The Epidemiology of Pre-Hospital EMS Treatment of Geriatric Patients in the City of Vienna—An Overview
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Acquisition
2.2. The Viennese EMS
2.3. Statistical Analysis
3. Results
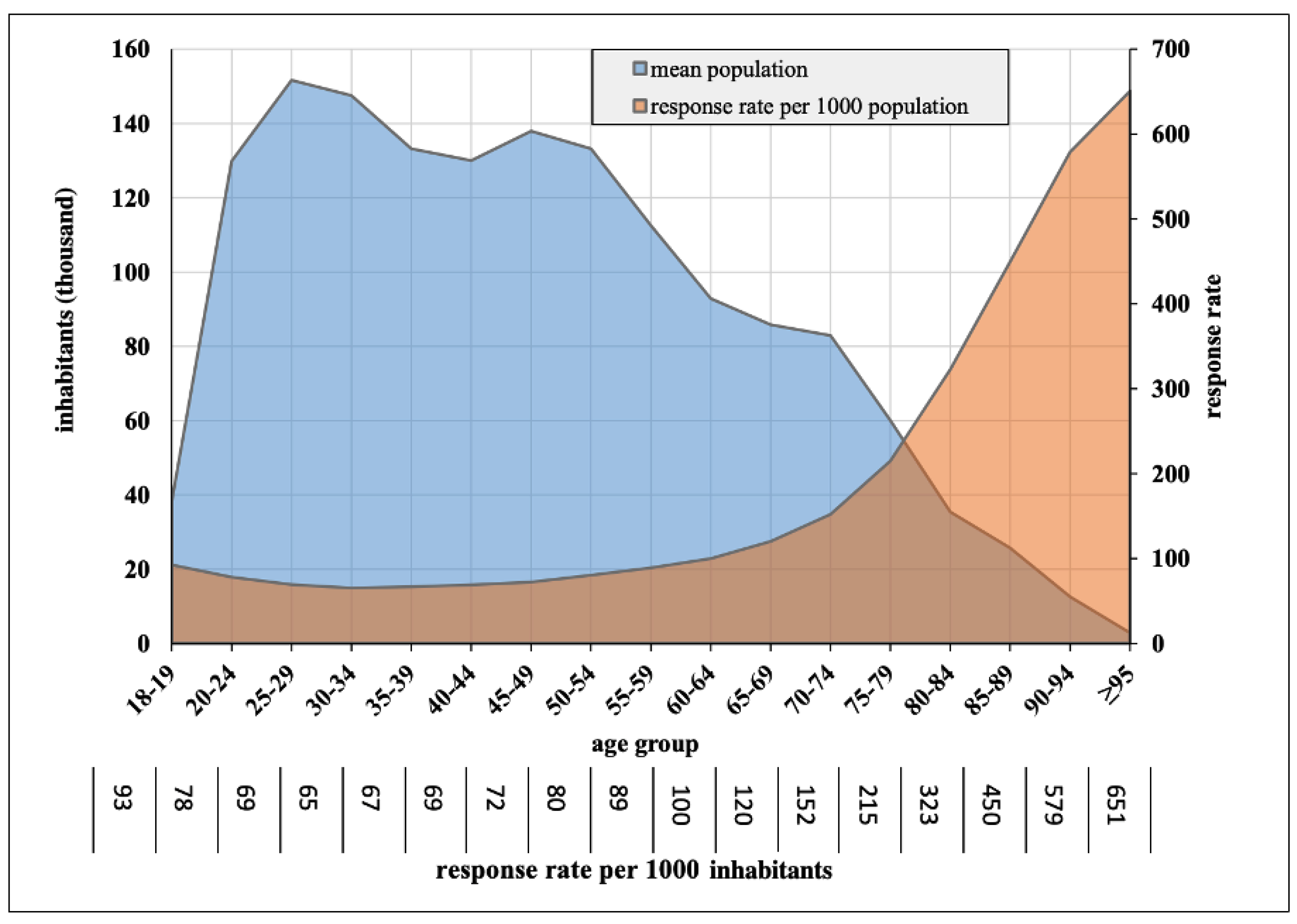
3.1. EMS Responses
3.2. Age and Gender
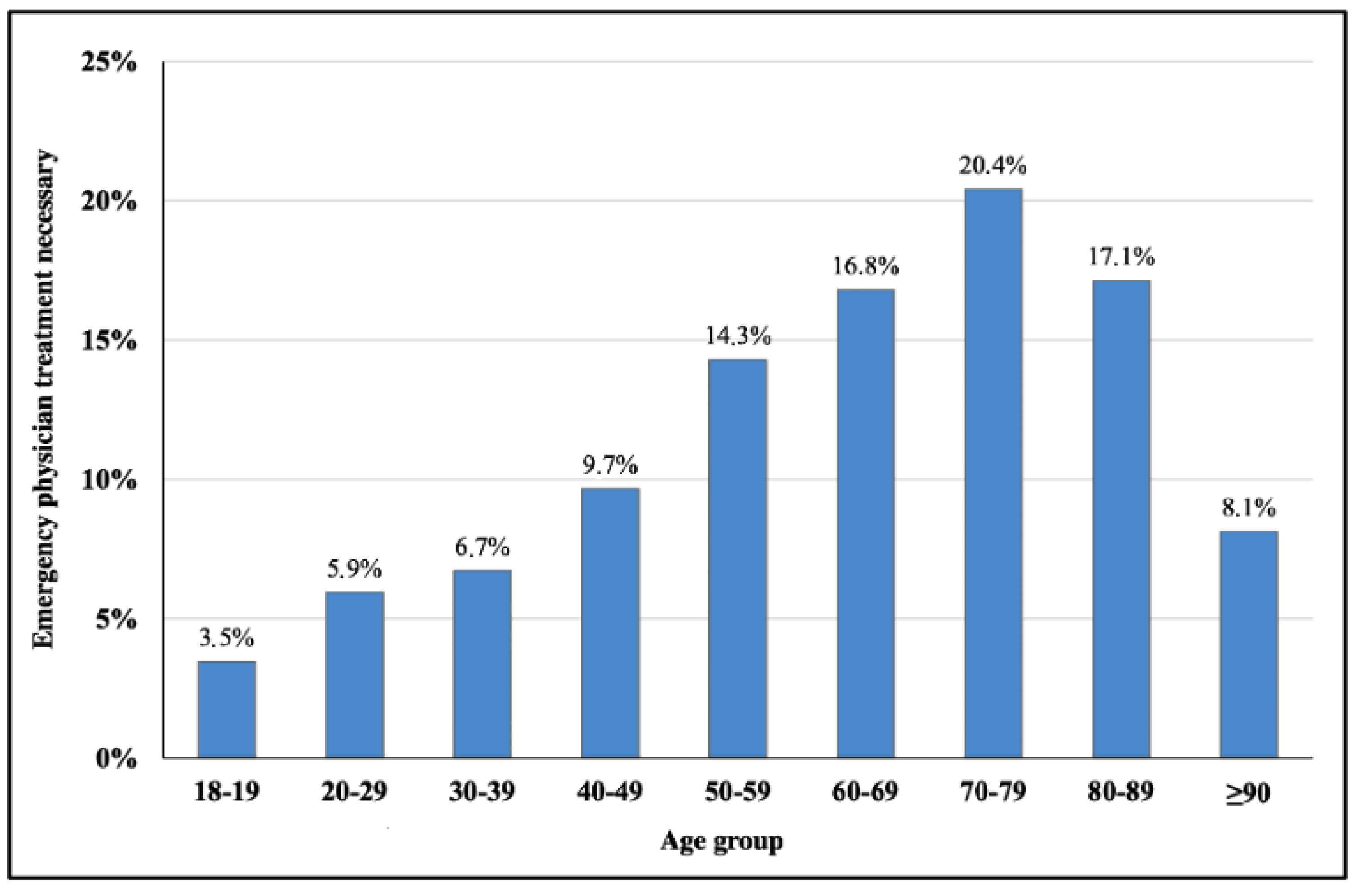
3.3. Emergency Physicians
3.4. Transport and Non-Transport
4. Discussion
4.1. Response Rates in International Comparison
4.2. Low Urgency Missions
4.3. A growing Strain on the System
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lowthian, J.A.; Cameron, P.A.; Stoelwinder, J.U.; Curtis, A.; Currell, A.; Cooke, M.W.; McNeil, J.J. Increasing utilisation of emergency ambulances. Aust. Health Rev. 2011, 35, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.N.; Bazarian, J.J.; Lerner, E.B.; Fairbanks, R.J.; Barker, W.H.; Auinger, P.; Friedman, B. The epidemiology of emergency medical services use by older adults: An analysis of the National Hospital Ambulatory Medical Care Survey. Acad. Emerg. Med. 2007, 14, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Lowthian, J.A.; Jolley, D.J.; Curtis, A.J.; Currell, A.; Cameron, P.A.; Stoelwinder, J.U.; McNeil, J.J. The challenges of population ageing: Accelerating demand for emergency ambulance services by older patients, 1995–2015. Med. J. Aust. 2011, 194, 574–578. [Google Scholar] [CrossRef]
- City of Vienna. Bevölkerungsprognose—Statistiken [Internet]. Available online: https://www.wien.gv.at/statistik/bevoelkerung/prognose/ (accessed on 27 November 2022).
