The Role of Maxillofacial Structure and Malocclusion on Condylar Displacement in Maximum Intercuspation and Centric Relation in Patients Seeking Orthodontic Treatment—A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Search Strategy
2.3. Eligibility Criteria
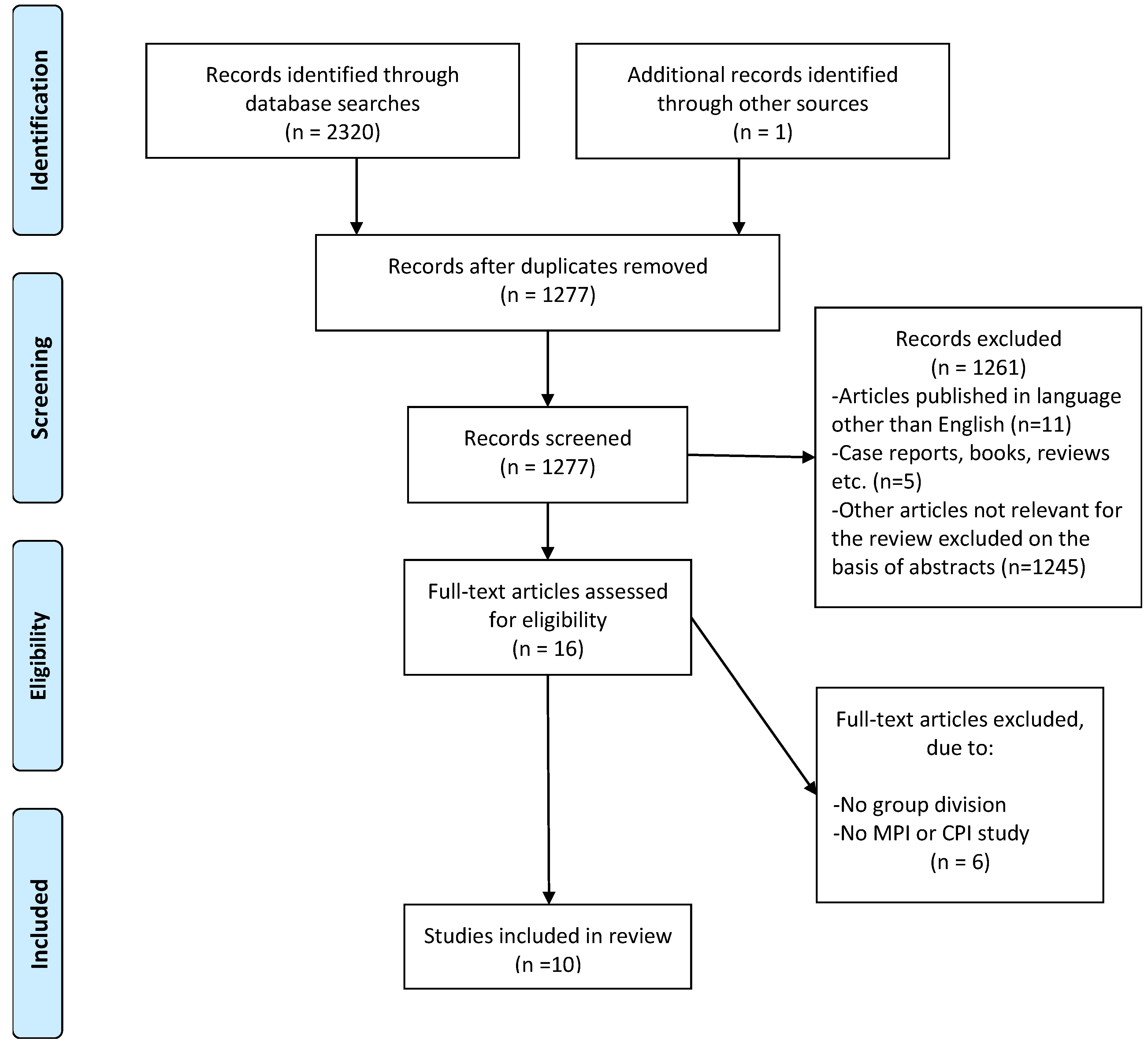
2.4. Search Results
2.5. Critical Appraisal of Individual Sources of Evidence
2.6. Data Analysis
3. Results
3.1. Assessment of CD According to Maxillofacial Structure in Different Vertical Skeletal Patterns
3.2. Assessment of CD According to Maxillofacial Structure in Sagittal Skeletal Patterns
3.3. Assessment of CD According to Vertical Malocclusions
3.4. Assessment of CD According to Horizontal Malocclusions
3.5. Assessment of CD According to Transverse Malocclusions
4. Discussion
4.1. CD in Different Vertical Skeletal Patterns and Malocclusions
4.2. CD in Different Sagittal Skeletal Patterns and Malocclusions
4.3. CD in Asymmetric Disorders
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database and Limits | Key Words | ||
| Semantic Fields: “Maxillofacial Structure Or Malocclusion” | Semantic Field: “Condylar Displacement” | ||
| PubMed (n = 897) | orthodontic OR cephalometr* OR sagittal skeletal OR sagittal relationship OR skeletal relationship OR skeletal pattern OR facial pattern OR vertical pattern OR vertical relationship OR “anb angle” OR horizontal relationship OR dentofacial deformit* OR dentofacial orthop* OR maxillofacial structure OR malocclusion OR occlusal relationship OR “midline shift” OR development, maxillofacial[MeSH Terms] OR abnormalities, maxillofacial[MeSH Terms] OR dental occlusion[MeSH Terms]) | AND | centric relation intercusp* OR centric slide OR condylar displacement OR centric discrepancy |
| Web of Science (n = 604) | orthodontic OR cephalometr* OR “sagittal skeletal” OR “sagittal relationship” OR “skeletal relationship” OR “skeletal pattern” OR “facial pattern” OR “vertical pattern” OR “vertical relationship” OR “anb angle” OR “horizontal relationship” OR “dentofacial deformit*” OR “dentofacial orthop*” OR “maxillofacial structure” OR “malocclusion” OR “occlusal relationship” OR “midline shift” OR “maxillofacial development” OR “maxillofacial abnormalities” OR “dental occlusion” | AND | centric relation intercusp* OR centric slide OR condylar displacement OR centric discrepancy |
| Scopus (n = 779) | orthodontic OR cephalometr* OR sagittal skeletal OR sagittal relationship OR skeletal relationship OR skeletal pattern OR facial pattern OR vertical pattern OR vertical relationship OR “anb angle” OR horizontal relationship OR dentofacial deformit* OR dentofacial orthop* OR maxillofacial structure OR malocclusion OR occlusal relationship OR “midline shift” OR maxillofacial development OR maxillofacial abnormalities OR dental occlusion | AND | centric relation intercusp* OR centric slide OR condylar displacement OR centric discrepancy |
| The Cochrane Library (n = 40) | orthodontic OR cephalometr* OR sagittal skeletal OR sagittal relationship OR skeletal relationship OR skeletal pattern OR facial pattern OR vertical pattern OR vertical relationship OR “anb angle” OR horizontal relationship OR dentofacial deformit* OR dentofacial orthop* OR maxillofacial structure OR malocclusion OR occlusal relationship OR “midline shift” OR development, maxilofacial [MeSH Terms]. OR abnormalities, maxillofacial[MeSH Terms]. OR dental occlusion[MeSH Terms]) | Centric relation-maximum intercuspation discrepancy OR Centric Relation-Centric Occlusion discrepancy OR Centric Slide OR centric discrepancy | |
References
- Ferro, K.J.; Morgano, S.M.; Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; McGarry, T.J. The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar]
- Okeson, J.P. Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future. Am. J. Orthod. Dentofac. Orthop. 2015, 147 (Suppl. 5), S216–S223. [Google Scholar] [CrossRef]
- Roth, R.H. The maintenance system and occlusal dynamics. Dent. Clin. N. Am. 1976, 20, 761–788. [Google Scholar] [CrossRef]
- Roth, R.H. Functional occlusion for the orthodontist. J. Clin. Orthod. 1981, 15, 4–15, 32–40. [Google Scholar] [PubMed]
- Roth, R.H. Temporomandibular pain-dysfunction and occlusal relationships. Angle Orthod. 1973, 43, 136–153. [Google Scholar] [PubMed]
- Dawson, P. Evaluation, Diagnosis, and Treatment of Occlusal Problems, 2nd ed.; C.V. Mosby: St. Louis, MO, USA, 1989. [Google Scholar]
