Patients’ Buying Behavior for Non-Reimbursed Off-Loading Devices Used in Diabetic Foot Ulcer Treatment—An Observational Study during COVID-19 Pandemic from a Romanian Physical Therapy Unit
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. DFU Dressing, Bandages, and Padding Procedures
2.3. Off-Loading Methods
2.3.1. Removable Casts Walkers
RCW Internal Components Personalization
2.3.2. Therapeutic Footwear with Inserted Prefabricated Foot Insoles
The Therapeutic Footwear
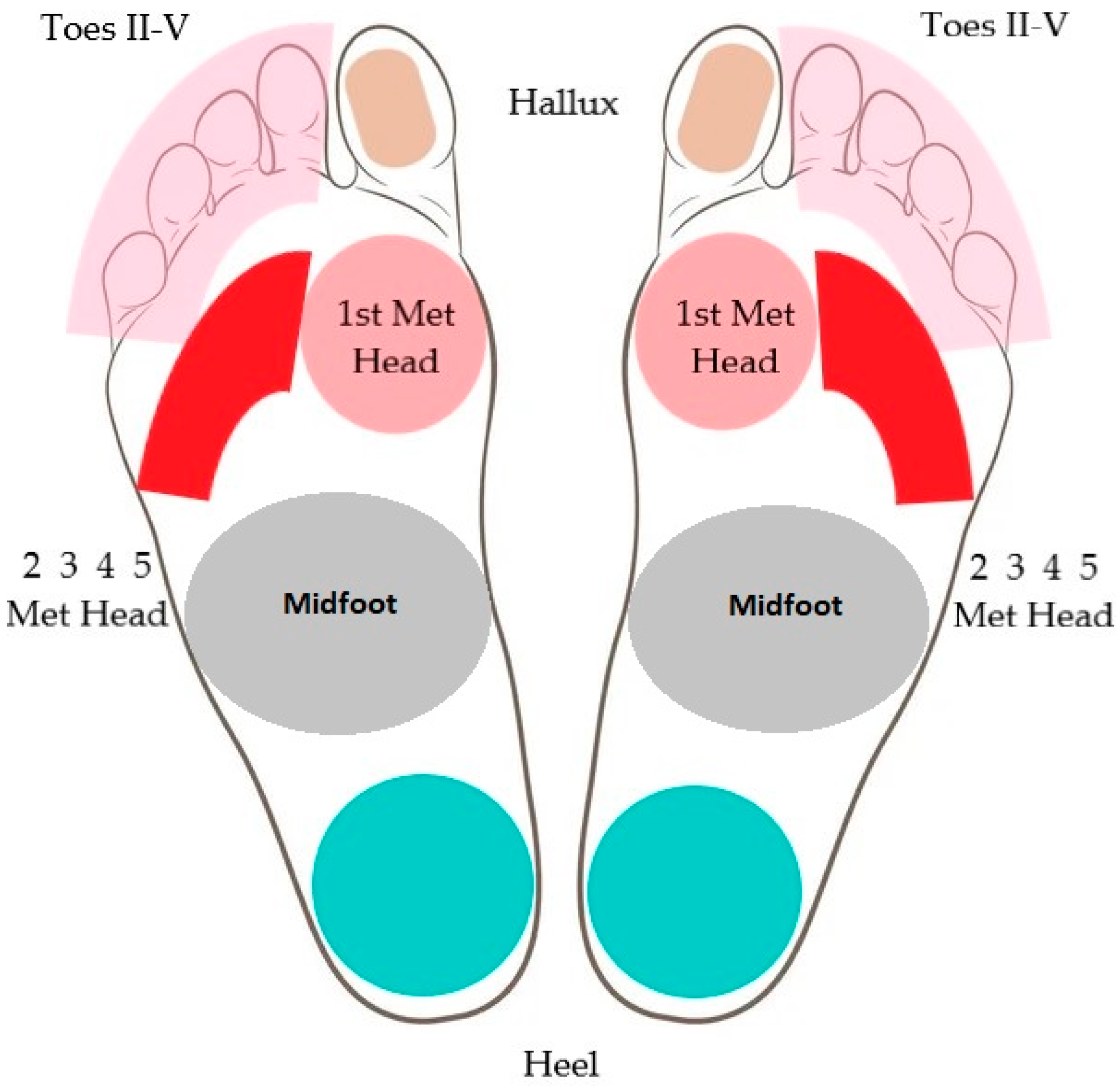
Prefabricated Foot Insoles
2.3.3. Personal off-the-Shelf Footwear with Inserted Prefabricated Foot Insoles
2.3.4. Personal off-the-Shelf Footwear
2.4. Statistical Analysis
3. Results
3.1. Participants’ Characteristics
3.2. Study Group Diabetic Foot Characteristics
3.3. Study Group Treatment
3.4. Contributing Factors for Off-Loading Choices and DFU Healing
3.5. Encountered Situations during Remote Monitorization
3.5.1. Remote Communication-Related Situations
3.5.2. Encountered Self-Treatment Errors
3.5.3. Encountered Complications
3.5.4. Poor Hygiene
3.5.5. Medical Devices Deterioration
3.6. Patients Lost from the Study
4. Discussion
4.1. Treatment Choices
4.2. Factors That Influenced Buying Behavior
4.3. Treatment Efficiency
4.4. Study Limitations
5. Conclusions
Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Foundation. IDF Diabetes Atlas—9th Edition. 2019. Available online: https://diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf (accessed on 3 June 2022).
- Mota, M.; Popa, S.G.; Mota, E.; Mitrea, A.; Catrinoiu, D.; Cheta, D.M.; Guja, C.; Hancu, N.; Ionescu-Tirgoviste, C.; Lichiardo-pol, R.; et al. Prevalence of diabetes mellitus and prediabetes in the adult Romanian population: PREDATORR study. J. Diabetes 2016, 8, 336–344. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation (2009) Diabetes Atlas. 4th Edition. Available online: http://www.idf.org/sites/default/files/da5/IDF%20Diabetes%20Atlas%204th%20edition.pdf (accessed on 7 July 2023).
