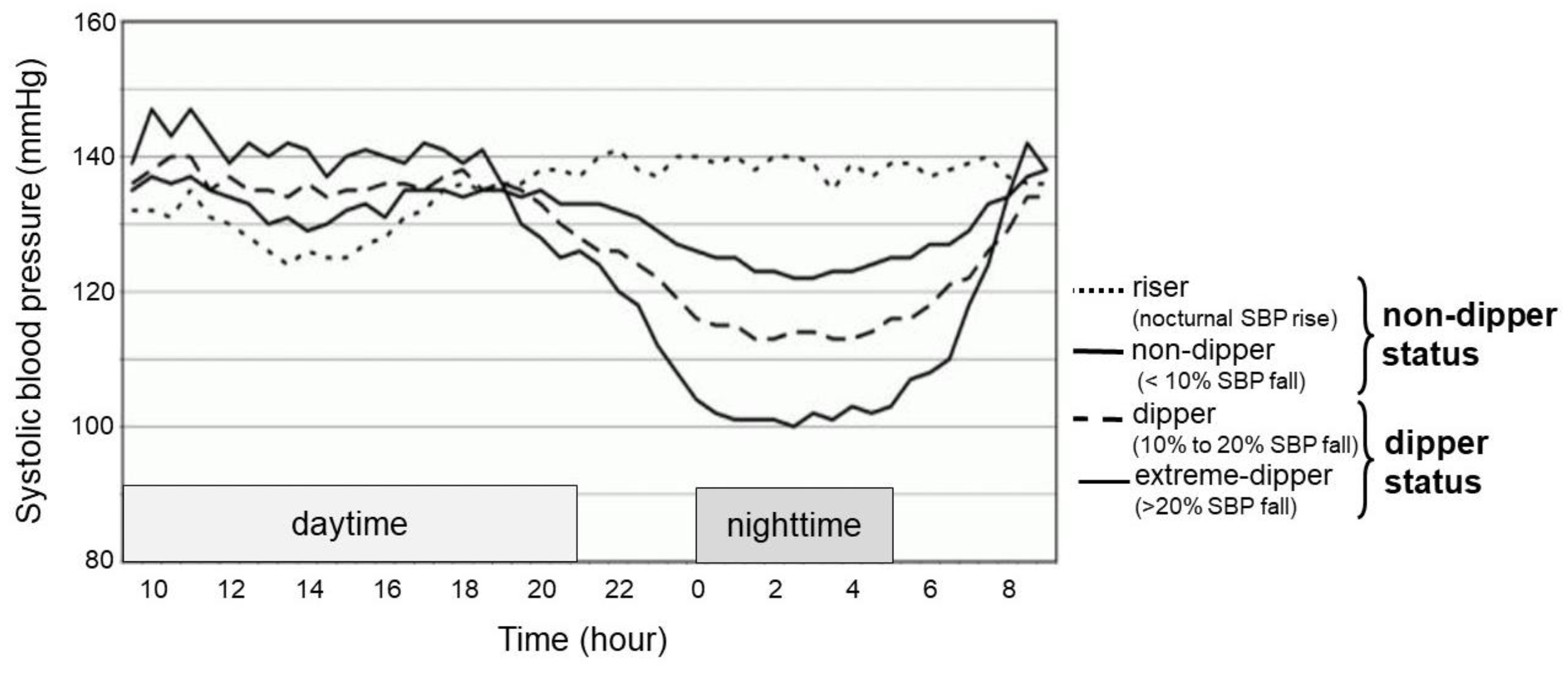
1. Background
2. Methods
2.1. Patient Selection
2.2. Collected Data
2.3. Primary and Secondary Concerns
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Factors Associated with Non-Dipper Status
3.3. Factors Associated with Systolic Blood Pressure among Those with Non-Dipper Status
4. Discussion
4.1. Hyperuricemia and Non-Dipper Status
4.2. Chronic Inflammation and Further Incremental Blood Pressure
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Pickering, T.G. Recommendations for the use of home (self) and ambulatory blood pressure monitoring. Am. J. Hypertens. 1995, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Staessen, J.A.; Thijs, L.; Fagard, R.; O’Brien, E.T.; Clement, D.; de Leeuw, P.W.; Mancia, G.; Nachev, C.; Palatini, P.; Parati, G.; et al. Predicting cardiovascular risk using conventional vs. ambulatory blood pressure in older patients with systolic hypertension. JAMA 1999, 282, 539–546. [Google Scholar] [CrossRef]
- Shimada, K.; Kawamoto, A.; Matsubayashi, K.; Nishinaga, M.; Kimura, S.; Ozawa, T. Diurnal blood pressure variations and silent cerebrovascular damage in elderly patients with hypertension. J. Hypertens. 1992, 10, 875–878. [Google Scholar]
- Hoshide, S.; Kario, K.; Hoshide, Y.; Umeda, Y.; Hashimoto, T.; Kunii, O.; Ojima, T.; Shimada, K. Associations between nondipping of nocturnal blood pressure decrease and cardiovascular target organ damage in strictly selected community-dwelling normotensives. Am. J. Hypertens. 2003, 16, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Davidson, M.B.; Hix, J.K.; Vidt, D.G.; Brotman, D.J. Association of impaired diurnal blood pressure variation with a subsequent decline in glomerular filtration rate. Arch. Intern. Med. 2006, 166, 846–852. [Google Scholar] [CrossRef]
- Kario, K.; Pickering, T.G.; Matsuo, T.; Hoshide, S.; Schwartz, J.E.; Shimada, K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension 2001, 38, 852–857. [Google Scholar] [CrossRef]
- Ohkubo, T.; Hozawa, A.; Yamaguchi, J.; Kikuya, M.; Ohmori, K.; Michimata, M.; Matsubara, M.; Hashimoto, J.; Hoshi, H.; Araki, T.; et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: The Ohasama study. J. Hypertens. 2002, 20, 2183–2189. [Google Scholar] [CrossRef]
- Turak, O.; Özcan, F.; Tok, D.; İşleyen, A.; Sökmen, E.; Taşoğlu, I.; Aydoğdu, S.; Sen, N.; McFann, K.; Johnson, R.J.; et al. Serum Uric Acid, Inflammation, and nondipping circadian pattern in essential hypertension. J. Clin. Hypertens 2013, 15, 7–13. [Google Scholar] [CrossRef]
- Erden, M.; Kocaman, S.A.; Poyraz, F.; Topal, S.; Sahinarslan, A.; Boyacı, B.; Cengel, A.; Yalçın, M.R. Incremental effects of serum uric acid levels, autonomic dysfunction, and low-grade inflammation on nocturnal blood pressure in untreated hypertensive patients and normotensive individuals. Turk Kardiyol. Dern. Ars. 2011, 39, 531–539. [Google Scholar] [CrossRef][Green Version]