- Slavicek, R. Clinical and instrumental functional analysis and treatment planning. Part 4. Instrumental analysis of mandibular casts using the mandibular position indicator. J. Clin. Orthod. 1988, 22, 566–575. [Google Scholar] [PubMed]
- Shildkraut, M.; Wood, D.P.; Hunter, W.S. The CR-CO discrepancy and its effect on cephalometric measurements. Angle Orthod. 1994, 64, 333–342. [Google Scholar]
- Wood, D.P.; Korne, P.H. Estimated and true hinge axis: A comparison of condylar displacements. Angle Orthod. 1992, 62, 167–175, discussion 176. [Google Scholar]
- Okeson, J.P. Management of Temporomandibular Disorders and Occlusion, 8th ed.; Elsevier: St. Louis, MO, USA, 2019. [Google Scholar]
- Ackerman, J.L.; Proffit, W.R. Soft tissue limitations in orthodontics: Treatment planning guidelines. Angle Orthod. 1997, 67, 327–336. [Google Scholar] [PubMed]
- Roth, R.H. Occlusion and condylar position. Am. J. Orthod. Dentofac. Orthop. 1995, 107, 315–318. [Google Scholar] [CrossRef]
- Zonnenberg, A.J.J.; Türp, J.C.; Greene, C.S. Centric relation critically revisited-What are the clinical implications? J. Oral Rehabil. 2021, 48, 1050–1055. [Google Scholar] [CrossRef]
- Ponces, M.J.; Tavares, J.P.; Lopes, J.D.; Ferreira, A.P. Comparison of condylar displacement between three biotypological facial groups by using mounted models and a mandibular position indicator. Korean J. Orthod. 2014, 44, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Weffort, S.Y.; de Fantini, S.M. Condylar displacement between centric relation and maximum intercuspation in symptomatic and asymptomatic individuals. Angle Orthod. 2010, 80, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Cordray, F.E. Most condylar discrepancies not detectable clinically. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 15A. [Google Scholar] [CrossRef] [PubMed]
- Cordray, F.E. The importance of the seated condylar position in orthodontic correction. Quintessence Int. 2002, 33, 284–293. [Google Scholar] [PubMed]
- Rinchuse, D.J.; Kandasamy, S. Articulators in orthodontics: An evidence-based perspective. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 299–308. [Google Scholar] [CrossRef]
- Rinchuse, D.J.; Kandasamy, S. Orthodontic dental casts: The case against routine articulator mounting. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Suvinen, T.I.; Reade, P.C.; Kemppainen, P.; Könönen, M.; Dworkin, S.F. Review of aetiological concepts of temporomandibular pain disorders: Towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J. Pain 2005, 9, 613–633. [Google Scholar] [CrossRef]
- Golanska, P.; Saczuk, K.; Domarecka, M.; Kuć, J.; Lukomska-Szymanska, M. Temporomandibular Myofascial Pain Syndrome-Aetiology and Biopsychosocial Modulation. A Narrative Review. Int. J. Env. Res. Public Health 2021, 18, 7807. [Google Scholar] [CrossRef] [PubMed]
- Padala, S.; Padmanabhan, S.; Chithranjan, A.B. Comparative evaluation of condylar position in symptomatic (TMJ dysfunction) and asymptomatic individuals. Indian J. Dent. Res. 2012, 23, 122. [Google Scholar] [PubMed]
- He, S.S.; Deng, X.; Wamalwa, P.; Chen, S. Correlation between centric relation–maximum intercuspation discrepancy and temporomandibular joint dysfunction. Acta Odontol. Scand. 2010, 68, 368–376. [Google Scholar] [CrossRef]
- Cordray, F.E. Articulated dental cast analysis of asymptomatic and symptomatic populations. Int. J. Oral Sci. 2016, 8, 126–132. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Alzaid, A.A.; Campbell, S.D. The Relationship Between Centric Occlusion and The Maximal Intercuspal Position and Their Use as Treatment Positions for Complete Mouth Rehabilitation: Best Evidence Consensus Statement. J. Prosthodont. 2021, 30, 26–33. [Google Scholar] [CrossRef]
- Maruyama, T.; Miyauchi, S.; Umekoji, E. Analysis of the mandibular relationship of TMJ dysfunction patients using the Mandibular Kinesiograph. J. Oral Rehabil. 1982, 9, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Crawford, S.D. Condylar axis position, as determined by the occlusion and measured by the CPI instrument, and signs and symptoms of temporomandibular dysfunction. Angle Orthod. 1999, 69, 103–115, discussion 115–116. [Google Scholar] [PubMed]
- Cordray, F.E. Three-dimensional analysis of models articulated in the seated condylar position from a deprogrammed asymptomatic population: A prospective study. Part 1. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 619–630. [Google Scholar] [CrossRef]