- Hicks, C.W.; Selvin, E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr. Diab. Rep. 2019, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- Shiferaw, W.S.; Akalu, T.Y.; Work, Y.; Aynalem, Y.A. Prevalence of diabetic peripheral neuropathy in Africa: A systematic review and meta-analysis. BMC Endocr. Disord. 2020, 20, 49. [Google Scholar] [CrossRef] [PubMed]
- Owolabi, L.F.; Alghamdi, M.; Adamu, B.; Taura, M.G.; Jibo, A.; Almansour, M.; Alaklabi, S.N.; Alghamdi, M.A.; Alotaibi, Y.A.; Imam, I.A.; et al. Magnitude of diabetic peripheral neuropathy in Saudi Arabia: A systematic review and meta-analysis. BMC Endocr. Disord. 2022, 22, 266. [Google Scholar] [CrossRef]
- Pop-Busui, R.; Lu, J.; Lopes, N.; Jones, T.L.; BARI 2D Investigators. Prevalence of diabetic peripheral neuropathy and relation to glycemic control therapies at baseline in the BARI 2D cohort. J. Peripher. Nerv. Syst. 2009, 14, 1–13. [Google Scholar] [CrossRef]
- Sun, J.; Wang, Y.; Zhang, X.; Zhu, S.; He, H. Prevalence of peripheral neuropathy in patients with diabetes: A systematic review and meta-analysis. Prim. Care Diabetes 2020, 14, 435–444. [Google Scholar] [CrossRef]
- Aday, A.W.; Matsushita, K. Epidemiology of Peripheral Artery Disease and Polyvascular Disease. Circ. Res. 2021, 128, 1818–1832. [Google Scholar] [CrossRef]
- American Diabetes Association. Peripheral arterial disease in people with diabetes. Diabetes Care 2003, 26, 3333–3341. [Google Scholar] [CrossRef]
- Soyoye, D.O.; Abiodun, O.O.; Ikem, R.T.; Kolawole, B.A.; Akintomide, A.O. Diabetes and peripheral artery disease: A review. World J. Diabetes 2021, 12, 827–838. [Google Scholar] [CrossRef]
- Allison, M.A.; Criqui, M.H.; McClelland, R.L.; Scott, J.M.; McDermott, M.M.; Liu, K.; Folsom, A.R.; Bertoni, A.G.; Sharrett, A.R.; Homma, S.; et al. The effect of novel cardiovascular risk factors on the ethnic-specific odds for peripheral arterial disease in the Multi-Ethnic Study of Atherosclerosis (MESA). J. Am. Coll. Cardiol. 2006, 48, 1190–1197. [Google Scholar] [CrossRef]
- Ding, N.; Sang, Y.; Chen, J.; Ballew, S.H.; Kalbaugh, C.A.; Salameh, M.J.; Blaha, M.J.; Allison, M.; Heiss, G.; Selvin, E.; et al. Cigarette smoking, smoking cessation, and long-term risk of 3 major atherosclerotic diseases. J. Am. Coll. Cardiol. 2019, 74, 498–507. [Google Scholar] [CrossRef] [PubMed]
- Fowkes, F.G.; Rudan, D.; Rudan, I.; Aboyans, V.; Denenberg, J.O.; McDermott, M.M.; Norman, P.E.; Sampson, U.K.; Williams, L.J.; Mensah, G.A.; et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: A systematic review and analysis. Lancet 2013, 382, 1329–1340. [Google Scholar] [CrossRef]
- Geiss, L.S.; Li, Y.; Hora, I.; Albright, A.; Rolka, D.; Gregg, E.W. Resurgence of diabetes-related nontraumatic lower-extremity amputation in the young and middle-aged adult U.S. population. Diabetes Care 2019, 42, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Menke, A.; Casagrande, S.; Geiss, L.; Cowie, C.C. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. JAMA 2015, 314, 1021–1029. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: Report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Ballew, S.H.; Tanaka, H.; Szklo, M.; Heiss, G.; Coresh, J.; Matsushita, K. 2017 ACC/AHA blood pressure classification and incident peripheral artery disease: The Atherosclerosis Risk in Communities (ARIC) study. Eur. J. Prev. Cardiol. 2020, 27, 51–59. [Google Scholar] [CrossRef]
- Ang, G.Y.; Yap, C.W.; Saxena, N. Effectiveness of Diabetes Foot Screening in Primary Care in Preventing Lower Extremity Amputations. Ann. Acad. Med. Singap. 2017, 46, 417–423. [Google Scholar] [CrossRef]
- Pop-Busui, R.; Herman, W.H.; Feldman, E.L.; Low, P.A.; Martin, C.L.; Cleary, P.A.; Waberski, B.H.; Lachin, J.M.; Albers, J.W. DCCT and EDIC studies in type 1 diabetes: Lessons for diabetic neuropathy regarding metabolic memory and natural history. Curr. Diab. Rep. 2010, 10, 276–282. [Google Scholar] [CrossRef]
- Calles-Escandon, J.; Lovato, L.C.; Simons-Morton, D.G.; Kendall, D.M.; Pop-Busui, R.; Cohen, R.M.; Bonds, D.E.; Fonseca, V.A.; Ismail-Beigi, F.; Banerji, M.A.; et al. Effect of intensive compared with standard glycemia treatment strategies on mortality by baseline subgroup characteristics: The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Diabetes Care 2010, 33, 721–727. [Google Scholar] [CrossRef]
- Owings, T.M.; Apelqvist, J.; Stenström, A.; Becker, M.; Bus, S.A.; Kalpen, A.; Ulbrecht, J.S.; Cavanagh, P.R. Plantar pressures in diabetic patients with foot ulcers which have remained healed. Diabet. Med. 2009, 26, 1141–1146. [Google Scholar] [CrossRef]
- Van Houtum, W.H.; Lavery, L.A.; Harkless, L.B. The impact of diabetes-related lower-extremity amputations in the Netherlands. J. Diabetes Complicat. 1996, 10, 325–330. [Google Scholar] [CrossRef]
- Bondor, C.I.; Veresiu, I.A.; Florea, B.; Vinik, E.J.; Vinik, A.I.; Gavan, N.A. Epidemiology of diabetic foot ulcers and amputations in Romania: Results of a cross-sectional quality of life questionnaire-based survey. J. Diab. Res. 2016, 2016, 5439521. [Google Scholar] [CrossRef] [PubMed]
- Singh, N.; Armstrong, D.G.; Lipsky, B.A. Preventing foot ulcers in patients with diabetes. JAMA 2005, 293, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Reiber, G.E. Epidemiology of Foot Ulcers and Amputations in the Diabetic Foot. In The Diabetic Foot, 6th ed.; Bowker, J.H., Pfeifer, M.A., Eds.; Mosby: St. Louis, MO, USA, 2001; pp. 13–22. [Google Scholar]
- CDC. National Diabetes Fact Sheet. 2007. Available online: http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf (accessed on 4 August 2023).
