Prediction of Tubal Rupture in Ectopic Pregnancy Using Methotrexate Treatment Protocols and Hematological Markers
Abstract
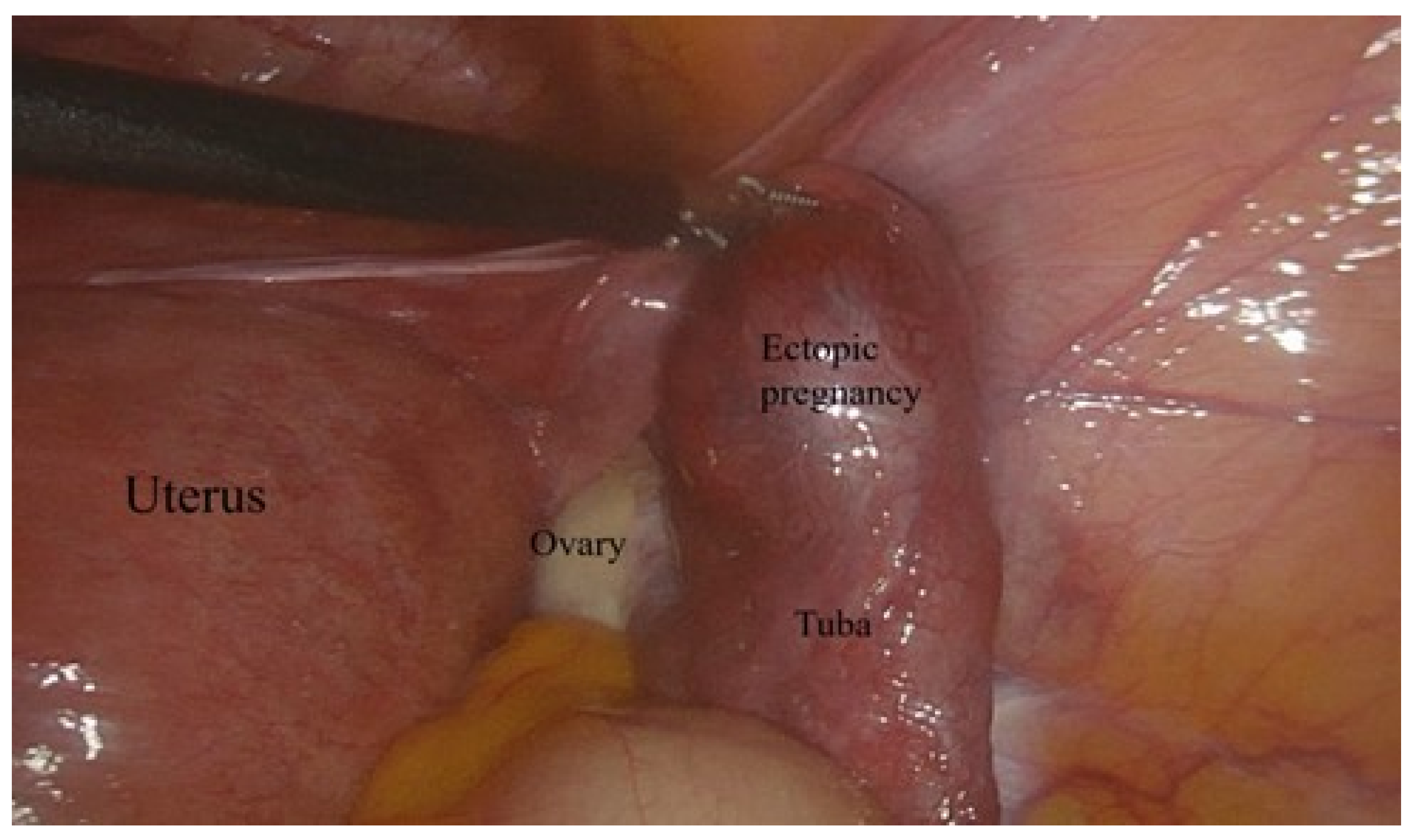
:1. Introduction
2. Materials and Methods
Methotrexate Treatment Protocols
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bachman, E.A.; Barnhart, K. Medical Management of Ectopic Pregnancy: A Comparison of Regimens. Clin. Obstet. Gynecol. 2012, 55, 440. [Google Scholar] [CrossRef] [PubMed]
- Mullany, K.; Minneci, M.; Monjazeb, R.; Coiado, C.O. Overview of Ectopic Pregnancy Diagnosis, Management, and Innovation. Women’s Health 2023, 19, 17455057231160349. [Google Scholar] [CrossRef] [PubMed]
- Kingsbury, B.; Sam, D.; Jeyasudha, R.; Thomas, E.; Rebekah, G.; Lionel, J. Ectopic Pregnancies: Catch Them Early, Treat Them Wisely! J. Fam. Med. Prim. Care 2020, 9, 4911–4918. [Google Scholar] [CrossRef]
- Akkaya, H.; Uysal, G. Can Hematologic Parameters Predict Treatment of Ectopic Pregnancy? Pak. J. Med. Sci. 2017, 33, 937–942. [Google Scholar] [CrossRef] [PubMed]
- Alkatout, I.; Honemeyer, U.; Strauss, A.; Tinelli, A.; Malvasi, A.; Jonat, W.; Mettler, L.; Schollmeyer, T. Clinical Diagnosis and Treatment of Ectopic Pregnancy. Obstet. Gynecol. Surv. 2013, 68, 571–581. [Google Scholar] [CrossRef]
- Leziak, M.; Żak, K.; Frankowska, K.; Ziółkiewicz, A.; Perczyńska, W.; Abramiuk, M.; Tarkowski, R.; Kułak, K. Future Perspectives of Ectopic Pregnancy Treatment—Review of Possible Pharmacological Methods. Int. J. Environ. Res. Public. Health 2022, 19, 14230. [Google Scholar] [CrossRef]
- David, M. Ectopic Pregnancies: Current Diagnostics and Treatment. Gynakologie 2023, 56, 462–470. [Google Scholar] [CrossRef]
- Eskicioglu, F.; Turan, G.A.; Gur, E.B. The Efficacy of Platelet Activation Indicators for the Diagnosis of Tubal Ectopic Pregnancy. Pak. J. Med. Sci. 2015, 31, 745. [Google Scholar] [CrossRef]
- Eskicioğlu, F.; Özdemir, A.T.; Turan, G.A.; Gür, E.B.; Kasap, E.; Genç, M. The Efficacy of Complete Blood Count Parameters in the Diagnosis of Tubal Ectopic Pregnancy. Ginekol. Pol. 2014, 85, 823–827. [Google Scholar] [CrossRef]
- Ayar Madenli, A.; Çali Öztürk, H. The Evaluation of Success and Failure of Methotrexate Treatment in Ectopic Pregnancy. Anatol. Curr. Med. J. 2022, 4, 449–454. [Google Scholar] [CrossRef]
