Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
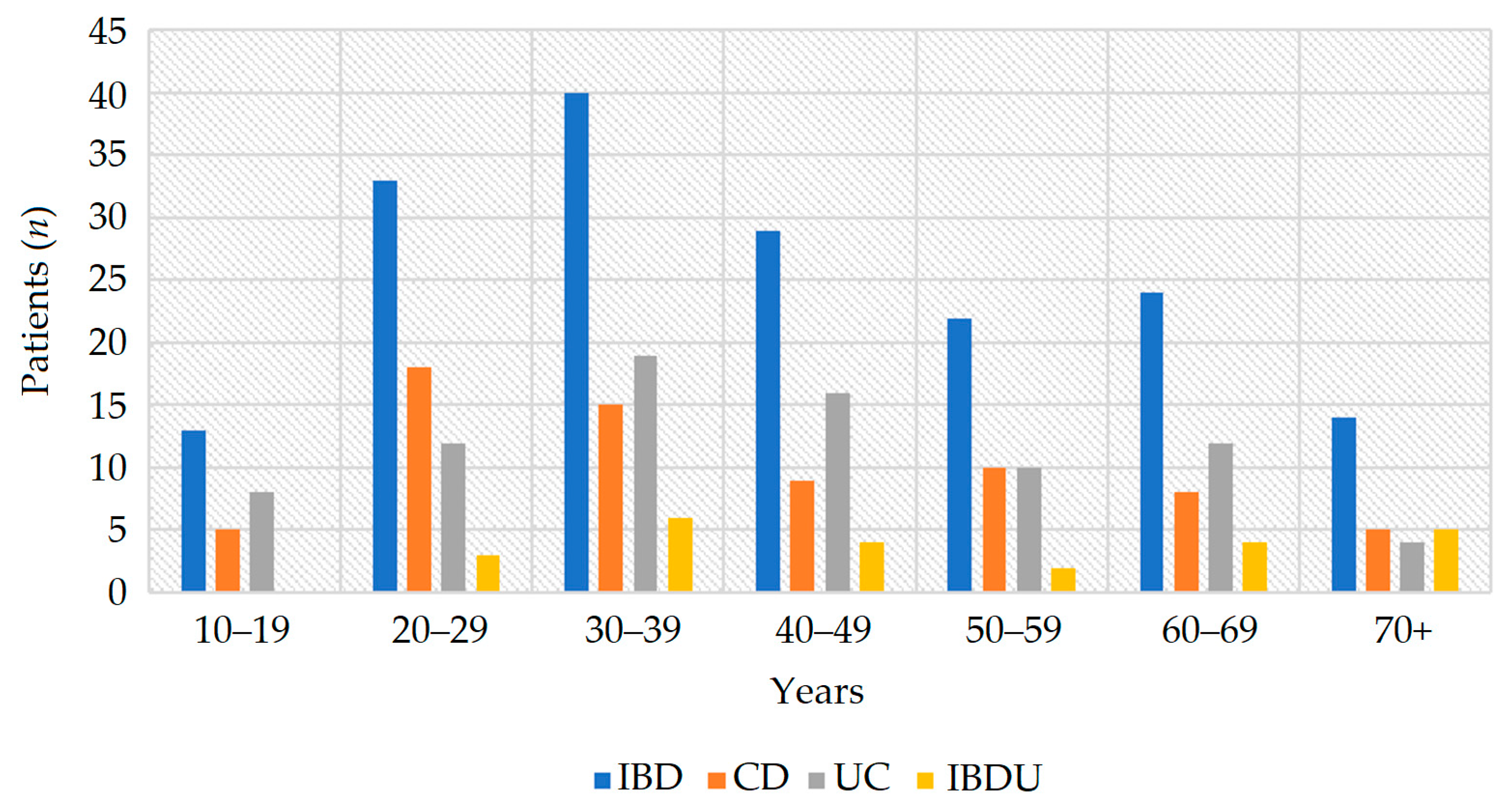
3.1. Clinical Characteristics
3.2. Prevalence
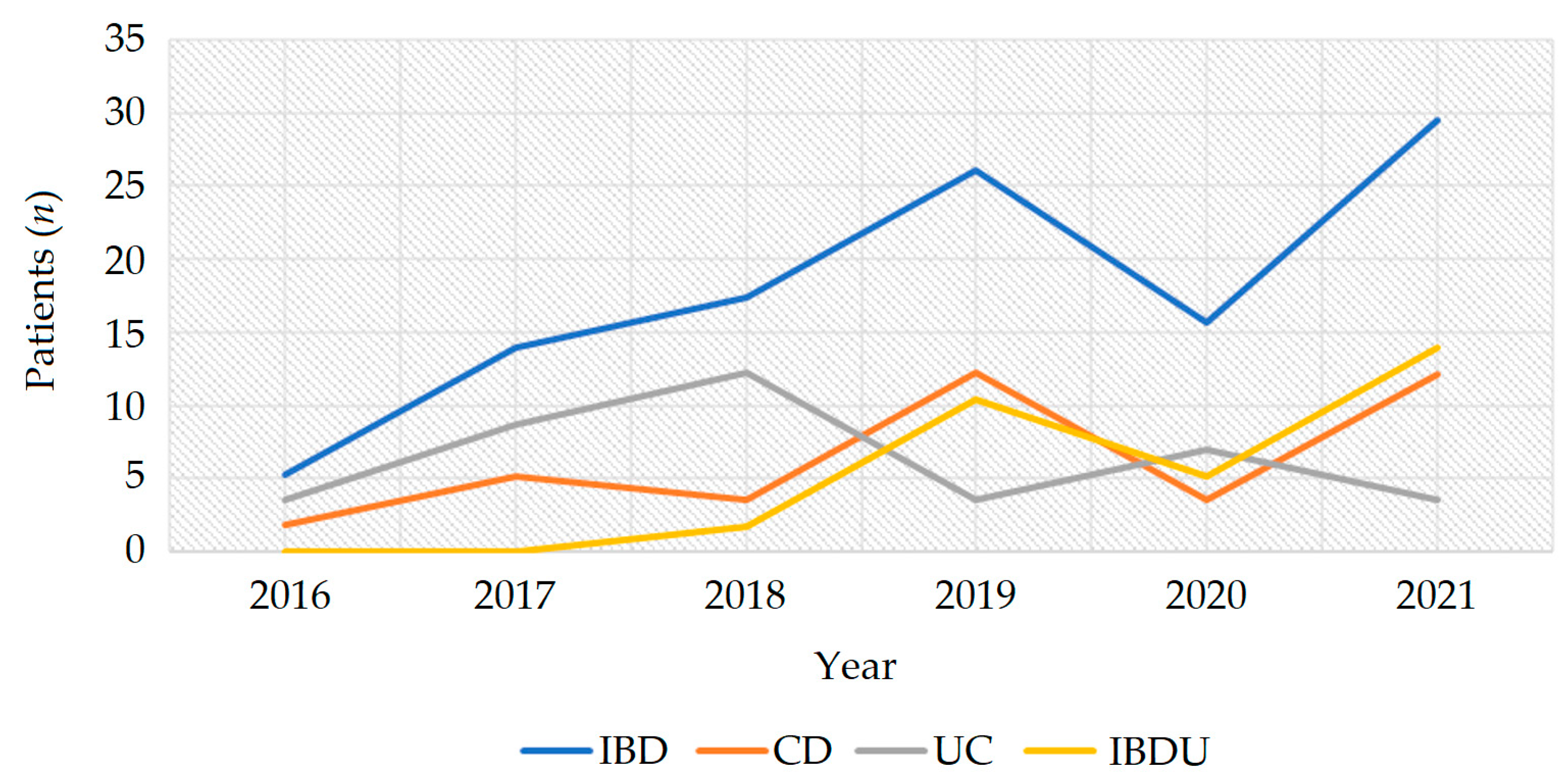
3.3. Incidence
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Actis, G.C.; Pellicano, R.; Fagoonee, S.; Ribaldone, D.G. History of Inflammatory Bowel Diseases. J. Clin. Med. 2019, 8, 1970. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, G.G.; Ng, S.C. Globalisation of inflammatory bowel disease: Perspectives from the evolution of inflammatory bowel disease in the UK and China. Lancet Gastroenterol. Hepatol. 2016, 1, 307–316. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crocetti, E.; Bergamaschi, W.; Russo, A.G. Population-based incidence and prevalence of inflammatory bowel diseases in Milan (Northern Italy), and estimates for Italy. Eur. J. Gastroenterol. Hepatol. 2021, 33, e383–e389. [Google Scholar] [CrossRef]
- Macaluso, F.S.; Mocci, G.; Orlando, A.; Scondotto, S.; Fantaci, G.; Antonelli, A.; Leone, S.; Previtali, E.; Cabras, F.; Cottone, M.; et al. Prevalence and incidence of inflammatory bowel disease in two Italian islands, Sicily and Sardinia: A report based on health information systems. Dig. Liver Dis. 2019, 51, 1270–1274. [Google Scholar] [CrossRef] [PubMed]