- Aboalnaga, A.A.; Amer, N.M.; Alhammadi, M.S.; Fayed, M.M.S. Positional and dimensional TMJ characteristics in different temporomandibular disorders: A cross-sectional comparative study. Cranio J. Craniomandib. Sleep Pract. 2022, ahead of print, 1–9. [Google Scholar] [CrossRef]
- Celić, R.; Jerolimov, V.; Pandurić, J. A study of the influence of occlusal factors and parafunctional habits on the prevalence of signs and symptoms of TMD. Int. J. Prosthodont. 2002, 15, 43–48. [Google Scholar] [PubMed]
- Miller, J.R.; Burgess, J.A.; Critchlow, C.W. Association between mandibular retrognathia and TMJ disorders in adult females. J. Public Health Dent. 2004, 64, 157–163. [Google Scholar] [CrossRef]
- Egermark, I.; Magnusson, T.; Carlsson, G.E. A 20-year follow-up of signs and symptoms of temporomandibular disorders and malocclusions in subjects with and without orthodontic treatment in childhood. Angle Orthod. 2003, 73, 109–115. [Google Scholar]
- Abrahamsson, C.; Henrikson, T.; Nilner, M.; Sunzel, B.; Bondemark, L.; Ekberg, E.C. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int. J. Oral Maxillofac. Surg. 2013, 42, 752–758. [Google Scholar] [CrossRef]
- Lai, Y.C.; Yap, A.U.; Türp, J.C. Prevalence of temporomandibular disorders in patients seeking orthodontic treatment: A systematic review. J. Oral Rehabil. 2020, 47, 270–280. [Google Scholar] [CrossRef]
- Manfredini, D.; Segu, M.; Arveda, N.; Lombardo, L.; Siciliani, G.; Rossi, A.; Guarda-Nardini, L. Temporomandibular Joint Disorders in Patients With Different Facial Morphology. A Systematic Review of the Literature. J. Oral Maxillofac. Surg. 2016, 74, 29–46. [Google Scholar] [CrossRef] [PubMed]
- Michelotti, A.; Rongo, R.; D’Antò, V.; Bucci, R. Occlusion, orthodontics, and temporomandibular disorders: Cutting edge of the current evidence. J. World Fed. Orthod. 2020, 9, S15–S18. [Google Scholar] [CrossRef]
- Jiménez-Silva, A.; Tobar-Reyes, J.; Vivanco-Coke, S.; Pastén-Castro, E.; Palomino-Montenegro, H. Centric relation-intercuspal position discrepancy and its relationship with temporomandibular disorders. A systematic review. Acta Odontol Scand. 2017, 75, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.R.; Moore, R.N.; DuBois, L.M. Mandibular condyle position: Comparison of articulator mountings and magnetic resonance imaging. Am. J. Orthod. Dentofac. Orthop. 1993, 104, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Kandasamy, S.; Greene, C.S.; Obrez, A. An evidence-based evaluation of the concept of centric relation in the 21st century. Quintessence Int. 2018, 49, 755–760. [Google Scholar] [PubMed]
- Yap, A.U.; Chen, C.; Wong, H.C.; Yow, M.; Tan, E. Temporomandibular disorders in prospective orthodontic patients. Angle Orthod. 2021, 91, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Paknahad, M.; Shahidi, S.; Abbaszade, H. Correlation between condylar position and different sagittal skeletal facial types. J. Orofac. Orthop. Fortschr. Kieferorthopadie 2016, 77, 350–356. [Google Scholar] [CrossRef]
- Paknahad, M.; Shahidi, S. Association between condylar position and vertical skeletal craniofacial morphology: A cone beam computed tomography study. Int. Orthod. 2017, 15, 740–751. [Google Scholar] [CrossRef]
- Park, I.; Kim, J.; Park, Y. Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern. Korean J. Orthod. 2015, 45, 66–73. [Google Scholar] [CrossRef]
- Burke, G.; Major, P.; Glover, K.; Prasad, N. Correlations between condylar characteristics and facial morphology in Class II preadolescent patients. Am. J. Orthod. Dentofac. Orthop. 1998, 114, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.J.; Baek, S.H.; Kim, T.W.; Nahm, D.S. Discrimination of internal derangement of temporomandibular joint by lateral cephalometric analysis. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 331–339. [Google Scholar] [CrossRef]
- Hwang, C.J.; Sung, S.J.; Kim, S.J. Lateral cephalometric characteristics of malocclusion patients with temporomandibular joint disorder symptoms. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 497–503. [Google Scholar] [CrossRef]
- Stringert, H.G.; Worms, F.W. Variations in skeletal and dental patterns in patients with structural and functional alterations of the temporomandibular joint: A preliminary report. Am. J. Orthod. 1986, 89, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Gidarakou, I.K.; Tallents, R.H.; Kyrkanides, S.; Stein, S.; Moss, M. Comparison of skeletal and dental morphology in asymptomatic volunteers and symptomatic patients with bilateral degenerative joint disease. Angle Orthod. 2003, 73, 71–78. [Google Scholar]