- Khani, B.; Behnamfar, F.; Taghiyar, L. Which Protocol Is Better for Treatment of Ectopic Pregnancy by Methotrexate? Single-Dose or Multiple-Dose. Adv. Biomed. Res. 2020, 9, 59. [Google Scholar] [CrossRef]
- Frías Sánchez, Z.; Pantoja Garrido, M.; Fernández Ruiz, M.; Vico de Miguel, F.J.; Pantoja Rosso, F.J. Management of Cervical Ectopic Pregnancy. Medical Treatment with a Multiple-Dose Regimen of Intramuscular Methotrexate: A Case Report. Clin. Investig. Ginecol. Obstet. 2019, 46, 81–85. [Google Scholar] [CrossRef]
- Laibl, V.; Takacs, P.; Kang, J. Previous Ectopic Pregnancy as a Predictor of Methotrexate Failure. Int. J. Gynecol. Obstet. 2004, 85, 177–178. [Google Scholar] [CrossRef] [PubMed]
- Boychuk, A.V.; Khlibovska, O.I.; Yakymchuk, Y.B. Ectopic Pregnancy and Its Long-Term Results. Wiad. Lek. 2020, 73, 139–144. [Google Scholar] [CrossRef]
- Lüdke, D.; Yan, Q.; Rohmann, P.F.W.; Wiermer, M. NLR We There yet? Nucleocytoplasmic Coordination of NLR-Mediated Immunity. New Phytol. 2022, 236, 24–42. [Google Scholar] [CrossRef]
- Yuk, J.S.; Lee, J.H.; Park, W.I.; Ahn, H.S.; Kim, H.J. Systematic Review and Meta-Analysis of Single-Dose and Non-Single-Dose Methotrexate Protocols in the Treatment of Ectopic Pregnancy. Int. J. Gynecol. Obstet. 2018, 141, 295–303. [Google Scholar] [CrossRef]
- Yang, C.; Cai, J.; Geng, Y.; Gao, Y. Multiple-Dose and Double-Dose versus Single-Dose Administration of Methotrexate for the Treatment of Ectopic Pregnancy: A Systematic Review and Meta-Analysis. Reprod. Biomed. Online 2017, 34, 383–391. [Google Scholar] [CrossRef]
- Galstyan, K.; Kurzel, R.B. Serum Beta-HCC Titers Do Not Predict Ruptured Ectopic Pregnancy. Int. J. Fertil. Womens Med. 2006, 51, 14–16. [Google Scholar]
- Bibi, H.; Akhter, S.; Nasir, S.; Sadia, B. Efficacy of Methotrexate Treatment, Nonsurgical Treatment of Ectopic Pregnancy (EP). Pak. J. Med. Health Sci. 2022, 16, 161–163. [Google Scholar] [CrossRef]
- Yang, A.P.; Liu, J.; Tao, W.Q.; Li, H. ming The Diagnostic and Predictive Role of NLR, d-NLR and PLR in COVID-19 Patients. Int. Immunopharmacol. 2020, 84, 106504. [Google Scholar] [CrossRef]