- Di Domenicantonio, R.; Cappai, G.; Arcà, M.; Agabiti, N.; Kohn, A.; Vernia, P.; Biancone, L.; Armuzzi, A.; Papi, C.; Davoli, M. Occurrence of inflammatory bowel disease in central Italy: A study based on health information systems. Dig. Liver Dis. 2014, 46, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Valpiani, D.; Manzi, I.; Mercuriali, M.; Giuliani, O.; Ravaioli, A.; Colamartini, A.; Bucchi, L.; Falcini, F.; Ricci, E. A model of an inflammatory bowel disease population-based registry: The Forlì experience (1993–2013). Dig. Liver Dis. 2018, 50, 32–36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Piscaglia, A.C.; Lopetuso, L.R.; Laterza, L.; Gerardi, V.; Sacchini, E.; Leoncini, E.; Boccia, S.; Stefanelli, M.L.; Gasbarrini, A.; Armuzzi, A. Epidemiology of inflammatory bowel disease in the Republic of San Marino: The “EPIMICI-San Marino” study. Dig. Liver Dis. 2019, 51, 218–225. [Google Scholar] [CrossRef] [PubMed]
- Caviglia, G.P.; Rosso, C.; Stalla, F.; Rizzo, M.; Massano, A.; Abate, M.L.; Olivero, A.; Armandi, A.; Vanni, E.; Younes, R.; et al. On-Treatment Decrease of Serum Interleukin-6 as a Predictor of Clinical Response to Biologic Therapy in Patients with Inflammatory Bowel Diseases. J. Clin. Med. 2020, 9, 800. [Google Scholar] [CrossRef] [PubMed]
- Carli, E.; Caviglia, G.P.; Pellicano, R.; Fagoonee, S.; Rizza, S.; Astegiano, M.; Saracco, G.M.; Ribaldone, D.G. Incidence of Prostate Cancer in Inflammatory Bowel Disease: A Meta-Analysis. Medicina 2020, 56, 85. [Google Scholar] [CrossRef] [PubMed]
- Ribaldone, D.G.; Pellicano, R.; Actis, G.C. The gut and the inflammatory bowel diseases inside-out: Extra-intestinal manifestations. Minerva Gastroenterol. Dietol. 2019, 65, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Kuenzig, M.E.; Manuel, D.G.; Donelle, J.; Benchimol, E.I. Life expectancy and health-adjusted life expectancy in people with inflammatory bowel disease. CMAJ 2020, 192, E1394–E1402. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://servizi.regione.piemonte.it/catalogo/pista-piemonte-statistica-bdde (accessed on 15 July 2022).