- Hidaka, O.; Adachi, S.; Takada, K. The difference in condylar position between centric relation and centric occlusion in pretreatment Japanese orthodontic patients. Angle Orthod. 2002, 72, 295–301. [Google Scholar]
- Aboalnaga, A.A.; Amer, N.M.; Elnahas, M.O.; Salah Fayed, M.M.; Soliman, S.A.; El Dakroury, A.E.; Labib, A.H. Fahim, F.H. Malocclusion and Temporomandibular Disorders: Verification of the Controversy. J. Oral Facial Pain Headache 2019, 33, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Utt, T.W.; Meyers, C.E.; Jr Wierzba, T.F.; Hondrum, S.O. A three-dimensional comparison of condylar position changes between centric relation and centric occlusion using the mandibular position indicator. Am. J. Orthod Dentofac. Orthop. 1995, 107, 298–308. [Google Scholar] [CrossRef]
- Girardot, A. The nature of condylar displacement in patients with temporomandibular pain-dysfunction. Orthod. Rev. 1987, 1, 16–23. [Google Scholar] [PubMed]
- Karl, P.J.; Foley, T.F. The use of a deprogramming appliance to obtain centric relation records. Angle Orthod. 1999, 69, 117–124, discussion 124–125. [Google Scholar]
- Wood, D.P.; Elliott, R.W. Reproducibility of the centric relation bite registration technique. Angle Orthod. 1994, 64, 211–220. [Google Scholar] [PubMed]
- Hicks, S.T.; Wood, D.P. Recording condylar movement with two facebow systems. Angle Orthod. 1996, 66, 293–300. [Google Scholar]
- Rosner, D.; Goldberg, G.F. Condylar retruded contact position and intercuspal position correlation in dentulous patients. Part I: Three-dimensional analysis of condylar registrations. J. Prosthet. Dent. 1986, 56, 230–239. [Google Scholar] [CrossRef] [PubMed]
- Dawson, P.E. A classification system for occlusions that relates maximal intercuspation to the position and condition of the temporomandibular joints. J. Prosthet. Dent. 1996, 75, 60–66. [Google Scholar] [CrossRef] [PubMed]
- He, H.; Fu, M. Analysis of the mandibular position in malocclusion patients. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2000, 3, 34–39. [Google Scholar]
- Rosner, D. Hinge axis translation from retruded contact position to intercuspal position in dentulous subjects in treatment. J. Prosthet. Dent. 1982, 48, 713–718. [Google Scholar] [CrossRef]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef]
- Chandra, S.; Shahi, A.K. Centric Relation in Asymptomatic Hypodivergent and Hyperdivergent Skeletal Pattern. Int. J. Sci. Study 2016, 3, 6–12. [Google Scholar]
- Girardot, R.A., Jr. Comparison of condylar position in hyperdivergent and hypodivergent facial skeletal types. Angle Orthod. 2001, 71, 240–246. [Google Scholar]
- Barrera-Mora, J.M.; Escalona, E.E.; Labruzzi, C.A.; Carrera, J.M.L.; Ballesteros, E.J.C.; Reina, E.S.; Rocabado, M. The Relationship Between Malocclusion, Benign Joint Hypermobility Syndrome, Condylar Position and TMD Symptoms. Cranio J. Craniomandib. Sleep Pract. 2012, 30, 121–130. [Google Scholar] [CrossRef]
- Radej, I.; Szarmach, I. The Role of Maxillofacial Structure on Condylar Displacement in Maximum Intercuspation and Centric Relation. Biomed. Res. Int. 2022, 2022, 1439203. [Google Scholar] [CrossRef]
- Ari-Demirkaya, A.; Biren, S.; Ozkan, H.; Küçükkeleş, N. Comparison of deep bite and open bite cases: Normative data for condylar positions, paths and radiographic appearances. J. Oral Rehabil. 2004, 31, 213–224. [Google Scholar] [CrossRef]
- Turasi, B.; Ari-Demirkaya, A.; Biren, S. Comparison of increased overjet cases and controls: Normative data for condylar positions. J. Oral Rehabil. 2007, 34, 129–135. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Fayed, M.S.; Labib, A. Three-dimensional assessment of condylar position and joint spaces after maxillary first premolar extraction in skeletal Class II malocclusion. Orthod. Craniofacial Res. 2017, 20, 71–78. [Google Scholar] [CrossRef]
- Gurbanov, V.; Bas, B.; Öz, A.A. Evaluation of Stresses on Temporomandibular Joint in the Use of Class II and III Orthodontic Elastics: A Three-Dimensional Finite Element Study. J. Oral Maxillofac. Surg. 2020, 78, 705–716. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, D.; Lombardo, L.; Siciliani, G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: End of an era? J. Oral Rehabil. 2017, 44, 908–923. [Google Scholar] [CrossRef] [PubMed]