- Kurtoglu, E.; Kokcu, A.; Celik, H.; Tosun, M.; Malatyalioglu, E. May Ratio of Neutrophil to Lymphocyte Be Useful in Predicting the Risk of Developing Preeclampsia? A Pilot Study. J. Matern. Fetal Neonatal Med. 2015, 28, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Kanmaz, A.G.; Inan, A.H.; Beyan, E.; Budak, A. Role of Various Complete Blood Count Parameters in Predicting the Success of Single-Dose Methotrexate in Treating Ectopic Pregnancy. Pak. J. Med. Sci. 2018, 34, 1132–1136. [Google Scholar] [CrossRef]
- Kan, Ö.; Gemici, A.; Alkilic, A.; Cetindag, E.N.; Cakir, C.; Dur, R.; Altay, M. The Effect of Preoperative Neutrophil-To-Lymphocyte Ratio and Platelet-To-Lymphocyte Ratio on Predicting Rupture Risk in Tubal Ectopic Pregnancies. Gynecol. Obstet. Invest. 2019, 84, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Hai, L.; Hu, Z.-D. The Clinical Utility of Neutrophil to Lymphocyte Ratio in Pregnancy Related Complications: A Mini-Review. J. Lab. Precis. Med. 2020, 5, 1. [Google Scholar] [CrossRef]
- Amin, K.M. Non-Surgical Treatment of Ectopic Pregnancy. Prensa Med. Argent. 2019, 105, 1325–1329. [Google Scholar] [CrossRef]
- Elito Júnior, J.; Ferreira, D.F.; Araujo Júnior, E.; Stavale, J.N.; Camano, L. Values of Beta-Human Chorionic Gonadotrofin as a Risk Factor for Tubal Pregnancy Rupture Evaluated by Histopathology. J. Matern. Fetal Neonatal Med. 2014, 27, 637–639. [Google Scholar] [CrossRef] [PubMed]
- Song, T.; Kim, M.K.; Kim, M.L.; Jung, Y.W.; Yun, B.S.; Seong, S.J. Single-Dose versus Two-Dose Administration of Methotrexate for the Treatment of Ectopic Pregnancy: A Randomized Controlled Trial. Human. Reprod. 2016, 31, dev312. [Google Scholar] [CrossRef] [PubMed]
- Li, P.C.; Lin, W.Y.; Ding, D.C. Risk Factors and Clinical Characteristics Associated with a Ruptured Ectopic Pregnancy: A 19-Year Retrospective Observational Study. Medicine 2022, 101, e29514. [Google Scholar] [CrossRef]

| Total | Group 1 Single-Dose MTX (n = 50), Mean ± SD | Group 2 Double-Dose MTX (n = 48), Mean ± SD | Group 3 Multiple-Dose MTX (n = 30), Mean ± SD | p-Value | |
|---|---|---|---|---|---|
| Age | 31.91 ± 5.93 | 31.06 ± 6.14 | 32.29 ± 6.19 | 33.04 ± 5.09 | 0.340 |