- Silverberg, M.S.; Satsangi, J.; Ahmad, T.; Arnott, I.D.; Bernstein, C.N.; Brant, S.R.; Caprilli, R.; Colombel, J.F.; Gasche, C.; Geboes, K.; et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a working party of the 2005 Montreal world congress of gastroenterology. Can. J. Gastroenterol. 2005, 19, 5–36. [Google Scholar] [CrossRef] [PubMed]
- Vanni, R. Epidemiological study of inflammatory bowel disease in Bra, Piemonte, Italy: Methodological problems. In Proceedings of the FISMAD Conference, Palermo, Italy, 29 September–3 October 2007. [Google Scholar]
- Tursi, A.; Elisei, W.; Picchio, M. Incidence and prevalence of inflammatory bowel diseases in gastroenterology primary care setting. Eur. J. Intern. Med. 2013, 24, 852–856. [Google Scholar] [CrossRef] [PubMed]
- Alboraie, M.; Piscoya, A.; Tran, Q.T.; Mendelsohn, R.B.; Butt, A.S.; Lenz, L.; Alavinejad, P.; Emara, M.H.; Samlani, Z.; Altonbary, A.; et al. The global impact of COVID-19 on gastrointestinal endoscopy units: An international survey of endoscopists. Arab. J. Gastroenterol. 2020, 21, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, M.; Jess, T. Implications of the changing epidemiology of inflammatory bowel disease in a changing world. United Eur. Gastroenterol J. 2022, 10, 1113–1120. [Google Scholar] [CrossRef] [PubMed]
- Annese, V.; Duricova, D.; Gower-Rousseau, C.; Jess, T.; Langholz, E. Impact of New Treatments on Hospitalisation, Surgery, Infection, and Mortality in IBD: A Focus Paper by the Epidemiology Committee of ECCO. J. Crohns Colitis 2016, 10, 216–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Candido, F.D.; Fiorino, G.; Spadaccini, M.; Danese, S.; Spinelli, A. Are Surgical Rates Decreasing in the Biological Era In IBD? Curr Drug Targets 2019, 20, 1356–1362. [Google Scholar] [CrossRef] [PubMed]
- Burgess, C.J.; Jackson, R.; Chalmers, I.; Russell, R.K.; Hansen, R.; Scott, G.; Henderson, P.; Wilson, D.C. The inexorable increase of biologic exposure in paediatric inflammatory bowel disease: A Scottish, population-based, longitudinal study. Aliment. Pharmacol. Ther. 2022, 56, 1453–1459. [Google Scholar] [CrossRef] [PubMed]
| Municipality | Population (n) | IBD (n) | CD (n) | UC (n) | IBDU (n) | IBD Witout Clinical Data (n) |
|---|---|---|---|---|---|---|
| Bra | 25,996 | 87 M = 48; F = 39 | 31 M = 14; F = 17 | 39 M = 24; F = 15 | 12 M = 7; F = 5 | 5 M = 3; F = 2 |
| Ceresole d’Alba | 1791 | 3 M =1; F = 2 | 2 M = 0; F = 2 | 1 M = 1; F = 0 | 0 | 0 |
| Cherasco | 8098 | 18 M = 9; F = 9 | 11 M = 6; F = 5 | 4 M = 1; F = 3 | 3 M = 2; F = 1 | 0 |
| Santa Vittoria d’Alba | 2504 | 11 M = 7; F = 4 | 3 M = 3; F = 0 | 6 M = 3; F = 3 | 2 M = 1; F = 1 | 0 |
| La Morra | 2379 | 5 M = 3; F = 2 | 2 M = 1; F = 1 | 1 M = 1; F = 0 | 1 M = 0; F = 1 | 1 M = 1; F = 0 |
| Narzole | 3014 | 6 M = 5; F = 1 | 1 M = 1; F = 0 | 4 M = 3; F = 1 | 1 M = 1; F = 0 | 0 |