- Dygas, S.; Szarmach, I.; Radej, I. Assessment of the Morphology and Degenerative Changes in the Temporomandibular Joint Using CBCT according to the Orthodontic Approach: A Scoping Review. Biomed. Res. Int. 2022, 2022, 6863014. [Google Scholar] [CrossRef] [PubMed]
- Afzal, A.; Qamruddin, I. Relation between centric slide and angle’s classification. J. Coll. Physicians Surg. Pakistan. 2005, 15, 481–484. [Google Scholar]
- Pullinger, A.G.; Seligman, D.A.; Gornbein, J.A. A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J. Dent. Res. 1993, 72, 968–979. [Google Scholar] [CrossRef]
- Ackerman, J.L.; Proffit, W.R. The characteristics of malocclusion: A modern approach to classification and diagnosis. Am. J. Orthod. 1969, 56, 443–454. [Google Scholar] [CrossRef]
- Klar, N.A.; Kulbersh, R.; Freeland, T.; Kaczynski, R. Maximum intercuspation-centric relation disharmony in 200 consecutively finished cases in a gnathologically oriented practice. Semin. Orthod. 2003, 9, 109–116. [Google Scholar] [CrossRef]
- Severt, T.R.; Proffit, W.R. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int. J. Adult Orthodon. Orthognath. Surg. 1997, 12, 171–176. [Google Scholar]
- Haraguchi, S.; Takada, K.; Yasuda, Y. Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 2002, 72, 28–35. [Google Scholar] [PubMed]
- Ishizaki, K.; Suzuki, K.; Mito, T.; Tanaka, E.M.; Sato, S. Morphologic, functional, and occlusal characterization of mandibular lateral displacement malocclusion. Am. J. Orthod. Dentofac. Orthop. 2010, 137, e1–e9, discussion 454–455. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Papers evaluating effects of orthodontic variables on condylar displacement using a mandibular or condylar position indicator: (i) Cephalometric variables (ii) Malocclusion | (i) Not original articles (ii) Articles published in languages other than English (iii) Articles not conforming with PICO (iiii) Case reports, books, reviews |
| Ponces et al. [14] | Chandra et al. [61] | Girardot [62] | Radej et al. [64] | Hidaka et al. [49] | Ari-Demirkaya et al. [65] | Barrera-Mora et al. [63] | Utt et al. [51] | He et al. [58] | Turasi et al. [66] | |
|---|---|---|---|---|---|---|---|---|---|---|
| Was the sample frame appropriate to address the target population? | Y | Y | Y | Y | U | U | Y | U | Y | U |
| Were study participants sampled in an appropriate way? | Y | Y | Y | Y | Y | U | Y | Y | Y | U |
| Was the sample size adequate? | Y | Y | Y | U | Y | Y | Y | Y | U | Y |
| Were the study subjects and the setting described in detail? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the data analysis conducted with sufficient coverage of the identified sample? | Y | Y | Y | U | Y | Y | Y | Y | Y | Y |
| Were valid methods used for the identification of the condition? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was the condition measured in a standard, reliable way for all participants? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Was there appropriate statistical analysis? | Y | Y | Y | Y | Y | Y | Y | U | Y | Y |
| Was the response rate adequate, and if not, was the low response rate managed appropriately? | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| Author | Aim of Study | Country of Origin | Age (y.o) | TMD Symptoms | Number of Assessed patients/Joints | Main Group of Division | Assessed Variable CD | Method of Registering CR | Method of Deprogramming | Main Correlations and Conclusions |
|---|---|---|---|---|---|---|---|---|---|---|
| Ponces et al. [14] | Clarify the relationship between facial type and condylar position. | Portugal | 12–46.2 (adolescents and adults) | asymptomatic | 108/216 (36/72 per group) | hyperdivergent, hypodivergent and intermediate skeletal facial type | x, z | Roth’s power centric | 10-min interposition of cotton roles | More extensive CD in the hyperdivergent group in the vertical dimension than hypodivergent and intermediate *. More extensive CD in the hypodivergent group in the horizontal dimension. No significant difference in horizontal displacement between groups. |
| Chandra et al. [61] | Evaluate and compare the CR and centric occlusion (CO) in asymptomatic subjects with hyperdivergent and hypodivergent facial skeletal type. | India | 16–30 (young adult having completed growth) | asymptomatic | 70/140 (35/70 per group) | hyperdivergent and hypodivergent skeletal facial type | x, y, z | modified Roth’s power centric | 10-min interposition of cotton roles | Hyperdivergent subjects had greater displacement of the condyle in the horizontal dimensions *. Hyperdivergent subjects had greater rearward movement of the condyle *. Hyperdivergent subjects had greater displacement of the condyle in the vertical plane *. No differences between the groups in the medio-lateral dimension. |