- Bus, S.A.; Armstrong, D.G.; Crews, R.T.; Gooday, C.; Jarl, G.; Kirketerp-Moller, K.; Viswanathan, V.; Lazzarini, P.A. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2023 update). Diabetes Metab. Res. Rev. 2023, 25, e3647. [Google Scholar] [CrossRef]
- Lavery, L.A.; Vela, S.A.; Lavery, D.C.; Quebedeaux, T.L. Reducing dynamic foot pressures in high-risk diabetic subjects with foot ulcerations. A comparison of treatments. Diabetes Care 1996, 19, 818–821. [Google Scholar] [CrossRef] [PubMed]
- Gutekunst, D.J.; Hastings, M.K.; Bohnert, K.L.; Strube, M.J.; Sinacore, D.R. Removable cast walker boots yield greater forefoot off-loading than total contact casts. Clin. Biomech. 2011, 26, 649–654. [Google Scholar] [CrossRef]
- Piaggesi, A.; Goretti, C.; Iacopi, E.; Clerici, G.; Romagnoli, F.; Toscanella, F.; Vermigli, C. Comparison of removable and irremovable walking boot to total contact casting in offloading the neuropathic diabetic foot ulceration. Foot Ankle Int. 2016, 37, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Raspovic, A.; Landorf, K.B. A survey of offloading practices for diabetes-related plantar neuropathic foot ulcers. J. Foot Ankle Res. 2014, 7, 35. [Google Scholar] [CrossRef]
- Wu, S.C.; Jensen, J.L.; Weber, A.K.; Robinson, D.E.; Armstrong, D.G. Use of pressure offloading devices in diabetic foot ulcers: Do we practice what we preach? Diabetes Care 2008, 31, 2118–2119. [Google Scholar]
- Barwick, A.L.; van Netten, J.J.; Reed, L.F.; Lazzarini, P.A. Independent factors associated with wearing different types of outdoor footwear in a representative inpatient population: A cross-sectional study. J. Foot Ankle Res. 2018, 29, 11–19. [Google Scholar] [CrossRef]
- van Netten, J.J.; Lazzarini, P.A.; Armstrong, D.G.; Bus, S.A.; Fitridge, R.; Harding, K.; Kinnear, E.; Malone, M.; Menz, H.B.; Perrin, B.M.; et al. Diabetic Foot Australia guideline on footwear for people with diabetes. J. Foot Ankle Res. 2018, 11, 2. [Google Scholar] [CrossRef]
- Rizzo, L.; Tedeschi, A.; Fallani, E.; Coppelli, A.; Vallini, V.; Iacopi, E.; Piaggesi, A. Custom-made orthesis and shoes in a structured follow-up program reduces the incidence of neuropathic ulcers in high-risk diabetic foot patients. Int. J. Low. Extrem. Wounds 2012, 11, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Arts, M.L.; Waaijman, R.; de Haart, M.; Keukenkamp, R.; Nollet, F.; Bus, S.A. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet. Med. 2012, 29, 1534–1541. [Google Scholar] [CrossRef] [PubMed]
- Luo, B.; Cai, Y.; Chen, D.; Wang, C.; Huang, H.; Chen, L.; Gao, Y.; Ran, X. Effects of Special Therapeutic Footwear on the Prevention of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Diabetes Res. 2022, 26, 9742665. [Google Scholar] [CrossRef]
- van Schie, C.; Ulbrecht, J.S.; Becker, M.B.; Cavanagh, P.R. Design criteria for rigid rocker shoes. Foot Ankle Int. 2000, 21, 833–844. [Google Scholar] [CrossRef] [PubMed]
- Uccioli, L.; Faglia, E.; Monticone, G.; Favales, F.; Durola, L.; Aldeghi, A.; Quarantiello, A.; Calia, P.; Menzinger, G. Manufactured shoes in the prevention of diabetic foot ulcers. Diabetes Care 1995, 18, 1376–1378. [Google Scholar] [CrossRef]
- Praet, S.F.; Louwerens, J.W. The influence of shoe design on plantar pressures in neuropathic feet. Diabetes Care 2003, 26, 441–445. [Google Scholar] [CrossRef]
- Reints, R.; Hijmans, J.M.; Burgerhof, J.G.M.; Postema, K.; Verkerke, G.J. Effects of flexible and rigid rocker profiles on in-shoe pressure. Gait Posture 2017, 58, 287–293. [Google Scholar] [CrossRef]
- Preece, S.J.; Chapman, J.D.; Braunstein, B.; Bruggemann, G.P.; Nester, C.J. Optimisation of rocker sole footwear for prevention of first plantar ulcer: Comparison of group-optimised and individually-selected footwear designs. J. Foot Ankle Res. 2017, 10, 1–10. [Google Scholar] [CrossRef]
- Reiber, G.E.; Smith, D.G.; Wallace, C.; Sullivan, K.; Hayes, S.; Vath, C.; Maciejewski, M.L.; Yu, O.; Heagerty, P.J.; LeMaster, J. Effect of therapeutic footwear on foot reulceration in patients with diabetes: A randomized controlled trial. JAMA 2002, 287, 2552–2558. [Google Scholar] [CrossRef]
- Bus, S.A.; Waaijman, R.; Arts, M.; de Haart, M.; Busch-Westbroek, T.; van Baal, J.; Nollet, F. Effect of custom-made footwear on foot ulcer recurrence in diabetes: A multicenter randomized controlled trial. Diabetes Care 2013, 36, 4109–4116. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Barwick, A.; Butterworth, P.; Nancarrow, S. Footwear and insole design features that reduce neuropathic plantar forefoot ulcer risk in people with diabetes: A systematic literature review. J. Foot Ankle Res. 2020, 13, 30. [Google Scholar] [CrossRef] [PubMed]
- López-Moral, M.; Lázaro-Martínez, J.L.; García-Morales, E.; García-Álvarez, Y.; Álvaro-Afonso, F.J.; Molines-Barroso, R.J. Clinical efficacy of therapeutic footwear with a rigid rocker sole in the prevention of recurrence in patients with diabetes mellitus and diabetic polineuropathy: A randomized clinical trial. PLoS ONE 2019, 14, e0219537. [Google Scholar] [CrossRef] [PubMed]
- Lavery, L.A.; LaFontaine, J.; Higgins, K.R.; Lanctot, D.R.; Constantinides, G. Shear-reducing insoles to prevent foot ulceration in high-risk diabetic patients. Adv. Ski. Wound Care 2012, 25, 519–524; quiz 525–526. [Google Scholar] [CrossRef] [PubMed]
- Ulbrecht, J.S.; Hurley, T.; Mauger, D.T.; Cavanagh, P.R. Prevention of recurrent foot ulcers with plantar pressure-based in-shoe orthoses: The CareFUL prevention multicenter randomized controlled trial. Diabetes Care 2014, 37, 1982–1989. [Google Scholar] [CrossRef] [PubMed]
- Sen, C.K. Human Wound and Its Burden: Updated 2020 Compendium of Estimates. Adv. Wound Care 2021, 10, 281–292. [Google Scholar] [CrossRef]
- Shin, L.; Bowling, F.L.; Armstrong, D.G.; Boulton, A.J.M. Saving the Diabetic Foot During the COVID-19 Pandemic: A Tale of Two Cities. Diabetes Care 2020, 43, 1704–1709. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, B.S.B.; Froekjaer, J.; Bjerregaard, M.R.; Lauritsen, J.; Hangaard, J.; Henriksen, C.W.; Halekoh, U.; Yderstraede, K.B. A randomized controlled trial comparing telemedical and standard outpatient monitoring of diabetic foot ulcers. Diabetes Care 2015, 38, 1723–1729. [Google Scholar] [CrossRef]
- NHS England, Clinical Strategy for Service Management of Diabetic Foot Units during the COVID-19 Pandemic. Available online: https://www.england.nhs.uk/london/wp-content/uploads/sites/8/2020/04/5.-Covid-19-Clinical-Strategy-for-MDFTs-Crib-Sheet-02042020.pdf (accessed on 9 May 2023).