| Pocapaglia | 2848 | 9 M = 5; F = 4 | 4 M = 3; F = 1 | 2 M = 1; F = 1 | 2 M = 0; F = 2 | 1 M = 1; F = 0 |
| Sanfrè | 2632 | 9 M = 5; F = 4 | 2 M = 1; F = 1 | 6 M = 4; F = 2 | 0 | 1 M = 0, F = 1 |
| Sommariva Del Bosco | 5473 | 18 M = 11; F = 7 | 6 M = 3; F = 3 | 8 M = 5; F = 3 | 1 M = 0; F = 1 | 3 M = 3; F = 0 |
| Sommariva Perno | 2388 | 18 M = 8; F = 10 | 8 M = 3; F = 5 | 9 M = 4; F = 5 | 1 M = 1; F = 0 | 0 |
| Verduno | 492 | 2 M = 1; F = 1 | 0 | 1 M = 0; F = 1 | 1 M = 1; F = 0 | 0 |
| Healthcare Disctric of Bra | 57,615 | 186 M = 103; F = 83 | 70 M = 35; F = 35 | 81 M = 47; F = 34 | 24 M = 13; F = 11 | 11 M = 8; F = 3 |
| Municipality | IBD Prevalence (2021) | IBD Prevalence (2006) | Variation (%) 2006–2021 | CD Prevalence (2021) | UC Prevalence (2021) | IBDU Prevalence (2021) |
|---|---|---|---|---|---|---|
| Bra | 334.4 | 250 | +34% | 119.2 | 150.0 | 46.0 |
| Ceresole d’Alba | 167.5 | 290 | −42% | 111.7 | 55.8 | 0 |
| Cherasco | 222.2 | 160 | +39% | 135.8 | 49.4 | 37.0 |
| Santa Vittoria d’Alba | 439.3 | 270 | +63% | 119.8 | 239.6 | 79.9 |
| La Morra | 210.2 | 70 | +200% | 84.2 | 42.0 | 42.0 |
| Narzole | 199.1 | 150 | +33% | 33.2 | 132.7 | 33.2 |
| Pocapaglia | 315.9 | 70 | +351% | 140.4 | 70.2 | 70.2 |
| Sanfrè | 342.0 | 350 | −2% | 76.0 | 228.0 | 0 |
| Sommariva Del Bosco | 310.7 | 250 | +24% | 109.6 | 128.0 | 18.3 |
| Sommariva Perno | 753.8 | 250 | +202% | 335.0 | 376.9 | 41.9 |
| Verduno | 406.6 | 380 | +7% | 0 | 203.3 | 203.3 |
| Health Care Disctric of Bra | 321.2 | 220 | +46% | 121.5 | 138.9 | 41.7 |
| 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2016–2021 (Mean ± SD) | 2001–2006 (Mean) | Variation (%) 2006–2021 | |
|---|---|---|---|---|---|---|---|---|---|
| IBD | 5.3 | 13.9 | 17.4 | 26.1 | 15.7 | 29.5 | 18.0 ± 8.0 | 6.7 | 169% |
| CD | 1.8 | 5.2 | 3.5 | 12.2 | 3.5 | 12.1 | 6.4 ± 4.2 | 2.9 | 121% |
| UC | 3.5 | 8.7 | 12.2 | 3.5 | 7.0 | 3.5 | 6.4 ± 3.3 | 3.7 | 73% |
| IBDU | 0 | 0 | 1.7 | 10.4 | 5.2 | 13.9 | 5.2 ± 5.3 | N/A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caviglia, G.P.; Garrone, A.; Bertolino, C.; Vanni, R.; Bretto, E.; Poshnjari, A.; Tribocco, E.; Frara, S.; Armandi, A.; Astegiano, M.; et al. Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy. J. Clin. Med. 2023, 12, 641. https://doi.org/10.3390/jcm12020641
Caviglia GP, Garrone A, Bertolino C, Vanni R, Bretto E, Poshnjari A, Tribocco E, Frara S, Armandi A, Astegiano M, et al. Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy. Journal of Clinical Medicine. 2023; 12(2):641. https://doi.org/10.3390/jcm12020641
Chicago/Turabian StyleCaviglia, Gian Paolo, Angela Garrone, Chiara Bertolino, Riccardo Vanni, Elisabetta Bretto, Anxhela Poshnjari, Elisa Tribocco, Simone Frara, Angelo Armandi, Marco Astegiano, and et al. 2023. "Epidemiology of Inflammatory Bowel Diseases: A Population Study in a Healthcare District of North-West Italy" Journal of Clinical Medicine 12, no. 2: 641. https://doi.org/10.3390/jcm12020641