- Austrian National Statistics Office. Bevölkerung im Jahresdurchschnitt—STATISTIK AUSTRIA—Die Informationsmanager [Internet]. Available online: https://www.statistik.at/statistiken/bevoelkerung-und-soziales/bevoelkerung/bevoelkerungsstand/bevoelkerung-im-jahresdurchschnitt (accessed on 27 November 2022).
- Prückner, S.; Luiz, T.; Steinbach-Nordmann, S.; Nehmer, J.; Danner, K.; Madler, C. Emergency medicine--medicine for an ageing society. A contribution to the context of emergency missions for elderly people. Anaesthesist 2008, 57, 391–396. [Google Scholar] [CrossRef]
- Borský, P.; Holmannová, D.; Fiala, Z.; Borská, L.; Hruška, L.; Kučera, O. Physiology of ageing. Cas. Lek. Cesk. 2022, 161, 11–16. [Google Scholar] [PubMed]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Allione, A.; Pivetta, E.; Pizzolato, E.; Lorenzati, B.; Pomero, F.; Barutta, L.; Lauria, G.; Tartaglino, B. Determinants of inappropriate acute pain management in old people unable to communicate verbally in the emergency department. Turk. J. Emerg. Med. 2017, 17, 160–164. [Google Scholar] [CrossRef]
- Johnson, R.; Harmon, R.; Klammer, C.; Kumar, A.; Greer, C.; Beasley, K.; Wigstadt, S.; Ambrose, L.; VanDePol, E.; Jones, J. Cost-related medication nonadherence among elderly emergency department patients. Am. J. Emerg. Med. 2019, 37, 2255–2256. [Google Scholar] [CrossRef]
- Guo, D.Y.; Chen, K.H.; Chen, I.C.; Lu, K.Y.; Lin, Y.C.; Hsiao, K.Y. The Association Between Emergency Department Revisit and Elderly Patients. J. Acute. Med. 2020, 10, 20–26. [Google Scholar]
- Woitok, B.K.; Ravioli, S.; Funk, G.-C.; Lindner, G. Characteristics of very elderly patients in the emergency department—A retrospective analysis. Am. J. Emerg. Med. 2021, 46, 200–203. [Google Scholar] [CrossRef]
- Shenvi, C.L.; Platts-Mills, T.F. Managing the Elderly Emergency Department Patient. Ann. Emerg. Med. 2019, 73, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Barishansky, R.M. The Silver Tsunami: Are you Ready? America’s elderly population is exploding, and EMS services will have to reflect that. EMS World 2016, 45, 53–56. [Google Scholar] [PubMed]
- Baum, S.A.; Rubenstein, L. Old people in the emergency room: Age-related differences in emergency department use and care. J. Am. Geriatr. Soc. 1987, 35, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Bernoulli, L.; Zollinger, A. The NACA scale. Construct and predictive validity of the NACA scale for prehospital severity rating in trauma patients. Anaesthesist 2001, 50, 150–154. [Google Scholar] [CrossRef]
- Dami, F.; Darioli, V.; Pasquier, M. Association between the NACA score and clinical outcomes. Am. J. Emerg. Med. 2020, 38, 1692–1693. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.; Jensen, J.L.; Carter, A.J.E.; Travers, A.H.; Rockwood, K. The Epidemiology of Prehospital Emergency Responses for Older Adults in a Provincial EMS System. CJEM 2015, 17, 491–496. [Google Scholar] [CrossRef]