- Swerdlow, M.; Shin, L.; D’Huyvetter, K.; Mack, W.J.; Armstrong, D.G. Initial Clinical Experience with a Simple, Home System for Early Detection and Monitoring of Diabetic Foot Ulcers: The Foot Selfie. J. Diabetes Sci. Technol. 2023, 17, 79–88. [Google Scholar] [CrossRef]
- Hazenberg, C.E.; Bus, S.A.; Kottink, A.I.; Bouwmans, C.A.; Schönbach-Spraul, A.M.; van Baal, S.G. Telemedical home-monitoring of diabetic foot disease using photographic foot imaging—A feasibility study. J. Telemed. Telecare 2012, 18, 32–36. [Google Scholar] [CrossRef]
- van Netten, J.J.; Clark, D.; Lazzarini, P.A.; Janda, M.; Reed, L.F. The validity and reliability of remote diabetic foot ulcer assessment using mobile phone images. Sci. Rep. 2017, 7, 9480. [Google Scholar] [CrossRef]
- Kelahmetoglu, O.; Camlı, M.F.; Kirazoglu, A.; Erbayat, Y.; Asgarzade, S.; Durgun, U.; Mehdizade, T.; Yeniocak, A.; Yildiz, K.; Sonmez Ergun, S.; et al. Recommendations for management of diabetic foot ulcers during COVID-19 outbreak. Int. Wound J. 2020, 17, 1424–1427. [Google Scholar] [CrossRef]
- Meloni, M.; Izzo, V.; Giurato, L.; Gandini, R.; Uccioli, L. Management of diabetic persons with foot ulceration during COVID-19 health care emergency: Effectiveness of a new triage pathway. Diabetes Res. Clin. Pract. 2020, 165, 108245. [Google Scholar] [CrossRef] [PubMed]
- Jaly, I.; Iyengar, K.; Bahl, S.; Hughes, T.; Vaishya, R. Redefining diabetic foot disease management service during COVID-19 pandemic. Diabetes Metab. Syndr. 2020, 14, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Tao, F.; Tang, X.; Tao, H.; Luo, Y.; Cao, H.; Xiang, W.; Zhao, Y.; Jin, L. Surgical treatment of diabetic foot ulcers during the COVID-19 pandemic in China. J. Diabetes Complicat. 2020, 34, 107622. [Google Scholar] [CrossRef]
- Atri, A.; Kocherlakota, C.M.; Dasgupta, R. Managing diabetic foot in times of COVID-19: Time to put the best “foot” forward. Int. J. Diabetes Dev. Ctries. 2020, 1, 8. [Google Scholar] [CrossRef] [PubMed]
- Rogers, L.C.; Lavery, L.A.; Joseph, W.S.; Armstrong, D.G. All Feet on Deck: The Role of Podiatry During the COVID-19 Pandemic: Preventing Hospitalizations in an Overburdened Health-Care System, Reducing Amputation and Death in People with Diabetes. J. Am. Podiatr. Med. Assoc. 2023, 113, 20–051. [Google Scholar] [CrossRef] [PubMed]
- Health Quality Ontario. Fibreglass Total Contact Casting, Removable Cast Walkers, and Irremovable Cast Walkers to Treat Diabetic Neuropathic Foot Ulcers: A Health Technology Assessment. Ont. Health Technol. Assess. Ser. 2017, 17, 1–124. [Google Scholar]
- van Netten, J.J.; Seng, L.; Lazzarini, P.A.; Warnock, J.; Ploderer, B. Reasons for (non-)adherence to self-care in people with a diabetic foot ulcer. Wound Repair Regen. 2019, 27, 530–539. [Google Scholar] [CrossRef]
- Formosa, C.; Borg, A.; Papanas, N.; Mizzi, S. Adherence to Therapeutic Footwear in Type 2 Diabetes in Malta. Exp. Clin. Endocrinol. Diabetes 2020, 128, 244–245. [Google Scholar] [CrossRef]
- Tan, S.; Horobin, H.; Tunpraser, T. The lived experience of people with diabetes using off-the-shelf prescription footwear in Singapore: A qualitative study using interpretative phenomenological analysis. J. Foot Ankle Res. 2019, 12, 19. [Google Scholar] [CrossRef]
- Majid, U.; Argáez, C. Off-Loading Devices for People with Diabetic Neuropathic Foot Ulcers: A Rapid Qualitative Review [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2020 Jun 17. Available online: https://www.ncbi.nlm.nih.gov/books/NBK565247/ (accessed on 27 June 2023).
- Armstrong, D.C.; Lavery, L.A.; Harkless, L.B. Validation of a Diabetic Wound Classification System: The contribution of depth, infection, and ischemia to risk of amputation. Diabetes Care 1998, 21, 855–859. [Google Scholar] [CrossRef] [PubMed]
- Asociatia de Podiatrie. Available online: https://www.podiatrie.ro (accessed on 30 May 2023).