| Girardot [62] | Determine if the CR to intercuspal position discrepancy was larger in patients with hyperdivergent facial type compared with patients with hypodivergent facial type. | USA | 13–36 (young adult having completed or nearly completed growth) | asymptomatic | 66 (33 per group) | hyperdivergent and hypodivergent skeletal facial type | x, z | modified Roth’s power centric | n/a | There was a statistically significant greater distraction of the condyles in the hyperdivergent group in both the horizontal and vertical planes. |
| Radej et al. [64] | To evaluate the impact of the craniofacial structure and occlusal conditions on the position of the mandibular condyles’ articular heads in the MIP and compare the CR and MIP of the mandibular condyles prior to orthodontic treatment. | Poland | 11.5–50.3 | asymptomatic and symptomatic | 48/96 | 1. Helkimo Di0 and Di1 or Helkimo DiII or DiIII 2. Skeletal class I, II, III (ANB angle) 3. Hyper, normal and hypodivergent (SGo/NMe) 4. Posterior, normal and anteriorotation (SN/ML) 5. Angle’s classification I, II, II(1/2 unit), III, III(1/2) unit 6. Cross-bite and lingual occlusion or normal occlusion | x, y, z | Roth’s power centric | pulsatile biting of wooden spatula for a 10–15 min | 1. No correlation of CD with cephalometric measurements (ANB, SN-ML, SGo/NMe). 2. Correlation between CD in the transverse axis and SN-ML angle *. 3. Correlation between CD in anteroposterior axis and a midline shift of the mandible *. 4. Correlation between Angle’s classification of molar position on the right side and anteroposterior CD values *. Cephalometric measurements (ANB, Sgo/NMe, and SN-ML) do not provide sufficient information to predict the frequency, size, and direction of CD at the level of the condylar processes. Cast analysis in an articulator is particularly desirable in patients with Angle class I, in whom an anterior CD may mask the occurrence of an Angle class II in CR. It would allow an assessment of whether the malocclusion is the result of an eccentric shift of the mandible, in which the asymmetrical displacement of the condyles results in a mandibular midline shift. |
| Hidaka et al. [49] | Report the frequency, magnitude, and laterality of differences in condylar position between CO and CR before orthodontic treatment. Investigate how the differences vary according to age, gender, mandibular plane angle, or Angle classification. Compare the results with those of the Caucasian race. | Japan | 6.7–57.8 | n/a | 150 | age, gender, SN to mandibular plane angle, Angle classification | x, y, z | Roth’s power centric | n/a | No significant differences in the magnitude of CPI measurements were found among any set of groups. Angle class III subjects tended to have significant condylar displacement toward the left side *. The frequency, magnitude, or direction of CO-CR changes at the level of the condyles cannot be predicted by age, gender, Angle classification, ANB angle, or mandibular plane angle. |
| Ari-Demirkaya et al. [65] | Compare normal overbite, deep bite, and open bite cases clinically healthy TMJ regarding the difference between condylar positions in CR and CO, condylar paths, and radiographic findings of condylar appearance in order to establish normative data. | Turkey | 18–32 (adults) | asymptomatic | 90/180 (30/60 per group) | Normal overbite, deep bite, and open bite | x, y, z | bilateral manipulation technique described by Dawson | 10-min interposition of cotton roles | Open bite cases show larger vertical CR–CO slides and shorter protrusion paths than normal and deep overbite cases. The clinician should pay special attention to the TMJ status of open bite patients. |