- Umemura, S.; Arima, H.; Arima, S.; Asayama, K.; Dohi, Y.; Hirooka, Y.; Horio, T.; Hoshide, S.; Ikeda, S.; Ishimitsu, T.; et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens. Res. 2019, 42, 1235–1481. [Google Scholar] [CrossRef] [PubMed]
- Kansui, Y.; Matsumura, K.; Morinaga, Y.; Inoue, M.; Kiyohara, K.; Ohta, Y.; Goto, K.; Ohtsubo, T.; Ooboshi, H.; Kitazono, T. Impact of serum uric acid on incident hypertension in a worksite population of Japanese men. J. Hypertens. 2018, 36, 1499–1505. [Google Scholar] [CrossRef]
- Reboldi, G.; Verdecchia, P.; Saladini, F.; Pane, M.; Beilin, L.J.; Eguchi, K.; Imai, Y.; Kario, K.; Ohkubo, T.; Pierdomenico, S.D.; et al. Added predictive value of high uric acid for cardiovascular events in the Ambulatory Blood Pressure International Study. J. Clin. Hypertens. 2019, 21, 966–974. [Google Scholar] [CrossRef]
- Berni, A.; Bodd, M.; Fattori, E.B.; Cecioni, I.; Berardino, S.; Montuschi, F.; Chiostri, M.; Poggesi, L. Serum uric acid levels and renal damage in hyperuricemic hypertensive patients treated with renin-angiotensin system blockers. Am. J. Hypertens. 2010, 23, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Afsar, B.; Elsurer, R.; Ozdemir, F.N.; Sezer, S. Uric acid and nocturnal nondipping in hypertensive patients with normal renal function. J. Nephrol. 2008, 21, 406–411. [Google Scholar] [PubMed]
- Giallauria, F.; Predotti, P.; Casciello, A.; Grieco, A.; Russo, A.; Viggiano, A.; Citro, R.; Ravera, A.; Ciardo, M.; Guglielmi, M.; et al. Serum uric acid is associated with non-dipping circadian pattern in young patients (30–40 years old) with newly diagnosed essential hypertension. Clin. Exp. Hypertens. 2016, 38, 233–237. [Google Scholar] [CrossRef]
- Kario, K. Obstructive sleep apnea syndrome and hypertension: Ambulatory blood pressure. Hypertens. Res. 2009, 32, 428–432. [Google Scholar] [CrossRef]
- Mazzali, M.; Hughes, J.; Kim, Y.G.; Jefferson, J.A.; Kang, D.H.; Gordon, K.L.; Lan, H.Y.; Kivlighn, S.; Johnson, R.J. Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 2001, 38, 1101–1106. [Google Scholar] [CrossRef]
- Kurra, V.; Vehmas, T.; Eräranta, A.; Jokihaara, J.; Pirttiniemi, P.; Ruskoaho, H.; Tokola, H.; Niemelä, O.; Jukka Mustonen Pörsti, I. Effects of oxonic acid-induced hyperuricemia on mesenteric artery tone and cardiac load in experimental renal insufficiency. BMC Nephrol. 2015, 16, 35. [Google Scholar] [CrossRef]
- Kang, D.H.; Park, S.K.; Lee, I.K.; Johnson, R.J. Uric acid-induced C-reactive protein expression; Implication on cell proliferation and nitric oxide production of human vascular cells. J. Am. Soc. Nephrol. 2005, 16, 3553–3562. [Google Scholar] [CrossRef]