| Gravida | 2.55 ± 1.53 | 2.33 ± 1.56 | 2.39 ± 1.71 | 3.14 ± 1.04 | 0.114 |
| Parity | 1.11 ± 1.053 | 0.90 ± 0.968 | 1.03 ± 1.158 | 1.57 ± 0.945 | 0.048 |
| Initial β-hCG value (mIU/mL) | 5060.9 ± 1246.70 | 2763.6 ± 3342.46 | 6016.1 ± 3244.23 | 8654.1 ± 2304.63 | <0.001 |
| HGB (g/dL) | 12.1 ± 1.47 | 11.8 ± 1.62708 | 12.4 ± 1.32 | 12.4 ± 1.28 | 0.076 |
| HCT (%) | 36.7 ± 4.05 | 37.3 ± 3.27 | 37.7 ± 3.45 | 35.5 ± 4.68388 | 0.019 |
| MCV (fL) | 83.54 ± 9.71 | 84.92 ± 5.95 | 82.99 ± 10.98 | 79.9 ± 12.2 | 0.047 |
| MCH (pg) | 27.92 ± 3.27 | 28.2280 ± 2.41289 | 28.03 ± 4.03 | 27.33 ± 3.17 | 0.505 |
| MPV (fL) | 9.84 ± 1.27 | 9.6378 ± 1.21803 | 9.92 ± 1.29 | 9.99 ± 1.36 | 0.413 |
| PLT (K/mL) | 273 ± 624 | 262 ± 647 | 274 ± 548 | 284 ± 617 | 0.278 |
| WBC (K/μL) | 11.235 ± 11.059 | 12.594 ± 12.451 | 10.928 ± 12.691 | 9.672 ± 2.386 | 0.111 |
| PDW | 14.13 ± 4.54 | 13.91 ± 5.06 | 14.6 ± 5.02394 | 13.78 ± 2.6 | 0.529 |
| NLR | 3.57 ± 1.63 | 3.67 ± 1.98 | 2.8 ± 1.72 | 3.28 ± 1.88 | 0.192 |
| Variables | Rupture | p-Value | |
|---|---|---|---|
| No n = 92 (Mean ± SD)/(Min − Max) | Yes n = 36 (mean ± SD)/(Min − Max) | ||
| Age | 32.03 ± 6.21 | 31.85 ± 5.35 | 0.755 |
| BMI | 25.9 ± 3.28 | 24.1 ± 2.49 | 0.092 |
| Parity | 1.00 (0.00–5.00) | 1.00 (0.00–3.00) | 0.533 |
| HCT (%) | 37.188 ± 3.845 | 35.529 ± 4.373 | 0.038 |
| HGB (g/dL) | 12.298 ± 1.407 | 11.909 ± 1.600 | 0.182 |
| MCV (fL) | 86.50 (27.70–96.90) | 84.40 (73.50–97.30) | 0.340 |
| MCH (pg) | 29.00 (10.50–32.90) | 28.20 (23.10–33.10) | 0.246 |
| PLT (K/mL) | 266 (150–443) | 273 (160–476) | 0.716 |
| WBC (10^/uL) | 8.870 (7.31–94,600) | 9.900 (5690–46,800) | 0.057 |
| MPV (fL) | 10.10 (6.80–12.80) | 9.80 (7.20–12.60) | 0.263 |
| PDW | 12.90 (8.80–44.30) | 13.50 (9.00–41.30) | 0.567 |
| NLR | 2.50 (0.30–9.00) | 3.22 (0.75–11.32) | 0.030 |
| Initial β-hCG value (mIU/mL) | 5.171 (90–11.991) | 4.296 (33–20.421) | 0.879 |
| Time to negative β-hCG mIU/mL | 36 (10–155) | 32 (13–114) | 0.303 |
| 1 day | 3.558 (110–11.991) | 1.921 (560–19.097) | 0.669 |
| 4 days | 5.225 (102–15.502) | 4.996 (658–21.956) | 0.915 |
| 7 days | 5.856 (33–13.854) | 3.649 (102–14.264) | 0.428 |
| 9 days | 7.510 (76–48.604) | 3.178 (145–11.222) | 0.233 |
| Variables | Rupture | p-Value | ||
|---|---|---|---|---|