- Hingorani, A.; LaMuraglia, G.M.; Henke, P.; Meissner, M.H.; Loretz, L.; Zinszer, K.M.; Driver, V.R.; Frykberg, R.; Carman, T.L.; Marston, W.; et al. The management of diabetic foot: A clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. J. Vasc. Surg. 2016, 63 (Suppl. 2), 3S–21S. [Google Scholar] [CrossRef] [PubMed]
- Optima Molliter. Available online: http://www.molliter.com/prodotti/it/prodotto/darco/wcs (accessed on 20 April 2023).
- Optima Molliter. Available online: http://www.molliter.com/prodotti/it/prodotto/darco/bodyarmorproterm (accessed on 20 April 2023).
- Optima Molliter. Available online: http://www.molliter.com (accessed on 20 April 2023).
- Optima Molliter. Available online: http://www.molliter.com/it/prodotti/mac2 (accessed on 20 April 2023).
- Vasyli Medical. Available online: https://www.vasylimedical.com/products/signature-series/armstrong-ii (accessed on 20 April 2023).
- Algeos. Interpod Diabetic Interpod Diabetic. Available online: https://www.algeos.com/interpod-diabeticu (accessed on 25 May 2023).
- WhatsApp Web. Available online: https://web.archive.org/web/20220801161557/https://www.whatsapp.com/android/ (accessed on 22 May 2023).
- Withers, R.V.; Perrin, B.M.; Landorf, K.B.; Raspovic, A. Offloading effects of a removable cast walker with and without modification for diabetes-related foot ulceration: A plantar pressure study. J. Foot Ankle Res. 2023, 16, 27. [Google Scholar] [CrossRef]
- Optima Molliter. Available online: http://www.molliter.com/en/algoritmi (accessed on 8 July 2023).
- Optima Molliter. Available online: http://www.molliter.com/prodotti/it/prodotto/heelreliever (accessed on 12 August 2023).
- van Deursen, R. Footwear for the neuropathic patient: Offloading and stability. Diabetes Metab. Res. Rev. 2008, 24 (Suppl. 1), S96–S100. [Google Scholar] [CrossRef]
- Optima Molliter. Available online: http://www.molliter.com/media/prodottidoc/15/546MANUALE%20D’USO%20OPTIMA%20FASE%20ACUTA_%20INGLESE.pdf (accessed on 10 August 2023).
- DF Blog. Available online: https://diabeticfootonline.com/2020/05/30/salsa-rancho-los-amigos-guidelines-for-return-to-activity-in-remission-toeflowandgo-usc-ranchoresearchi-usc_vascular (accessed on 20 July 2023).
- IBM. Available online: https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-25 (accessed on 21 May 2023).
- Bus, S.A.; Armstrong, D.G.; van Deursen, R.W.; Lewis, J.E.; Caravaggi, C.F.; Cavanagh, P.R.; International Working Group on the Diabetic Foot. IWGDF guidance on footwear and offloading interventions to prevent and heal foot ulcers in patients with diabetes. Diabetes Metab. Res. Rev. 2016, 32 (Suppl. 1), 25–36. [Google Scholar] [CrossRef] [PubMed]
- Snyder, R.J.; Frykberg, R.G.; Rogers, L.C.; Applewhite, A.J.; Bell, D.; Bohn, G.; Fife, C.E.; Jensen, J.; Wilcox, J. The management of diabetic foot ulcers through optimal off-loading: Building consensus guidelines and practical recommendations to improve outcomes. J. Am. Podiatr. Med. Assoc. 2014, 104, 555–567. [Google Scholar] [CrossRef]
- Wu, S.C.; Crews, R.T.; Armstrong, D.G. The pivotal role of offloading in the management of neuropathic foot ulceration. Curr. Diab. Rep. 2005, 5, 423–429. [Google Scholar] [CrossRef]
- Crews, R.T.; Shen, B.J.; Campbell, L.; Lamont, P.J.; Boulton, A.J.; Peyrot, M.; Kirsner, R.S.; Vileikyte, L. Role and Determinants of Adherence to Off-loading in Diabetic Foot Ulcer Healing: A Prospective Investigation. Diabetes Care 2016, 39, 1371–1377. [Google Scholar] [CrossRef]
- Crawford, F.; Nicolson, D.J.; Amanna, A.E.; Martin, A.; Gupta, S.; Leese, G.P.; Heggie, R.; Chappell, F.M.; McIntosh, H.H. Preventing foot ulceration in diabetes: Systematic review and meta-analyses of RCT data. Diabetologia 2020, 63, 49–64. [Google Scholar] [CrossRef]
- Fernando, M.E.; Crowther, R.G.; Pappas, E.; Lazzarini, P.A.; Cunningham, M.; Sangla, K.S.; Buttner, P.; Golledge, J. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: A meta-analysis of observational studies. PLoS ONE 2014, 9, e99050. [Google Scholar] [CrossRef]
- Amin, N.; Doupis, J. Diabetic foot disease: From the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J. Diabetes 2016, 7, 153–164. [Google Scholar] [CrossRef]
- Schaper, N.C.; van Netten, J.J.; Apelqvist, J.; Bus, S.A.; Hinchliffe, R.J.; Lipsky, B.A.; IWGDF Editorial Board. Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes Metab. Res. Rev. 2020, 36 (Suppl. 1), e3266. [Google Scholar] [CrossRef]
- Nahas, M.R.; Gawish, H.M.; Tarshoby, M.M.; State, O.I.; Aboelyazid, A. Effect of simulated leg length discrepancy on plantar pressure distribution in diabetic patients with neuropathic foot ulceration. J. Wound Care 2011, 20, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Gurney, B.; Mermier, C.; Robergs, R.; Gibson, A.; Rivero, D. Effects of limb-length discrepancy on gait economy and lower-extremity muscle activity in older adults. J. Bone Joint Surg. Am. 2001, 83, 907–915. [Google Scholar] [CrossRef]
- Crews, R.T.; Candela, J. Decreasing an Offloading Device’s Size and Offsetting Its Imposed Limb-Length Discrepancy Lead to Improved Comfort and Gait. Diabetes Care 2018, 41, 1400–1405. [Google Scholar] [CrossRef]