- Forsgärde, E.-S.; Elmqvist, C.; Fridlund, B.; Svensson, A.; Andersson, R.; Rööst, M. Patients’ aged ≥ 65 years dispositions during ambulance assignments, including factors associated with non-conveyance to hospital: A longitudinal and comparative study. BMJ Open 2020, 10, e038885. [Google Scholar] [CrossRef]
- Tokuda, Y.; Abe, T.; Ishimatsu, S.; Hinohara, S. Ambulance transport of the oldest old in Tokyo: A population-based study. J. Epidemiol. 2010, 20, 468–472. [Google Scholar] [CrossRef]
- Huang, C.-C.; Chen, W.-L.; Hsu, C.-C.; Lin, H.-J.; Su, S.-B.; Guo, H.-R.; Chen, P.-C. Elderly and Nonelderly Use of a Dedicated Ambulance Corps’ Emergency Medical Services in Taiwan. BioMed Res. Int. 2016, 2016, 1506436. [Google Scholar] [CrossRef]
- McManamny, T.E.; Dwyer, R.; Cantwell, K.; Boyd, L.; Sheen, J.; Smith, K.; Lowthian, J.A. Emergency ambulance demand by older adults from rural and regional Victoria, Australia. Australas. J. Ageing 2021, 41, e74–e81. [Google Scholar] [CrossRef]
- Engel, P.; Wilp, T.; Lukas, R.P.; Harding, U.; Weber, T.P.; Van Aken, H.; Bohn, A. Do sociodemographic factors influence emergency medical missions?: Analysis in the City of Münster. Anaesthesist 2011, 60, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Behrendt, H.; Runggaldier, K. Ein Problemaufriss über den demographischen Wandel in der Bundesrepublik Deutschland: Auswirkungen auf die präklinische Notfallmedizin. Notf. Rettungsmed. 2009, 12, 45–50. [Google Scholar] [CrossRef]
- Nielsen, L.M.; Østergaard, L.G.; Maribo, T.; Kirkegaard, H.; Petersen, K.S. Returning to everyday life after discharge from a short-stay unit at the Emergency Department-a qualitative study of elderly patients’ experiences. Int. J. Qual. Stud. Health Well-Being 2019, 14, 1563428. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, L.M.; Maribo, T.; Kirkegaard, H.; Petersen, K.S.; Oestergaard, L.G. Development of a complex intervention aimed at reducing the risk of readmission of elderly patients discharged from the emergency department using the intervention mapping protocol. BMC Health Serv. Res. 2018, 18, 588. [Google Scholar] [CrossRef] [PubMed]
- Merriman, M.L. Pre-hospital discharge planning: Empowering elderly patients through choice. Crit. Care Nurs. Q. 2008, 31, 52–58. [Google Scholar] [CrossRef]
- Shen, Y.; Tay, Y.C.; Teo, E.W.K.; Liu, N.; Lam, S.W.; Ong, M.E.H. Association between the elderly frequent attender to the emergency department and 30-day mortality: A retrospective study over 10 years. World J. Emerg. Med. 2018, 9, 20–25. [Google Scholar] [CrossRef]
- Weiss, S.J.; A Ernst, A.; Miller, P.; Russell, S. Repeat EMS transports among elderly emergency department patients. Prehosp. Emerg. Care. 2002, 6, 6–10. [Google Scholar] [CrossRef]
- Moyet, J.; Douay, B.; Delattre, O.; Hannat, S.; Defouilloy, C.; Bloch, F. The usefulness of a short stay geriatric unit post emergency department for the facilitation of in-hospital care of elderly subjects. Eur. J. Emerg. Med. 2020, 27, 230–231. [Google Scholar] [CrossRef]