- Yu, M.A.; Sanchez-Lozada, L.G.; Johnson, R.J. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J. Hypertens. 2010, 28, 1234–1242. [Google Scholar] [CrossRef] [PubMed]
- Rizzoni, D.; Ciuceis, C.D.; Szczepaniak, P.; Paradis, P.; Schiffrin, E.L.; Guzik, T.J. Immune System and Microvascular Remodeling in Humans. Hypertension 2022, 79, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Dauphinot, V.; Roche, F.; Kossovsky, M.P.; Schott, A.M.; Pichot, V.; Gaspoz, J.M.; Gosse, P.; Barthelemy, J.C. C-reactive protein implications in new-onset hypertension in a healthy population initially aged 65 years: The Proof study. J. Hypertens. 2009, 27, 736–743. [Google Scholar] [CrossRef] [PubMed]
- Kanellis, J.; Watanabe, S.; Li, J.H.; Kang, D.H.; Li, P.; Nakagawa, T.; Wamsley, A.; Sheikh-Hamad, D.; Lan, H.Y.; Feng, L.; et al. Uric acid stimulates monocyte chemoattractant protein-1 production in vascular smooth muscle cells via mitogen-activated protein kinase and cyclooxygenase-2. Hypertension 2003, 41, 1287–1293. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.J.; Rodriguez-Iturbe, B.; Kang, D.H.; Feig, D.I.; Herrera-Acosta, J. A unifying pathway for essential hypertension. Am. J. Hypertens. 2005, 18, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, C.; Cherubini, A.; Ble, A.; Bos, A.J.G.; Maggio, M.; Dixit, V.D.; Lauretani, F.; Bandinelli, S.; Senin, U.; Ferrucci, L. Uric acid and inflammatory markers. Eur. Heart J. 2006, 27, 1174–1181. [Google Scholar] [CrossRef]
- Hornstrup, B.G.; Gjoerup, P.H.; Wessels, J.; Lauridsen, T.G.; Pedersen, E.C.; Bech, J.N. Nocturnal blood pressure decrease in patients with chronic kidney disease and in healthy controls–significance of obstructive sleep apnea and renal function. Int. J. Nephrol. Renovasc. Dis. 2018, 11, 279–290. [Google Scholar] [CrossRef]
- Cardoso, C.R.L.; Salles, G.F. Associations of the nocturnal blood pressure fall and morning surge with cardiovascular events and mortality in individuals with resistant hypertension. J. Hypertens. 2021, 39, 1177–1187. [Google Scholar] [CrossRef]

| Total (n = 154) | Non-Dipper (n = 56) | Dipper (n = 98) | |
|---|---|---|---|
| Demographics | |||
| Age (years) | 55.7 ± 11.9 | 57.8 ± 12.7 | 54.5 ± 11.2 |
| Male (number, %) | 88 (57) | 33 (59) | 55 (56) |
| Duration of hypertension (years) | 4.9 ± 6.7 | 5.6 ± 7.6 | 4.4 ± 6.1 |
| Smoking (number, %) | 41 (27) | 16 (29) | 25 (26) |
| Alcohol intake (g ethanol/day) | 13.4 ± 19.8 | 14.3 ± 22.5 | 12.8 ± 18.3 |
| Type 2 diabetes mellitus (number, %) | 2 (1) | 1 (2) | 0 (0) |
| Dyslipidemia (number, %) | 11 (7) | 6 (11) | 5 (5) |
| Body mass index (kg/m2) | 24.6 ± 3.9 | 25.5 ± 4.2 * | 24.1 ± 3.6 |
| Blood Pressure | |||