- Ababneh, A.; Finlayson, K.; Edwards, H.; Lazzarini, P.A. Factors associated with adherence to using removable cast walker treatment among patients with diabetes-related foot ulcers. BMJ Open Diabetes Res. Care 2022, 10, e002640. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lavery, L.A.; Kimbriel, H.R.; Nixon, B.P.; Boulton, A.J. Activity patterns of patients with diabetic foot ulceration: Patients with active ulceration may not adhere to a standard pressure off-loading regimen. Diabetes Care 2003, 26, 2595–2597. [Google Scholar] [CrossRef]
- Najafi, B.; Crews, R.T.; Wrobel, J.S. Importance of time spent standing for those at risk of diabetic foot ulceration. Diabetes Care 2010, 33, 2448–2450. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. India under COVID-19 lockdown. Lancet 2020, 395, 1315. [Google Scholar] [CrossRef]
- Wukich, D.K.; Raspovic, K.M.; Suder, N.C. Patients with diabetic foot disease fear major lower-extremity amputation more than death. Foot Ankle Spec. 2018, 11, 17–21. [Google Scholar] [CrossRef]
- Kerr, M.; Barron, E.; Chadwick, P.; Evans, T.; Kong, W.M.; Rayman, G.; Sutton-Smith, M.; Todd, G.; Young, B.; Jeffcoate, W.J. The cost of diabetic foot ulcers and amputations to the National Health Service in England. Diabet. Med. 2019, 36, 995–1002. [Google Scholar] [CrossRef]
- Petrakis, I.; Kyriopoulos, I.J.; Ginis, A.; Athanasakis, K. Losing a foot versus losing a dollar; a systematic review of cost studies in diabetic foot complications. Expert Rev. Pharmacoecon. Outcomes Res. 2017, 17, 165–180. [Google Scholar] [CrossRef] [PubMed]
- Sima, D.I.; Bondor, C.I.; Vereşiu, I.A.; Gâvan, N.A.; Borzan, C.M. Hospitalization Costs of Lower Limb Ulcerations and Amputations in Patients with Diabetes in Romania. Int. J. Env. Res. Public Health 2021, 18, 2230. [Google Scholar] [CrossRef]
- Eurostat. Mean and Median Income by Household Type—EU-SILC and ECHP Survey. Available online: https://ec.europa.eu/eurostat/databrowser/view/ILC_DI04/default/table?lang=en (accessed on 30 July 2023).
- Institutul national de Statistica. Castigul Salarial Mediu Net. Available online: https://insse.ro/cms/sites/default/files/com_presa/com_pdf/cs06r22_0.pdf (accessed on 30 July 2023).
- Institutul National de Statistica. Comunicat de Presa. Available online: https://insse.ro/cms/sites/default/files/com_presa/com_pdf/pensii_2022r.pdf (accessed on 30 July 2023).
- Dardari, D.; Franc, S.; Charpentier, G.; Orlando, L.; Bobony, E.; Bouly, M.; Xhaard, I.; Amrous, Z.; Sall, K.L.; Detournay, B.; et al. Hospital stays and costs of telemedical monitoring versus standard follow-up for diabetic foot ulcer: An open-label randomised controlled study. Lancet Reg. Health Eur. 2023, 32, 100686. [Google Scholar] [CrossRef]
- Khalifa, W.A.; Argoon, S.A.; AbdEllah-Alawi, M.H.M. Determinants of healing of diabetic foot ulcer comparing two offloading modalities: A randomized prospective study. Foot 2023, 56, 102016. [Google Scholar] [CrossRef] [PubMed]
- Lazzarini, P.A.; Jarl, G.; Gooday, C.; Viswanathan, V.; Caravaggi, C.F.; Armstrong, D.G.; Bus, S.A. Effectiveness of offloading interventions to heal foot ulcers in persons with diabetes: A systematic review. Diabetes Metab. Res. Rev. 2020, 36 (Suppl. 1), e3275. [Google Scholar] [CrossRef]
- Bonnet, J.B.; Macioce, V.; Jalek, A.; Bouchdoug, K.; Elleau, C.; Gras-Vidal, M.F.; Pochic, J.; Avignon, A.; Sultan, A. Covid-19 lockdown showed a likely beneficial effect on diabetic foot ulcers. Diabetes Metab. Res. Rev. 2022, 38, e3520. [Google Scholar] [CrossRef]
- Healy, A.; Naemi, R.; Chockalingam, N. The effectiveness of footwear and other removable off-loading devices in the treatment of diabetic foot ulcers: A systematic review. Curr. Diabetes Rev. 2014, 10, 215–230. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Nguyen, H.C.; Lavery, L.A.; van Schie, C.H.; Boulton, A.J.; Harkless, L.B. Off-loading the diabetic foot wound: A randomized clinical trial. Diabetes Care 2001, 24, 1019–1022. [Google Scholar] [CrossRef]
- Armstrong, D.G.; Lavery, L.A.; Wu, S.; Boulton, A.J. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: A randomized controlled trial. Diabetes Care 2005, 28, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Petersen, B.J.; Bus, S.A.; Rothenberg, G.M.; Linders, D.R.; Lavery, L.A.; Armstrong, D.G. Recurrence rates suggest delayed identification of plantar ulceration for patients in diabetic foot remission. BMJ Open Diabetes Res. Care 2020, 8, e001697. [Google Scholar] [CrossRef]
- Kee, K.K.; Nair, H.K.R.; Yuen, N.P. Risk factor analysis on the healing time and infection rate of diabetic foot ulcers in a referral wound care clinic. J. Wound Care 2019, 28 (Suppl. 1), S4–S13. [Google Scholar] [CrossRef] [PubMed]