| No (n = 92) n (%) | Yes (n = 36) n (%) | |||
| History of ectopic pregnancy | 1 | 89 (96.7) | 33 (94.3) | 0.615 |
| ≥2 | 3 (3.3) | 3 (5.7) | ||
| History of tubal surgery | No | 89 (95.7) | 31 (88.6) | 0.213 |
| Yes | 3 (3.3) | 5 (11.4) | ||
| History of IUD | No | 75 (80.6) | 28 (80.0) | >0.999 |
| Yes | 17 (19.4) | 8 (20.0) | ||
| History of infertility | No | 72 (78.5) | 30 (82.9) | 0.806 |
| Yes | 20 (21.5) | 6 (17.1) | ||
| History of PID | No | 76 (82.8) | 31 (85.7) | 0.794 |
| Yes | 16 (17.2) | 5 (14.3) | ||
| Smoking | No | 69 (74.2) | 27 (77.1) | 0.822 |
| Yes | 23 (25.8) | 9 (22.9) | ||
| Tubal lumen measurement * | Unmeasurable | 42 (45.6) | 13 (36.2) | 0.788 |
| <35 mm | 35 (38.0) | 15 (41.6) | ||
| ≥36 mm | 15 (16.3.) | 8 (22.2) | ||
| Ectopic site | Right tuba | 45 (48.9) | 17 (48.6) | >0.999 |
| Left tuba | 47 (51.1) | 19 (51.4) | ||
| Methotrexate regimen | Single dose | 24 (26.0) | 26 (72.4) | 0.002 |
| Double dose | 41 (44.5) | 7 (19.4) | ||
| Multiple doses | 27 (29.3) | 3 (8.3) | ||
| Salpingectomy | No | 71 (77.2) | 1 (2.9) | <0.001 |
| Yes | 21 (22.8) | 35 (97.2) | ||
| D/C | No | 53 (66.2) | 31 (86.10) | 0.015 |
| Yes | 29 (33.8) | 5 (13.8) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seyfettinoglu, S.; Adıguzel, F.I. Prediction of Tubal Rupture in Ectopic Pregnancy Using Methotrexate Treatment Protocols and Hematological Markers. J. Clin. Med. 2023, 12, 6459. https://doi.org/10.3390/jcm12206459
Seyfettinoglu S, Adıguzel FI. Prediction of Tubal Rupture in Ectopic Pregnancy Using Methotrexate Treatment Protocols and Hematological Markers. Journal of Clinical Medicine. 2023; 12(20):6459. https://doi.org/10.3390/jcm12206459
Chicago/Turabian StyleSeyfettinoglu, Sevtap, and Fikriye Işıl Adıguzel. 2023. "Prediction of Tubal Rupture in Ectopic Pregnancy Using Methotrexate Treatment Protocols and Hematological Markers" Journal of Clinical Medicine 12, no. 20: 6459. https://doi.org/10.3390/jcm12206459
APA StyleSeyfettinoglu, S., & Adıguzel, F. I. (2023). Prediction of Tubal Rupture in Ectopic Pregnancy Using Methotrexate Treatment Protocols and Hematological Markers. Journal of Clinical Medicine, 12(20), 6459. https://doi.org/10.3390/jcm12206459