| Barrera-Mora et al. [63] | To determine the association between TMD symptoms and condylar position, dento-skeletal malocclusion pattern, and benign joint hypermobility syndrome. | Spain | 20–30 | asymptomatic and symptomatic | 162 (140 + 22 control group) | gender, degree of hypermobility joint, joint dysfunction parameters of the TMJ, malocclusion pattern at dento-skeletal level: skeletal class (I, II, III), malocclusions (normal occlusion, class I, II, III, open bite), sagittal malocclusion (normal overjet, anterior crossbite, increased overjet) | x, y, z, h | Roth’s power centric | n/a | No statistically significant relationship between benign joint hypermobility syndrome and the amount of condylar displacement or TMD, but such a relationship does exist with malocclusion patterns, especially, malocclusion Class II and open bite. Anterior crossbite and condylar displacements in the vertical plane are risk factors in developing TMJ symptoms. |
| Utt et al. [51] | Make a three-dimensional comparison of condylar position in CO relative to the clinically captured CR on patients before initiation of orthodontic treatment. Report the frequency and magnitude of the differences between CO and CR positions at the level of the condyles, and examine the relationship of condylar position changes to other factors routinely available and traditionally considered by orthodontists before treatment. | USA | 7.75–38.17 | n/a | 107 | Angle classification, ANB angular measurement, age, gender | x, y, z | Roth’s power centric | n/a | Patient age, ANB angle, gender, or Angle classification cannot be used to predict frequency, magnitude, or direction of CO-CR changes at the level of the condyles. |
| He et al. [58] | Study the changes of condyle position and occlusion between CR and MI positions. | China | 14.5–18.5 | asymptomatic | 50 (25 per group) | Angle class I Angle class II | x, y, z | Roth’s power centric | n/a | When the mandible moved from CR to MI, overbite deepened, overjet decreased, and molar relationship became mesialized. No significant difference between Angle Class I and Angle Class II patients was observed in condylar position and occlusion changes. |
| Turasi et al. [66] | Compare normal overjet versus large overjet cases with clinically healthy temporomandibular joints; to establish normative data regarding the difference between condylar positions in CO and maximum intercuspation and deflective CO contacts. | Turkey | 18–29 | asymptomatic | 66 (33 per group) | large and normal overjet group | x, y, z | bilateral manipulation technique described by Dawson | 10-min interposition of cotton roles | Patients with increased overjet show some significant differences in the range and direction of CR-CO slides compared with normal overjet patients, even in healthy TMD-free cases. This study indicates that the clinician should pay special attention to the TMJ status of patients with a large overjet. |
| Author | Mean Delta x | Mean Delta z | Mean Delta y | Predominant Direction of Movement |
|---|---|---|---|---|
| Ponces et al. [14] | 0.84 hyperdivergent group 0.94 hypodivergent group | 1.65 * hyperdivergent group 1.05 hypodivergent group | n/a | posterior in the hyperdivergent and intermediate groups, anterior in the hypodivergent group |
| Chandra et al. [61] | 1.13 * hyperdivergent group (0.63 forward movement) (1.53 backward movement) 0.65 * hypodivergent group (0.95 forward movement) 0.44 backward movement) | 1.46 * hyperdivergent group 0.99 * hypodivergent group | 0.38 hyperdivergent group 0.39 hypodivergent group | n/a |
| Girardot [62] | 1.21 * hyperdivergent group (37.25 total forward movement) (42.5 total backward movement) 0.66 hypodivergent group (17.5 total forward movement) (26.3 total backward movement) | 1.7 * hyperdivergent group 1.2 hypodivergent group | n/a | n/a |
| Radej et al. [64] | 0.15: 0.18 anterorotation group 0.06 normal rotation group 0.64 posterorotation group 0.35 Angle class I right −0.26 * Angle class II right 0.31 Angle class III right | 0.76: 0.58 anteriorotation group 0.75 normal rotation group 1.32 posterorotation group 0.65 Angle class I right 0.79 Angle class II right 0.96 Angle class III right | −0.01: −0.13 anterorotation group 0.00 normal rotation group 0.26 * posterorotation group 0.04 Angle class I right −0.08 Angle class II right −0.07 Angle class III right | anteroinferior |
| Hidaka et al. [49] | −0.1 left 0.2 right | 1.0 left * 0.9 right * | 0.1 Angle class I 0.0 Angle class II −0.2 * Angle class III | downward with a smaller antero-posterior component |
| Ari-Demirkaya et al. [65] | 0.85 open bite group 0.78 deep bite group | 1.01 * open bite group 0.79 deep bite group | 0.54 open bite group 0.68 deep bite group | downward and forward |
| Barrera-Mora et al. [63] | n/a | n/a | 0.26 normal overjet 0.4 anterior crossbite * 0.15 increased overjet * | n/a |