- Petersen, B.J.; Rothenberg, G.M.; Lakhani, P.J.; Zhou, M.; Linders, D.R.; Bloom, J.D.; Wood, K.A.; Armstrong, D.G. Ulcer metastasis? Anatomical locations of recurrence for patients in diabetic foot remission. J. Foot Ankle Res. 2020, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Dalla Paola, L.; Faglia, E.; Caminiti, M.; Clerici, G.; Ninkovic, S.; Deanesi, V. Ulcer recurrence following first ray amputation in diabetic patients: A cohort prospective study. Diabetes Care 2003, 26, 1874–1878. [Google Scholar] [CrossRef]
- Vileikyte, L.; Peyrot, M.; Bundy, C.; Rubin, R.R.; Leventhal, H.; Mora, P.; Shaw, J.E.; Baker, P.; Boulton, A.J. The development and validation of a neuropathy- and foot ulcer-specific quality of life instrument. Diabetes Care 2003, 26, 2549–2555. [Google Scholar] [CrossRef]
- Vileikyte, L.; Gonzalez, J.S.; Leventhal, H.; Peyrot, M.F.; Rubin, R.R.; Garrow, A.; Ulbrecht, J.S.; Cavanagh, P.R.; Boulton, A.J. Patient Interpretation of Neuropathy (PIN) questionnaire: An instrument for assessment of cognitive and emotional factors associated with foot self-care. Diabetes Care 2006, 29, 2617–2624. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.S.; Peyrot, M.; McCarl, L.A.; Collins, E.M.; Serpa, L.; Mimiaga, M.J.; Safren, S.A. Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care 2008, 31, 2398–2403. [Google Scholar] [CrossRef] [PubMed]
- Monami, M.; Longo, R.; Desideri, C.M.; Masotti, G.; Marchionni, N.; Mannucci, E. The diabetic person beyond a foot ulcer: Healing, recurrence, and depressive symptoms. J. Am. Podiatr. Med. Assoc. 2008, 98, 130–136. [Google Scholar] [CrossRef]
- Vedhara, K.; Miles, J.N.; Wetherell, M.A.; Dawe, K.; Searle, A.; Tallon, D.; Cullum, N.; Day, A.; Dayan, C.; Drake, N.; et al. Coping style and depression influence the healing of diabetic foot ulcers: Observational and mechanistic evidence. Diabetologia 2010, 53, 1590–1598. [Google Scholar] [CrossRef]

















| Proposed Treatment Algorithm | Condition Severity | DFU Localization | Amputation Level | Proposed RCW |
|---|---|---|---|---|
| 1st choice | Unilateral DFU/unilateral DFU + mild/moderate infection/± mild/moderate ischemia), acute/chronic Charcot | Plantar/non-plantar  | Toes, transmetatarsals, rays  | Removable knee-high off-loading device  |
| 2nd choice | Unilateral DFU/unilateral DFU + mild/moderate infection/± mild/moderate ischemia), chronic Charcot | Plantar/non-plantar | Toes, transmetatarsals, rays | Removable ankle-height/below-ankle-height off-loading device |
  |   |  | ||
| 3rd choice | Unilateral DFU/unilateral DFU + mild/moderate infection/± mild/moderate ischemia), chronic Charcot | Plantar/non-plantar | Toes, transmetatarsals | Rigid fiberglass rocker-sole footwear + prefabricated foot orthotic |
 |  |  | ||
| Other choices | Unilateral DFU/unilateral DFU + mild/moderate infection/± mild/moderate ischemia) | Plantar/non-plantar | Lisfrank Chopard  |  |
Heel |   | |||
| Bilateral DFU/bilateral DFU + mild/moderate infection/± mild/moderate ischemia) | Plantar/non-plantar | Toes, transmetatarsals, rays, Lisfrank, Chopard |  |
| Participants’ Characteristics | Monitored Group (n = 45) |
|---|---|
| Age (years), arithmetic mean ± standard deviation | 61.91 ± 9.31 |
| Male, no. (%) | 38 (84.4) |
| Female, no. (%) | 7 (15.6) |
| BMI (kg/m2), median (25th–75th percentile) | 29.4 (27.47; 31.96) |
| Shoe size (EU size conversion) | 43 (42; 44) |
| Ex-smoker and smoker, no. (%) | 11 (26.2) |
| Non-smokers, no. (%) | 34 (73.8) |
| Active lifestyle, no. (%) | 14 (31.1) |
| Rural, no. (%) | 18 (40.9) |
| DM duration (years), arithmetic mean ± standard deviation | 14.27 ± 8.05 |
| HbA1c (%), median (25th–75th percentile) | 7.3 (6.35; 8.75) |
| Diabetic peripheral neuropathy, no. (%) | |
| Without | 0 (0.0) |
| Mild | 1 (2.2) |
| Moderate | 2 (4.4) |
| Severe | 42 (93.3) |
| Vitamin B supplementation, no. (%) | 4 (10.5) |
| With other neuropathy medication, no. (%) | 4 (9.5) |
| Peripheral arterial disease, no. (%) | 33 (73.3) |
| High blood pressure, no. (%) | 32 (84.2) |
| Cardiovascular disease, no. (%) | 19 (48.7) |
| Participants’ Diabetic Foot Characteristics | Monitored Group (n = 45) |
|---|---|
| Number of present DFUs on podiatric assessment, no. (%) | |
| One | 40 (88.9) |
| Two | 4 (8.9) |
| Three | 1 (2.2) |
| Actual DFU localization, no. (%) | |
| Left foot | 22 (48.9) |
| Right foot | 21 (46.7) |
| Both feet | 2 (4.4) |
| Actual DFU duration at the inclusion (weeks), median (25th–75th percentile) | 8 (3.5; 14) |
| DFU in the past, no. (%) | 30 (66.7) |
| Off-loading for previous DFUs other than actual DFUs, no. (%) | 2 (4.4) |
| No. of previous amputations, no. (%) | |
| One | 17 (37.8) |
| Two | 6 (13.3) |
| Three | 3 (6.7) |
| Four | 0 (0.0) |
| Five | 1 (2.2) |
| Charcot foot, no. (%) | 7 (15.6) |
| Foot deformities, no. (%) | 26 (57.8) |
| Revascularization, no. (%) | |
| Without | 21 (46.7) |
| Endovascular | 20 (44.4) |
| Bypass | 4 (8.9) |
| Parameters | Without Removable Walker (n = 17) | With Removable Walker (n = 28) | p |
|---|---|---|---|
| Age (years), arithmetic mean ± standard deviation | 61.47 ± 8.91 | 62.18 ± 9.7 | 0.808 a |
| Male, no. (%) | 17 (100) | 21 (75) | 0.034 b |
| Female, no. (%) | 0 (0) | 7 (25) | |