- Brucksch, A.; Hoffmann, F.; Allers, K. Age and sex differences in emergency department visits of nursing home residents: A systematic review. BMC Geriatr. 2018, 18, 151. [Google Scholar] [CrossRef]
| Total n = 1,277,172 | Non-Elderly (18–64 Years) n = 733,535 | Elderly (≥65 Years) n = 551,146 | p-Value | ||
|---|---|---|---|---|---|
| Annual responses, n | 159,647 | 91,692 | 67,955 | <0.001 | |
| Response rate, n per 1000 population | 105.6 | 76.0 | 222.6 | <0.001 | |
| Age, years (±SD) | 57.2 ± 22.2 | 41.0 ± 13.6 | 79.2 ± 8.4 | <0.001 | |
| Female, n (%) | 681,003 (53) | 357,520 (49) | 323,483 (60) | <0.001 | |
| Emergency physician treatment, n (%) | 68,227 (5) | 30,889 (4) | 37,338 (7) | <0.001 | |
| Emergency physician treatment rate, n per 1000 population | 5.6 | 3.2 | 15.3 | <0.001 | |
| Transport to hospital, n (%) * | 1,113,119 (8.7) | 645,523 (88) | 467,596 (85) | <0.001 | |
| Non-Transport, n (%) * | 163,990 (13) | 87,979 (12) | 76,011 (14) | <0.001 | |
| Reason of call, n (%) | medical condition | 840,673 (66) | 466,028 (64) | 374,645 (69) | <0.001 |
| trauma | 271,395 (21) | 165,375 (23) | 106,020 (20) | ||
| other | 164,562 (13) | 101,769 (14) | 62,793 (12) | ||
| NACA score, n (%) | I | 127,094 (10) | 76,067 (10) | 51,027 (9) | <0.001 |
| II | 810,359 (64) | 506,566 (69) | 303,793 (56) | ||
| III | 285,347 (22) | 128,002 (18) | 157,345 (29) | ||
| IV | 29,357 (2) | 13,609 (2) | 15,748 (3) | ||
| V | 7405 (0.6) | 3310 (0.5) | 4095 (0.8) | ||
| VI | 3758 (0.3) | 1720 (0.2) | 2038 (0.4) | ||
| VII | 13,323 (1.0) | 4108 (0.6) | 9215 (1.7) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krammel, M.; Drahohs, V.; Hamp, T.; Lemoyne, S.; Grassmann, D.; Schreiber, W.; Sulzgruber, P.; Schnaubelt, S. The Epidemiology of Pre-Hospital EMS Treatment of Geriatric Patients in the City of Vienna—An Overview. J. Clin. Med. 2023, 12, 643. https://doi.org/10.3390/jcm12020643
Krammel M, Drahohs V, Hamp T, Lemoyne S, Grassmann D, Schreiber W, Sulzgruber P, Schnaubelt S. The Epidemiology of Pre-Hospital EMS Treatment of Geriatric Patients in the City of Vienna—An Overview. Journal of Clinical Medicine. 2023; 12(2):643. https://doi.org/10.3390/jcm12020643
Chicago/Turabian StyleKrammel, Mario, Valentin Drahohs, Thomas Hamp, Sabine Lemoyne, Daniel Grassmann, Wolfgang Schreiber, Patrick Sulzgruber, and Sebastian Schnaubelt. 2023. "The Epidemiology of Pre-Hospital EMS Treatment of Geriatric Patients in the City of Vienna—An Overview" Journal of Clinical Medicine 12, no. 2: 643. https://doi.org/10.3390/jcm12020643
APA StyleKrammel, M., Drahohs, V., Hamp, T., Lemoyne, S., Grassmann, D., Schreiber, W., Sulzgruber, P., & Schnaubelt, S. (2023). The Epidemiology of Pre-Hospital EMS Treatment of Geriatric Patients in the City of Vienna—An Overview. Journal of Clinical Medicine, 12(2), 643. https://doi.org/10.3390/jcm12020643