| Utt et al. [51] | 0.59/0.59 Angle class I right/left 0.63/0.64 Angle class II right/left 0.62/0.62 Angle class II/1 right/left 0.7/0.75 Angle class II/2 right/left | 0.75/0.75 Angle class I right/left 0.91/0.88 Angle class II right/left 0.87/0.85 Angle class II/1 right/left 1.16/1.10 Angle class II/2 right/left | 0.26 Angle class I 0.27 Angle class II 0.27 Angle class II/1 0.25 Angle class II/2 | posteroinferior |
| He et al. [58] | 1.29 left 1.25 right | 1.59 left 1.56 right * | 0.59 | posterior and inferior |
| Turasi et al. [66] | 0.97 large overjet group 0.73 control group | 0.97 * large overjet group 0.64 control group | 0.86 * large overjet group 0.52 control group | downward and backward |
| Author | Number of Joints with Extreme Horizontal Displacement above or below 2 mm | Number of Joints with Extreme Vertical Displacement above 2 mm | Number of Joints with Extreme Transverse Displacement above 0.5 mm |
|---|---|---|---|
| Ponces et al. [14] | 14 (6.49%) Hyperdivergent group: 3 (4.17%) -posterior: 2 (2.78%) -anterior: 1 (1.39%) Hypodivergent group: 6 (8.33%) -posterior: 0 -anterior: 6 (8.33%) Intermediate group: 5 (6.9 4%) -posterior: 3 (4.17%) -anterior: 2 (2.78%) | 60 (27.77%) Hyperdivergent 25 (34.72%) Hypodivergent 17 (23.61%) Intermediate 18 (25%) | n/a |
| Chandra et al. [61] | 18 (12.86%) Hyperdivergent group: 15 (10.71%) Hypodivergent group: 3 (2.14%) | 21 (15%) Hyperdivergent group: 15 (21.43%) Hypodivergent group: 6 (8.57%) | n/a |
| Girardot [62] | 20/66 (30.3%) Hyperdivergent group: 16/33 (48.48%) -posterior: 10/33 (30.3%) -anterior: 6/33 (18.18%) Hypodivergent group: 4/33 (12.12%) -posterior: 3/33 (9.09%) -anterior: 1/33 (3.03%) | 24/66 (36.36%) Hyperdivergent: 19/33 (57.57%) Hypodivergent: 5/33 (15.15%) | n/a |
| Radej et al. [64] | 1 (1%) | 6 (6.3%) | 6 (6.3%) |
| Hidaka et al. [49] | 1 (0.7%) left side 2 (1.3%) right side | 14 (9.3%) left side 11 (7.3%) right side | 47 (31.3%) |
| Barrera-Mora et al. [63] | n/a | n/a | n/a |
| Utt et al. [51] | 5 (16.1%) Angle class I 15 (20.8%) Angle class II | n/a | 17 (15.9%) 4 (12.9%) Angle class I 7 (11.3%) Angle class II |
| He et al. [58] | 18% left side 17% right side | 31% left side 28% right side | 48% |
| Author | Number of Joints with Vertical CR-CO Slide >1 mm | Number of Joints with Anteroposterior CR-CO Slide > 1 mm | Number of Joints with Transverse CR-CO slide > 1 mm |
|---|---|---|---|
| Ari-Demirkaya et al. [65] | Open bite group: 50% * Deep bite group: 27% Control group: 17% | No difference between groups | Open bite group: 13% Deep bite group: 33% Control group: 13% |
| Turasi et al. [66] | 39% overjet group 18% control group | 39% overjet group 24% control group | 33% overjet group 15% control group |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radej, I.; Dargiewicz, E.; Sawczuk-Siemieniuk, M.; Ferrando Cascales, R.; Ferrando Cascales, Á.; Agustín-Panadero, R.; Szarmach, I. The Role of Maxillofacial Structure and Malocclusion on Condylar Displacement in Maximum Intercuspation and Centric Relation in Patients Seeking Orthodontic Treatment—A Scoping Review. J. Clin. Med. 2023, 12, 689. https://doi.org/10.3390/jcm12020689
Radej I, Dargiewicz E, Sawczuk-Siemieniuk M, Ferrando Cascales R, Ferrando Cascales Á, Agustín-Panadero R, Szarmach I. The Role of Maxillofacial Structure and Malocclusion on Condylar Displacement in Maximum Intercuspation and Centric Relation in Patients Seeking Orthodontic Treatment—A Scoping Review. Journal of Clinical Medicine. 2023; 12(2):689. https://doi.org/10.3390/jcm12020689
Chicago/Turabian StyleRadej, Ilona, Ewelina Dargiewicz, Magdalena Sawczuk-Siemieniuk, Raúl Ferrando Cascales, Álvaro Ferrando Cascales, Rubén Agustín-Panadero, and Izabela Szarmach. 2023. "The Role of Maxillofacial Structure and Malocclusion on Condylar Displacement in Maximum Intercuspation and Centric Relation in Patients Seeking Orthodontic Treatment—A Scoping Review" Journal of Clinical Medicine 12, no. 2: 689. https://doi.org/10.3390/jcm12020689
APA StyleRadej, I., Dargiewicz, E., Sawczuk-Siemieniuk, M., Ferrando Cascales, R., Ferrando Cascales, Á., Agustín-Panadero, R., & Szarmach, I. (2023). The Role of Maxillofacial Structure and Malocclusion on Condylar Displacement in Maximum Intercuspation and Centric Relation in Patients Seeking Orthodontic Treatment—A Scoping Review. Journal of Clinical Medicine, 12(2), 689. https://doi.org/10.3390/jcm12020689