| 24 h systolic BP (mmHg) | 142 ± 16 | 148 ± 17 * | 139 ± 16 |
| 24 h diastolic BP (mmHg) | 88 ± 11 | 89 ± 10 | 88 ± 12 |
| Daytime average systolic BP (mmHg) | 149 ± 17 | 149 ± 17 | 149 ± 17 |
| Daytime average diastolic BP (mmHg) | 92 ± 12 | 90 ± 11 | 93 ± 13 |
| Nighttime average systolic BP (mmHg) | 130 ± 20 | 144 ± 18 * | 121 ± 16 |
| Nighttime average diastolic BP (mmHg) | 80 ± 12 | 86 ± 10* | 76 ± 12 |
| Laboratory data | |||
| Serum uric acid (mg/dL) | 5.7 ± 1.6 | 6.0 ± 1.7 * | 5.5 ± 1.5 |
| High-sensitivity C-reactive protein (mg/dL) | 0.08 ± 0.13 | 0.10 ± 0.15 * | 0.07 ± 0.11 |
| Low-density lipoprotein cholesterol (mg/dL) | 116 ± 33 | 0.08 ± 0.13 | 0.08 ± 0.13 |
| High-density lipoprotein cholesterol (mg/dL) | 56 ± 15 | 52 ± 12 * | 57 ± 16 |
| Triglyceride (mg/dL) | 97 ± 54 | 110 ± 60 * | 90 ± 49 |
| Fasting glucose (mg/dL) | 96 ± 14 | 96 ± 14 | 96 ± 15 |
| HOMA-IR | 1.60 ± 1.84 | 1.73 ± 1.42 | 1.53 ± 2.04 |
| HbA1c (%) | 5.0 ± 0.5 | 5.1 ± 0.5 | 5.0 ± 0.4 |
| Plasma renin activity (ng/mL/hr) | 0.80 ± 0.67 | 0.75 ± 0.74 | 0.82 ± 0.63 |
| Plasma aldosterone concentration (pg/mL) | 74.2 ± 33.6 | 71.2 ± 37.5 | 75.9 ± 31.2 |
| Epinephrine (pg/mL) | 26.9 ± 18.8 | 25.5 ± 20.0 | 27.8 ± 18.2 |
| Norepinephrine (pg/mL) | 220 ± 87 | 200 ± 83 | 232 ± 88 |
| Adiponectin (μg/mL) | 10.1 ± 5.8 | 9.6 ± 5.4 | 10.4 ± 6.1 |
| Leptin (μg/mL) | 7.2 ± 6.5 | 8.0 ± 6.3 | 6.8 ± 6.6 |
| Nitric oxide metabolites (μmol/L) | 47.8 ± 31.1 | 41.4 ± 25.3 * | 50.1 ± 31.3 |
| Urinary data | |||
| Urinary sodium (mEq/day) | 191 ± 84 | 188 ± 83 | 195 ± 86 |
| Urinary C-peptide (μg/day) | 90 ± 53 | 92 ± 56 | 89 ± 52 |
| Urinary epinephrine (μg/day) | 11.4 ± 7.7 | 10.3 ± 8.6 | 12.0 ± 7.0 |
| Urinary norepinephrine (μg/day) | 162 ± 77 | 151 ± 70 | 169 ± 81 |
| Urinary dopamine (μg/day) | 1180 ± 1074 | 1058 ± 816 | 1242 ± 1188 |
| Creatinine clearance (mL/min/1.73m2) | 123 ± 36 | 121 ± 33 | 125 ± 37 |
| Echocardiographic findings | |||
| Left ventricular mass index (g/m2) | 122 ± 35 | 130 ± 29 * | 118 ± 37 |
| Left ventricular ejection fraction (%) | 66 ± 8 | 66 ± 8 | 67 ± 8 |
| E/A ratio | 0.95 ± 0.32 | 0.95 ± 0.33 | 0.96 ± 0.032 |
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| Factor | Odds Ratio | p Value | Odd Ratio | p Value |
| Age | 1.03 (1.00–1.06) | 0.10 | ||
| Male | 1.12 (0.58–2.18) | 0.74 | ||
| Body mass index | 1.10 (1.01–1.20) | <0.05 * | 1.08 (0.98–1.20) | 0.13 |
| Alcohol intake | 1.00 (0.99–1.02) | 0.68 | ||
| Serum uric acid | 1.25 (1.00–1.56) | <0.05 * | 1.03 (1.00–1.05) | <0.05 * |
| High-sensitivity C-reactive protein | 11.6 (0.67–201.0) | 0.093 | 4.59 (0.23–90.2) | 0.32 |
| HOMA-R | 1.06 (0.89–1.27) | 0.51 | ||
| Plasma renin activity | 0.85 (0.51–1.41) | 0.52 | ||
| Plasma aldosterone concentration | 0.96 (0.86–1.06) | 0.40 | ||