| BMI (kg/m2), median (25th–75th percentile) | 29.93 (27.04; 31.14) | 28.99 (27.41; 31.98) | 0.833 c |
| Rural, no. (%) | 11 (64.7) | 7 (25.9) | 0.011 d |
| Ex-smoker and smoker, no. (%) | 5 (31.3) | 6 (23.1) | 0.720 d |
| Non-smoker, no. (%) | 12 (68.7) | 22 (76.9) | |
| Lifestyle active, no. (%) | 6 (35.3) | 8 (28.6) | 0.637 d |
| HBP, no. (%) | 9 (64.3) | 23 (95.8) | 0.018 d |
| CVD, no. (%) | 7 (50) | 12 (48) | 1.000 d |
| DM duration (years), arithmetic mean ± standard deviation | 13.7 ± 7.11 | 14.68 ± 8.81 | 0.716 a |
| HbA1c, median (25th–75th percentile) | 7.65 (6.6; 8.55) | 7.05 (6.35; 8.8) | 0.830 c |
| DPN | |||
| Mild | 1 (5.9) | 0 (0) | 0.396 c |
| Moderate | 1 (5.9) | 1 (3.6) | |
| Severe | 15 (88.2) | 27 (96.4) | |
| Actual DFU duration | |||
| ≤4 weeks (1 month) | 5 (29.4) | 10 (35.7) | 0.762 c |
| 5–8 weeks (2 months) | 4 (23.5) | 6 (21.4) | |
| 9–16 weeks (3 -4 months) | 4 (23.5) | 5 (17.9) | |
| 17–32 weeks (5–8 months) | 2 (11.8) | 1 (3.6) | |
| 33–64 weeks (9–16 months) | 2 (11.8) | 1 (3.6) | |
| 65–208 weeks (10–16 months) | 0 | 3 (10.7) | |
| Not known | 0 | 1 (3.6) | |
| No. of amputations in the past, arithmetic mean ± standard Deviation | 0.65 ± 1.27 | 1.14 ± 0.93 | 0.018 c |
| No. of present DFUs/patient on podiatric assessment | |||
| 1 | 15 (88.2) | 25 (89.3) | 0.650 c |
| 2 | 2 (11.8) | 2 (7.1) | |
| 3 | 0 (0) | 1 (3.6) | |
| Foot | |||
| Left | 4 (23.5) | 18 (64.3) | 0.007 d |
| Right | 13 (76.5) | 8 (28.6) | |
| Both | 0 (0) | 2 (7.1) | |
| PAD, no. (%) | 7 (41.2) | 20 (74.1) | 0.029 d |
| Charcot foot, no. (%) | 1 (5.9) | 6 (21.4) | 0.227 b |
| Deformities, no. (%) | 8 (47.1) | 18 (64.3) | 0.257 d |
| DFUs in the past, no. (%) | 9 (52.9) | 21 (75) | 0.128 d |
| No. of pairs of protective footwear after initial podiatric evaluation | |||
| 0 | 0 (0) | 1 (3.6) | 0.710 c |
| 1 | 14 (82.4) | 23 (82.1) | |
| 2 | 3 (17.6) | 4 (14.3) | |
| Lost from the study, no. (%) | 5 (29.4) | 4 (14.3) | 0.265 b |
| Healed, no. (%) | 7 (58.3) 1 | 18 (75) 2 | 0.446 d |
| Infection, no. (%) | 3 (17.6) | 6 (21.4) | 1.000 b |
| With re-ulceration, no. (%) | 0 (0) 3 | 2 (11.1) 4 | 0.526 b |
| With amputations during follow-up, no. (%) | 1 (5.9) | 1 (3.6) | 1.000 b |
| No. of weeks to complete healing | |||
| ≤4 weeks (1 month) | 3 (42.9) 3 | 2 (11.1) 4 | 0.295 c |
| 5–8 weeks (2 months) | 4 (57.1) 3 | 3 (16.7) 4 | |
| 9–16 weeks (3 -4 months) | 0 (0) 3 | 9 (50) 4 | |
| 17–52 weeks (5–13 months) | 0 (0) 3 | 4 (22.2) 4 | |
| Total cost (EUR), arithmetic mean ± standard deviation | 308.11 ± 87.29 | 425.77 ± 93.33 | <0.001 c |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| Parameters | p | HR (95% Confidence Interval) | p | HR (95% Confidence Interval) |
| Age (years) | 0.025 | 1.05 (1.01; 1.09) | 0.026 | 1.05 (1.01; 1.09) |
| Male | 0.579 | |||
| BMI (kg/m2) | 0.772 | |||
| Rural | 0.316 | |||
| Ex-smoker and smoker | 0.586 | |||
| Lifestyle active | 0.851 | |||
| HBP | 0.047 | 2.79 (1.01; 7.71) | 0.020 | 3.44 (1.21; 9.76) |
| CVD | 0.275 | |||
| DM duration (years) | 0.440 | |||
| HbA1c | 0.159 | |||
| DPN | 0.451 | |||
| Number of amputations in the past | 0.870 | |||
| Number of present DFUs/patient on podiatric assessment | 0.134 | |||
| Foot left/right | 0.666 | |||
| Foot one/both | 0.039 | 4.93 (1.08; 22.42) | 0.232 | |
| PAD | 0.156 | |||
| Charcot foot | 0.379 | |||
| Deformities | 0.547 | |||
| Revascularization (with/without) | 0.902 | |||
| DFU in the past | 0.625 | |||
| Number of pairs of protective footwear after initial podiatric evaluation | 0.176 | |||
| Removable walker | 0.884 | |||
| Infection | 0.371 | |||
| Total cost (EUR) | 0.404 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dragoi, I.I.; Popescu, F.G.; Bowling, F.L.; Bondor, C.I.; Ionac, M. Patients’ Buying Behavior for Non-Reimbursed Off-Loading Devices Used in Diabetic Foot Ulcer Treatment—An Observational Study during COVID-19 Pandemic from a Romanian Physical Therapy Unit. J. Clin. Med. 2023, 12, 6516. https://doi.org/10.3390/jcm12206516
Dragoi II, Popescu FG, Bowling FL, Bondor CI, Ionac M. Patients’ Buying Behavior for Non-Reimbursed Off-Loading Devices Used in Diabetic Foot Ulcer Treatment—An Observational Study during COVID-19 Pandemic from a Romanian Physical Therapy Unit. Journal of Clinical Medicine. 2023; 12(20):6516. https://doi.org/10.3390/jcm12206516
Chicago/Turabian StyleDragoi, Iulia Iovanca, Florina Georgeta Popescu, Frank L. Bowling, Cosmina Ioana Bondor, and Mihai Ionac. 2023. "Patients’ Buying Behavior for Non-Reimbursed Off-Loading Devices Used in Diabetic Foot Ulcer Treatment—An Observational Study during COVID-19 Pandemic from a Romanian Physical Therapy Unit" Journal of Clinical Medicine 12, no. 20: 6516. https://doi.org/10.3390/jcm12206516
APA StyleDragoi, I. I., Popescu, F. G., Bowling, F. L., Bondor, C. I., & Ionac, M. (2023). Patients’ Buying Behavior for Non-Reimbursed Off-Loading Devices Used in Diabetic Foot Ulcer Treatment—An Observational Study during COVID-19 Pandemic from a Romanian Physical Therapy Unit. Journal of Clinical Medicine, 12(20), 6516. https://doi.org/10.3390/jcm12206516