| Epinephrine | 0.99 (0.98–1.01) | 0.48 | ||
| Norepinephrine | 1.00 (1.00–1.00) | 0.73 | ||
| Adiponectin | 0.98 (0.92–1.03) | 0.40 | ||
| Leptin | 1.03 (0.98–1.08) | 0.26 | ||
| Nitric oxide metabolites | 0.99 (0.98–1.00) | 0.070 | 0.99 (0.98–1.00) | 0.15 |
| Urinary sodium | 1.00 (1.00–1.00) | 0.66 | ||
| Urinary C-peptide | 1.00 (0.99–1.01) | 0.79 | ||
| Urinary epinephrine | 0.97 (0.92–1.02) | 0.21 | ||
| Urinary norepinephrine | 1.00 (1.00–1.00) | 0.98 | ||
| Urinary dopamine | 1.00 (1.00–1.00) | 0.33 | ||
| Creatinine clearance | 1.00 (0.99–1.01) | 0.57 | ||
| Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|
| Beta Value | p Value | Beta Value | p Value | |
| Age | 0.15 | 0.45 | ||
| Male | 1.51 | 0.77 | ||
| Body mass index | 0.98 | 0.093 | 0.55 | 0.38 |
| Alcohol intake | 0.10 | 0.37 | ||
| Serum uric acid | 2.62 | 0.074 | 1.43 | 0.096 |
| High-sensitivity C-reactive protein | 36.21 | <0.05 * | 30.85 | 0.065 |
| HOMA-R | −0.06 | 0.97 | ||
| Plasma renin activity | −3.73 | 0.27 | ||
| Plasma aldosterone concentration | −0.79 | 0.24 | ||
| Epinephrine | −0.02 | 0.55 | ||
| Norepinephrine | −0.04 | 0.24 | ||
| Adiponectin | −0.19 | 0.70 | ||
| Leptin | 0.22 | 0.59 | ||
| Nitric oxide metabolites | −0.08 | 0.44 | ||
| Urinary sodium | 0.03 | 0.36 | ||
| Urinary C-peptide | 0.03 | 0.56 | ||
| Urinary epinephrine | 0.23 | 0.45 | ||
| Urinary norepinephrine | 0.01 | 0.92 | ||
| Urinary dopamine | 0.00 | 0.95 | ||
| Creatinine clearance | −0.08 | 0.31 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koike, T.; Imamura, T.; Tomoda, F.; Ohara, M.; Fujioka, H.; Kakeshita, K.; Yamazaki, H.; Kinugawa, K. Factors Associating with Non-Dipping Pattern of Nocturnal Blood Pressure in Patients with Essential Hypertension. J. Clin. Med. 2023, 12, 570. https://doi.org/10.3390/jcm12020570
Koike T, Imamura T, Tomoda F, Ohara M, Fujioka H, Kakeshita K, Yamazaki H, Kinugawa K. Factors Associating with Non-Dipping Pattern of Nocturnal Blood Pressure in Patients with Essential Hypertension. Journal of Clinical Medicine. 2023; 12(2):570. https://doi.org/10.3390/jcm12020570
Chicago/Turabian StyleKoike, Tsutomu, Teruhiko Imamura, Fumihiro Tomoda, Maiko Ohara, Hayato Fujioka, Kota Kakeshita, Hidenori Yamazaki, and Koichiro Kinugawa. 2023. "Factors Associating with Non-Dipping Pattern of Nocturnal Blood Pressure in Patients with Essential Hypertension" Journal of Clinical Medicine 12, no. 2: 570. https://doi.org/10.3390/jcm12020570
APA StyleKoike, T., Imamura, T., Tomoda, F., Ohara, M., Fujioka, H., Kakeshita, K., Yamazaki, H., & Kinugawa, K. (2023). Factors Associating with Non-Dipping Pattern of Nocturnal Blood Pressure in Patients with Essential Hypertension. Journal of Clinical Medicine, 12(2), 570. https://doi.org/10.3390/jcm12020570








